Abstract
Pesticides are a major class of pollutants of concern for the health of life and ecosystems. For instance, acetamiprid is a new-generation chloronicotinyl insecticide widely used as an alternative to organophosphates and carbamates to control insect pests. Acetamiprid is designed to target nicotinic acetylcholine receptors in insects, but its extensive use has led to adverse effects in non-targeted organisms including mammals. Traces of acetamiprid have been detected in various food products, water and soil. Moreover, the metabolism of acetamiprid generates toxic metabolites detected in the brain, liver, plasma and urine of rodents. Prolonged environmental or accidental exposure to acetamiprid alters hematological, biochemical and structural profiles, leading to neurological, hepatorenal, immunological, genotoxic and reproductive effects. Here we review acetamiprid metabolism and toxicity studies in mammals. Therapeutic use of plant extracts and antioxidants against acetamiprid-generated oxidative stress are also summarized. Genetic damage, chromosomal aberrations and depletion of antioxidants suggest that oxidative stress is the main mechanism for acetamiprid-induced toxicity.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Acetamiprid, (E)-N′-[(6-Chloro-3-pyridyl)methyl]-N2-Cyano-N′-methylacetamidine, is the new-generation chloronicotinyl insecticide with structural similarity to nicotine (Devan et al. 2015a) (Table 1). Acetamiprid was first synthesized in the year 1984, whereas the first commercial product containing acetamiprid was registered in 2002 for crops and livestocks. Since the last decade, acetamiprid is broadly used in agricultural, domestic and public health activities as a replacement of more hazardous pesticides like organophosphates, carbamates and pyrethroids (Kocaman and Topaktaş 2007; Craddock et al. 2019). In agriculture, acetamiprid has been used globally to control sucking insects, aphids, leafhoppers, moths, beetles, hemipterans, lepidopteron and pests of commercial crops along with fruits, flowers and ornamental plants (Kocaman and Topaktaş 2007; Kong et al. 2017; Bagri and Jain 2019). In domestic and public health activities, acetamiprid is used to control flies, cockroaches, mosquitoes, ticks, and mites and is found to be equally effective at various stages of their growth (Çavaş et al. 2012). It has been used commercially in cherry farming also, due to its great effectiveness against cherry fruit fly larvae (Devan et al. 2015a).
Long-term and unplanned use of organophosphate and organochlorine pesticides in agriculture and domestic field has caused pesticide resistance in several insect pests (Tomizawa and Casida 2005; Mosbah et al. 2018). Acetamiprid has overcome this resistant limitation effectively and is known to act significantly against insect pests (Gupta and Gajbhiye 2007; Guohong et al. 2009; Wallace 2014; Gasmi et al. 2017; Mosbah et al. 2018; Annabi et al. 2019). Presently, acetamiprid-based products are sold throughout the world under various trade names like Pristine, Assail, Mospilan, Epik and Chipko (Elbert et al. 2008; Renaud et al. 2018). Production and use of acetamiprid in India have increased consistently from 42 metric tonnes in 2014–2015 to 114 metric tonnes in 2019–2020 (Statistical database, India 2021).
Acetamiprid is an agonist at nicotinic acetylcholine receptors which make it highly efficient for controlling insect pests. In insects, acetamiprid exposure interrupts nerve transmission, alters membrane potential and ultimately results in neuronal hyper excitation, paralysis and death (Elbert et al. 2008; Tian et al. 2016; Gasmi et al. 2017). Although acetamiprid is highly toxic to insects (Tomizawa and Casida 2005; Çavaş et al. 2014; Chakroun et al. 2016), various studies have shown that acetamiprid has significant affinities for mammalian nicotinic acetylcholine receptors that is responsible for its toxicity to mammalian tissues also (Wallace 2014; Terayama et al. 2016; Shamsi et al. 2021). Some studies have reported inhibition of mRNA expression of α3, α4 and α7 nicotinic acetylcholine receptor subunits in rats cerebellar cells (Kimura-Kuroda et al. 2012), different brain regions (Terayama et al. 2016) and testis of mice (Terayama et al. 2018) following acetamiprid exposure. In mammals, nicotinic acetylcholine receptors are majorly located in the neuromuscular (Albuquerque et al. 2009; Martinez and Akaaboune 2021) and reproductive system (Ge et al. 2005; Kumar and Meizel 2005). The severity of acetamiprid toxicity is mainly governed by duration and dose of exposure. In humans, acetamiprid poisoning has been reported to induce memory dysfunctions, respiratory failure, vomiting, nausea, hypotension, convulsions, muscular weakness and hypothermia (Imamura et al. 2010; Kushwaha et al. 2018; Shamsi et al. 2021).
Traces of acetamiprid has been detected in soil (2 μg/kg) (Bonmatin et al. 2021), water (2.50 ng/L, 0.2–7.7 μg/L) (Zoumenou et al. 2019), food (Craddock et al. 2019) and in crops including mustard (0.01–0.91 μg/g) (Pramanik et al. 2006), gram (0.010–0.394 μg/g) (Gupta et al. 2005), chilly (0.0207–0.1039 μg/g) (Sanyal et al. 2008) and watermelon (0.002–0.085) (Wu et al. 2012). Acetamiprid can be absorbed through dermal, oral and nasal routes or through contaminated food, water and soil (Marın et al. 2004). Various studies regarding acetamiprid exposure have shown that oxidative stress generation might be the general mechanism for its toxicity to various organs in mammalian models. Oxidative stress-mediated apoptosis and DNA damage have been demonstrated in acetamiprid induced toxicity in mammals (Annabi et al. 2019; Kara et al. 2020). Acetamiprid mediated oxidative stress generation inside living tissue damages lipids and proteins through the accumulation of free radicals and is closely associated with hepatotoxicity, neurotoxicity, nephrotoxicity, cytotoxicity, genotoxicity, reproductive and developmental toxicity (Zhang et al. 2011; Devan et al. 2015b; Rasgele et al. 2015). Several studies have shown the toxic effects of acetamiprid alone and in combination with other pesticides also. The continuous and wide usages of acetamiprid in the present decade make it imperative to review the toxic effects of acetamiprid in mammals. Therefore, the present review highlights the toxic effects of acetamiprid, oxidative stress generation and the antioxidant’s role to combat acetamiprid-induced toxicity in mammals.
Absorption and metabolism of acetamiprid
Acetamiprid is readily soluble in water and can easily contaminate the food resources in the environment (Xu et al. 2019; Gaweł et al. 2019). Direct and indirect exposure to acetamiprid is closely associated with its accumulation in various tissues (Marın et al. 2004; Bonmatin et al. 2021). In fact, studies have reported significant levels of acetamiprid and its metabolites in the liver, kidney and other tissues of mice (Ford and Casida 2006). Mice orally exposed to acetamiprid (30 mg/kg b.wt) showed a higher amount of acetamiprid residues in liver tissue than kidney, suggesting organ-specific accumulation of acetamiprid inside the body (Yi-Wang et al. 2012). Other studies also reported higher acetamiprid concentration in liver tissue than testis in rodents (Zhang et al. 2011; Devan et al. 2015b). Even, acetamiprid and its metabolites have been detected in feces of rats exposed to 100 μM of acetamiprid (Kolanczyk et al. 2020). A case study reported acetamiprid and its metabolites in blood, liver, stomach and urine sample of 7-year girl, who died due to intoxication of very high dose of acetamiprid (Yeter and Aydın 2014). The acetamiprid level was detected in the stomach, blood and liver while its metabolites were detected only in the stomach. Earlier, Marın et al. (2004) also observed the highest concentration of acetamiprid in urine samples collected after 13–15 h of exposure that decreased to nil after 28 h in the farmers working in green houses. These farmers encountered acetamiprid exposure either through nasal or dermal routes during the spraying activity in the green houses.
The absorption of acetamiprid in living tissues has not been evaluated in detail. An in vitro study by Brunet et al. (2008) investigated the role of temperature and concentration on acetamiprid absorption in human colon carcinoma cells (CaCo-2-14). At 37 °C, 100% absorption of acetamiprid was detected that reduced to 33% at 4 °C suggesting a significant role of temperature in acetamiprid absorption. In CaCo-2-14 cells, acetamiprid was absorbed through both apical to basal and basal to apical pathways. Interestingly, basal to apical pathway was concentration independent while the apical to basal pathway was concentration-dependent, which suggested the involvement of some membranous transporters in acetamiprid uptake inside the cells. Further, the sodium transporter, ATP-dependent active transporter and membrane proteinaceous transporters were also evaluated for their role in acetamiprid uptake inside CaCo-2-14 cells. The absence of sodium transporter inhibited the transport of acetamiprid confirming its involvement in the uptake of acetamiprid, whereas ATP depletion and trypsin treatment showed an increase in acetamiprid uptake suggesting that acetamiprid uptake by these cells is inhibited through ATP-dependent active transporter and other membranous proteinaceous transporters. Additionally, the treatment of taxol (inhibitor of multidrug resistance pump) and daunorubicin (inhibitor of multidrug resistance protein) to these cells decreased the efflux of acetamiprid. The study confirmed the involvement of these carrier-mediated efflux proteins in acetamiprid transport.
Acetamiprid is known to metabolize readily inside the living tissues through demethylation, deacetylation and hydrolysis of cyano-imine linkage (Table 2). Urine analysis of 50 children (less than 3 years of age) who never had direct exposure of acetamiprid showed the presence of acetamiprid metabolite; N-desmethyl-acetamiprid in total 39 children that suggested environmental contamination as a route of exposure (Ueyama et al. 2020). Kolanczyk et al. (2020) reported that acetamiprid is mainly converted to N-desmethyl-acetamiprid (C9H9ClN4) in microsomes of rats. Ichikawa et al. (2019) also detected N-desmethyl-acetamiprid in 14 out of 57 urine samples collected on 1st and 2nd postnatal day; and in 7 out of 59 urine samples collected on 14th postnatal day from infants born to mothers who had no history of direct acetamiprid exposure. The study suggested that these mothers might have been exposed to acetamiprid through environmental contamination which metabolized into N-desmethyl-acetamiprid leading to its increased level in the blood that might have crossed the placenta and accumulated in the fetus. Further, the study also suggested that N-desmethyl-acetamiprid could accumulate in brain via nicotinic acetylcholine receptors which might affect neurological development. Some other studies also detected acetamiprid metabolites in various tissues and fluids and found N-desmethyl-acetamiprid as common and the most detectable metabolite (Yeter and Aydın 2014). These findings suggested N-desmethyl-acetamiprid as a major metabolite of acetamiprid (Taira et al. 2013; Marfo et al. 2015) that might be associated with toxicity symptoms of acetamiprid exposure.
The metabolite N-desmethyl-acetamiprid has been shown to exert some toxicity symptoms. In relation to this, Marfo et al. (2015) detected the presence of 6 ppb N-desmethyl-acetamiprid in urine samples of patients with symptoms having memory loss, finger tremors, headache, fatigue, palpitation, pain and cough, and 4.4 ppb of N-desmethyl-acetamiprid in patients with headache, fatigue, pain and cough, while 2.2 ppb of N-desmethyl-acetamiprid was detected in non-symptomatic group suggesting the role of N-desmethyl-acetamiprid concentration in symptom prevalence. In addition, a field survey by Kabata et al. (2016) also detected N-desmethyl-acetamiprid in urine samples of many farmers. It was observed that the concentration of N-desmethyl-acetamiprid was higher in the urine samples of the farmers without known history of kidney diseases, while low concentration of N-desmethyl-acetamiprid was detected from the urine samples of the farmers with history of chronic kidney diseases.
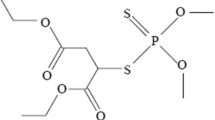
Metabolism of acetamiprid has also been investigated to identify the presence of the metabolites in different organs. Taira et al. (2013) identified 27 metabolites of different neonicotinoids in urine samples of mice, intraperitoneally injected with acetamiprid (10 mg/kg b.wt), imidacloprid (10 mg/kg b.wt) and clothianidin (20 mg/kg b.wt). Out of 27 detected metabolites, 4 were exclusively related to acetamiprid while 4 metabolites were common with imidacloprid and clothianidin. Ford and Casida (2006) intraperitoneally administered mice with 10 and 20 mg/kg b.wt of acetamiprid and reported that acetamiprid was metabolized to ACE-dm (C9H9ClN4), ACE-dm-NCONH2 (C9H11ClN4O), ACE-acet (C9H11ClN2O), ACE-dm-acet (C8H9ClN2O) and ACE-U (C4H7N3) as explained in Table 2. The ACE-dm (N-desmethyl-acetamiprid) and ACE-U metabolites were detected in brain, liver, plasma and urine samples. Further, ACE-dm-acet was prominently observed in brain, liver and urine samples, while ACE-dm-NCONH2 was detected only in urine samples of mice. Some studies have shown the presence of acetamiprid in feces also suggesting its biliary excretion. Ogawa et al. (2018) studied metabolic profiling of plasma samples collected at 0–96 h after intravenous administration of 7.1 and 21.7 mg/kg b.wt acetamiprid in Wistar rats. Four metabolites labeled as M1 (C9H9ClN4), M2 (C8H9ClN2O), M3 (C4H7N3) and M4 (C7H7NO2S) were detected (Table 2). C9H9ClN4 (N-desmethyl-acetamiprid), C8H9ClN2O (ACE-dm-acet), C4H7N3 (ACE-U) and C7H7NO2S were acetamiprid metabolites detected in plasma. N-desmethyl-acetamiprid was a majorly detected metabolite and its concentration along with ACE-dm-acet and ACE-U increased to the maximum level at 4–6 h and was eliminated at 48 h; while ACE-dm-acet increased to the maximum level at 12–24 h and was eliminated at 72 h. Based on these evidences, the general pathway of acetamiprid metabolism is hypothesized in Fig. 1.
Metabolic fate of acetamiprid inside mammals, modified after Ford and Casida 2006; Taira et al. 2013; Yamamuro et al. 2014; Ogawa et al. 2018. Initial steps of metabolism of acetamiprid involves N-demethylation to form (E)-N1-[(6-chloro-3-pyridyl)methyl]-N2-cyano-acetamidine and also involves cyanohydrolysis to form N-[(6-chloropyridin-3-yl)methyl] acetamide. Further, breakdown of these metabolites involves cyanoimine cleavage, N-deacetylation leading to formation of other metabolites. Some products of acetamiprid metabolism, detected inside body are supposed to be generated through biomodulation involving addition of some molecules
Acetamiprid-induced toxicity
General toxicity
Wide and continuous use of acetamiprid has presented it as an environmental toxicant and its exposure imposes organ system toxicity adversely affecting immune physiology, ion balance and behavior. Easy solubility and rapid biological interaction of acetamiprid make the living tissues more susceptible to its exposure. The residue of acetamiprid has been reported in urine (Taira et al. 2013; Ichikawa et al. 2019), digestive tract (Yeter and Aydın 2014) and brain (Ford and Casida 2006) and acetamiprid has been shown to accumulate in liver and testis tissue of mice (Zhang et al. 2011). The LD50 of oral exposure is observed to be 200–220 mg/kg b.wt in rats (Kong et al. 2017; Gasmi et al. 2017; Shamsi et al. 2021), whereas LD50 for exposure through drinking water is observed to be 1000 mg/kg b.wt in rats (Hataba et al. 2014; Shahin 2018). However, the LD50 in rats varies from 140 to 417 mg/kg b.wt depending upon the gender and the strains of rats (FAO Panel of Experts on Pesticide Residues in Food and the Environment. and WHO Core Assessment Group on Pesticide Residues 2012; Arican et al. 2019). Various animal studies have shown the dose-dependent acetamiprid toxicity and suggested the generation of oxidative stress in various tissues.
Sub-chronic oral exposure of acetamiprid was observed to induce oxidative stress mediated structural alterations in liver and kidney (Karaca et al. 2019), hematological and biochemical alterations in hepatic tissue of rats (Chakroun et al. 2016) in dose-dependent manner. Acetamiprid is also known to cause impaired locomotors activity, tremors and nervous system-associated disorders in mice. The down-regulation in efferent nerve transmission and abnormal generation of afferent transmission at neuromuscular synapse might be associated with its neurotoxic symptoms (Dukhnytskyi et al. 2020). Acetamiprid exposure is shown to affect the synaptic strength of neurons, desensitize ionic receptors (Mondal et al. 2014; Mandal et al. 2015) and neural degeneration (Shamsi et al. 2021) in the hippocampus of rats. Acetamiprid exposure is known to alter socio-sexual and anxiety behavior (Sano et al. 2016), memory loss, impaired learning ability and also decline the activity latency time in rats (Mondal et al. 2014; Mandal et al. 2015). Moreover, prenatal acetamiprid exposure has also shown neurodevelopment toxicity (Kimura-Kuroda et al. 2012, 2016), skeletal abnormalities (Abouzeid 2018) and altered expressions of proliferating and metabolizing genes (Terayama et al. 2018; Nakayama et al. 2019). In addition, neuro-developmental toxicity induced by prenatal exposure of acetamiprid was also reported during neocortex organogenesis in mice (Kagawa and Nagao 2018). The altered gene expressions might be the major reason for abnormal organogenesis and developmental toxicity.
The acetamiprid exposure has also been reported to cause ion imbalance inside the cells. In fact, acetamiprid administration (40 mg/kg b.wt, 21 days) increased cerebellum Ca2+ levels suggesting inhibition of Na+/K+, Ca2+ and Mg2+ ATPase activity in rat’s brain (Dhouib et al. 2017). Further, culture of cerebellum cells of neonatal rats, treated with nicotine, acetamiprid and imidacloprid (1, 10 and 100 μM of each), attenuated excitatory Ca2+ influx in concentration-dependent manner (Kimura-Kuroda et al. 2012). However, Zhang et al. (2012) depicted that acetamiprid exposure (30 mg/kg b.wt) was associated with decreased Ca2+ concentration in plasma and kidney tissue of rats resulting in hypocalcemia that might have caused renal dysfunctioning. Further, the change in ionic physiology along with oxidative stress might lead to cytoskeleton modulations that causes structural changes and antioxidants depletion.
Acetamiprid exposure has been shown to cause a reduction in antioxidant enzyme activities, induce inflammation along with necrosis and apoptosis in the liver and kidney of rats. Similarly, acetamiprid also exerts toxic effects on reproductive physiology. Decreased testosterone levels and damage to testicular tissue were detected in mice (Chawseen 2011) and rats (Kong et al. 2017). Ibrahim et al. (2020) depicted oxidative stress mediated structural and physical dysfunctioning of reproductive organs in rats following chronic acetamiprid exposure. Moreover, acetamiprid exposure is reported to cause cytotoxicity and molecular modulations in different cells. Marzouki et al. (2017) investigated the immune toxicity of acetamiprid and spleen profile of mice against virulence factor Mycobacterium tuberculosis and reported significant immuno-suppression. They observed a significant decrease in spleen weight along with fibrous tissue proliferation and white pulp disintegration and suggested that histopathological changes might be related to the observed immuno-suppression. In addition, chronic exposure to acetamiprid also causes molecular alterations and disturbs mitochondrial activities. Gasmi et al. (2017) have shown a close association of reactive oxygen species generation and increased membranous permeability that causes impairment in enzyme activity of brain mitochondria. Disturbance in cellular protein expression through oxidative stress may impose the apoptotic effects of acetamiprid both in vitro and in vivo (El-Bialy et al. 2020; Gomez et al. 2020). These findings suggested that along with oxidative damage, acetamiprid exposure also causes cytotoxic and apoptotic effects in rodents, which can be related to humans also.
Recently, various case studies have reported toxicity and physical symptoms of acetamiprid exposure in humans. In humans, physical symptoms consist of nausea, vomiting, weakness, convulsions, tachycardia, increased heart rate, increased urine flow, hypotension, hypoxia and thirst (Imamura et al. 2010) followed by lactic acidosis (Pirasath et al. 2021) suggesting that physical symptoms of acute acetamiprid poisoning in mammals coincide with symptoms of organophosphate poisoning. Acute ingestion of acetamiprid pesticides in humans is reported to cause death also. A case study has reported causality of 7-year-old girl who was intentionally subjected to the unknown acute high dose of acetamiprid by her sibling (Yeter and Aydın 2014). Additionally, Kushwaha et al. (2018) also reported the symptoms similar to organophosphate poisoning in 2.5-year-old buffalo who swallowed 100 g of acetamiprid. Non-lethal exposure of acetamiprid to living animals led to the rise of its metabolites in the body (Ford and Casida 2006; Ogawa et al. 2018) and the concentration of acetamiprid and its metabolites has shown a relationship with toxicity of various vital organs. These evidences confirm that acetamiprid is highly toxic to the mammalian system also and may generate system-specific detrimental effects.
Oxidative stress generation
Oxidative stress is a physiological condition that arises from the imbalance between reactive oxygen species generation and antioxidant depletion inside the cells (Abdollahi et al. 2004; Poljsak et al. 2013). Oxidative stress depletes the biological pool of oxygen inside tissues and results in over production of oxygen free radicals that affect cellular membranes and the integrity of biological macromolecules (Abdollahi et al. 2004). Membranous lipids, proteins and DNA molecules are highly prone to oxidative damage owing to their high oxygen demand and affinity toward free radicals. Living organisms have a natural mechanism to mitigate oxidative stress through enzymatic and non-enzymatic antioxidants (Pisoschi and Pop 2015). It is well known that superoxide dismutase and catalase constitute the first line of defense against pesticides generated superoxide and peroxides radicals (Poljsak et al. 2013). In addition, several non-enzymatic antioxidants constitute the second line of defense against oxidative stress. Glutathione is the most potent non-enzymatic antioxidant related to oxidative stress mitigation and detoxification of xenobiotics. These non-enzymatic antioxidants not only utilize these free radicals but also assist repair to damaged tissues. Progressive in vitro and in vivo studies have shown that acetamiprid exposure results in significant reactive oxygen species generation that imbalance both enzymatic and non-enzymatic antioxidants.
In vitro studies
Acetamiprid has been shown to cause degenerative changes in various in vitro studies. Rats pheochromocytoma adrenal medulla cells (PC12) treated with acetamiprid (100–700 μM) resulted in a significant increase in malondialdehyde levels, reactive oxygen species generation and loss of mitochondrial membrane potential which altered oxygen uptake and metabolism inside PC12 cells (Annabi et al. 2019). Kara et al. (2020) observed that the pancreatic cell line (AR42J) treated with acetamiprid (1–6 mM) caused non-significant reactive oxygen species production but significantly reduced glutathione levels at higher concentrations. It was suggested that the inner mitochondrial membrane damage observed in these cells might be associated with the acetamiprid mediated glutathione depletion. Isolated trophoblast cells (HTR-8/SVneo) treated with commercial acetamiprid formulation (10 and 100 μM) were shown to increase reactive oxygen species production and superoxide generation followed by decreased glutathione S-transferase, catalase and superoxide dismutase activities in concentration and time-dependent manner (Gomez et al. 2020). Umbilical cord blood erythrocytes exposed to acetamiprid (4, 40 and 400 nM) for 3 h showed a significant decrease in catalase and superoxide dismutase activities; increase in reactive oxygen species level and 4-hydroxy-2-nonenal content at 40 and 400 nM concentration depicting oxidative stress-mediated increased lipid peroxidation in erythrocytes (Quintana et al. 2018). Thus, at cellular level acetamiprid exposure might impose oxidative stress mediated alteration of antioxidant status in dose-dependent manner.
In vivo studies
Exposure of acetamiprid to living tissues leads to the production of free radicals inside tissues. The interaction of free radicals with cells causes a cascade of reactions leading to tissue damage through oxidation of structural molecules and depletion of antioxidants capacity. These free radicals are associated with numerous pathological processes and oxidative stress generation. Various in vivo studies have confirmed the generation of oxidative stress following acetamiprid exposure. It has been shown that chronic exposure to acetamiprid significantly increased malondialdehyde levels, injury biomarkers and decreased superoxide dismutase and catalase activities along with histopathological degeneration in dose-dependent manner in liver and kidney tissues of rats suggesting generation of oxidative stress as a root cause of toxicity (Hataba et al. 2014; Chakroun et al. 2016; El-Bialy et al. 2020). Karaca et al. (2019) also showed dose-dependent increase in malondialdehyde levels, decreased glutathione content, increased level of liver enzymes and histopathological degeneration in liver and kidney tissues of rats orally administered with acetamiprid. Further, the histopathological examination revealed acetamiprid as more toxic to the liver compared to kidney tissues in rats.
Antioxidant depletion and oxidants generation is considered as a dual mechanism of acetamiprid action and may lead to apoptosis progression. Besides this, lipid peroxidation is reported as a major oxidative damage marker after acetamiprid exposure. Lipids are basic building blocks of cellular structures; hence oxidation of lipids is closely associated with histopathological alterations and altered antioxidants capacity. Various studies have shown an increase in lipid peroxidation, depletion of glutathione and also a decrease in various antioxidant enzymes along with structural changes in the liver and kidney (Devan et al. 2015b; Doltade et al. 2019), and plasma and testis of rats (Arıcan et al. 2020). Similarly, acetamiprid exposure also significantly increased malondialdehyde levels, total oxidant status and pro-inflammatory cytokines; decreased total antioxidant status, glutathione, superoxide dismutase and catalase levels leading to oxidative stress generation in kidney tissue of mice (Erdemli et al. 2020). Acetamiprid also acts as a cellular degenerative as evidenced by hormonal imbalance, apoptosis and histopathological alternations in the testis of rats (Arıcan et al. 2020). Studies have shown that oxidative stress is closely associated to a decrease in body and organs weight; an increase in lipid peroxidation, and physiological alterations in sperm of rats (Mosbah et al. 2018; Kenfack et al. 2018) and guinea pigs (Guiekep et al. 2019) following acetamiprid exposure.
Alterations in cellular antioxidants defense physiology due to acetamiprid exposure may initiate severe oxidative damage inside the tissue. A study by Khovarnagh and Seyedalipour (2021) observed that acetamiprid administration increased lipid peroxidation; decreased glutathione level and total antioxidants capacity, protein and albumin level and also induced structural changes in brain and liver tissues of rats. Further, a significant increase in alanine aminotransferase, aspartate aminotransferase, alkaline phosphatase and lactate dehydrogenase, observed in the study suggested oxidative stress-mediated hepatic tissue damage and alteration in antioxidants capacity. Earlier, acetamiprid exposure was reported to increase plasma aspartate aminotransferase, alanine aminotransferase and alkaline phosphatase activities; urea and creatinine level (Hataba et al. 2014) followed by ion imbalance, increase in membrane permeability and pro-inflammatory cytokines production in rats (Mondal et al. 2015). A recent study has also reported significant increase in malondialdehyde levels and accumulation of phenylalanine and branched chain amino acids and decrease in antioxidants activity in liver tissue of mice exposed to acetamiprid suggesting that lipid accumulation due to disturbance in amino acid metabolism might be responsible for oxidative stress generation (Yan et al. 2020). Mice exposed to 20 mg/kg b.wt of acetamiprid resulted in increased lipid peroxidation levels, decreased superoxide dismutase, catalase and glutathione peroxidase activities followed by increase in WBC count, bilirubin and lactate dehydrogenase level suggesting anemia and oxidative damage in erythrocytes (Chelly et al. 2019).
The brain is easily targeted by free radicals. High oxygen demand and lipid content make it more susceptible to oxidative damage. Various studies have reported oxidative stress-mediated damage to the brain following acetamiprid exposure. Sub-chronic acetamiprid exposure (40 mg/kg b.wt) showed an increase in malondialdehyde levels, superoxide dismutase and catalase activities and disturbed cerebellum acetyl cholinesterase and butyryl cholinesterase activity and thiol content in the brain of rats (Dhouib et al. 2017). However, Gasmi et al. (2016) observed depletion of glutathione and total lipids, decrease in glutathione peroxidase and catalase activities followed by elevation of cytosolic proteins and carbohydrate levels in the brain tissue of rats chronically exposed to acetamiprid suggesting acetamiprid induced β-oxidation and free radicals generation. Later, Gasmi et al. (2017) also observed decreased respiratory potential and increased membranous permeability followed by an imbalance of redox status in brain mitochondria of rats following acetamiprid exposure for 90 days.
Along with free radical generation, acetamiprid exposure is reported to produce nitric oxide by perturbating the electron transport chain, which ultimately increases reactive nitrogen species. Chronic acetamiprid exposure (10 and 30 mg/kg b.wt) has been shown to increase nitric oxide and malondialdehyde levels; a decrease of catalase, glutathione peroxidase and superoxide dismutase activities, ATP and cyclic adenosine monophosphate production resulting in mitochondrial damage in Leydig cells of rats (Zhang et al. 2011; Kong et al. 2017). Other studies have also demonstrated that rats administered with acetamiprid (100 mg/kg b.wt, 30 days) resulted in an increase in malondialdehyde and nitric oxide level, proinflammatory cytokine production along with the concomitant decrease in antioxidants activity in the liver (Shahin 2018) and kidney tissues (Alhusaini et al. 2019). The various in vivo toxicity studies related to acetamiprid exposure are summarized in Table 3.
The results of in vivo and in vitro studies suggest free radicals mediated cytotoxic, genotoxic, neurotoxic and hepatotoxic effects of acetamiprid exposure. It may be speculated that oxidative stress generation might be responsible for acetamiprid mediated mammalian toxicity.
Genetic damage and apoptosis
Acetamiprid is easily incorporated inside the tissues. Apart from oxidative damage, acetamiprid is reported to interfere as a mutagen and may cause changes in gene expression; that collectively might induce cellular apoptosis. Apoptosis is a cellular process of programmed cell death that is regulated by pro-apoptotic and anti-apoptotic protein. Oxidative stress, DNA damage and altered gene expression are prime inducers for intrinsic apoptosis.
In vitro studies
The in vitro genotoxicity, cytotoxicity and subsequent DNA damage along with molecular damage following acetamiprid exposure has been shown by various studies (Kocaman and Topaktaş 2007; Çavaş et al. 2012; Muranli et al. 2015; Senyildiz et al. 2018). Trophoblast cells treated with acetamiprid (1, 10 and 100 μM) showed up-regulated Bax (a pro-apoptotic protein) expression and down-regulated expression of Bcl-2 (an anti-apoptotic protein) along with decreased cellular viability with the increment in duration and concentration of exposure (Gomez et al. 2020). Apoptosis is linked to numerous damages to the genetic material and cellular harmony of the tissue. In relation to this, the study by Annabi et al. (2019) observed a significant decrease in cell viability, increase in DNA damage and caspases-dependent apoptosis in PC12 cells treated with 100–700 μM of acetamiprid. Additional studies also have shown acetamiprid exposure mediated decrease in cell survival and increased DNA damage in the AR42J cells (Kara et al. 2020) and human lung fibroblast cells (Çavaş et al. 2014). At cellular level acetamiprid exposure mediated apoptosis is closely associated to various degenerative process affecting cell viability and cellular harmony.
The effects of acetamiprid on genetic susceptibility inside cell models have been evaluated in some studies. A study by Senyildiz et al. (2018) revealed increased DNA damage following acetamiprid exposure (0.125, 0.25, 0.5, 1, 2 and 4 mM) for 24 and 48 h in human neuroblastoma cells (SHSY-5Y) and human hepatocellular carcinoma cells (HepG2) in dose-dependent manner. Further, the results indicated that cytotoxicity and DNA damage was more evident in human neuroblastoma cells than human hepatocellular carcinoma cells exposed to acetamiprid for the same duration. Furthermore, comet assay (used for single and double-strand DNA damage) and γH2AX foci formation assay (used for double-strand DNA break) showed decreased cell survival, increased micronuclei frequency and single and double-stranded DNA breakage in human colon carcinoma cells treated with acetamiprid. It was also observed that minimal concentration of 75 μM was the threshold to induce cytotoxic effects while 25 and 50 μM concentration of acetamiprid were detected as non-cytotoxic (Çavaş et al. 2012). It might be possible that acetamiprid alters the activity of DNA segments and results in epigenetic alterations in genome.
The studies have also suggested that acetamiprid exposure along with other pesticides has more pronounced synergistic toxic effects. Blood lymphocytes treated with a different mixture of acetamiprid and propineb (0.625 + 12.5, 1.25 + 25, 2.5 + 50 μg/mL) for 24 and 48 h showed an increase in micronuclei frequency, while the decrease in nuclear division index was shown only at 1.25 μg of acetamiprid exposure for 48 h. The study revealed that acetamiprid alone treatment at low concentration could not induce any cytotoxic or genotoxic effects in human peripheral blood lymphocytes but induced genotoxic effects at combined exposure suggesting synergetic effects of acetamiprid and propineb (Muranli et al. 2015). Similar to this, exposure to acetamiprid (25, 30, 35 and 40 μg/mL) for 24 and 48 h and acetamiprid along with cypermethrin (12.5 + 2.5, 15 + 5 and 17.5 + 7.5 μg/mL) induced chromosomal aberrations, sister chromatids exchange, micronuclei formation and decreased mitotic index, nuclear division index and proliferation index with an increase in the concentration and exposure time in human peripheral blood lymphocytes (Kocaman and Topaktaş 2007, 2010). Accumulating evidences from these studies has confirmed that combined exposure of acetamiprid with other pesticides shows more pronounced degenerative effects at cellular levels.
In vivo studies
Acetamiprid is known to have extensive cytotoxic and genotoxic effects, and various studies have confirmed acetamiprid exposure mediated DNA damage and cellular apoptosis in mammalian tissues. Acetamiprid exposure might affect various tissues at different scales within organs depending upon the biochemistry and physiology of the tissues. El-Bialy et al. (2020) reported that acetamiprid and lambda-cyhalothrin mixture (2.14 mg/kg b.wt) induced cellular injuries and apoptosis in hepatic and renal tissues of rats suggesting that oxidative stress generation might be the driving force for apoptosis and reduced cell viability following exposure to these insecticides.
Sub-chronic acetamiprid exposure was also shown to induce apoptosis in kidney tissue of mice (Erdemli et al. 2020) and necrosis and membrane disruption in brain tissues of rats (Dhouib et al. 2017). Bagri and Jain (2019) observed that acetamiprid exposure caused chromosomal aberrations and DNA damage in erythrocytes of mice suggesting the cytotoxic and genotoxic potential of acetamiprid. Acetamiprid is also considered to be carcinogenic that might cause imprinting disorders. Studies have shown the mutagenic potential of acetamiprid toxicity. In one such study, acetamiprid exposure was shown to decrease 5-methyl cytosine levels in liver tissue of rats in a dose-dependent manner. However, in the brain tissue of these rats, DNA damage was observed only with high dose exposure indicating organ-specific toxicity of acetamiprid (Arican et al. 2019). In addition, the gene expression of DNA methyltransferases was also decreased both in liver and brain tissues. These studies suggest that acetamiprid might induce genomic instability; increases carcinogenic risk and can lead to neurodegeneration. Various in vitro and in vivo studies showing genotoxicity and cytotoxicity of acetamiprid exposure are presented in Table 4.
Developmental toxicity
Developmental toxicity consists of birth defects and organ developmental disorders following either prenatal or postnatal exposure. Developmental toxicity is evaluated by accessing organ growth parameters and various genes responsible for the normal remodeling of tissues. It is closely associated with time of exposure during prenatal and postnatal. In prenatal exposure, generally, organogenesis and genes are affected the most, which may generate severe birth abnormalities. Postnatal exposure is generally associated with growth deformities and abnormal physiology. The widespread use of acetamiprid from the last few decades has shown that it might affect the early developmental stage. Several in vitro and in vivo studies have shown that acetamiprid severely affects fetal development and may lead to long-lasting health effects.
Acetamiprid has been reported to induce abnormalities in pregnant mice and is found to be teratogenic. Oral administration of acetamiprid (5 mg/kg b.wt) in pregnant mice was observed to trigger abnormal neuronal distribution, microglial activation, decreased thickness and growth of cortical plate and reduced neurogenesis; indicating that acetamiprid might cross the blood–brain barrier and induces morphological alterations in radial fibers of developing neocortex (Kagawa and Nagao 2018). Further, exposure to nicotine, acetamiprid and imidacloprid (1, 10 and 100 μM of each) down-regulated Ca2+ influx, induced alternations in transcriptome and caused mild disturbances in Purkinje cells dendrites arborization in concentration-dependent manner and thus led to developmental disorders in rat’s brain (Kimura-Kuroda et al. 2012, 2016). Acetamiprid treatment (31.4 mg/kg b.wt, 9 days) during the gestation period was reported to cause a reduction in placental and fetus weight in pregnant rats. It was also shown that acetamiprid treatment-induced dwarfism, eye abnormalities, hemorrhage, underdeveloped lung and heart hypertrophy along with structural anomalies of a skeletal system like improper ossification, short ribs and absences of phalanges, sacral and caudal vertebrae (Abouzeid 2018). The results suggested that acetamiprid is highly toxic during organogenesis as it disturbs placental redox status, hormonal metabolism, transport across the placenta and mediates early embryonic death or delays ossification.
Acetamiprid exposure also affects the embryonic cell proliferation and zygote formation. The studies indicate that acetamiprid treatment (0.1, 1 and 100 μM) decreases blastocysts cell count, cell proliferation and increases the frequency of cell death in 2-celled embryo development in hybrid mice produced from crossing between C57BL/6 and 6DBA/2 strains; thus affecting embryonic development in mice (Babelova et al. 2017). The results suggested that the presence of acetamiprid and its commercial products in microenvironment of zygote prior to implantation could decrease quality and development of embryo. Earlier, Gu et al. (2013) also studied toxic effects of acetamiprid (500 μM or 5 mM) upon mouse sperm functions and developmental progressions of 2-cell embryo in in vitro culture and naturally fertilized zygotes. The results indicated that acetamiprid possessed lesser adverse effects on spermatozoa functions. In naturally fertilized zygotes acetamiprid exposure significantly decreased blastocyst formation, whereas no detectable decrease in blastocyst formation was observed in developmental progression of in vitro culture of 2-celled embryo. Further, no effect on development ability was observed in both cases. The contrasting results of these studies might be due to different development ability of hybrid strains of mice used for study.
Oral treatment of acetamiprid (5 mg/kg b.wt), from postnatal day 12–26th in mice neonates significantly decreased neural stem cell proliferation gene (C1dU), neuronal cell count and increased the microglial production suggesting impaired neurogenesis in neonates hippocampal region (Nakayama et al. 2019). In another study, PC12 cells firstly treated with nerve growth factors (50 ng/mL) for 5 days and then exposed to acetamiprid (10 μM) on the 6th day showed mild affect on neurite outgrowth but significantly altered gene expression through regulation of Camk2α and gap-43 gene transcription. The findings revealed that acetamiprid induces developmental neurotoxicity at a higher concentrations by an alternation of gap-43 genes (Christen et al. 2017). Up regulation of gap-43 gene is suggested as an adaptive response to maintain brain growth. The findings indicated that acetamiprid exposure is closely associated with neurite outgrowth inhibition, axonal remodeling and may cause neuro degeneration in the developing brain.
Acetamiprid also exerts toxic effects on reproductive physiology in adults. Mice exposed to commercial formulations of acetamiprid and glyphosate showed a significant decrease in serum testosterone levels both at individual and combined exposure. Histological analysis also showed a significant differences in diameter and thickness of seminiferous tubules, lumen dilation and seminiferous tubules degeneration in a dose-dependent manner compared to the controls indicating the toxic effects of acetamiprid on reproductive functions (Chawseen 2011). Additional studies have also supported the fact that acetamiprid exposure alters the structure and physiology of reproductive organs of rats (Ibrahim et al. 2020) and guinea pigs (Guiekep et al. 2019) and also reduces sperm count and causes stillbirths in humans (Neghab et al. 2014).
Progressive evidences have also reported the modulation of genes related to reproductive and neuromuscular functions following acetamiprid exposure. The acetamiprid mediated reactive oxygen species generation is associated with mitochondrial damage and cyclic adenosine monophosphate abnormality. Cyclic adenosine monophosphate controls steroidogenesis and regulates testosterone biosynthesis through the actions of steroidogenic enzyme encoding genes. In relation to this, the study of Kong et al. (2017) has documented acetamiprid mediated significant down regulation of Star, Cyp11a1, Hsd3b in male rats. Star, Cyp11al and Hsd3b are cyclic adenosine monophosphate dependent essential proteins associated with the conversion of cholesterol to testosterone in Leydig cells. In addition, perpetrate action of acetamiprid on gene expression levels of Star, Cyp11a1, Cyp17a, Lhr, Hsd17b1 (testosterone metabolizing genes) and Top2a, Ki67 (proliferating genes) has also been observed in dose-dependent manner in the testis of mice born to acetamiprid treated females (Terayama et al. 2018). In rats, higher acetamiprid concentration was observed in testis than blood (Kong et al. 2017); whereas in mice, acetamiprid concentration was observed to be higher in blood than testis (Terayama et al. 2018) indicating higher accumulation of acetamiprid in testis of rats compared to mice. Further, the study also suggested that mature rodents may be more sensitive to acetamiprid exposure compared to immature rodents. These findings suggested the detrimental effects of acetamiprid induced reactive oxygen species generation and mitochondrial damage in Leydig cells on steroidal biosynthesis and organogenesis. Thus, acetamiprid exposure causes significant alterations in organogenesis, gene regulations, developmental and reproductive physiology in mammals. Alterations in Ca2+ and other cellular signaling along with gene and hormonal abnormalities were common mechanism for developmental toxicity.
Therapeutics for acetamiprid-induced toxicity
Progressive studies have shown that acetamiprid exposure mediated toxicity results in oxidative stress generation, diminishes antioxidants levels and promotes DNA damage and apoptosis. To counteract these damages, antioxidant supplement is supposed to overcome diminished antioxidant status that ultimately prevents oxidative stress. Exogenous antioxidants, after administration; act like endogenous ones and neutralize oxidative stress generated free radicals effects. Certain antioxidants are reported to possess great anti-inflammatory, anti-cancerous, anti-aging and anti-neoplastic activities and thus prevent free radicals mediated oxidative damage of macromolecules. Supplementation of appropriate antioxidants in proper concentration has proven highly efficient to overcome pesticides-induced oxidative stress by counteracting deleterious effects of free radicals (Pisoschi and Pop 2015; Neha et al. 2019).
One such antioxidant, vitamin E is suggested to maintain structural integrity, biomembrane permeability and macromolecular physiology inside the cells. A study has shown the efficacy of vitamin E (20 mg/kg b.wt) against acetamiprid exposure-induced reproductive toxicity. The findings suggested that vitamin E mediated reduced p38 levels could have prevented malondialdehyde and nitric oxide formations, and thus oxidative stress generation in mice (Zhang et al. 2011). The p38 is mitogen-activated protein kinase that enhances oxidative stress through phosphorylation and p38 deficient cells are shown resistant to reactive oxygen species induced apoptosis. Simultaneous treatment of acetamiprid and vitamin E for 35 days significantly inhibited acetamiprid mediated membranous damage in mitochondria of Leydig cells and restored testosterone levels well as semen quality in rats (Kong et al. 2017).
Similarly, the study of Zhang et al. (2012) showed that 20 mg/kg b.wt vitamin E was effective to reduce histolopathogical alterations like atrophy, capsular widening, inflammation and fragmentation along with increased Ca2+ and decreased phosphorus ion concentration in kidney tissue of acetamiprid exposed mice. Vitamin E treatment also maintained hematological and biochemical parameters as evidenced by decreased levels of urea and creatinine and increased uric acid levels thus reported to attenuate chronic degenerative effects of acetamiprid exposure in kidney tissue of mice. Yi-Wang et al. (2012) also showed the protective effects of vitamin E against acetamiprid toxicity. They reported a reduction in acetamiprid induced neurological symptoms, decreased alanine aminotransferase, aspartate aminotransferase and alkaline phosphatase activities and increased total protein and albumin on vitamin E supplementation. The decrease in tissue injury markers suggested the ameliorative potential of vitamin E against free radicals generation.
Vitamin E might be able to reduce acetamiprid induced toxicity either by mediating acetamiprid excretion from the body or by quenching reactive metabolites of acetamiprid. In relation to this, liquid chromatography—mass spectrometry analysis revealed that vitamin E effectively decreased acetamiprid residues in liver and kidney tissues of mice (Yi-Wang et al. 2012). Oral treatment of melatonin (20 mg/kg b.wt) and vitamin E (100 mg/kg b.wt) in acetamiprid treated mice reduced lipid peroxidation levels, total oxidant status, pro-inflammatory cytokine production, caspases-3 expression and maintained antioxidants level in plasma and kidney tissues (Erdemli et al. 2020).
Nowadays, herbal plants are gaining attention because of their safe and potential ameliorative effects against pesticide-induced oxidative damage. Curcumin is a natural poly phenolic compound mainly obtained from the rhizome of the turmeric plant. It has been used as a potent ameliorative agent because of its antioxidative, anti-inflammatory, anti-microbial, anti-cancerous activities and its ability to cross the blood–brain barrier. It is also known to have protective effects against acetamiprid induced toxicity. The antioxidant activities of curcumin might be due to its structural motif i.e.: phenolic hydroxyl group and β-diketone structure that scavenges free radicals (Dinkova-Kostova and Talalay 1999). Oral administration of curcumin (100 mg/kg b.wt) significantly inhibited lipid peroxidation and oxidation of glutathione and also ameliorated the superoxide dismutase, catalase and glutathione reductase activities in liver and brain tissues along with inhibition of acetamiprid induced structural alterations in liver, brain and kidney tissues of rats. However, it was observed that curcumin treatment was more effective against low-dose exposure than high dosage exposure (Doltade et al. 2019).
Additional findings have also suggested the neuroprotective role of curcumin by mitigating oxidative stress and maintaining the enzymatic and ion channel activities. Dhouib et al. (2017) reported that treatment of curcumin (100 mg/kg b.wt) significantly improved neurobehavioral performance, acetyl cholinesterase activity and decreased malondialdehyde levels, and maintained antioxidant enzymes activities and Ca2+ levels in the cerebellum of rats exposed to acetamiprid for 21 days. Further, curcumin supplementation also increased cell viability, thiol content and protected against histopathological alternations; however, it could not prevent apoptosis in rats cerebellum (Dhouib et al. 2017). Another study by Marzouki et al. (2017) also observed that oral administration of curcumin (100 mg/kg b.wt) stimulates humoral and cellular immune response through partially restoring IgG1, IgG2a and anti-rCFP32 antibodies, increased splenocytes proliferation and also prevented histological damage indicating that curcumin might induce T-cell activity and thus restore antibody production. These studies suggested that curcumin have immuno-proliferative properties and maintains immune mechanism in acetamiprid exposure induced toxicity.
Nigella sativa is an aromatic plant, native to western Asia, northern Africa and Eastern Europe. Its seeds and oil are used to treat various diseases particularly associated with the respiratory tract. Nigella sativa oil (0.5 ml/kg/day, orally for 45 days) has been reported to reverse acetamiprid exposure (27 mg/kg b.wt, 45 days) mediated reproductive toxicity by reducing lipid peroxidation levels and also improved reproductive organs weight, testosterone level, sperm count and sperm motility (Mosbah et al. 2018). Various studies have also investigated the ameliorative potentials of amino-acid (L-cysteine) derived compounds and suggested reactive oxygen species scavenging as the main mechanism of action for these compounds (Hong et al. 2003; Harvey et al. 2008; Lasram et al. 2014; Bhardwaj and Saraf 2017). In relation to this, a study has revealed that N-acetyl cysteine (160 mg/kg b.wt) and S-methyl-L-cysteine (100 mg/kg b.wt) co-treatment significantly abolished oxidative stress biomarkers, elevated antioxidant levels and maintained histological architecture in liver and brain tissues of rats (Khovarnagh and Seyedalipour 2021). N-acetyl cysteine is a thiol compound obtained from garlic, onion, asparagus, cauliflowers and broccoli. A recent in vitro study has claimed that N-acetyl cysteine (2 mM) is effective to increase cell viability and stimulates catalase, superoxide dismutase and glutathione S-transferase activities; and decreases reactive oxygen species production, protein oxidation and lipid peroxidation along with DNA damage in human first-trimester trophoblast cell line (HTR-8-Svneo) exposed to acetamiprid (0.1–100 μM) indicating its ameliorative potential against oxidative stress, apoptosis, cell death and bio molecular damage (Gomez et al. 2020).
Quercetin is a plant flavonoid obtained majorly from fruits and vegetables including, nuts, berries, apples, soybeans and broccoli. Quercetin, a natural antioxidant has been shown to ameliorate chronic acetamiprid exposure (3.14 mg/kg b.wt, 90 days) induced neurotoxicity by inhibiting lipid peroxidation, oxidation of antioxidants and maintaining levels of brain cytosolic proteins, lipids and carbohydrates in albino rats (Gasmi et al. 2016). Alhusaini et al. (2019) also showed ameliorative potential of quercetin (100 mg/kg b.wt) and N-glutathione (300 mg/kg b.wt) against acetamiprid exposure (100 mg/kg b.wt, 30 days) in kidney tissues of rats. Another study reported that quercetin and N-glutathione co-administration significantly reduced creatinine, urea, uric acid, nitric oxide and malondialdehyde levels, prevented glutathione oxidation and decreased TNF-α, ICAM-1, NF-KB protein expression followed by controlled membrane alternation, cellular outflow, immune response and glomerular filtration rate. The use of fullerenol nanoparticles has also been shown to protect against acetamiprid induced cytotoxicity and genotoxicity in lung fibroblast cell lines by decreasing DNA damage and increased cell survival (Çavaş et al. 2014).
Many natural extracts of plants are reported to have antioxidant potential against the toxicity of many compounds. The ameliorative potentials of these natural extracts have been evaluated against acetamiprid induced toxicity also. Ginseng is a plant extract containing phenolic, alkaloid and flavonoid substances and is derived from Panax quinquefolius and Panax ginseng. Ginseng has natural antioxidant properties and is widely used as a medicine and health supplement that shows amelioration against reactive oxygen species generation (Kitts et al. 2000; Kim et al. 2005; Ramesh et al. 2012; Lee et al. 2017). Studies have also evaluated the effects of ginseng against acetamiprid induced toxicity. El-Bialy et al. (2020) showed the protective potential of ginseng aqueous extract (200 mg/kg b.wt) pre-treatment against hepato-renal toxicity induced by commercial pesticide mixture containing lambda-cyhalothrin (30 g/L) and acetamiprid (17 g/L). The extract decreased aspartate aminotransferase, alanine aminotransferase, malondialdehyde, nitric oxide, urea and creatinine levels while significantly increased total protein, globulin, glutathione and catalase activities; and mitigated histopathological alterations and apoptosis in hepatic and renal tissues of Wistar rats.
The synergistic protective effect of various plant extracts has also been shown against acetamiprid mediated hepatotoxicity. Shahin (2018) demonstrated that a combination of ginseng, green tea and cinnamon leaf extract ameliorated acetamiprid (100 mg/kg b.wt) induced liver damage as was evident from the decreased oxidative stress, and pro-inflammatory cytokine levels in rats. Further, the findings revealed that ginseng attenuated altered liver profile as confirmed by decreased aspartate aminotransferase and alanine aminotransferase activities and decreased levels of cholesterol, triglycerides, low-density lipoproteins and increased levels of total proteins, albumin, globulins and thyroid hormones followed by the improved antioxidant status of glutathione peroxidase and glutathione levels. It was suggested that ginseng, green tea and cinnamon have antioxidant potential, regulate metabolizing enzyme capacity synergistically at the gene level and show anti-allergic properties that might be responsible for hepatoprotection against acetamiprid exposure.
The leaves extracts rich in polyphenolic compounds also possess strong antioxidant properties and ameliorative potential against oxidative stress (Badmus et al. 2011; Mohan et al. 2013; Toledo et al. 2019). In relation to this, ethanolic extract of Mangifera indica leaves (50, 100 and 200 mg/kg b.wt) has also been shown to significantly decreases malondialdehyde levels, superoxide dismutase and catalase activities; increases glutathione and testosterone levels, reduced sperm abnormalities and thus attenuated reproductive toxicity induced by acetamiprid exposure in guinea pigs (Guiekep et al. 2019). Rhanterium suaveolens extracts are reported to have antioxidant, antimicrobial, hepatoprotective and anti-cholinesterase activities (Bouaziz et al. 2009; Amrani et al. 2014; Chemsa et al. 2016). Chelly et al. (2019) revealed that Rhanterium suaveolens methanolic extracts (300 mg/kg b.wt) reduced hemolytic anemia, oxidative stress and maintained hematological profile by preventing reactive oxygen species generation, maintaining enzymatic and non-enzymatic antioxidants and improving RBC count, hemoglobin and hematocrit level in erythrocytes of mice treated with acetamiprid.
Thus, various compounds have been evaluated to mitigate the acetamiprid toxicity in various organs (Table 5). Findings have revealed that most compounds ameliorate acetamiprid mediated toxicity via modulating oxidative stress and antioxidant status. It has been suggested that mitigation of oxidative stress could be the underlying mechanism of these protective compounds. Besides, having the same general mechanism, the effects of these compounds varies from organ to organ, suggesting that their ameliorative mechanism might have some specificity. These mechanisms need to be evaluated at the molecular level also, to evaluate their efficiency and specificity. A better understanding of these mechanisms will help the researchers to discover the highly efficient antidote for acetamiprid toxicity.
Perspective
Many studies have evaluated the toxicity of acetamiprid in non-target species and have demonstrated the close interaction between environmental residues of acetamiprid and their associated toxicity in mammals. Recent data has also supported the role of acetamiprid and its metabolites in different organ-associated toxicity. However acetamiprid-tissue interaction has been poorly characterized in terms of toxicokinetics and toxicodynamics and more technique-oriented studies are still warranted to gain insight the toxicity of acetamiprid in non-target species especially mammals. Further, in the reported studies several issues remain to be investigated. The first step would be more extensive identification and detection of acetamiprid residues levels in different abiotic factors, food products relevant in terms of human uptake. This would help in the identification of possible routes of environmental exposure. Further, interaction of acetamiprid with cellular transporter should be investigated in terms of toxicokinetics and toxicodynamics. The literature indicates that only some studies have provided qualitative data and only a few studies have insighted into the quantitative data. Hence, to evaluate the physiological and biochemical interaction of acetamiprid both qualitative and quantitative data should be evaluated to detect the inhibitory concentration of acetamiprid and its metabolites on different cellular molecules.
Various studies have evaluated the acetamiprid mediated toxicity in different in vitro and in vivo mammalian models and findings have confirmed the role of oxidative stress and involvement of apoptosis in toxic effects of acetamiprid. Although numerous studies have depicted lipid peroxidation and protein oxidation as general aftermath associated with acetamiprid exposure, more studies should be carried out probably involving the mass spectrometry-based lipidomic analysis and infrared spectroscopy-based functional group analysis to reveal tissue-specific lipid and protein profiles. Regarding the toxicity of acetamiprid, the last but not the least and probably the most important step would be to integrate findings from various in vitro and in vivo studies with known data in humans. In addition, regarding neurotoxicity and developmental toxicity, region-specific investigations involving molecular levels and genetic expressions of regulatory genes would be more helpful to describe the possible mechanisms of organ-associated toxicity. The findings of these studies would probably help to identify the initiation of toxicity cascades and to understand the possible mechanisms of toxicity.
The studies have also evaluated the effects of notable antioxidants against acetamiprid toxicity. However numerous antioxidants are being used worldwide, while limited information regarding their ameliorative potentials against acetamiprid has been evaluated. It is necessary to investigate the influence of the commonly used antioxidants with respect to their molecular level of interactions and effects on the bimolecular profile. In addition, some antioxidants are known to act synergistically when used simultaneously. Hence it would be a good approach to treat acetamiprid exposed individuals with a suitable combination of antioxidants. Meanwhile, the dosage and side effects of these antioxidants should also be determined as well.
Conclusion
Acetamiprid was synthesized to control insect pests in agriculture and community health considering its advantage of being less toxic to mammals than other pesticides. However, growing evidence depicts acetamiprid as a potential toxicant in different mammalian organs. It is widely persisting in the environment and evidences are accumulating for potential neurotoxic, hepatotoxic, immunotoxic and genotoxic exposure for mammals including humans. It is pertinent to evaluate the toxic effects and mechanism of acetamiprid toxicity in non-target species also. Acetamiprid is known to cause toxicity in a multistep cascade associated with nicotinic acetylcholine receptor inhibition and reactive oxygen species generation. The results of various studies have suggested that acetamiprid exposure causes oxidative stress and dysregulation of antioxidants levels leading to DNA damage and activation of the apoptosis pathway along with other detrimental effects (Fig. 2). The growing evidence has suggested an imperative need to evaluate the molecular interaction of acetamiprid and its metabolites with nicotinic acetylcholine subunits and inflammations, apoptosis and cancer pathway proteins. A greater understanding of acetamiprid biotransformation and the mechanism of oxidative stress generation may help to identify the most likely target that could help to design better abatement of acetamiprid toxicity in mammals. Although, accumulating evidence has suggested antioxidant, anti-apoptotic, anti-mutagenic and anti-inflammatory properties of some natural compounds against acetamiprid toxicity in various organs, it is imperative to establish the functional and molecular mechanisms of ameliorative substances against acetamiprid mediated organ toxicity pathways. More diverse studies regarding exposure to non-target species and conclusive ameliorative evidence are particularly warranted that might be helpful to develop a better understanding and formation of effective approach and will pave the path for more improved management and applications of acetamiprid in the future. Meanwhile, eco-friendly alternatives i.e. green pesticides, integrated pest management should be evaluated and incorporated to check their effectiveness against targeted pests. Possible areas of applications of acetamiprid should be identified and an effective combination of green pesticides and biological controls also including a reasonable amount of synthetic pesticides could be a sustainable approach to control pests.
General toxic effects of acetamiprid exposure inside mammals. Acetamiprid and its associated metabolites alters mitochondrial membrane potential, mediates free radical generation and depletes antioxidants status leading to oxidation of lipids and proteins along with DNA damage, inflammation and apoptosis. ΔѰm: mitochondrial membrane potential; ACMP: acetamiprid; ALP: alkaline phosphatase; ALT: alanine aminotransferase; AST: aspartate aminotransferase; ATP: adenosine triphosphate; cAMP: cyclic adenosine monophosphate; CAs: Chromosomal aberrations; DMAP: N-desmethyl acetamiprid; GDI: genetic damage index; ICAM-1: intracellular adhesion molecule-1; IL-6: interleukin 6; IL-10: interleukin 10; LDH: lactate dehydrogenase; MDA: malondialdehyde; MI: mitotic index; MN: micronuclei; NDI: nuclear division index; NF-KB: nuclear factor-kappa-B; NO: nitric oxide; Nrf2: nuclear factor erythroid 2-related factor; PI: proliferative index; PO: protein oxidation; ROS: reactive oxygen species; SCE: sister chromatids exchange; TBARS: thio-barbituric acid reactive substances; TNF-α: tumor necrosis factor α; TOS: total oxidant status
References
Abdollahi M, Ranjbar A, Shadnia S et al (2004) Pesticides and oxidative stress: a review. Med Sci Monitor 10:RA141–RA147
Abouzeid S (2018) Developmental toxicity of acetamiprid in rats. World J Pharm Pharmaceutical Sci. https://doi.org/10.20959/wjpps20182-10933
Albuquerque EX, Pereira EFR, Alkondon M, Rogers SW (2009) Mammalian nicotinic acetylcholine receptors: from structure to function. Physiol Rev 89:73–120. https://doi.org/10.1152/physrev.00015.2008
Alhusaini A, Fadda LM, Ali HM et al (2019) Mitigation of acetamiprid - induced renotoxicity by natural antioxidants via the regulation of ICAM, NF-kB and TLR 4 pathways. Pharmacol Rep 71:1088–1094. https://doi.org/10.1016/j.pharep.2019.06.008
Amrani A, Benaissa O, Boubekri N et al (2014) Effet hépatoprotecteur et antiradicalaire d’un extrait butanolique de Rhantherium suaveolens. Phytothérapie 12:386–392. https://doi.org/10.1007/s10298-014-0871-5
Annabi E, Ben Salem I, Abid-Essefi S (2019) Acetamiprid, a neonicotinoid insecticide, induced cytotoxicity and genotoxicity in PC12 cells. Toxicol Mech Methods 29:580–586. https://doi.org/10.1080/15376516.2019.1624907
Arican YE, Karaman EF, Özden S (2019) The subcronic effects of acetamipride on the global DNA methylation levels in Sprague-Dawley rat brain and liver. İstanbul J Pharm 49:167–172. https://doi.org/10.26650/IstanbulJPharm.2019.19058
Arıcan EY, Gökçeoğlu Kayalı D, Ulus Karaca B et al (2020) Reproductive effects of subchronic exposure to acetamiprid in male rats. Sci Rep 10:8985. https://doi.org/10.1038/s41598-020-65887-0
Babeľová J, Šefčíková Z, Čikoš Š et al (2017) Exposure to neonicotinoid insecticides induces embryotoxicity in mice and rabbits. Toxicology 392:71–80. https://doi.org/10.1016/j.tox.2017.10.011
Badmus JA, Adedosu TO, Fatoki JO et al (2011) Lipid peroxidation inhibition and antiradical activities of some leaf fractions of Mangifera indica. Acta Pol Pharm 68:23–9
Bagri P, Jain SK (2019) Assessment of acetamiprid-induced genotoxic effects in bone marrow cells of Swiss albino male mice. Drug Chem Toxicol 42:357–363. https://doi.org/10.1080/01480545.2018.1429461
Bhardwaj JK, Saraf P (2017) N-acetyl cysteine-mediated effective attenuation of methoxychlor-induced granulosa cell apoptosis by counteracting reactive oxygen species generation in caprine ovary. Environ Toxicol 32:156–166. https://doi.org/10.1002/tox.22221
Bonmatin J-M, Mitchell EA, Glauser G et al (2021) Residues of neonicotinoids in soil, water and people’s hair: a case study from three agricultural regions of the Philippines. Sci Total Environ 757:143822. https://doi.org/10.1016/j.scitotenv.2020.143822
Bouaziz M, Dhouib A, Loukil S et al (2009) Polyphenols content, antioxidant and antimicrobial activities of extracts of some wild plants collected from the south of Tunisia. Afr J Biotech 8(24):7017–7027
Brunet J-L, Maresca M, Fantini J, Belzunces LP (2008) Intestinal absorption of the acetamiprid neonicotinoid by Caco-2 cells: transepithelial transport, cellular uptake and efflux. J Environ Sci Health B 43:261–270. https://doi.org/10.1080/03601230701771446
Çavaş T, Çinkılıç N, Vatan Ö et al (2012) In vitro genotoxicity evaluation of acetamiprid in CaCo-2 cells using the micronucleus, comet and γH2AX foci assays. Pestic Biochem Physiol 104:212–217. https://doi.org/10.1016/j.pestbp.2012.08.004
Çavaş T, Çinkılıç N, Vatan Ö, Yılmaz D (2014) Effects of fullerenol nanoparticles on acetamiprid induced cytoxicity and genotoxicity in cultured human lung fibroblasts. Pestic Biochem Physiol 114:1–7. https://doi.org/10.1016/j.pestbp.2014.07.008
Chakroun S, Ezzi L, Grissa I et al (2016) Hematological, biochemical, and toxicopathic effects of subchronic acetamiprid toxicity in Wistar rats. Environ Sci Pollut Res 23:25191–25199. https://doi.org/10.1007/s11356-016-7650-9
Chawseen MA (2011) Effects of acetamiprid and glyphosate pesticides on testis and serum testosterone level in male mice. J Duhok Univ 14:299–306
Chelly S, Chelly M, Salah HB et al (2019) HPLC-DAD Analysis, Antioxidant and Protective Effects of Tunisian Rhanterium suaveolens against Acetamiprid Induced Oxidative Stress on Mice Erythrocytes. Chem Biodivers 16:e1900428. https://doi.org/10.1002/cbdv.201900428
Chemsa AE, Erol E, Öztürk M et al (2016) Chemical constituents of essential oil of endemic Rhanterium suaveolens Desf. growing in Algerian Sahara with antibiofilm, antioxidant and anticholinesterase activities. Nat Prod Res 30:2120–2124. https://doi.org/10.1080/14786419.2015.1110705
Christen V, Rusconi M, Crettaz P, Fent K (2017) Developmental neurotoxicity of different pesticides in PC-12 cells in vitro. Toxicol Appl Pharmacol 325:25–36. https://doi.org/10.1016/j.taap.2017.03.027
Craddock HA, Huang D, Turner PC et al (2019) Trends in neonicotinoid pesticide residues in food and water in the United States, 1999–2015. Environ Health 18:1–16. https://doi.org/10.1186/s12940-018-0441-7
Devan RKS, Prabu PC, Panchapakesan S (2015a) Immunotoxicity assessment of sub-chronic oral administration of acetamiprid in Wistar rats. Drug Chem Toxicol 38:328–336. https://doi.org/10.3109/01480545.2014.966382
Devan RS, Mishra A, Prabu PC et al (2015b) Sub-chronic oral toxicity of acetamiprid in Wistar rats. Toxicol Environ Chem 97:1236–1252. https://doi.org/10.1080/02772248.2015.1092542
Dhouib IB, Annabi A, Doghri R et al (2017) Neuroprotective effects of curcumin against acetamiprid-induced neurotoxicity and oxidative stress in the developing male rat cerebellum: biochemical, histological, and behavioral changes. Environ Sci Pollut Res Int 24:27515–27524. https://doi.org/10.1007/s11356-017-0331-5
Dinkova-Kostova AT, Talalay P (1999) Relation of structure of curcumin analogs to their potencies as inducers of Phase 2 detoxification enzymes. Carcinogenesis 20:911–914. https://doi.org/10.1093/carcin/20.5.911
Doltade S, Lonare M, Raut S, Telang A (2019) Evaluation of acetamiprid mediated oxidative stress and pathological changes in male rats: ameliorative effect of curcumin. Proc Natl Acad Sci India Sect B Biol Sci 89:191–199. https://doi.org/10.1007/s40011-017-0934-0
Dukhnytskyi V, Sokolyuk V, Boiko P et al (2020) The acute toxicity assesment of mospilan RP and Actara 25 WG for white mice. J World’s Poultry Res. https://doi.org/10.36380/jwpr.2020.41
Elbert A, Haas M, Springer B et al (2008) Applied aspects of neonicotinoid uses in crop protection. Pest Manag Sci 64:1099–1105. https://doi.org/10.1002/ps.1616
El-Bialy BES, Abd Eldaim MA, Hassan A, Abdel-Daim MM (2020) Ginseng aqueous extract ameliorates lambda-cyhalothrin-acetamiprid insecticide mixture for hepatorenal toxicity in rats: role of oxidative stress-mediated proinflammatory and proapoptotic protein expressions. Environ Toxicol 35:124–135. https://doi.org/10.1002/tox.22848
Erdemli ME, Zayman E, Erdemli Z et al (2020) Protective effects of melatonin and vitamin E in acetamiprid-induced nephrotoxicity. Environ Sci Pollut Res 27:9202–9213. https://doi.org/10.1007/s11356-019-06754-y
FAO Panel of Experts on Pesticide Residues in Food and the Environment., WHO Core Assessment Group on Pesticide Residues (2012) Pesticide residues in food - 2011: toxicological evaluations/Joint meeting of the FAO panel of experts on pesticide residues in food and the environment and the WHO core assessment group on pesticide residues, Geneva, Switzerland, 20–29 September 2011. World Health Organization, Geneva
Ford KA, Casida JE (2006) Chloropyridinyl neonicotinoid insecticides: diverse molecular substituents contribute to facile metabolism in mice. Chem Res Toxicol 19:944–951. https://doi.org/10.1021/tx0600696
Gasmi S, Rouabhi R, Kebieche M et al (2016) Neurotoxicity of acetamiprid in male albino rats and the opposite effect of quercetin. BioTechnol Indian J 12:14–22
Gasmi S, Kebieche M, Rouabhi R et al (2017) Alteration of membrane integrity and respiratory function of brain mitochondria in the rats chronically exposed to a low dose of acetamiprid. Environ Sci Pollut Res Int 24:22258–22264. https://doi.org/10.1007/s11356-017-9901-9
Gaweł M, Kiljanek T, Niewiadowska A et al (2019) Determination of neonicotinoids and 199 other pesticide residues in honey by liquid and gas chromatography coupled with tandem mass spectrometry. Food Chem 282:36–47. https://doi.org/10.1016/j.foodchem.2019.01.003
Ge R-S, Dong Q, Sottas CM et al (2005) Gene expression in rat leydig cells during development from the progenitor to adult stage: a cluster analysis1. Biol Reprod 72:1405–1415. https://doi.org/10.1095/biolreprod.104.037499
Gomez SD, Bustos PS, Sánchez VG et al (2020) Trophoblast toxicity of the neonicotinoid insecticide acetamiprid and an acetamiprid-based formulation. Toxicology 431:152363. https://doi.org/10.1016/j.tox.2020.152363
Gu Y, Li Y, Huang X et al (2013) Reproductive effects of two neonicotinoid insecticides on mouse sperm function and early embryonic development in vitro. PLoS ONE 8:e70112. https://doi.org/10.1371/journal.pone.0070112
Guiekep AJN, Kenfack A, Ngoula F et al (2019) Attenuating effects of Mangifera indica leaves ethanolic extract against acetamiprid induced reproductive toxicity in male guinea pigs. Vet Res Forum 10:187–192. https://doi.org/10.30466/vrf.2019.95154.2292
Guohong X, Guoguang L, Dezhi S, Liqing Z (2009) Kinetics of acetamiprid photolysis in solution. Bull Environ Contam Toxicol 82:129–132. https://doi.org/10.1007/s00128-008-9520-8
Gupta S, Gajbhiye VT (2007) Persistence of Acetamiprid in Soil. Bull Environ Contam Toxicol 78:349–352. https://doi.org/10.1007/s00128-007-9097-7
Gupta RK, Gupta S, Gajbhiye VT et al (2005) Residues of imidacloprid, acetamiprid and thiamethoxam in gram. Pestic Res J 17:46–50
Harvey BH, Joubert C, Du Preez JL, Berk M (2008) Effect of chronic N-acetyl cysteine administration on oxidative status in the presence and absence of induced oxidative stress in rat striatum. Neurochem Res 33:508–517. https://doi.org/10.1007/s11064-007-9466-y
Hataba AA, Keshta AT, Mead H, El-Shafey N (2014) Hematological, Biochemical and Histological alterations induced by oral administration of Thiamethoxam and Acetamiprid in male rats. Biochem Lett 10:113–125
Hong S-Y, Yang J-O, Lee E-Y, Lee Z-W (2003) Effects of N-acetyl-L-cysteine and glutathione on antioxidant status of human serum and 3T3 fibroblasts. J Korean Med Sci 18:649–654. https://doi.org/10.3346/jkms.2003.18.5.649
Ibrahim HZ, El-Banna SG, El Rafea AA (2020) Acetamiprid, insecticide-induced oxidative damage on reproductive parameters male rats. Alexandria J Veterinary Sci. 64
Ichikawa G, Kuribayashi R, Ikenaka Y et al (2019) LC-ESI/MS/MS analysis of neonicotinoids in urine of very low birth weight infants at birth. PLoS ONE 14:e0219208. https://doi.org/10.1371/journal.pone.0219208
Imamura T, Yanagawa Y, Nishikawa K et al (2010) Two cases of acute poisoning with acetamiprid in humans. Clin Toxicol (phila) 48:851–853. https://doi.org/10.3109/15563650.2010.517207
Kabata R, Nanayakkara S, Senevirathna S et al (2016) Neonicotinoid concentrations in urine from chronic kidney disease patients in the North Central Region of Sri Lanka. Jrnl of Occup Health 58:128–133. https://doi.org/10.1539/joh.15-0140-BR
Kagawa N, Nagao T (2018) Neurodevelopmental toxicity in the mouse neocortex following prenatal exposure to acetamiprid. J Appl Toxicol 38:1521–1528. https://doi.org/10.1002/jat.3692
Kara M, ÖztaŞ E, Özhan G (2020) Acetamiprid-induced Cyto- and genotoxicity in the AR42J pancreatic cell line. Turk J Pharm Sci 17:474–479. https://doi.org/10.4274/tjps.galenos.2019.89719
Karaca BU, Arican YE, Boran T et al (2019) Toxic effects of subchronic oral acetamiprid exposure in rats. Toxicol Ind Health 35:679–687. https://doi.org/10.1177/0748233719893203
Kenfack A, Guiekep NAJ, Ngoula F et al (2018) Reproductive toxicity of acetamiprid in male Guinea pig (Cavia porcellus). J Anim Sci Vet Med 3:105–111. https://doi.org/10.31248/JASVM2018.101
Khovarnagh N, Seyedalipour B (2021) Antioxidant, histopathological and biochemical outcomes of short-term exposure to acetamiprid in liver and brain of rat: the protective role of N-acetylcysteine and S-methylcysteine. Saudi Pharmaceutical J. https://doi.org/10.1016/j.jsps.2021.02.004
Kim SH, Park KS, Chang MJ, Sung JH (2005) Effects of Panax ginseng extract on exercise-induced oxidative stress. J Sports Med Phys Fitness 45:178
Kimura-Kuroda J, Komuta Y, Kuroda Y et al (2012) Nicotine-like effects of the neonicotinoid insecticides acetamiprid and imidacloprid on cerebellar neurons from neonatal rats. PLoS ONE 7:e32432. https://doi.org/10.1371/journal.pone.0032432
Kimura-Kuroda J, Nishito Y, Yanagisawa H et al (2016) Neonicotinoid insecticides alter the gene expression profile of neuron-enriched cultures from neonatal rat cerebellum. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph13100987
Kitts DD, Wijewickreme AN, Hu C (2000) Antioxidant properties of a North American ginseng extract. Mol Cell Biochem 203:1–10. https://doi.org/10.1023/A:1007078414639
Kocaman AY, Topaktaş M (2007) In vitro evaluation of the genotoxicity of acetamiprid in human peripheral blood lymphocytes. Environ Mol Mutagen 48:483–490. https://doi.org/10.1002/em.20309
Kocaman AY, Topaktaş M (2010) Genotoxic effects of a particular mixture of acetamiprid and alpha-cypermethrin on chromosome aberration, sister chromatid exchange, and micronucleus formation in human peripheral blood lymphocytes. Environ Toxicol 25:157–168. https://doi.org/10.1002/tox.20485
Kolanczyk RC, Tapper MA, Sheedy BR, Serrano JA (2020) In vitro metabolism of imidacloprid and acetamiprid in rainbow trout and rat. Xenobiotica 50:805–814. https://doi.org/10.1080/00498254.2019.1694197
Kong D, Zhang J, Hou X et al (2017) Acetamiprid inhibits testosterone synthesis by affecting the mitochondrial function and cytoplasmic adenosine triphosphate production in rat Leydig cells†. Biol Reprod 96:936. https://doi.org/10.1093/biolre/iox007
Kumar P, Meizel S (2005) Nicotinic acetylcholine receptor subunits and associated proteins inhuman sperm*. J Biol Chem 280:25928–25935. https://doi.org/10.1074/jbc.M502435200
Kushwaha N, Mohan A, Bhikane AU (2018) Accidental acetamiprid poisoning in a buffalo. Iran J Vet Res 19:318–320
Lasram MM, Lamine AJ, Dhouib IB et al (2014) Antioxidant and anti-inflammatory effects of N-acetylcysteine against malathion-induced liver damages and immunotoxicity in rats. Life Sci 107:50–58. https://doi.org/10.1016/j.lfs.2014.04.033
Lee Y-M, Yoon H, Park H-M et al (2017) Implications of red Panax ginseng in oxidative stress associated chronic diseases. J Ginseng Res 41:113–119. https://doi.org/10.1016/j.jgr.2016.03.003
Mandal PS, Mondal S, Karnam SS, Purohit K (2015) A behavioral study on learning a memory in adult Sprague Dawley rat in induced acetamiprid toxicity. Explor Anim Med Res 5:27–32
Marfo JT, Fujioka K, Ikenaka Y et al (2015) Relationship between Urinary N-desmethyl-acetamiprid and typical symptoms including neurological findings: a prevalence case-control study. PLoS ONE 10:e0142172. https://doi.org/10.1371/journal.pone.0142172
Marın A, Vidal JM, Gonzalez FE et al (2004) Assessment of potential (inhalation and dermal) and actual exposure to acetamiprid by greenhouse applicators using liquid chromatography–tandem mass spectrometry. J Chromatogr B 804:269–275. https://doi.org/10.1016/j.jchromb.2004.01.022
Martinez-Pena Y, Valenzuela I, Akaaboune M (2021) The metabolic stability of the nicotinic acetylcholine receptor at the neuromuscular junction. Cells 10:358. https://doi.org/10.3390/cells10020358
Marzouki S, Bini Dhouib I, Benabdessalem C et al (2017) Specific immune responses in mice following subchronic exposure to acetamiprid. Life Sci 188:10–16. https://doi.org/10.1016/j.lfs.2017.08.022
Mohan CG, Deepak M, Viswanatha GL et al (2013) Anti-oxidant and anti-inflammatory activity of leaf extracts and fractions of Mangifera indica. Asian Pac J Trop Med 6:311–314. https://doi.org/10.1016/s1995-7645(13)60062-0
Mondal S, Sengupta T, Pradhan S et al (2014) Impaired learning and memory after a week-long exposure of acetamiprid in adult rats. Adv Anim Vet Sci 2:543–548. https://doi.org/10.14737/journal.aavs/2014/2.10.543.548
Mondal S, Mukhopadhayay SK, Kumar S et al (2015) Haematobiochemical profile in chronic acetamiprid exposure in Sprague Dawley rats. Adv Anim Vet Sci 3:384–394. https://doi.org/10.14737/journal.aavs/2015/3.7.384.394
Mosbah R, Djerrou Z, Mantovani A (2018) Protective effect of Nigella sativa oil against acetamiprid induced reproductive toxicity in male rats. Drug Chem Toxicol 41:206–212. https://doi.org/10.1080/01480545.2017.1337127
Muranli FDG, Rasgele PG, Kekecoglu M et al (2015) Potential genotoxicity of acetamiprid and propineb singly or in combination in cultured human peripheral blood lymphocytes by using MN assay. Fresenius Environ Bull 24:3947–3955
Nakayama A, Yoshida M, Kagawa N, Nagao T (2019) The neonicotinoids acetamiprid and imidacloprid impair neurogenesis and alter the microglial profile in the hippocampal dentate gyrus of mouse neonates. J Appl Toxicol 39:877–887. https://doi.org/10.1002/jat.3776
Neghab M, Momenbella-Fard M, Naziaghdam R et al (2014) The effects of exposure to pesticides on the fecundity status of farm workers resident in a rural region of Fars province, southern Iran. Asian Pacific J Trop Biomed 4:324–328. https://doi.org/10.12980/APJTB.4.2014C586
Neha K, Haider MR, Pathak A, Yar MS (2019) Medicinal prospects of antioxidants: a review. Eur J Med Chem 178:687–704. https://doi.org/10.1016/j.ejmech.2019.06.010
Ogawa T, Ueyama J, Suzuki T et al (2018) In vivo metabolic profiling for acetamiprid in rat plasma by liquid chromatography quadrupole time-of-flight mass spectrometry. Med Mass Spectrom 2:34–40. https://doi.org/10.24508/mms.2018.06.003
Pirasath S, Senthuran R, Athirayan C et al (2021) Acute poisoning with acetamiprid: a case report. J Med Case Rep 15:419. https://doi.org/10.1186/s13256-021-02919-x
Pisoschi AM, Pop A (2015) The role of antioxidants in the chemistry of oxidative stress: a review. Eur J Med Chem 97:55–74. https://doi.org/10.1016/j.ejmech.2015.04.040
Poljsak B, Šuput D, Milisav I (2013) Achieving the balance between ROS and antioxidants: when to use the synthetic antioxidants. Oxid Med Cell Longev. https://doi.org/10.1155/2013/956792
Pramanik SK, Bhattacharyya J, Dutta S et al (2006) Persistence of acetamiprid in/on mustard (Brassica juncea L.). Bull Environ Contam Toxicol 76:356–360. https://doi.org/10.1007/s00128-006-0929-7
Quintana MM, Rivero Osimani V, Magnarelli G et al (2018) The insecticides chlorpyrifos and acetamiprid induce redox imbalance in umbilical cord blood erythrocytes in vitro. Pestic Biochem Physiol 148:87–92. https://doi.org/10.1016/j.pestbp.2018.04.001
Ramesh T, Kim S-W, Hwang S-Y et al (2012) Panax ginseng reduces oxidative stress and restores antioxidant capacity in aged rats. Nutr Res 32:718–726. https://doi.org/10.1016/j.nutres.2012.08.005
Rasgele PG, Oktay M, Kekecoglu M, Muranli FDG (2015) The histopathological investigation of liver in experimental animals after short-term exposures to pesticides. Bulgarian J Agr Sci 21:446–453
Renaud M, Akeju T, Natal-da-Luz T et al (2018) Effects of the neonicotinoids acetamiprid and thiacloprid in their commercial formulations on soil fauna. Chemosphere 194:85–93. https://doi.org/10.1016/j.chemosphere.2017.11.102
Sano K, Isobe T, Yang J et al (2016) In utero and lactational exposure to acetamiprid induces abnormalities in socio-sexual and anxiety-related behaviors of male mice. Front Neurosci 10:228. https://doi.org/10.3389/fnins.2016.00228
Sanyal D, Chakma D, Alam S (2008) Persistence of a neonicotinoid insecticide, acetamiprid on chili (Capsicum annum L.). Bull Environ Contam Toxicol 81:365–368. https://doi.org/10.1007/s00128-008-9479-5
Şenyildiz M, Kilinc A, Sibel O (2018) Investigation of the genotoxic and cytotoxic effects of widely used neonicotinoid insecticides in HepG2 and SH-SY5Y cells. Toxicol Ind Health. https://doi.org/10.1177/0748233718762609
Shahin MI (2018) Hepatoprotective effect of ginseng, green tea, cinnamon their combination against acetamiprid-induced oxidative stress in rats. Asian J Biol 5:1–13. https://doi.org/10.9734/AJOB/2018/38202
Shamsi M, Soodi M, Shahbazi S, Omidi A (2021) Effect of Acetamiprid on spatial memory and hippocampal glutamatergic system. Environ Sci Pollut Res Int. https://doi.org/10.1007/s11356-020-12314-6
Statistical Database|Directorate of plant protection, quarantine & storage|GOI. http://ppqs.gov.in/statistical-database. Accessed 28 Sep 2021
Taira K, Fujioka K, Aoyama Y (2013) Qualitative profiling and quantification of neonicotinoid metabolites in human urine by liquid chromatography coupled with mass spectrometry. PLoS ONE 8:e80332. https://doi.org/10.1371/journal.pone.0080332
Terayama H, Endo H, Tsukamoto H et al (2016) Acetamiprid accumulates in different amounts in murine brain regions. Int J Environ Res Public Health 13:937. https://doi.org/10.3390/ijerph13100937
Terayama H, Qu N, Endo H et al (2018) Effect of acetamiprid on the immature murine testes. Int J Environ Health Res 28:683–696. https://doi.org/10.1080/09603123.2018.1504897
Tian Y, Wang Y, Sheng Z et al (2016) A colorimetric detection method of pesticide acetamiprid by fine-tuning aptamer length. Anal Biochem 513:87–92. https://doi.org/10.1016/j.ab.2016.09.004
Toledo RCL, Brito LF, Caetano MMM et al (2019) Acute treatment with Mangifera indica L. leaf extract attenuates liver inflammation in rats fed a cafeteria diet. Food Funct 10:4861–4867. https://doi.org/10.1039/c9fo00651f
Tomizawa M, Casida JE (2005) Neonicotinoid insecticide toxicology: mechanisms of selective action. Annu Rev Pharmacol Toxicol 45:247–268. https://doi.org/10.1146/annurev.pharmtox.45.120403.095930
Ueyama J, Aoi A, Ueda Y et al (2020) Biomonitoring method for neonicotinoid insecticides in urine of non-toilet-trained children using LC-MS/MS. Food Addit Contaminants Part A 37:304–315. https://doi.org/10.1080/19440049.2019.1696020
Wallace DR (2014) Acetamiprid. In: Encyclopedia of toxicology. Elsevier. pp 30–32. https://doi.org/10.1016/B978-0-12-386454-3.00091-9
Wu J, Wang K, Zhang H (2012) Dissipation and residue of acetamiprid in watermelon and soil in the open field. Bull Environ Contam Toxicol 89:644–648. https://doi.org/10.1007/s00128-012-0733-5
Xu M, Huang H, Li N et al (2019) Occurrence and ecological risk of pharmaceuticals and personal care products (PPCPs) and pesticides in typical surface watersheds, China. Ecotoxicol Environ Saf 175:289–298. https://doi.org/10.1016/j.ecoenv.2019.01.131
Yamamuro T, Ohta H, Aoyama M, Watanabe D (2014) Simultaneous determination of neonicotinoid insecticides in human serum and urine using diatomaceous earth-assisted extraction and liquid chromatography–tandem mass spectrometry. J Chromatogr B 969:85–94. https://doi.org/10.1016/j.jchromb.2014.06.008
Yan S, Meng Z, Tian S et al (2020) Neonicotinoid insecticides exposure cause amino acid metabolism disorders, lipid accumulation and oxidative stress in ICR mice. Chemosphere 246:125661. https://doi.org/10.1016/j.chemosphere.2019.125661
Yeter O, Aydın A (2014) Determination of acetamiprid and IM-1-2 in postmortem human blood, liver, stomach contents by HPLC-DAD. J Forensic Sci 59:287–292. https://doi.org/10.1111/1556-4029.12368
Yi-Wang J-JZ, Xiang H-Y, Jia-Hua Z, Wang X-Z (2012) Acetamiprid residues in male mice and its effect on liver function. J Anim Vet Adv 11:2706–2710
Zhang J, Yi W, Xiang H et al (2011) Oxidative stress: role in acetamiprid-induced impairment of the male mice reproductive system. Agric Sci China 10:786–796. https://doi.org/10.1016/S1671-2927(11)60063-1
Zhang J, Wang Y, Xiang H, Wang X (2012) Nephrotoxicity of acetamiprid on male mice and the rescue role of vitamin E. J Anim Vet Adv 11:2721–2726
Zoumenou BGYM, Aïna MP, Imorou Toko I et al (2019) Occurrence of acetamiprid residues in water reservoirs in the cotton basin of northern benin. Bull Environ Contam Toxicol 102:7–12. https://doi.org/10.1007/s00128-018-2476-4
Acknowledgements
Author Annu Phogat is thankful to University Grant Commission, New Delhi for Junior Research Fellowship.
Funding
None.
Author information
Authors and Affiliations
Contributions
The authors conceptualized the ideas and design of this review jointly. AP and JS searched the relevant literature and compiled the first draft. VK and VM critically analyzed the first draft and designed the final manuscript. All the authors approved the final manuscript and provided their consent for publication.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Phogat, A., Singh, J., Kumar, V. et al. Toxicity of the acetamiprid insecticide for mammals: a review. Environ Chem Lett 20, 1453–1478 (2022). https://doi.org/10.1007/s10311-021-01353-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10311-021-01353-1