Abstract
Sleep quality of medical students has generated conflicting results in China. The aim of this study was to evaluate the sleep quality of medical students in China by meta-analysis. Electronic databases were searched for studies concerning the sleep quality of medical students using the Pittsburgh sleep quality index (PSQI) published before March 6, 2017. Pooled weighted mean difference (WMD) and 95% confidence interval (95% CI) were estimated with fixed or random effect models depending on the heterogeneity. Subgroup analyses, sensitivity analyses and publication bias were also performed. Eleven studies (7154 medical students and 9073 non-medical students) were included in this meta-analysis. The sleep quality of medical students was significantly higher in scores of subjective sleep quality (WMD, 0.137; 95% CI 0.049–0.224; P = 0.002), sleep duration (WMD, 0.147; 95% CI 0.069–0.225; P < 0.001), daytime dysfunction (WMD, 0.194; 95% CI 0.077–0.311; P = 0.001) and the total scores (WMD, 0.524; 95% CI 0.152–0.896; P = 0.006). On the contrary, there was no significant difference in sleep latency, habitual sleep efficiency, sleep disturbance and use of sleeping medications. This meta-analysis indicates that the sleep quality of medical students is worse than non-medical students in China. Further large and well-designed studies are needed to confirm these findings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sleep is an essential part of daily living and is vital to maintaining normal levels of physical activities and cognitive skills [1, 2]. As recommended, adolescents (10–17 years old) sleep for 8.5–9.5 h per night and those persons ≧18 years of age obtain 7–9 h of sleep per night [3]. Adequate quality sleep is important for human. Lack of sleep or inadequate sleep can lead to brain dysfunction, immunological and metabolic collapse, and if it is sufficiently prolonged, it will ultimately lead to death [4]. What is more, poor sleep quality has been associated with increased medical expenses, poor working performance, and elevated risk for psychiatric disorders [5]. In a word, it has a negative effect on general health and also on quality of life [6].
Because of the unique setting of living condition such as added stress with academic challenge, social interaction within the mixed cultural pool, medical students have high prevalence of mental distress [7]. And it is suggested that medical students experience high rates of emotional problems and suicidal ideation such as anxiety, depression, burnout or even symptoms resembling post-traumatic stress disorder [8, 9]. Beginning as early as the 1960s, a lot of articles have emphasized the need to offer support for medical students to protect and enhance their self-care and well-being [10, 11]. The physical and mental health of medical students has got more and more attention. Due to academics and rigorous clinical training, medical students are very easy to developing sleep impairment and medical students are regarded as a population that is more susceptible to sleep-related problems [12, 13]. Poor sleep quality among medical students not only affects learning, memory and cognition, but also leads to physical and psychological morbidities [14].
The sleep quality of medical students has been most extensively studied and discussed in China, it may be caused by the special background of Chinese medical education. The system of higher medical education is different all over the world [15]. Different from the single medical education system for other countries, there are several medical education systems coexistent in China including the five system levels of 3, 5, 6, 7, 8 [16]. But the system levels of 3 and 5 are the main types, so the total medical education systems are pretty shorter than other countries [16]. In addition, most of the countries strictly limit the enrollment of medical students [17]. But in China after the enrollment expansion policy of colleges and universities beginning in the end of 1990s, the amount of medical students has become more numerous which cause high employment pressure to medical students [18]. And most of them do not want to work in grassroots communities, central and western parts of China [19]. In this context, the employment pressure of medical students is rising, and it is higher than other countries [19]. To control the influence of different cultural backgrounds, races and related factors on sleep quality, only Chinese medical students were chosen in this meta-analysis.
As we know, the gold standard for the assessment of sleep quality is polysomnography (PSG) and/or electroencephalographic (EEG) spectral content analysis, but both kinds of them have practical limits in large sample studies and in field studies [20]. To overcome these limitations, self-report retrospective and prospective questionnaires have been developed. The most widely used standardized questionnaire is the Pittsburgh sleep quality index (PSQI), which is designed to measure sleep quality over the previous month [21].
The PSQI questionnaire measures subjective sleep quality, sleep habits and sleep disturbances over a 1-month period, and discriminate between normal and poor sleepers [22]. It contains 19 self-rated items with 7 components (subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medications, and daytime dysfunction). Each component is scored from 0 to 3, the seven components of the PSQI scores were then added to produce a global PSQI score ranging from 0 to 21. The PSQI has developed together with an effort to adapt it to different cultures and languages [23, 24]. It was revealed that PSQI had a good internal consistency, test–retest reliability, and high validity in Chinese [25].
Though the PSQI questionnaire has been widely used in evaluating the sleep quality of medical students in China, but the result is inconsistent. In order to derive a more precise estimation, we carried out a meta-analysis to summarize the eligible articles by increasing the sample sizes. This research will inform intervention targets and provide direction for further research into the sleep quality of medical students.
Materials and methods
Literature search and selection of studies
A systematic literature search was performed towards the electronic databases including PubMed, Web of Science (SCIE), Chinese Biomedical Database (CBM), the Chinese National Knowledge Infrastructure (CNKI), the Chinese Wanfang Database, the Chinese VIP Database and searched for studies up to March 6, 2017, using the following terms: (‘‘medical students’’ or ‘‘medical college students’’ or “medical undergraduates” or “college students” or “university students” or “undergraduates”) AND (“sleep quality” or “quality of sleep” or “sleeping quality” or “sleep disorder” or “sleep disorders” or “sleep–wake disorder” or “sleep disturbance”) AND (“PSQI” or “the Pittsburgh sleep quality index”) by two researches. On the other hand, we searched the reference to identify other potential articles.
Inclusion and exclusion criteria
To meet the analysis requirements, included studies should fulfill the following criteria: (a) studies of cross-sectional observational design; (b) sleep quality was assessed by Pittsburgh sleep quality index (PSQI); (c) two groups of participants including medical students and non-medical students; (d) the study reported complete information on the mean and standard deviation of seven dimensions of PSQI; (e) studies conducted in Chinese population. Studies were excluded if they met the following criteria: (a) case reports, reviews, lectures, editorials or correspondence letters; (b) only the most recent ones with the most complete dataset were ultimately selected if there were duplicated studies; (c) difference studies presenting the same comparison(s) were excluded to prevent overrepresentation.
Data extraction and quality assessment
For studies included in this meta-analysis, a standard data extraction form was used by two reviewers and the consensus was achieved for all data. First author, year of publication, sampling methods, sampling area, sample size, male to female ratio (M:F), mean and standard deviation of seven dimensions and global PSQI scores in medical students and non-medical students were extracted. The quality of the studies included in this meta-analysis was assessed by an 11-item checklist which was recommended by Agency for Healthcare Research and Quality (AHRQ) [26]. An item would be scored “1” if it was answered “yes”; if it was answered “no” or “unclear”, then the item scored “0”. Article quality was assessed as follows: low quality = 0–3; moderate quality = 4–7; high quality = 8–11.
Statistical analysis
Data management and statistical analyses were completed with the STATA software (version 14.0; Stata Corp, College Station, TX, USA). If a study gave sample sizes, means and standard deviations separately for non-medical students with different majors, this paper combined them into a single group. Pooled weighted mean difference (WMD) and 95% confidence interval (95% CI) were used to assess the sleep quality between medical school students and non-medical school students. The heterogeneity across individual studies was evaluated with Q statistic (P < 0.10 was considered to be of statistical significance) and I 2 statistic (I 2 > 50% was considered to be of statistical significance) [27]. If there was no heterogeneity, the fixed effects model was used; otherwise, the random effects model was used [28, 29]. To identify potential sources of heterogeneity, subgroup analysis were carried out based on male to female ratio and study area. Publication bias was tested by Begg’s and Egger’s test. [30, 31]. Sensitivity analyses were performed by omitting one study each time to reflect the accuracy and stability of the analytic results. Statistical significance was defined as two-sided P value less than 0.05.
Results
Characteristics of studies
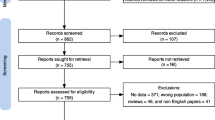
The initial search yielded 2232 articles, 2221 of them were rejected after further screening. Finally, a total of 11 full text articles satisfied the inclusion and exclusion criteria, including 7154 medical students and 9073 non-medical students [32,33,34,35,36,37,38,39,40,41,42]. All of them were performed in Chinese population. Figure 1 describes the procedure for study selection. The main characteristics of eligible studies are shown in Table 1.
Quantitative data synthesis
The main results of the meta-analysis are summarized in Table 2. The sleep quality of medical students was significantly higher in scores of subjective sleep quality (WMD, 0.137; 95% CI 0.049–0.224; P = 0.002), sleep duration (WMD, 0.147; 95% CI 0.069–0.225; P < 0.001), daytime dysfunction (WMD, 0.194; 95% CI 0.077–0.311; P = 0.001) and the total scores (WMD, 0.524; 95% CI 0.152–0.896; P = 0.006). On the contrary, there was no significant difference in sleep latency, habitual sleep efficiency, sleep disturbance and use of sleeping medications. The forest plots are shown in Figs. 2, 3, 4, 5, 6, 7, 8, 9.
Table 3 presents the results of subgroup analysis. Because of the limit information provided by the original studies, subgroup analysis based on male to female ratio was performed in our study. It was divided into two groups according to the characteristic of the data. The first one was the group of gender imbalance that the difference between male to female ratio was greater than 0.15, the other one was the group of gender balance which was considered that the difference between male to female ratio was less than or equal to 0.15. It showed statistical significance in subjective sleep quality, sleep duration, sleep disturbance, daytime dysfunction and the total scores in the group of gender imbalance. And there was no significance in sleep latency, habitual sleep efficiency and use of sleeping medications. It also showed statistical significance in subjective sleep quality, sleep duration, daytime dysfunction and the total scores in the group of gender balance. And there was no significance in sleep latency, habitual sleep efficiency, sleep disturbance and use of sleeping medications.
Publication bias and sensitivity analysis
Publication bias was not detected in Begg’s tests except for sleep duration (Table 2). Egger regression tests did not suggest a significant publication bias for habitual sleep efficiency and use of sleeping medications. However, Egger tests indicated a significant publication bias in other components and the total scores (Table 2). Sensitivity analysis sequentially excluding each individual study did not significantly change the pooled WMDs except for the use of sleeping medications and the total scores (Figs. S1–S8). When the research of Wei [34] was excluded, the result changed to WMD, −0.019; 95% CI −0.036 to −0.002 for the study of use of sleeping medications and WMD, 0.450; 95% CI −0.0004–0.900 for the total scores.
Discussion
Medicine is recognized as one of the most stressful fields of education and medical students are regarded as a population that is more susceptible to sleep-related problems [13, 43]. Purim KS’s study conducted in Brazil showed the total scores of PSQI was 5.90 ± 2.39 in medical students [44]. However, the mean global PSQI score of Chinese medical students was around 6.16 in most of the studies included in this meta-analysis. The components of PSQI and the total scores of Purim KS’s study were better than most Chinese medical students except for use of sleeping medications. The study conducted in Lithuanian showed that the global PSQI scores was 7.3 ± 2.9 for medical students, it was worse than most of the medical students in China [45]. A study conducted by Giri P revealed that the global PSQI scores were 5.28 ± 2.39 in Indian medical undergraduates [46]. Most of the studies included in this meta-analysis were worse than this study. Because of the different cultural backgrounds, the PSQI of medical students make a great difference all over the world.
In this circumstance, we conducted this study to learn the sleep conditions of Chinese medical students comprehensively. As far as we know, this meta-analysis represents the first effort to systematically assess the sleep quality of medical students.
Based on 11 cross-sectional studies, this meta-analysis revealed that the sleep quality of Chinese medical students was significantly worse in respect of total scores, subjective sleep quality, sleep duration and daytime dysfunction domains. Whereas, no significant difference was observed in sleep latency, habitual sleep efficiency, sleep disturbance and use of sleeping medications. However, the sensitivity analysis changed the results of use of sleeping medications and the total scores. When the study of Wei [34] was excluded, the results of them had been changed. It might be caused by the large sample size of Wei’s study. There were only 7154 medical students; the study of Wei occupied 2368. In addition, the authors compared the sleep quality of medical students with engineering students. But the male to female ratio was seriously unbalanced between two groups. In the medical students, the male to female ratio was 590:1778; nevertheless, it was 1038:604 in the engineering students. So, the results revealed by this meta-analysis should be interpreted with caution. Because of the high heterogeneity detected in this meta-analysis, we conducted subgroup analysis to explore the source of heterogeneity. Poor sleep quality is often attributed to a range of modifiable, and non-modifiable factors [47]. Gender is identified as a vital role among non-modifiable factors, as many studies report a higher rate of sleep problems in females [48]. But owing to the insufficient information, we could only carry out subgroup analysis based on the male to female ratio. According to the characteristic of the data, studies were divided into two groups (the group of gender imbalance and the group of gender balance). The group of gender imbalance still had high heterogeneity and results showed that the sleep quality of medical students was significantly worse in terms of subjective sleep quality, sleep duration, sleep disturbance, daytime dysfunction and the total scores domains. But we should make conclusions with caution on account of the unbalance male to female ratio. However, in the group of gender balance, the heterogeneity got much smaller. On this basis, we speculated that the unbalance of male to female ratio might be a source of the heterogeneity. In this group, the results had statistical significance in terms of subjective sleep quality, sleep duration, daytime dysfunction and total scores domains. There was still no significance in sleep latency, habitual sleep efficiency, sleep disturbance and use of sleeping medications. And the results in the group of gender balance were consistent with the overall results.
Meta-analysis is known as a method to increase the sample size and statistical power for a more reliable result through combining comparable articles. In this meta-analysis, it was revealed that the sleep quality of medical students was worse than non-medical students in some domains. University students should deal with stressors, such as long class schedules, overloaded lessons, and academic performance concerns [49]. Medical students are often thought to have more stressors than most of non-medical students like less free time, longer courses, and longer working hours [50]. When they feel difficult to manage the stress, these stressors may lead to sleep disorders in them [51]. Because of the highly demand of professional and academic requirements, medical students have to reduce their sleeping hours to achieve their desired goal [52]. Due to the reduction of sleeping hours, the sleep duration of medical students was worse than non-medical students. Due to the lack of sleep, they feel tired and sleepy; so the daytime dysfunction and subjective sleep quality are worse. Though their sleeping time is short, but the time they spend to fall asleep have no significance compared with non-medical students and there is no other special thing to influence their sleeping. In a word, the results are mainly caused by the insufficient sleep hours. Though, medical students want to achieve their goal through the reduction of sleeping hours. It is also reported that poor sleep quality has been correlated with worse academic achievement before exams [53]. And poor sleep quality frequently co-occurs with mental disorders. So, effective measures are needed to improve the situation in this population. The stress should be reduced in this population. Teachers and parents should tell them the right way to face the pressure. And medical students should correct their attitudes towards various stressful things.
This study provided the evidence of sleep quality of medical students was worse than non-medical students in China. But, results in the present meta-analysis should be interpreted with caution due to the following limitations. Firstly, publication bias was detected in our meta-analysis. Secondly, only eleven Chinese published studies were ultimately included in this meta-analysis. We undoubtedly missed some potential studies in other languages, which may be one reason for the publication bias. Thirdly, this study was based on individual unadjusted estimates without adjusted for potentially confounding factors such as gender, grade, body mass index (BMI), family background and other factors. Fourthly, only cross-sectional studies were adopted which was not sufficiently powerful to demonstrate a causal relationship.
In conclusion, this meta-analysis suggests that the sleep quality of medical students is worse than non-medical students in China. Given the limitations of the studies included in the meta-analysis, further studies with more well-designed investigations are required to validate our results.
References
Ohayon MM, Carskadon MA, Guilleminault C, et al. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. 2004;27:1255–73.
Prehn-Kristensen A, Munz M, Molzow I, et al. Sleep promotes consolidation of emotional memory in healthy children but not in children with attention-deficit hyperactivity disorder. PLoS One. 2013;8:e65098.
Assaad S, Costanian C, Haddad G, et al. Sleep patterns and disorders among university students in Lebanon. J Res Health Sci. 2014;14:198–204.
Tononi G, Cirelli C. Sleep and the price of plasticity: from synaptic and cellular homeostasis to memory consolidation and integration. Neuron. 2014;81:12–34.
Curcio G, Tempesta D, Scarlata S, et al. Validity of the Italian version of the Pittsburgh sleep quality index (PSQI). Neurol Sci. 2013;34:511–9.
Asghari A, Farhadi M, Kamrava SK, et al. Subjective sleep quality in urban population. Arch Iran Med. 2012;15:95–8.
Melese B, Bayu B, Wondwossen F, et al. Prevalence of mental distress and associated factors among Hawassa University medical students, Southern Ethiopia: a cross-sectional study. BMC Res Notes. 2016;9:485.
Doulougeri K, Panagopoulou E, Montgomery A. (How) do medical students regulate their emotions? BMC Med Educ. 2016;16:312.
Rotenstein LS, Ramos MA, Torre M, et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: a systematic review and meta-analysis. JAMA. 2016;316:2214–36.
Earley LW, Johnson DG. Medical student health. J Med Educ. 1969;44:35–45.
Dyrbye LN, Shanafelt TD. Medical student distress: a call to action. Acad Med. 2011;86:801–3.
Surani AA, Zahid S, Surani A, et al. Sleep quality among medical students of Karachi. Pak J Pak Med Assoc. 2015;65:380–2.
Alsaggaf MA, Wali SO, Merdad RA, et al. Sleep quantity, quality, and insomnia symptoms of medical students during clinical years. Relationship with stress and academic performance. Saudi Med J. 2016;37:173–82.
Sahraian A, Javadopur A. Sleep disruption and its correlation to psychological distress among medical students. Shiraz E Med J. 2010;11:12–7.
Yin J. Comparison of academic degree and schooling length of clinical medicine between China and foreign countries [In Chinese]. China Med Educ Technol. 2016;30:502–7.
Lu GN. A comparative study based on Chinese and foreign higher medical education system [In Chinese]. Asia-Pac Educ. 2015:120.
Huang ZJ, Wu YX. Medical educational model in foreign countries and schooling system reform of medical education in China [In Chinese]. Northwest Med Educ. 2007;15:573–5.
Luo BC, Shi W, Li Y, et al. Excellent doctor education and the re-orientation of the development of Chinese medical education [In Chinese]. Med Philos (A). 2016;37:74–8.
Cai Y. In the context of new medical reform policy, the employment situation of medical students and a survey of strategies. [In Chinese]. Hum Resour Dev. 2016:138–139.
Krystal AD, Edinger JD. Measuring sleep quality. Sleep Med. 2008;9:S10–7.
Buysse DJ, Reynolds CF, Monk TH, et al. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213.
Shim J, Kang SW. Behavioral factors related to sleep quality and duration in adults. J Lifestyle Med. 2017;7:18–26.
Bertolazi AN, Fagondes SC, Hoff LS, et al. Validation of the Brazilian Portuguese version of the Pittsburgh sleep quality index. Sleep Med. 2011;12:70–5.
Doi Y, Minora M, Uchiyama M, et al. Psychometric assessment of subjective sleep quality using the Japanese version of the Pittsburgh sleep quality index (PSQI-J) in psychiatric disordered and control subjects. Psychiatry Res. 2000;97:165–72.
Liu XC, Tang MQ, Hu L, et al. Reliability and validity of the Pittsburgh sleep quality index [In Chinese]. Chin J Psychiatry. 1996;29:103–7.
Rostom A, Dubé C, Cranney A, et al. Celiac Disease. Evidence Report/Technology Assessment No. 104. Agency for Healthcare Research and Quality (US). 2004. http://www.ncbi.nlm.nih.gov/books/NBK35156/. Accessed Sept 2004.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58.
Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1959;22:719–48.
Der Simonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trial. 1986;7:177–88.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–101.
Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34.
Yao XD, Shen ZF, Xiang HQ, et al. Investigation and analysis of medical students sleep quality [In Chinese]. J Jiaxing Univ. 2006;18:126–8.
Gao L, Sun HY, Jia F. Comparative analysis on sleep quality between medical and normal university students [In Chinese]. Chin J School Doctor. 2007;21:417–8.
Wei CQ. Comparative analysis on sleep quality between medical and engineering university students [In Chinese]. Chin J Sch Health. 2009;30:1027–8.
Zheng TS, Zheng YY, Mao GY, et al. The investigation of sleep quality and cognitive on college students [In Chinese]. Med Soc. 2010;23:84–6.
Chen YJ. Research on the relationship among anger, presleep through control and sleep quality of college students. [In Chinese] Master thesis, Fujian Normal University, 2011.
Zhang JS. Investigation on sleeping quality of university students and its influential factors. [In Chinese] Master thesis, Wuhan University of Science and Technology, 2012.
Huang L, Zhu K, Sun C, et al. Comparative analysis on sleep quality and its influencing factors between medical and non-medical undergraduate students [In Chinese]. Fudan Univ J Med Sci. 2013;40:303–8.
Luo JY, Huang JM, Wei JS, et al. Investigation on sleep quality and sleepiness of students in guangzhou college [In Chinese]. China Mod Med. 2014;21:168–74.
Zhang LL. The relationship between cyber bullying and sleep disorder among the students of three high vocational colleges in Anhui province. [In Chinese] Master thesis, Anhui Medical University, 2014.
Ding J. Relationship among sleep beliefs and attitude, sleep effort, perfectionism and sleep quality in college students. [In Chinese] Master thesis, Zhengzhou University, 2015.
Zheng YN, Hu W, Wen YY, et al. Quality of sleep and influencing factors among freshmen in Ganzhou [In Chinese]. Chin J Sch Health. 2017;38:57–9.
Shah M, Hasan S, Malik S, et al. Perceived stress, sources and severity of stress among medical undergraduates in a Pakistani medical school. BMC Med Educ. 2010;10:2.
Purim KS, Guimarães AT, Titski AC, et al. Sleep deprivation and drowsiness of medical residents and medical students. Rev Col Bras Cir. 2016;43:438–44.
Preišegolavičiūtė E, Leskauskas D, Adomaitienė V. Associations of quality of sleep with lifestyle factors and profile of studies among Lithuanian students. Medicina (Kaunas). 2010;46:482–9.
Giri P, Baviskar M, Phalke D. Study of sleep habits and sleep problems among medical students of pravara institute of medical sciences loni, Western maharashtra, India. Ann Med Health Sci Res. 2013;3:51–4.
Bruck D, Astbury J. Population study on the predictors of sleeping difficulties in young Australian women. Behav Sleep Med. 2012;10:84–95.
Zhang B, Wing YK. Sex differences in insomnia: a meta-analysis. Sleep. 2006;29:85–93.
Dyrbye LN, Thomas MR, Shanafelt TD. Medical student distress: causes, consequences, and proposed solutions. Mayo Clin Proc. 2005;80:1613–22.
Shad R, Thawani R, Goel A. Burnout and sleep quality: a cross-sectional questionnaire-based study of medical and non-medical students in India. Cureus. 2015;7:e361.
Mazurkiewicz R, Korenstein D, Fallar R, et al. The prevalence and correlations of medical student burnout in the pre-clinical years: a cross-sectional study. Psychol Health Med. 2012;17:188–95.
Waqas A, Khan S, Sharif W, et al. Association of academic stress with sleeping difficulties in medical students of a Pakistani medical school: a cross sectional survey. Peer J. 2015;3:e840.
Ahrberg K, Dresler M, Niedermaier S, et al. The interaction between sleep quality and academic performance. J Psychiatr Res. 2012;46:1618–22.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research received no grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors declare no conflict of interests.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
41105_2017_118_MOESM1_ESM.tif
Fig. S1 Sensitivity analysis of subjective sleep quality between medical students and non-medical students (TIFF 6549 kb)
41105_2017_118_MOESM4_ESM.tif
Fig. S4 Sensitivity analysis of habitual sleep efficiency between medical students and non-medical students (TIFF 6549 kb)
41105_2017_118_MOESM6_ESM.tif
Fig. S6 Sensitivity analysis of use of sleeping medications between medical students and non-medical students (TIFF 6549 kb)
41105_2017_118_MOESM8_ESM.tif
Fig. S8 Sensitivity analysis of the total scores of PSQI between medical students and non-medical students (TIFF 6549 kb)
Rights and permissions
About this article
Cite this article
Yu, D., Ren, Q., Dong, B. et al. The sleep quality of medical students in China: a meta-analysis. Sleep Biol. Rhythms 15, 299–310 (2017). https://doi.org/10.1007/s41105-017-0118-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41105-017-0118-6