Abstract
Aim
Several studies have shown high prevalence rates of sleep problems among medical students, including insufficient sleep duration, poor sleep quality, and excessive daytime sleepiness. This review aims to systematically summarize the existing literature on sleep problems among medical students and consequently estimate the prevalence of these disturbances.
Subject and Methods
The MEDLINE, EMBASE, ScienceDirect, and ProQuest Medical databases, the Google Scholar engine, and reference lists of retrieved articles were systematically searched and evaluated for quality.
Results
Forty–three studies involving a total of 18,619 students from 13 countries were included in the analyses. Results showed that the mean pooled sleep duration (K = 16, N = 10,512) was 6.3 h per night for medical students, [95% confidence interval (CI) 6.0–6.6]. The results also indicated that 55% [95% CI 48.0%–62.0%] of students reported poor sleep quality (K = 33, N = 15,462) according to the Pittsburgh Sleep Quality Index (PSQI); the mean pooled score of 6.3. Excessive daytime sleepiness (K = 18, N = 5688) was reported by 31.0% [95% CI 24.4%–37.7%] of students according to the Epworth Sleepiness Scale (ESS). Age and gender were not significant moderators for sleep quality or excessive daytime sleepiness. Some differences were obtained between countries, suggesting that cultural values, local conditions, and environment all have an impact on sleep practices and attitudes.
Conclusion
Sleep problems are highly prevalent among medical students and are therefore a severe problem. Prevention and intervention programs targeting these are therefore highly recommended for future studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Research evidence indicates that sufficient sleep duration and good sleep quality are essential for neurocognitive functioning (Tononi and Cirelli 2006), psychomotor performance (Huber et al. 2004), and physical and mental health (AlDabal and BaHammam 2011). Epidemiological studies have found that sleep problems are associated with an increased risk for cardiovascular disease (US Institute of Medicine Committee on Sleep Medicine and Research 2006), psychiatric problems, particularly mood and anxiety disorders (Hidalgo and Caumo 2002; Krystal 2012), social problems (Eller et al. 2006), road traffic accidents (Stutts et al. 2003; Drake et al. 2010), and reduced academic performance (Belenky et al. 2003; Medic et al. 2017).
The American Academy of Sleep Medicine and the Sleep Research Society jointly recommend 7 hours of sleep per night for adults, and up to 9 hours of sleep per night for adolescents and younger adults to promote optimal health (Watson et al. 2015). However, research has shown that the prevalence of short sleepers, defined as those who get less than 6 hours of sleep per night, increased from 7.6% in 1975 to 9.3% in 2006 (Knutson et al. 2010). In addition, average sleep duration decreased among adults between 1985 and 2012 (Ford et al. 2015). Similarly, sleep duration for adolescents decreased between 1991 and 2012, with an increasing proportion of adolescents getting less than 7 hours of sleep per night (Keyes et al. 2015). Additionally, a recent review showed that 70% of college students get less than 7 hours of sleep per night and have irregular sleep schedules, and that 50% report daytime sleepiness (Hershner and Chervin 2014).
The overall prevalence rate of sleep problems has been estimated to be 20.4% among adults (Hublin et al. 2001) and 25% among adolescents (Ohayon et al. 2000). The higher prevalence rate of sleep problems among adolescents is attributed to an interaction of biological factors, such as changes in chronotype, and environmental factors, such as social evening activities and media use. A combination of these factors may cause later bed-times while getting-up times remain early in the morning (Carskadon et al. 1993). University students, who represent an age group experiencing the transition from adolescence to adulthood, appear to be a high-risk group for sleep problems (Buboltz et al. 2001). This vulnerability can be explained by changes in lifestyle factors, including increased independence, new relationships, academic responsibilities, more night-time activities, and access to alcohol and other substances (Taylor et al. 2013). It is therefore not surprising that approximately 50% of university students exhibit poor sleep quality and/or excessive daytime sleepiness compared to 36% of the general population (Oginska and Pokorski 2006; Lund et al. 2010), and that they suffer from more disturbed sleep than individuals from the general population (Jiang et al. 2015). The above-mentioned sleep problems can negatively affect students’ daytime functioning and academic achievement. A recent study showed, for example, that chronic sleep reduction affected students’ academic performance and predicted the students’ concentration level, even when other lifestyle factors were controlled for (van der Heijden et al. 2018).
Medical students represent a university cohort which appears to be highly vulnerable to sleep problems (Azad et al. 2015). They have increased rates of insufficient sleep duration, poor sleep quality, and excessive daytime sleepiness. For a narrative review, see Azad et al. 2015. Possible explanations for these elevated prevalence rates of sleep problems are the long duration and intensity of academic study, clinical duties that include overnight and on-call shifts, and dealing with illness and death, which can be emotionally challenging (Azad et al. 2015). It is also well established that pre-sleep worries, rumination, and stress-related hyperarousal can negatively affect sleep (Harvey 2000; Thomsen et al. 2003; Akerstedt et al. 2007). All of these are commonly experienced by medical students as their study is very demanding and time-consuming, consequently reducing students’ free-time activities and life–work balance (Yu et al. 2017). In many countries, getting a place at medical school requires high grades, leading to pressure and competition among students, both prior to and after admission. Although multiple studies have investigated sleep problems among medical students, prevalence rates vary greatly between them. This may be the result of cross-cultural diversity, and different assessment methods and/or definitions of what constitutes sleep disturbance (Azad et al. 2015). There is currently no published meta-analysis of sleep problems in medical students. Thus, the present study aims to examine the pooled prevalence of sleep problems in medical students around the world using English language research studies (Medeiros et al. 2001; Lima et al. 2002; Bahammam et al. 2005; Kang and Chen 2009; Zailinawati et al. 2009; Brick et al. 2010; Sahraian and Javadpour 2010; James et al. 2011; Abdulghani et al. 2012; Mazurkiewicz et al. 2012; ElArab et al. 2014; Giri et al. 2013; Pagnin et al. 2014; Rique et al. 2014; Ramamoorthy et al. 2014; Prashanth et al. 2015; Mirghani et al. 2015; Surani et al. 2015; Waqas et al. 2015; Alsaggaf et al. 2016; Elwasify et al. 2016; Kumar and Vandana 2016; Mohammadbeigi et al. 2016; Rasekhi et al. 2016; Saygın et al. 2016; Siddiqui et al. 2016; Wang et al. 2016; Yazdi et al. 2016; Almojali et al. 2017; AlQahtani et al. 2017; Asiri et al. 2018; Corrêa et al. 2017; Fawzy and Hamed 2017; Gladius et al. 2017; Ibrahim et al. 2017; Johnson et al. 2017; Mokros et al. 2017; Najafi Kalyani et al. 2017; Priya et al. 2017; Sarbazvatan et al. 2017; Alnomsi et al. 2018; Nadeem et al. 2018; Rathi et al. 2018).
Sleep problems and their daytime consequences include a wide range of complaints, such as insufficient sleep duration, poor sleep quality, excessive daytime sleepiness, and difficulty initiating and/or maintaining sleep (Azad et al. 2015; Kalmbach et al. 2017). In the current review, sleep problems were defined as including one of three components, namely insufficient sleep duration, poor sleep quality, or excessive daytime sleepiness. Due to the differences in the definition of each of these components as well as used, measurement tools and cut-off values used, each one was meta-analysed separately.
Methods
This systematic review and meta-analysis was guided by the preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement (Liberati et al. 2009).
Data sources and searches
Two members of our review team (MT and NA) independently conducted an electronic literature search using four databases; namely, MEDLINE, EMBASE, ScienceDirect, and ProQuest Medical and Google Scholar engine. The following keywords were used: ‘medical students’ plus ‘sleep disturbance’ or ‘sleep problems’ or ‘sleep quality’ or ‘sleep duration’ or ‘excessive daytime sleepiness’ or ‘sleep disorder’ or ‘sleep habit’ or ‘sleep hygiene’. The search was limited to English language research papers published from inception of the databases until the second week of September 2018. The review team manually screened the references of the identified papers for potential inclusion in the review.
Study selection
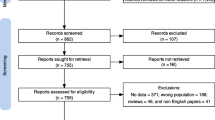
Our review included observational studies that aimed to study the prevalence of sleep problems among medical students. To be included, research studies had to meet the following criteria: (1)published in the English language, (2) date of publication before the second week of September 2018, (3) medical students assessed as the target population, and (4) reported data on the prevalence of sleep disturbance using a validated, commonly utilized measurement tool. Specifically, we included studies that reported sleep duration per night and/or used the Pittsburgh Sleep Quality Index (PSQI) (Buysse et al. 1989) for sleep quality or the Epworth Sleepiness Scale (ESS) (Johns 1991) for excessive daytime sleepiness. Exclusion criteria were: (1) case reports and case series, (2) studies that reported results for medical students with non-medical students in the same group, but without providing a subgroup analysis, (3) lack of study availability and inability to obtain the full text after contacting the authors, and (4) studies that focused on specific sleep disorders (e.g., sleep apnea) among medical students. The flow diagram of study inclusion is shown in Fig. 1.
Outcomes and measures
The anticipated outcome of this systematic review and meta-analysis was to report the prevalence of sleep problems among medical students. The specific measures were to: (1) report the pooled mean duration of sleep per night, (2) determine the average PSQI score and corresponding prevalence of poor sleep quality as measured by the index, (3) determine the prevalence of excessive daytime sleepiness as measured by the ESS, and (4) investigate age, gender, and country as covariates/factors of sleep quality and excessive daytime sleepiness among medical students. Two members of the review team (HJ and MF) independently screened titles, abstracts, and full texts and assessed studies for eligibility criteria, as well as performing the data extraction and research summary. Any disagreements were resolved through discussion with a third reviewer (AA) to reach consensus.
Data extraction
Data were independently extracted by two reviewers (HJ and MT), and checked by a third reviewer (NA or MF). The following information was extracted and tabulated systematically: study authors, study country, study period, sampling method, age, proportion of male gender, sample size, assessment instruments and cut-offs of sleep quality (PSQI) and excessive daytime sleepiness (ESS), and the main key results of sleep prevalence.
Quality evaluation
Two reviewers (HJ and MF) independently assessed the methodological quality of the studies using a standardized checklist consisting of six items in terms of sample size and sampling technique, utilized measurement tools, and statistical analyses. The item scores ranged between zero and six, with scores of zero to two corresponding to low quality, three or four to medium quality, and five or six to high quality. Disagreements between the two reviewers were resolved by consensus after discussion with a third reviewer (AA). See Supplementary Material 1.
Data synthesis and analysis
Data were pooled using random-effects model according to the DerSimonian–Laird method. Results reported prevalence and corresponding 95% confidence intervals (CIs). Furthermore, data were presented graphically using forest plots. An assessment of study heterogeneity using the I2 statistic was performed, with a value of 75–100% considered to represent high heterogeneity. Between-study heterogeneity was also assessed by the Cochran (Q) statistic test and tau2 (τ2). A leave-one-out sensitivity analysis was performed by iteratively removing one study at a time to confirm that our findings were not driven by any single study. The meta-regression technique was applied to examine covariates of sleep quality and daytime sleepiness among medical students, with subgroup analysis being conducted to analyse for the country-of-origin factor among students. Funnel plots were used to visually assess publication bias, and rank-order correlations were also computed. Funnel plots are a visual tool for examining publication bias in meta-analysis. In the present study, we used the funnel plot of precision to produce scatterplots of logit event rate, which is a derivative of prevalence estimate from individual studies (horizontal axis) against a measure of study precision (vertical axis). Standard error was used as a measure of study precision in our plots. Duval and Tweedie’s trim-and-fill procedure was used to calculate adjusted point estimates. Meta-analyses were performed using OpenMetaAnalyst software provided by the Centre for Evidence Synthesis in Health, School of Public Health at Brown University. Funnel plots and related publication bias tests were performed using Comprehensive Meta-Analysis, version 2.0 (Borenstein et al. 2005). Other descriptive statistical analyses were carried out using STATA 14.0 (StataCorp 2015).
Results
Characteristics of included studies
Forty-three studies, involving a total of 18,619 respondents from 13 countries, contributed to the analyses (see Table 1). All of the studies were published after the year 2001, and approximately two-thirds of the literature had been published within the past 5 years. The median number of respondents per study was 278 (range: 27–6085), and their median age was 21 years (range: 19–28 years). Approximately 60% of the participants were females. Table 2 provides a systematic summary of the studies included in this review. The mean score of the quality assessment was 4.2, ranging from 3.0 to 6.0.
All of the 43 studies had an observational, cross-sectional research design. K represents the number of the studies and N represents the number of participants in that particular analysis. Sixteen studies (K = 16, N = 10,512) reported sleep duration. Thirty-three studies (K = 33, N = 15,462) reported the prevalence of poor sleep quality, using the number of events (participants with PSQI ≥ 5) and total study sample size. Twenty-three studies (K = 23, N = 13,403) reported mean PSQI scores and corresponding standard deviations (SD). Finally, 18 studies (K = 18, N = 5688) reported the prevalence of excessive daytime sleepiness, using the number of events (participants with ESS ≥ 10) and total study sample size. All of the studies included in this meta-analysis reported their prevalence rates primarily using standard cut-offs of 5 or 10 points or greater for PSQI and ESS respectively.
Sleep problems among medical students
Sleep duration
Meta-analytic pooling of the point estimates of sleep duration per night yielded that medical students sleep about 6.3 h per night [95% CI 6.0–6.6], with statistically significant evidence of between-study heterogeneity (Q = 1413, τ2 = 0.32, I2 = 98.93%, P < 0.001). Figure 2 demonstrates the results of sleep duration per night. Sensitivity analysis indicated that no study influenced the results by more than 0.1 h of sleep per night analysis. Publication bias was assessed via visual inspection of the funnel plot (Kendall’s τ without continuity correction = 0.21, P = 0.30). This visual inspection of the plot (see Fig. 3) indicated no bias. Duval and Tweedie’s procedure showed that if the point estimate was to be adjusted for bias left or right of the mean, it would remain unchanged for the random effects model.
Sleep quality
Meta-analytic pooling of the point estimates of the PSQI values yielded that medical students scored 6.3 on the PSQI [95% CI 5.7–6.8], with statistically significant evidence of between–study heterogeneity (Q = 2734, τ2 = 1.6, I2 = 99%, P < 0.001). The meta-analytic pooling of the prevalence estimates of poor sleep quality according to the PSQI yielded a pooled prevalence rate of 55%, [95% CI 48.0%–62.0%], with statistically significant evidence of between-study heterogeneity (Q = 2538, τ2 = 0.04, I2 = 98.7%, P < 0.001). The raw prevalence estimates of poor sleep quality reported among medical students using the PSQI ranged from 27.8% to 83.4%. Figure 4 demonstrates the meta-analysis of poor sleep quality. Sensitivity analysis indicated that no study affected the prevalence estimate by more than 1%. A visual inspection of the funnel plot (Kendall’s τ without continuity correction = 0.01, P = 0.09) (see Fig. 5) indicated no publication bias. Duval and Tweedie’s procedure indicated that if the point estimate was to be adjusted for bias left or right of the mean, it would remain unchanged for random effects model.
As a measure of heterogeneity, I2 was 99%, indicating that heterogeneity characterized the studies investigating sleep quality in medical students. In order to explain this figure, covariate analyses were conducted for age and gender. Results revealed that age (β = −0.007, P = 0.721) and gender (β = 0.1, P = 0.694) were not significant moderators for the prevalence of poor sleep quality.
Furthermore, a subgroup analysis of the pooled prevalence of poor sleep quality by country was conducted (see Fig. 6). Results showed that the heterogeneity index as measure by I2 showed an improvement for some countries, with a lower pooled prevalence rate for Brazil 49.9% (95% CI 37.1%–62.8%, I2 = 90.94%, P < 0.001), a higher pooled prevalence rate for Iran 59.9% (95% CI 53.2%–66.6%, I2 = 84%, P < 0.001), and a similar pooled rate to the overall prevalence for Egypt 54.2% (95% CI 51.9%–56.5, I2 = 3.5%, P = 0.3).
Some countries did not show an in improvement in the heterogeneity index; however, their pooled prevalence of poor sleep quality increased by approximately 5%. This included Pakistan with 60.8% (95% CI 38.2%–83.4% I2 = 98.5%, P < 0.001) and Saudi Arabia with 60.5% (95% CI 42.3%–78.8% I2 = 98.8%, P < 0.001).
Excessive daytime sleepiness
The meta–analytic pooling of the estimates of excessive daytime sleepiness yielded a crude prevalence rate of 31.0%, [95% CI 24.4%–37.7%], with statistically significant evidence of between-study heterogeneity (Q = 603, τ2 = 0.02, I2 = 97%, P < 0.001). The raw prevalence estimates of excessive daytime sleepiness reported among medical students using the ESS ranged from 10.3% to 63%, as demonstrated in Fig. 7. Sensitivity analysis indicated that no study affected the prevalence estimate by more than 1%, suggesting that the overall prevalence estimate was powered to the methodological quality of each research study included. A visual inspection of the funnel plot (Kendall’s τ without continuity correction = −0.25, P = 0.13) (see Fig. 8) indicated no publication bias. Duval and Tweedie’s procedure revealed that if the point estimate were to be adjusted for bias left or right of the mean, it would remain unchanged for the random effects model.
I2 was 97%, indicating that heterogeneity characterized the studies investigating excessive daytime sleepiness in medical students. In order to explain this figure, covariate analyses were conducted for age and gender. Results indicated that age (β = 0.12, P = 0.589) and gender (β = 0.27, P = 0.377) were not significant moderators.
Furthermore, a subgroup analysis of the pooled prevalence of excessive daytime sleepiness by country was conducted (see Fig. 9). Results showed that the heterogeneity index as measured by I2 showed an improvement in the heterogeneity index for some countries: with lower pooled prevalence for USA with 28.1% (95% CI 23.7%–32.6%, I2 = 0%, P = 329) and India with 24.7% (95% CI 9.6%–39.8%, I2 = 96%, P < 0.001), or with higher pooled prevalence in the case of Saudi Arabia with 38.4% (95% CI 29.9%–46.8%, I2 = 92.5%, P < 0.001) and Brazil with 52.4% (95% CI 31.9%– 72.9, I2 = 93%, P < 0.001).
Discussion
Results of the current meta-analysis demonstrate that insufficient sleep duration is a common problem among medical students, as they slept on average only 6.3 h per night, which is less than the recommended amount. Additionally, 55% of the students reported poor sleep quality (PSQI≥5) with an average PSQI score of 6.3, and 31.0% reported excessive daytime sleepiness (ESS ≥ 10). Age and gender were not significant moderators for poor sleep quality or excessive daytime sleepiness. Subgroup analysis revealed some differences between countries. The prevalence of poor sleep quality was lower in Brazil, but higher in Iran, Pakistan, and Saudi Arabia, compared to the overall estimate. For excessive daytime sleepiness, India and USA showed a lower prevalence, while Brazil and Saudi Arabia exhibited higher prevalence compared to the overall estimate.
Our results indicate that the sleep duration of medical students is deficient by at least 1, and up to 3 hours, as the sleep duration recommendation is 7 to 9 hours for young adults and adults (Watson et al. 2015). An experiment by van Dongen and colleagues demonstrated that a 2-week restriction of sleep (6 or fewer hours per night) produced cognitive performance deficits comparable to 2 nights of complete sleep deprivation (Dongen et al. 2003). The study concluded that even relatively moderate sleep restriction can seriously impair waking neurobehavioral functions in healthy adults (Dongen et al. 2003). This indicates that insufficient sleep in medical students may severely impair their work. Despite these alarming results, one has to be aware that there are individual differences in sleep need and vulnerability to sleep loss (Dongen et al. 2003). This suggests that some students can function well with this amount of sleep, whereas others may be severely impaired. Therefore, assessing sleep debt, which reflects an individual’s amount of sleep relative to his/her sleep need, might be a better indication of problematic sleep. Additionally, it should be mentioned that the included studies on sleep durations did not address the problem of individuals’ chronotype and sleep regularity. It has been shown that chronotype changes over a lifetime, and individuals become more evening-types during adolescence and young adulthood, peaking at the age of 20 years (Roenneberg et al. 2004), which is in line with the median age of 21 years of the participants in the studies in this meta-analysis. These changes in chronotype imply that adolescents and young adults tend to go to bed late, they still have to get up early in the morning to attend their classes, which leads to an intense sleep debt during the week. Often, individuals compensate this sleep debt at the weekends by sleeping in on Saturday and Sunday mornings. This chronic misalignment between a person’s preferred sleep/wake schedule and sleep/wake timing imposed by his/her work schedule has been referred to as social jetlag (Roenneberg et al. 2004). Supporting the idea that such sleep problems severely affect students’ functioning, it has been shown that students with early chronotypes have better academic achievement (Haraszti et al. 2014; Enright and Refinetti 2017; Zerbini and Merrow 2017; Mirghani 2017) but less psychological well-being (Dimitrov et al. 2018).
A comprehensive meta-analysis of sleep duration and sleep patterns among Chinese university students (including medical students) showed that the pooled mean sleep duration was seven hours per night [95% CI 6.8–7.3] (Li et al. 2017). The same meta-analysis demonstrated that the percentage of students with sleep duration shorter than 7 hours per night was 43.9% [95% CI 36.9%–51.1%] (Li et al. 2017). The variation in sleep duration between our meta-analysis and the meta-analysis from China may indicate that medical students are even more affected by insufficient sleep than other students. On the other hand, the differences may point to discrepancies in socio-economic and cultural factors. Divergent attitudes towards academic achievement and performance are another important cultural aspect. As mentioned before, pre-sleep worries and rumination, which are likely to be associated with academic attitudes and performance pressure, negatively affect students’ sleep (Harvey 2000; Thomsen et al. 2003; Akerstedt et al. 2007).
The present meta-analysis indicates that the majority of medical students experienced poor sleep quality with an average PSQI score of 6.3, which is above the cut-off score used to differentiate good from poor sleepers. Interestingly, the mean global PSQI score of Chinese medical students was around 6.16 in most of the studies included in a Chinese meta-analysis (Yu et al. 2017). These results are of high importance, as they indicate that our findings can be generalized to medical students. Previous studies have shown that poor sleep quality negatively affects students’ academic performance (Veldi et al. 2005; van der Heijden et al. 2018) as well as their psychological well-being, thereby increasing anxiety and depressive symptoms (Abdussalam et al. 2013; Sawyer et al. 2015; Choueiry et al. 2016) and further highlighting the importance of sleep quality for students’ daytime functioning.
Approximately one-third of the medical students experienced excessive daytime sleepiness, which may be the consequence of insufficient sleep duration and/or poor sleep quality. A meta-analysis in adolescents showed that the relationship between excessive daytime sleepiness and academic performance was stronger than the relationship between sleep duration and academic performance or sleep quality and academic performance (Dewald et al. 2010), highlighting the relevance of this problem.
Moderator analyses indicated that age and gender were not significantly associated with sleep quality or excessive daytime sleepiness. The relationship between gender and sleep problems has been controversial among university-age students. For example, results from India (Giri et al. 2013) and Pakistan (Surani et al. 2015) showed that female students had a higher prevalence of sleep problems compared to male students, whereas findings from Iran (Yazdi et al. 2016) and Saudi Arabia (Siddiqui et al. 2016), showed that male students had a higher rate of sleep problems compared to female students. Finally, studies from the USA (Mazurkiewicz et al. 2012) and China (Li et al. 2017) suggested no statistically significant gender difference between males and females. The absence of effect for age may be explained by the narrow age range of the samples included in this meta-analysis. Investigating an age-by-gender interaction may be interesting for future studies, as research has generally shown developmental variation between males and females. Subgroup analyses showed some differences between countries, suggesting that cultural values, local conditions, and environment all play a role in sleep practices and attitudes. This aspect could be explored further by future reviews once a viable number of studies is available.
Based on our results, it can be concluded that the high prevalence of sleep issues among medical students requires ongoing monitoring and accurate diagnosis. Further, management interventions may reduce these problems and possibly prevent the development of sleep disorders such as insomnia, or physical or mental health problems. One approach to improving individuals’ sleep, especially in relatively young samples, is to supply sleep hygiene knowledge, including information on bedtime routines, regular sleep schedules, electronic media use, etc. This approach has the advantage of being relatively cost-effective, since many students can be reached at the same time. However, it has also been shown that sleep hygiene knowledge does not necessarily improve sleep hygiene practice (Brown et al. 2002). Evaluating and applying more individually tailored sleep intervention or treatment programs is therefore recommended for future studies.
Limitations
Findings from the current meta-analysis should be interpreted in light of four main limitations. First, high heterogeneity (as measured by I2) is unavoidable in epidemiological meta-analyses (Sedov et al. 2018; Li et al. 2018). In our meta-analysis, substantial heterogeneity remained despite conducting moderator analyses using meta-regression techniques or after performing subgroup analyses. Due to limited common information in the studies, additional sources of heterogeneity, such as lifestyle factors and stress, could not be explored.
Second, the studies included in this review were all cross-sectional surveys. However, longitudinal research of changes in sleep quality during medical education is needed to understand the factors associated with sleep problems among this population. Third, the prevalence rates were based on self-report instruments. Both the PSQI and the ESS are important clinical and research tools, but they only represent specific aspects of sleep, sleep quality, and excessive daytime sleepiness. Thus, future research is encouraged to investigate other sleep characteristics such as objective sleep quality measurement, including polysomnography. Fourth, most included studies did not differentiate between students with and without sleeping disorders (e.g., insomnia), although this may be relevant for estimating prevalence rates of sleep problems.
Conclusions
Findings from this systematic review and meta-analysis show that medical students experience insufficient sleep duration, with a mean 6.3 h per night. More than half (55%) of the students had poor quality of sleep as measured by the PSQI, and one third (31.0%) experienced excessive daytime sleepiness as measured by the ESS. Future studies are needed to identify, prevent, and treat sleep problems in this population.
References
Abdulghani HM, Alrowais NA, Bin-Saad NS et al (2012) Sleep disorder among medical students: relationship to their academic performance. Med Teach 34(Suppl 1):S37–S41. https://doi.org/10.3109/0142159X.2012.656749
Abdussalam A, Salman MT, Gupta S et al (2013) Poor quality of sleep and its relationship with depression in first year medical students. Adv Life Sience Technol 12:17–21
Akerstedt T, Kecklund G, Axelsson J (2007) Impaired sleep after bedtime stress and worries. Biol Psychol 76:170–173. https://doi.org/10.1016/j.biopsycho.2007.07.010
AlDabal L, BaHammam AS (2011) Metabolic, endocrine, and immune consequences of sleep deprivation. Open Respir Med J 5:31–43. https://doi.org/10.2174/1874306401105010031
Almojali AI, Almalki SA, Alothman AS et al (2017) The prevalence and association of stress with sleep quality among medical students. J Epidemiol Glob Health 7:169–174. https://doi.org/10.1016/j.jegh.2017.04.005
Alnomsi SJ, Albalawi KS, Alali OY et al (2018) The chronotype (eveningness–morningness) effects on academic achievement among medical students in Tabuk City, Saudi Arabia. Egypt J Hosp Med 71:3504–3507
AlQahtani MS, Alkhaldi TM, Al-Sultan AM et al (2017) Sleeping disorders among medical students in Saudi Arabia; in relation to anti-insomnia medications. Egypt J Hosp Med 69(7):2750–2753
Alsaggaf MA, Wali SO, Merdad RA, Merdad LA (2016) Sleep quantity, quality, and insomnia symptoms of medical students during clinical years. Relationship with stress and academic performance. Saudi Med J 37:173–182. https://doi.org/10.15537/smj.2016.2.14288
Asiri AK, Almetrek MA, Alsamghan AS et al (2018) Impact of Twitter and WhatsApp on sleep quality among medical students in King Khalid University, Saudi Arabia. Sleep Hypn 20:247–252
Azad MC, Fraser K, Rumana N et al (2015) Sleep disturbances among medical sudents: a global perspective. J Clin Sleep Med 11:69–74. https://doi.org/10.5664/jcsm.4370
Bahammam AS, Al-Khairy OK, Al-Taweel AA (2005) Sleep habits and patterns among medical students. Neurosci Riyadh Saudi Arab 10:159–162
Belenky G, Wesensten NJ, Thorne DR et al (2003) Patterns of performance degradation and restoration during sleep restriction and subsequent recovery: a sleep dose–response study. J Sleep Res 12:1–12
Borenstein M, Hedges L, Higgins J, Rothstein H (2005) Comprehensive meta-analysis (version 2). Biostat, Englewood
Brick CA, Seely DL, Palermo TM (2010) Association between sleep hygiene and sleep quality in medical students. Behav Sleep Med 8:113–121. https://doi.org/10.1080/15402001003622925
Brown FC, Buboltz WC, Soper B (2002) Relationship of sleep hygiene awareness, sleep hygiene practices, and sleep quality in university students. Behav Med Wash DC 28:33–38. https://doi.org/10.1080/08964280209596396
Buboltz WC, Brown F, Soper B (2001) Sleep habits and patterns of college students: a preliminary study. J Am Coll Health J ACH 50:131–135. https://doi.org/10.1080/07448480109596017
Buysse DJ, Reynolds CF, Monk TH et al (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28:193–213
Carskadon MA, Vieira C, Acebo C (1993) Association between puberty and delayed phase preference. Sleep 16:258–262
Choueiry N, Salamoun T, Jabbour H et al (2016) Insomnia and relationship with anxiety in university students: a cross-sectional designed study. PLoS One 11:e0149643. https://doi.org/10.1371/journal.pone.0149643
de Corrêa CC, de Oliveira FK, Pizzamiglio DS et al (2017) Sleep quality in medical students: a comparison across the various phases of the medical course. J Bras Pneumol 43:285–289. https://doi.org/10.1590/S1806-37562016000000178
Dewald JF, Meijer AM, Oort FJ et al (2010) The influence of sleep quality, sleep duration and sleepiness on school performance in children and adolescents: a meta-analytic review. Sleep Med Rev 14:179–189. https://doi.org/10.1016/j.smrv.2009.10.004
Dimitrov A, Veer IM, Kleeblatt J et al (2018) Chronotype is associated with psychological well-being depending on the composition of the study sample. J Health Psychol 2018:1359105317751618. https://doi.org/10.1177/1359105317751618
Dongen HPAV, Rogers NL, Dinges DF (2003) Sleep debt: theoretical and empirical issues. Sleep Biol Rhythms 1:5–13. https://doi.org/10.1046/j.1446-9235.2003.00006.x
Drake C, Roehrs T, Breslau N et al (2010) The 10-year risk of verified motor vehicle crashes in relation to physiologic sleepiness. Sleep 33:745–752
ElArab HE, Rabie MA, Ali DH (2014) Sleep behavior and sleep problems among a medical student sample in relation to academic performance: a cross-sectional questionnaire-based study. Middle East Curr Psychiatry 21:72–80
Eller T, Aluoja A, Vasar V, Veldi M (2006) Symptoms of anxiety and depression in Estonian medical students with sleep problems. Depress Anxiety 23:250–256. https://doi.org/10.1002/da.20166
Elwasify M, Barakat DH, Fawzy M et al (2016) Quality of sleep in a sample of Egyptian medical students. Middle East Curr Psychiatry 23:200–207
Enright T, Refinetti R (2017) Chronotype, class times, and academic achievement of university students. Chronobiol Int 34:445–450. https://doi.org/10.1080/07420528.2017.1281287
Fawzy M, Hamed SA (2017) Prevalence of psychological stress, depression and anxiety among medical students in Egypt. Psychiatry Res 255:186–194. https://doi.org/10.1016/j.psychres.2017.05.027
Ford ES, Cunningham TJ, Croft JB (2015) Trends in self-reported sleep duration among US adults from 1985 to 2012. Sleep 38:829–832. https://doi.org/10.5665/sleep.4684
Giri PA, Baviskar MP, Phalke DB (2013) Study of sleep habits and sleep problems among medical students of Pravara Institute of Medical Sciences Loni, Western Maharashtra, India. Ann Med Health Sci Res 3:51–54
Gladius H, Sowmiya K, Vidya D et al (2017) A study of mobile phone usage on sleep disturbance, stress and academic performance among medical students in Tamil Nadu. Int J Community Med Public Health 5:365–368. https://doi.org/10.18203/2394-6040.ijcmph20175814
Haraszti RÁ, Ella K, Gyöngyösi N et al (2014) Social jetlag negatively correlates with academic performance in undergraduates. Chronobiol Int 31:603–612. https://doi.org/10.3109/07420528.2013.879164
Harvey AG (2000) Pre-sleep cognitive activity: a comparison of sleep-onset insomniacs and good sleepers. Br J Clin Psychol 39(Pt 3):275–286
Hershner SD, Chervin RD (2014) Causes and consequences of sleepiness among college students. Nat Sci Sleep 6:73–84. https://doi.org/10.2147/NSS.S62907
Hidalgo MP, Caumo W (2002) Sleep disturbances associated with minor psychiatric disorders in medical students. Neurol Sci 23:35–39. https://doi.org/10.1007/s100720200021
Huber R, Ghilardi MF, Massimini M, Tononi G (2004) Local sleep and learning. Nature 430:78–81. https://doi.org/10.1038/nature02663
Hublin C, Kaprio J, Partinen M, Koskenvuo M (2001) Insufficient sleep—a population-based study in adults. Sleep 24:392–400
Ibrahim N, Badawi F, Mansouri Y et al (2017) Sleep quality among medical students at King Abdulaziz University:a cross-sectional study. J Community Med Health Educ 7:1–6. https://doi.org/10.4172/2161-0711.1000561
Institute of Medicine (US) Committee on Sleep Medicine and Research (2006) Sleep disorders and sleep deprivation: an unmet public health problem. National Academies Press (US), Washington (DC)
James BO, Omoaregba JO, Igberase OO (2011) Prevalence and correlates of poor sleep quality among medical students at a Nigerian university. Ann Niger Med 5:1–5. https://doi.org/10.4103/0331-3131.84218
Jiang X, Hardy LL, Baur LA et al (2015) Sleep duration, schedule and quality among urban Chinese children and adolescents: associations with routine after-school activities. PLoS One 10:e0115326. https://doi.org/10.1371/journal.pone.0115326
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14:540–545
Johnson KM, Simon N, Wicks M et al (2017) Amount of sleep, daytime sleepiness, hazardous driving, and quality of life of second year medical students. Acad Psychiatry 41:669–673
Kalmbach DA, Arnedt JT, Song PX et al (2017) Sleep disturbance and short sleep as risk factors for depression and perceived medical errors in first-year residents. Sleep 40. https://doi.org/10.1093/sleep/zsw073
Kang J-H, Chen S-C (2009) Effects of an irregular bedtime schedule on sleep quality, daytime sleepiness, and fatigue among university students in Taiwan. BMC Public Health 9:248
Keyes KM, Maslowsky J, Hamilton A, Schulenberg J (2015) The great sleep recession: changes in sleep duration among US adolescents, 1991–2012. Pediatrics 135:460–468. https://doi.org/10.1542/peds.2014-2707
Knutson KL, Van Cauter E, Rathouz PJ et al (2010) Trends in the prevalence of short sleepers in the USA: 1975–2006. Sleep 33:37–45
Krystal AD (2012) Psychiatric disorders and sleep. Neurol Clin 30:1389–1413. https://doi.org/10.1016/j.ncl.2012.08.018
Kumar A, Vandana AAN (2016) Analgesics self-medication and its association with sleep quality among medical undergraduates. J Clin Diagn Res JCDR 10:FC07–FC11. https://doi.org/10.7860/JCDR/2016/22504.8953
Li L, Wang Y-Y, Wang S-B et al (2017) Sleep duration and sleep patterns in Chinese university students: a comprehensive meta-analysis. J Clin Sleep Med 13:1153–1162. https://doi.org/10.5664/jcsm.6760
Li L, Wang Y-Y, Wang S-B et al (2018) Prevalence of sleep disturbances in Chinese university students: a comprehensive meta-analysis. J Sleep Res 27(3):e12648. https://doi.org/10.1111/jsr.12648
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6:e1000100. https://doi.org/10.1371/journal.pmed.1000100
Lima PF, Medeiros ALD, Araujo JF (2002) Sleep–wake pattern of medical students: early versus late class starting time. Braz J Med Biol Res 35:1373–1377
Lund HG, Reider BD, Whiting AB, Prichard JR (2010) Sleep patterns and predictors of disturbed sleep in a large population of college students. J Adolesc Health 46:124–132. https://doi.org/10.1016/j.jadohealth.2009.06.016
Mazurkiewicz R, Korenstein D, Fallar R, Ripp J (2012) The prevalence and correlations of medical student burnout in the pre-clinical years: a cross-sectional study. Psychol Health Med 17:188–195. https://doi.org/10.1080/13548506.2011.597770
Medeiros ALD, Mendes DB, Lima PF, Araujo JF (2001) The relationships between sleep–wake cycle and academic performance in medical students. Biol Rhythm Res 32:263–270
Medic G, Wille M, Hemels ME (2017) Short- and long-term health consequences of sleep disruption. Nat Sci Sleep 9:151–161. https://doi.org/10.2147/NSS.S134864
Mirghani HO (2017) The effect of chronotype (morningness/eveningness) on medical students’ academic achievement in Sudan. J Taibah Univ Med Sci 12:512–516. https://doi.org/10.1016/j.jtumed.2017.03.007
Mirghani HO, Mohammed OS, Almurtadha YM, Ahmed MS (2015) Good sleep quality is associated with better academic performance among Sudanese medical students. BMC Res Notes 8:706. https://doi.org/10.1186/s13104-015-1712-9
Mohammadbeigi A, Absari R, Valizadeh F et al (2016) Sleep quality in medical students; the impact of over-use of mobile cell-phone and social networks. J Res Health Sci 16:46–50
Mokros Ł, Witusik A, Michalska J et al (2017) Sleep quality, chronotype, temperament and bipolar features as predictors of depressive symptoms among medical students. Chronobiol Int 34:708–720. https://doi.org/10.1080/07420528.2017.1316730
Nadeem A, Cheema MK, Naseer M, Javed H (2018) Assessment of sleep quality and patterns suggestive of somniopathies among students of Army Medical College, Rawalpindi. Pak Armed Forces Med J 68 (1):143–148
Najafi Kalyani M, Jamshidi N, Salami J, Pourjam E (2017) Investigation of the relationship between psychological variables and sleep quality in students of medical sciences. Depress Res Treat 2017:7143547. https://www.hindawi.com/journals/drt/2017/7143547/. Accessed 13 Apr 2018
Oginska H, Pokorski J (2006) Fatigue and mood correlates of sleep length in three age-social groups: school children, students, and employees. Chronobiol Int 23:1317–1328. https://doi.org/10.1080/07420520601089349
Ohayon MM, Roberts RE, Zulley J et al (2000) Prevalence and patterns of problematic sleep among older adolescents. J Am Acad Child Adolesc Psychiatry 39:1549–1556
Pagnin D, de Queiroz V, Carvalho YTMS et al (2014) The relation between burnout and sleep disorders in medical students. Acad Psychiatry 38:438–444. https://doi.org/10.1007/s40596-014-0093-z
Prashanth S, Kavyashree HM, Krishnamurthy L et al (2015) Quality of sleep in medical students. J Public Health Med Res 3:8–10
Priya J, Singh J, Kumari S (2017) Study of the factors associated with poor sleep among medical students. Indian J Basic Appl Med Res 6:422–429
Ramamoorthy S, Mohandas MP, Sembulingam P et al (2014) Prevalence of excessive daytime sleepiness (EDS) among medical students. World J Pharm Res 3(4)
Rasekhi S, Ashouri FP, Pirouzan A (2016) Effects of sleep quality on the academic performance of undergraduate medical students. Health Scope 5:e31641
Rathi A, Ransing RS, Mishra KK, Narula N (2018) Quality of sleep among medical students: relationship with personality traits. J Clin Diagn Res 12(9):VC01–VC04
Rique GLN, Fernandes Filho GMC, Ferreira ADC, de Sousa-Muñoz RL (2014) Relationship between chronotype and quality of sleep in medical students at the Federal University of Paraiba, Brazil. Sleep Sci 7:96–102. https://doi.org/10.1016/j.slsci.2014.09.004
Roenneberg T, Kuehnle T, Pramstaller PP et al (2004) A marker for the end of adolescence. Curr Biol CB 14:R1038–R1039. https://doi.org/10.1016/j.cub.2004.11.039
Sahraian A, Javadpour A (2010) Sleep disruption and its correlation to psychological distress among medical students. Shiraz E Med J 11:12–17
Sarbazvatan H, Amini A, Aminisani N, Shamshirgaran SM (2017) Sleep quality and academic progression among students of Tabriz University of Medical Sciences, Northwest of Iran. Res Dev 6:29–33
Sawyer A, Fisher A, Llewellyn C, Gregory AM (2015) Self-reported sleep quality, weight status and depression in young adult twins and siblings. BMC Obes 2:50. https://doi.org/10.1186/s40608-015-0079-8
Saygın M, Öztürk Ö, Gonca T et al (2016) Investigation of sleep quality and sleep disorders in students of medicine. Turk Thorac J 17:132–140. https://doi.org/10.5578/ttj.30513
Sedov ID, Cameron EE, Madigan S, Tomfohr-Madsen LM (2018) Sleep quality during pregnancy: A meta-analysis. Sleep Med Rev 38:168–176. https://doi.org/10.1016/j.smrv.2017.06.005
Siddiqui AF, Al-Musa H, Al-Amri H et al (2016) Sleep patterns and predictors of poor sleep quality among medical students in King Khalid University, Saudi Arabia. Malays J Med Sci 23:94–102. https://doi.org/10.21315/mjms2016.23.6.10
StataCorp (2015) Stata Statistical Software: Release 14. StataCorp LP, College Station, TX
Stutts JC, Wilkins JW, Scott Osberg J, Vaughn BV (2003) Driver risk factors for sleep-related crashes. Accid Anal Prev 35:321–331
Surani AA, Zahid S, Surani A et al (2015) Sleep quality among medical students of Karachi, Pakistan. J Pak Med Assoc 65:380–382
Taylor DJ, Bramoweth AD, Grieser EA et al (2013) Epidemiology of insomnia in college students: relationship with mental health, quality of life, and substance use difficulties. Behav Ther 44:339–348. https://doi.org/10.1016/j.beth.2012.12.001
Thomsen DK, Mehlsen MY, Christensen S, Zachariae R (2003) Rumination--relationship with negative mood and sleep quality. Personal Individ Differ 34:1293–1301. https://doi.org/10.1016/S0191-8869(02)00120-4
Tononi G, Cirelli C (2006) Sleep function and synaptic homeostasis. Sleep Med Rev 10:49–62. https://doi.org/10.1016/j.smrv.2005.05.002
van der Heijden KB, Vermeulen MCM, Donjacour CEHM et al (2018) Chronic sleep reduction is associated with academic achievement and study concentration in higher education students. J Sleep Res 27:165–174. https://doi.org/10.1111/jsr.12596
Veldi M, Aluoja A, Vasar V (2005) Sleep quality and more common sleep-related problems in medical students. Sleep Med 6:269–275. https://doi.org/10.1016/j.sleep.2004.12.003
Wang L, Qin P, Zhao Y et al (2016) Prevalence and risk factors of poor sleep quality among Inner Mongolia Medical University students: A cross-sectional survey. Psychiatry Res 244:243–248. https://doi.org/10.1016/j.psychres.2016.04.011
Waqas A, Khan S, Sharif W et al (2015) Association of academic stress with sleeping difficulties in medical students of a Pakistani medical school: a cross sectional survey. PeerJ 3:e840. https://doi.org/10.7717/peerj.840
Watson NF, Badr MS, Belenky G et al (2015) Recommended amount of sleep for a healthy adult: a joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep 38:843–844. https://doi.org/10.5665/sleep.4716
Yazdi Z, Loukzadeh Z, Moghaddam P, Jalilolghadr S (2016) Sleep hygiene practices and their relation to sleep quality in medical students of Qazvin University of Medical Sciences. J Caring Sci 5:153–160. https://doi.org/10.15171/jcs.2016.016
Yu D, Ren Q, Dong B et al (2017) The sleep quality of medical students in China: a meta-analysis. Sleep Biol Rhythms 15:299–310. https://doi.org/10.1007/s41105-017-0118-6
Zailinawati AH, Teng CL, Chung YC et al (2009) Daytime sleepiness and sleep quality among Malaysian medical students. Med J Malaysia 64:108–110
Zerbini G, Merrow M (2017) Time to learn: How chronotype impacts education. PsyCh J 6:263–276. https://doi.org/10.1002/pchj.178
Author information
Authors and Affiliations
Contributions
HJ and AA designed the study. MT, NA and MF conducted electronic and manual literature search. HJ performed statistical analyses and wrote the first draft along with JDF. AA and MF provided intellectual contributions to strengthening the manuscript and suggested additional data analyses. All authors provided critical revisions of manuscript and approved the final version.
Corresponding author
Ethics declarations
Ethical approval
This article does not contain any studies with human participants performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Conflict of interest statement
The authors declare that there is no conflict of interest regarding the publication of this article.
Declaration of competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOC 49 kb)
Rights and permissions
About this article
Cite this article
Jahrami, H., Dewald-Kaufmann, J., Faris, M.AI. et al. Prevalence of sleep problems among medical students: a systematic review and meta-analysis. J Public Health (Berl.) 28, 605–622 (2020). https://doi.org/10.1007/s10389-019-01064-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10389-019-01064-6