Abstract
Recently, sealers based on calcium silicates were developed as a new class of endodontic sealers. Inspired by the excellent sealing ability and biocompatibility of calcium silicate-based cements, these sealers establish a biological point of view on the obturation of root canals. No longer, the bacteria-tight seal against reinfection of the root canal is the only goal of root canal obturation. Antibacterial properties as well as bioactive inducement of periapical healing and hard tissue formation are added to the portfolio of sealers. Ready-to-use sealers consisting of only one component with a need for external water supply from, e.g., body fluid and two components sealers with internal water supply were introduced to the market. Both of these material types have the same setting reactions in common whereby a hydration reaction of the calcium silicate is followed by a precipitation reaction of calcium phosphate. Though the available sealers are all based on calcium silicates, they consist of different compositions. Due to this aspect, differences in their physical and chemical properties as well as in their in vitro characteristics were described. Studies addressing the clinical impact of calcium silicate-based sealers on outcome are still sparse. The bioactive potential of sealers based on calcium silicates is a consequence of the slight solubility of these materials even after setting, but solubility of the sealer might also compromise the quality of sealing a root canal against regrowth and reinfection. Further clinical investigations are required to evaluate the clinical relevance of the gulf between bioactivity and solubility.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cements based on a composition of calcium and silicate such as mineral trioxide aggregate [1] (e.g., ProRoot MTA, Dentsply Sirona, York, USA) or Biodentine (Septodont, St. Maur-des-Fossés, France) have been introduced to modern dentistry over the past 2 decades and are well established [1]. Due to their excellent sealing ability and biocompatibility, these cements are used for many clinical applications such as pulp capping in primary and permanent teeth, root-end filling, perforation repair, and apical plug for teeth with open apices [1, 2]. With regard to the favorable characteristics of calcium silicate-based cements, endodontic sealers based on the compositions of calcium silicates have been introduced over the last years.
The first endodontic sealer of this new class introduced in 2007 was iRoot SP (Innovative Bioceramix, Vancouver, Canada) which was associated with the attribute “bioceramic”. Since then, other products based on calcium silicates were introduced and different classifications have been proposed to delimit this new class of endodontic sealers from conventional sealers. Bioceramic is a term introduced for an important subset of biomaterials [3] and includes materials that can be classified as bioinert, bioactive or biodegradable according to the interaction with surrounding tissues [4]. Bioceramics can be implanted into the body without causing a foreign body reaction [5] and are compositions of alumina and zirconia, bioactive glass, glass ceramics, calcium silicates, hydroxyapatite and resorbable calcium phosphates, and radiotherapy glasses [6]. iRoot SP is mainly composed of di- and tricalcium silicates and, therefore, it can be classified as a bioceramic. As seen in the following, the setting reaction of calcium silicates results in the precipitation of calcium phosphate, which can encourage bioactivity and tissue growth after contact [7]. Nonetheless, bioceramics is a wide field in medicine and calcium silicate-based cements or sealers only display a small subset of bioceramics, as bioceramics can further be divided into bioinert, bioactive and biodegradable [4]. Calcium silicates mainly belong to bioactive bioceramics as these durable materials can undergo interfacial interactions with surrounding tissue [4]. Unfortunately, the term “bioceramic” does not delimit sealers based on calcium silicates from other bioactive bioceramics or other bioceramic material types such as calcium phosphate-based sealers [8]. Due to the hydraulic setting reaction, meaning that calcium silicate sets by reacting with water provided by tissue fluids and then is stable in water or humid conditions [9], sealers based on calcium silicate have also been announced as hydraulic sealers [10, 11]. The biological properties of calcium silicates depend on the formation of calcium hydroxide as a by-product of this hydration reaction [9, 12]. Therefore, the term “hydraulic” is not precisely enough for describing sealers based on calcium silicate as slight solubility in water of these is a major concern of such a classification as can be seen in the following.
Based on the materials’ main component, calcium silicate, the sealers of this group are announced “calcium silicate-based sealers” (CSBS) in the following. This terminology according to the major component is used throughout all other endodontic sealers as well. The CSBS class contains a group of premixed CSBS with need for external water supply and a group of two components CSBS with internal water supply (Table 1). Both of these materials have the same setting reactions in common. The first reaction is a hydration reaction, which can be found in two different types (A, B) [7]:
The hydration reaction is followed by a precipitation reaction of calcium phosphate:
Some other sealers available on the market contain bound calcium silicates embedded in different matrices. Matrices such as silicones (GuttaFlow BioSeal, Coltène Whaledent, Langenau, Germany), resins (Smartpaste Bio, DRFP Ltd, Stamford, UK), or calcium salicylates (MTA Fillapex, Angelus, Londrina, Brazil) were described. The biological effect of calcium silicates in an inert matrix is questionable [12] and, therefore, these sealers were not further discussed in this review.
The aim of this focused review is to present a structured literature review of the current knowledge concerning CSBS.
Literature research strategy
This review aimed to present the literature about CSBS. A preliminary literature research on reviews concerning CSBS was performed in August 2018 using the search terms “calcium silicate[All Fields]) AND based[All Fields] AND sealer[All Fields]) AND Review[ptyp]]”, “bioceramic[All Fields] AND sealer[All Fields]) AND Review[ptyp]”, “endodontic[All Fields] AND bioceramic[All Fields]) AND Review[ptyp]”, and “hydraulic[All Fields] AND sealer[All Fields] AND Review[ptyp]”. 11 relevant literature reviews [4, 5, 8, 13,14,15,16,17,18,19,20] were identified in the field of CSBS with none of them giving an adequate, extensive and to date overview about all characteristics of CSBS.
An electronic literature research in the database PubMed was performed in September 2018 using the search terms “calcium silicate“[All Fields]) AND based[All Fields] AND sealer[All Fields]”, “hydraulic[All Fields] AND sealer[All Fields]”, “bioceramic[All Fields] AND sealer[All Fields]”, “bioceramic[All Fields] AND endodontic[All Fields]”, “iRoot SP[Supplementary Concept] OR “iRoot SP“[All Fields] OR “iroot sp“[All Fields]”, “endosequence[All Fields] AND “bc“[All Fields] AND sealer[All Fields]”, “total[All Fields] AND fill[All Fields] AND sealer[All Fields]”, “bioroot[All Fields] AND “rcs“[All Fields]”, “endo[All Fields] AND cpm[All Fields]”, “endo[All Fields] AND c.p.m.[All Fields]”, “endoseal[All Fields] AND mta[All Fields]”, “well[All Fields] AND “root“[All Fields] AND “st“[All Fields] AND “sealer“[All Fields]”, “tech[All Fields] AND biosealer[All Fields] AND endo[All Fields]”, “nano-ceramic[All Fields] AND sealer[All Fields]”. The titles and abstracts were screened for relevance and the remaining articles were ordered in full text. Language was restricted to English. The systematic search resulted in 194 articles, of which 26 were excluded due to the following reasons: review, studies concerning experimental sealers, study not focusing on CSBS, insufficient data for a particular sealer. Relevant numbers of publications were provided for iRoot SP and the identically composed sealers EndoSequence BC Sealer (Brasseler USA, Savannah, USA) and Total Fill BC Sealer (FKG Dentaire, La Chaux-de-Fonds, Switzerland) as well as for BioRoot RCS (Septodont), Endoseal MTA (Maruchi, Wonju, Korea) and Endo CPM (EGEO SRL, Buenos Aires, Argentina). 168 articles were considered relevant and included into this review.
Other products found in the literature were ProRoot Endo Sealer (Dentsply), TechBiosealer Endo (Isasan SRL, Revello Porro, Italy), Well-Root ST (Vericom, Gangwon-Do, Korea) and Nano-ceramic Sealer (B&L Biotech, Fairfax, USA), for which no sufficient data could be provided at the date this review was written. Therefore, these products and other experimental CSBS were excluded from this review. A newly launched product is EndoSequence BC Sealer Hi-Flow (Brasseler), which was not included in this review because of a lack of publications. It is a new development of EndoSequence BC Sealer and the first CSBS optimized for warm obturation techniques. All other CSBS are yet only available for cold obturation techniques [21] because of the expected intracanal temperatures [22] and the unknown effects of intracanal heating on CSBS.
In this review, only sealers were considered; thus, root canal filling materials which are designed to be used in combination with a core material. Calcium silicate-based cements, repair or so-called “putty” materials, which are also partially released for root canal obturation, are not included.
Table 1 provides a list of CSBS available on the international market and gives an overview about identical brands, product delivery and compositions. Identical products that can be purchased under different brand names according to the sales region are summed up under the first introduced product of the group and named accordingly in the following.
Composition and properties
Different formulations of CSBS have been introduced after the introduction of the first CSBS iRoot SP. Due to the major component of all CSBS, calcium silicate, their setting reaction is comparable. Calcium silicates form various phases of calcium silicate hydrate after hydration such as porous colloidal calcium silicate hydrate gel and radial acicular calcium silicate hydrate crystals, calcium hydroxide crystals, hexacalcium aluminate trisulphate crystals and calcium monosulfoaluminate or calcium monocarboaluminate. Porous calcium silicate hydrate sets into a solid network. The setting reaction requires several days to complete the hydration and hardening phases throughout the material [14, 23].
Whilst all products differ in their composition, a major difference exists in the type of delivery between premixed products with external water supply (body fluid) and two-component products with internal water supply (Table 1).
Physiochemical properties
Material characterization
Premixed ready-to-use formulations prone for external water supply and two-component self-curing materials are available as described above. Though different formulations were established, all CSBS have the main component calcium silicates in common [10]. To evaluate the material’s characterizations, energy-dispersive spectroscopy (EDS) is used for elemental analysis whilst X-ray diffraction analysis (XRD) is used to characterize the main crystalline phases present in the material and scanning electron microscopy (SEM) is commonly used to characterize the microstructure of sealer surfaces. Raman spectroscopy is commonly used to investigate the chemical structures of materials.
EDS
CSBS are composed of a cement matrix with embedded radiopacifiers [24]. The cement phase mainly consists of calcium and silicon [24]. Calcium and phosphate increase on the surface of iRoot SP was reported in EDS analysis, which was proven to be carbonated apatite [25]. EDS analysis showed the presence of precipitates with high proportions of calcium on the surface of iRoot SP after immersion in simulated body fluid [26]. Immersion in phosphate buffered saline leads to a surface precipitation of calcium hydroxyapatite on BioRoot RCS [27] (Fig. 1). Immersed in HBSS, BioRoot RCS forms an interfacial zone at the dentin distinct from the rest of the sealer [24].
Portland cements are known to contain different trace elements such as arsenic or lead [28]. The containment of trace elements was reported for Endoseal MTA, which exhibits high levels of aluminum [24]. BioRoot RCS was reported to be free of heavy metal trace elements [29] and is composed of pure tricalcium silicate [24].
XRD
The analysis of the material characterization via XRD revealed the presence of different radiopacifiers in the CSBS. Zirconium oxide is used in BioRoot RCS while zirconium oxide and bismuth oxide were found in Endoseal MTA [10]. In wavelength-dispersive X-ray spectroscopy, lesser calcium and silicon incorporation into human root dentin was found for iRoot SP compared to Biodentine and MTA [30].
SEM
iRoot SP has a regular surface in SEM when freshly mixed and a well-distributed coating composed of small spherulites after 28 days [25]. After solubility tests, morphological changes in the surface of iRoot SP with a loss of matrix and more distinguishable filler particles, and high levels of calcium and carbon on the surface were reported [31].
Raman spectroscopy
Heating BioRoot RCS to 250 °C for 30 or 60 s to simulate the effect of warm vertical compaction techniques did not affect the chemical structure of BioRoot RCS [32]. In a recent study, maximum temperatures of 56 °C inside the root canal during warm vertical compaction techniques [22] were reported, relativizing the above-mentioned results.
Radiopacity
iRoot SP [25, 33,34,35,36], BioRoot RCS [10, 27, 37, 38], Endoseal MTA [10, 35, 39], and Endo CPM [40,41,42] were reported to fulfill the requirements laid down in the ISO-norm 6876:2012 with a radiopacity greater than 3 mm aluminum thickness.
Flow and film thickness
The sealers iRoot SP [33, 35, 36, 43], BioRoot RCS [10], Endoseal MTA [10, 35, 39], and Endo CPM [41] were reported to fit the requirements laid down in the ISO-norm 6876:2012 of flow greater than 17 mm. BioRoot RCS slightly failed to reach this threshold in one study [37]. A temperature rise to 140 °C reduced the flow of iRoot SP from 22.9 ± 0.9 to 13.3 ± 1.5 mm [44].
The sealers iRoot SP [43], BioRoot RCS [10], and Endoseal MTA [10] fulfilled the ISO specification of film thickness lesser than 50 µm in several studies. Contradictory results concerning film thickness were reported for BioRoot RCS in one study [37]. Higher film thickness compared to AH Plus (Dentsply DeTrey, Konstanz, Germany) was found for iRoot SP [43].
Setting time
Regarding premixed CSBS with the need of external water supply for the setting reaction, contradictory results were reported. Prolonged setting times were found for iRoot SP of 52 h [25] up to 168 h [45]. In contrast, according to one study iRoot SP did not set completely in humid incubator conditions within 4 weeks [35], whereas other studies reported that iRoot SP set within 2.7 h [43] respectively 4.7 h [36] under the same conditions. A temperature rise to 140 °C reduced the setting time of iRoot SP [43]. Full setting under dry conditions [10] and setting within 20 h under humid incubator conditions [35] was related for Endoseal MTA.
Setting time analysis under dry conditions revealed full setting of two-component sealer BioRoot RCS [10]. Setting times of approximately 5 h were accounted for BioRoot RCS [27, 38] whilst BioRoot RCS set within 27 min in one study [37]. The immersion of BioRoot RCS and Endoseal MTA in Hank’s balanced salt solution (HBSS) or Dulbecco's modified eagle medium (DMEM) extended the setting time of these sealers [10].
Water sorption and solubility
The water sorption of iRoot SP [25, 46], BioRoot RCS [10] and Endoseal MTA [10] was reported to be higher than that of AH Plus extending close to the limitations of the ISO-norm 4049 recommending less than 40 mg/mm3 after 28 days.
Higher sorption of iRoot SP compared to other BC materials was related [25]. High initial water sorption shortly after setting, but less 7 days after setting, was found for BioRoot RCS [38]. Fluid uptake of BioRoot RCS and Endoseal MTA was higher than that of AH Plus irrespective of the immersion medium (distilled water, HBSS or DMEM) [10]. Fluid uptake of BioRoot RCS increased over a 28-day period while the fluid uptake of Endoseal MTA decreased over the same period after high initial fluid uptake [10].
Higher solubility exceeding the ISO 6876 requirements of less than 3% weight loss after immersion in water for 24 h was reported for BioRoot RCS [10, 47, 48] and iRoot SP [47, 48]. The same results were reported for iRoot SP after 7 days [31, 36] and 30 days [36] of immersion. On the contrary, solubility not exceeding 3% within 24 h as stated in the ISO 6873 was accounted for iRoot SP [43, 46], BioRoot RCS [49], Endoseal MTA [10, 39] and Endo CPM [42] in other studies. Overall, compared to epoxy resin-based sealers, solubility of CSBS was found to be higher [10, 31, 43, 46,47,48,49]. Solubility of iRoot SP was also higher compared to other BC materials [25]. BioRoot RCS was related to less solubility 7 days after the sealer set compared to freshly set sealer [38]. In distilled water, higher solubility was found for BioRoot RCS compared to the immersion in PBS, which reduced the solubility of BioRoot RCS [27, 49]. A long-term investigation of solubility found that the solubility of BioRoot RCS was in accordance with the ISO 6876 requirements even over a 6-month period when stored in phosphate buffered saline [49].
Porosity, compressive strength and expansion
Higher porosity of iRoot SP compared to other BC materials was reported [25]. BioRoot RCS [10, 38] and Endoseal MTA [10] were shown to possess higher porosity than AH Plus in one study. The porosity of BioRoot RCS and Endoseal MTA decreased over a 28-day period when immersed in HBSS [10].
The surface microhardness of iRoot SP and Endoseal MTA decreased when immersed in PBS for 14 days compared to the incubation at 100% humidity [50].
Endoseal MTA showed slightly higher expansion than laid down in the ISO-norm 6876, but lesser expansion than epoxy resin-based sealers when immersed in water for 30 days [35]. iRoot SP showed a slight reduction of volume under the same conditions [36] in one study, whilst contrarily a slight expansion was reported in another study [44]. In another study, Endoseal MTA exhibited a higher dimensional change than AH Plus [39].
Leaching of ions
High leaching of calcium was reported for iRoot SP [31, 33, 51] with a higher calcium release in the initial 14 days and a decrease of calcium release at the end of a 28-day period [25]. Immersed in PBS for a period of 7 days, calcium ion release from iRoot SP decreased at the end of the period [30]. Calcium release of iRoot SP was lower than of MTA [30]. High calcium release in the initial phase after mixture was also related for BioRoot RCS [33, 37, 38] and Endo CPM [52] with BioRoot RCS presenting higher calcium ion release than other CSBS [10, 53]. BioRoot RCS kept leaching calcium for 28 days [37]. Leaching of aluminum and bismuth was found for Endoseal MTA [10].
Alkalinizing/pH
Before and after setting, iRoot SP showed a high alkaline pH [33, 43, 51] as well as within a 24-h period [47, 48]. iRoot SP also showed high alkalizing potential of the immersion solution for a period of 14 days [25] respectively 28 days [36] with a decrease of the pH at the end of a 28-day period [25, 36]. Similarly, high alkaline pH for BioRoot RCS at 3 h and 24 h after mixing [47, 48], and high alkalizing potential in the initial 14-day phase [38] were reported. High alkaline pH was also found for Endoseal MTA [35, 39] and Endo CPM [54]. Endo CPM kept its alkalizing potential at least over a 7-day period [42, 52]. BioRoot RCS and Endoseal MTA were shown to constantly increase the pH of the immersion solution over a 28-day period [10, 35, 37]. In a long-term investigation, the pH of BioRoot RCS decreased continuously over a 6-month period but still was found to be alkaline after 6-month immersion in distilled water and after 4 months in PBS [49].
Highlights of physiochemical properties
-
CSBS were mostly reported to fit the requirements laid down in the ISO-norm 6876 regarding radiopacity, film thickness, flow and solubility.
-
Immersion of BioRoot RCS in phosphate buffered saline led to a surface precipitation of calcium hydroxyapatite in vitro, which is an evident indication for the bioactivity of CSBS.
-
The alkalizing potential of CSBS was high for all CSBS in the initial state, and long-term alkaline activity was accounted for BioRoot RCS.
Interaction with dentin
Dentinal tubule penetration
Dentinal tubule penetration as deep as 2 mm was reported for iRoot SP [55]. Compared to the epoxy resin-based sealer AH Plus, some studies related significantly higher dentinal tubule penetration of iRoot SP [56,57,58], whereas other studies did not find differences in the dentinal tubule penetration of iRoot SP and epoxy resin-based sealers [59, 60]. The use of chelating agents [61] or irrigation activation techniques [56] for smear layer removal in the final irrigation protocol promoted the dentinal tubule penetration of iRoot SP. iRoot SP and Endoseal MTA showed better adhesion to root dentin than AH Plus [62]. Inconsistent findings regarding the dentinal tubule penetration were published for BioRoot RCS. Whilst one study found a higher dentinal tubule penetration compared to an epoxy resin-based sealer [63], less dentinal tubule penetration of BioRoot RCS was reported in other studies [24, 64]. Temporary intracanal dressing with calcium hydroxide decreased the dentinal tubule penetration of BioRoot RCS [63]. Superior dentinal tubule penetration of Endoseal MTA compared to BioRoot RCS and AH Plus was found [24]. Enhanced mineralization of the root dentin beyond the sealer tags inside dentinal tubules was proven for Endoseal MTA [65] and the presence of phosphate buffered saline (PBS) even enhanced this mineralization effect [65].
Leakage/Sealing
Lesser dye leakage was reported for iRoot SP compared to AH Plus [66, 67]. The combination of iRoot SP with CPoints (polymer obturation cone with expanding ability after water sorption) (Endodontic Innovations Ltd., St. Austell, UK) resulted in lesser apical dye leakage than when combined with conventional gutta-percha single cones [68]. No difference for apical leakage was found between iRoot SP and AH Plus by fluid filtration methods in several studies [46, 69], whereas two studies reported higher apical leakage for iRoot SP compared to AH Plus [70, 71]. Investigated by fluid filtration method, iRoot SP provided a better sealing ability than MTA Fillapex [72]. The sealing ability of iRoot SP was stable over a 3-month period [72]. Even a better sealing ability than MTA against bacterial leakage over a 3-month period was reported [73]. When using either conventional or bioceramic impregnated gutta-percha points, a similar bacterial leakage of Enterococcus faecalis was found after obturation with iRoot SP compared to AH Plus [74]. Regarding endotoxine leakage, iRoot SP was associated with a significantly higher leakage compared to AH 26 (Dentsply Sirona) after a 21-day incubation period [75]. Similar bacterial leakage of Endoseal MTA with single-cone obturation and AH Plus with warm vertical compaction was reported [76]. Obturation using Endo CPM caused significantly higher dye leakage compared to Sealapex (Kerr, Orange, USA) [77], MTA Fillapex [77] or AH 26 [78] and was also associated with significantly higher bacterial leakage of E. faecalis compared to AH Plus [79, 80].
Filling quality
A lesser amount of void areas inside the sealer and less gap regions at the root canal wall were found for iRoot SP compared to the epoxy resin-based sealer AH Plus [57]. Contradictorily, other studies reported comparable amounts of pores after obturation with iRoot SP compared to epoxy resin-based sealers [81,82,83,84], or even more and greater gaps in the apical third of the root canal [60, 85]. iRoot SP also showed higher film thickness inside the root canal after obturation using the cold lateral compaction technique [85]. A higher void volume was related to BioRoot RCS compared to AH Plus in a micro-CT analysis [86] and via confocal laser scanning microscopy [64]. A SEM analysis revealed a poor adaption to the root canal wall for Endo CPM [42].
Regarding obturation of artificial lateral canals with the single-cone technique, iRoot SP insufficiently filled these accessory canals, whilst AH Plus sealed these canals well [87]. When using the single-cone technique, the use of bioceramic impregnated gutta-percha points resulted in more gaps inside the iRoot SP sealer phase compared to conventional gutta-percha cones [88]. A higher amount of voids was found in Endoseal MTA used with single-cone technique compared to AH Plus used with the warm vertical compaction technique [89], which might be a consequence of the different techniques used. Heating BioRoot RCS up to 250 °C for 11 min to simulate the effect of warm vertical compaction techniques resulted in a weight loss of 15% of BioRoot RCS [32].
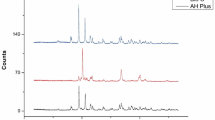
Push-out bond strength (POBS)
Higher POBS was reported for iRoot SP (Fig. 2) compared to epoxy resin-based sealers [90,91,92] when used with single-cone technique and the POBS of iRoot SP increased over a 3-month period at 37 °C and 100% humidity [93]. When used in combination with the lateral compaction technique, lower POBS of iRoot SP was found compared to AH Plus [94] in one study, whereas no differences occurred in another study [95]. After immersion in simulated body fluid [26] or at 100% humidity [96] for 30 days, the POBS of iRoot SP was lower than that of AH Plus. Moderate moist conditions inside the root canal prior to obturation improved the POBS of iRoot SP [90, 97,98,99] at incubation times of 7–30 days. Contrarily, the POBS of iRoot SP was not influenced by the degree of canal dryness in another study [100]. After a 6-week period of incubation, remoistening the root canal prior to obturation did not influence the POBS of iRoot SP when used in combination with the lateral compaction technique anymore [97]. The POBS of iRoot SP was comparable to those of AH Plus, either with the use of bioceramic-coated or conventional gutta-percha [93] points after single-cone obturation. Also the obturation without a core material resulted in the same POBS like the obturation of iRoot SP with gutta-percha [101]. In another study, the use of glass ionomer-impregnated gutta-percha (Activ GP, Brasseler) or experimental apatite phosphate-coated gutta-percha points did not significantly improve the POBS of iRoot SP compared to conventional gutta-percha [102]. Contrarily, the use of CPoints and iRoot SP with single-cone obturation resulted in higher POBS in oval canals than AH Plus and gutta-percha used according to the lateral compaction technique [103].
A negative effect on the POBS was found for iRoot SP when used according to the continuous wave technique compared to the single-cone technique [104] or the cold lateral compaction [21]. When used with warm vertical compaction, the POBS of iRoot SP was significantly lower than that of AH Plus after 30 days of incubation [105], which was also the case when no core material was used for obturation [106, 107]. However, another study failed to show any differences between iRoot SP and AH Plus when used without a core material [108]. After immersion in PBS for 30 days, lower POBS of iRoot SP compared to AH Plus after obturation without a core material was reported [109]. Irrigation with NaOCl [106] or EDTA [106] was reported to increase the POBS of iRoot SP while another study reported no such effect for EDTA [110]. The combination of different neutralizing irrigation solutions (NaOCl, chlorhexidine, saline) after EDTA did not affect the POBs of iRoot SP compared to irrigation with EDTA only [111]. The removal of smear layer with an Er:YAG laser increased POBS of iRoot SP [106]. Calcium hydroxide remnants were reported to lower the POBS of iRoot SP in one study [112], whereas in another study temporary intracanal calcium hydroxide dressing increased the POBS of iRoot SP [96]. In other studies, intracanal dressing with either calcium hydroxide or double antibiotic paste exerted no impact on the POBS of iRoot SP [92, 113], whereas a dressing with triple antibiotic paste increased the POBS of iRoot SP [113]. Chlorhexidine (CHX) remnants reduced the POBS of iRoot SP [100].
The POBS of BioRoot RCS (Fig. 2) was inferior compared to AH Plus when used according the single-cone technique [114, 115]. The use of EDTA as a final irrigant had an adverse impact on the POBS of BioRoot RCS, whereas CHX enhanced the dislodgement resistance [115].
Endoseal MTA was reported with lower POBS than AH Plus [116]. The POBS of Endo CPM (Fig. 2) was lower compared to AH Plus or BioRoot RCS after single-cone obturation in one study [114], whereas in another study the POBS of Endo CPM was higher than that of AH Plus when lateral compaction was used for obturation [117].
Tooth discoloration
It is well known from hydraulic calcium silicate cements that they may lead to discoloration of the hard tooth substance, which is of clinical relevance especially in anterior teeth, e.g., after dental trauma [118]. Causal are containing heavy metals such as bismuth oxide used as radiopacifier [119, 120] or iron [121]. The oxidation of these metals after contact with sodium hypochlorite or the uptake of blood components may play a role [121,122,123].
Regarding calcium silicate-based sealers, there are only few publications concerning tooth discoloration. In case iRoot SP was used for obturation, tooth discoloration was comparable to AH Plus in an in vitro study over a 6-month period [124]. The same results were found for Endoseal MTA in an in vitro study over a 2-month period [125]. It may be speculated that sealers without bismuth oxide and other heavy metals may show less tooth discoloration in long-term observation.
Post-endodontic characteristics
Root canal obturation with iRoot SP as sealer increased the fracture resistance of canal-filled roots with comparable fracture resistance like teeth obturated with AH Plus [126,127,128]. The fracture resistance of iRoot SP-obturated teeth was higher than the fracture resistance of iRoot canals were only filled with a temporary calcium hydroxide dressing [51]. Regarding the fracture resistance of human premolars, no difference in the fracture resistance occurred when the canals were filled with either AH Plus or iRoot SP [129]. Several studies confirmed even higher fracture resistance following canal obturation using iRoot SP compared to AH Plus [130, 131], to the calcium hydroxide-based sealer Apexit (Ivoclar Vivadent, Ellwangen, Germany) [131] or to a glass ionomer-based sealer [132]. Contradictorily, according to another study, roots filled with iRoot SP showed lower fracture resistance than roots filled with a glass ionomer-based sealer [133]. Dentin microhardness was not affected by iRoot SP [134]. Different irrigation regimes exerted no impact on the fracture resistance of roots obturated with iRoot SP [135].
iRoot SP did not adversely affect the bond strength of fiber posts inserted with a self-adhesive resin luting material in one study [136]. Contrarily, lower push-out bond strength of adhesively bonded fiber posts was reported twice after the use of iRoot SP compared to AH Plus [137, 138]. Furthermore, the removal of iRoot SP was more difficult than that of AH Plus during post-space preparation with or without activation of the irrigants [139].
Retreatment
Higher amounts of residual filling material after retreatment were found for iRoot SP compared to an epoxy resin-based [140] or a zinc oxide–eugenol-based sealer [141]. In a micro-CT study, iRoot SP showed significantly more sealer remnants than AH Plus regardless of whether or not chloroform was used as a solvent during the retreatment using engine-driven nickel–titanium (NiTi) instruments [142]. No difference was found for AH Plus and iRoot SP regarding remaining filling material after rotary or manual retreatment in other studies [59, 143, 144]. The use of laser-activated photon-induced photoacoustic streaming (PIPS) improved the removal of iRoot SP [144]. Regarding the time needed to regain working length during the retreatment process, no differences were found between iRoot SP and epoxy resin-based sealers in several studies [59, 140, 145], whereas according to two studies more time was required to remove iRoot SP than AH Plus [146, 147]. Similar results were obtained in a further study in as far as the removal of iRoot SP was more time consuming than removal of a zinc oxide eugenol-based sealer when using NiTi files [141].
Regarding the retreatment of BioRoot RCS and Endo CPM, only one study has been published yet. Compared to an epoxy resin-based sealer, less sealer remnants and less retreatment time were reported both with manual or rotary NiTi instrumentation [148].
Highlights of dentinal interaction
-
CSBS mostly presented leakage compared to epoxy resin-based sealers.
-
No relevant tooth discoloration was reported for CSBS.
-
Deeper dentinal tubule penetration, higher push-out bond strength compared to other CSBS and higher resistance to fracture compared to canal obturation using epoxy resin-based sealers were published for iRoot SP.
-
CSBS predominantly presented a higher void volume in obturation compared to epoxy resin-based sealers.
-
Retreatment of CSBS is possible, but impeded removal of CSBS was reported in some studies.
Biological characteristics
Antibacterial effect
iRoot SP showed a more pronounced antibacterial effect than an epoxy resin-based sealer and a comparable effect alike MTA [149]. An antibacterial effect against E. faecalis [150], Escherichia coli [151], Lactobacillus [151], Pseudomonas aeruginosa [151], Staphylococcus aureus [150, 151] and antifungal activity against Candida albicans [151, 152] have been found for iRoot SP, but its antimicrobial effect against Candida albicans and S. aureus was inferior compared to AH Plus [150]. Even against E. faecalis, iRoot SP exerted a pronounced antibacterial effect directly after mixing and continued to be an antibacterial for a 7-day period [153], whereas another study failed to corroborate the antibacterial effect of iRoot SP against E. faecalis [154]. One hour after mixing, the antibacterial effect of iRoot SP was inferior to AH Plus, but reached the same level after 24 h [155]. In a direct contact test, iRoot SP showed a pronounced antibacterial activity after 6, 15 and 60 min of contact time [48]. These findings are in accordance with another investigation that found similar antibacterial effects inside dentinal tubules for iRoot SP and AH Plus [156].
Both BioRoot RCS and iRoot SP showed a more pronounced antibacterial activity on E. faecalis than AH Plus in a direct contact test [48]. However, compared to iRoot SP, the antibacterial activity of BioRoot RCS was lower in a direct contact test after 6 min but equal after 15 min and 60 min [48]. An inhibition zone was reported for BioRoot RCS in agar diffusion test, whereas no such zone was found for iRoot SP [48]. The antibacterial effect on E. faecalis inside dentinal tubules was more pronounced for BioRoot RCS than for AH Plus [157].
Endo CPM exerted an antimicrobial effect against E. faecalis, S. aureus, P. aeruginosa, Micrococcus luteus and Candida albicans in agar diffusion tests [158], while no antibacterial effect against E. faecalis in a direct contact test was detected [54].
Cytotoxicity and bioactivity
Good biocompatibility was reported for iRoot SP [159] with a relatively high presence of macrophages after subcutaneous implantation in rats [160]. iRoot SP was found to be non-cytotoxic on periodontal ligament (PDL) fibroblasts [154, 161,162,163,164] and with an acceptable cytocompatibility on human fibroblasts [48, 165,166,167]. Moreover, iRoot SP did not exert marked toxic effect on mouse fibroblasts [168], and its cytotoxicity was lower compared to AH Plus [169], to MTA Fillapex [170, 171] or to a zinc oxide–eugenol-based sealer [171, 172]. iRoot SP was associated with low expression of pro-inflammatory mediators after contact with human PDL cells and good osteogenic potential [161]. Also the genotoxicity on PDL cells of iRoot SP was found to be low [162]. After a direct contact with gingival fibroblasts, the use of iRoot SP was associated with higher number of viable cells and lesser micronucleus formation (genotoxicity) compared to AH Plus [155], while on the contrary another study reported comparable cytotoxicity of iRoot SP and AH Plus on human tooth germ stem cells [173]. In MTT assay, iRoot SP was found to be non-toxic on human osteoblast-like cells [174] and showed only moderate cytotoxicity on mouse osteoblasts over a 6-week period [45]. Compared to AH Plus, lesser cytotoxicity of iRoot SP on mouse fibroblasts [175] and on human bone marrow cells was reported [176], which is in line with other investigations in which iRoot SP caused a lesser toxic response [177], a reduction of calcitonin gene-related peptide release [178] and, therefore, lesser activation of nociceptors [178] in rat trigeminal ganglion neurons than AH Plus.
iRoot SP showed good biocompatibility in contact with macrophages, induced polarization of the macrophages [179] and promoted the release of pro-inflammatory cytokines in macrophages in the presence of lipopolysaccharide (LPS) comparable to MTA [180]. After the contact of iRoot SP with human tooth germ stem cells, differentiation into odontoblast-like cells occurred [181]. Furthermore, in the presence of iRoot SP, human osteoblast-like cells produced more mineralized matrix gene and protein expression compared to AH Plus [174]. In a dog study, significantly better healing of periapical tissues was observed for iRoot SP after a 3-month period compared to a calcium hydroxide-based sealer [182].
BioRoot RCS showed low toxicity and genotoxicity on PDL cells [162, 163], and proved to be biocompatible on human PDL cells [183] and gingival fibroblasts [48, 167]. In another study, however, BioRoot RCS was toxic on gingival fibroblasts after 1 and 28 days of exposure [10]. On the other hand, BioRoot RCS was less cytotoxic than an epoxy resin-based sealer on fibroblasts [184] and less cytotoxic on human PDL cells than a zinc oxide–eugenol-based sealer [185]. Biocompatibility and bioactivity of BioRoot RCS on human pulp stem cells have been reported [186], and the cytotoxicity on human bone marrow cells of this sealer was less pronounced compared to AH Plus [176]. This sealer induced a higher secretion of angiogenic and osteogenic growth factors compared to a zinc oxide-eugenol sealer [185]. These findings are in agreement with the results of other investigations in as far as BioRoot RCS was biocompatible on human osteoblast and positively influenced their cell metabolism (bioactivity) [187].
Endoseal MTA exerted inferior biocompatibility compared to BioRoot RCS on human PDL cells [188]. Endoseal MTA did not promote the growth of gingival fibroblasts on its surface, whereas this was observed for BioRoot RCS [24]. Endoseal MTA showed stable cell activity of gingival fibroblast after 1 day and 28 days of exposure [10], and better biocompatibility than AH Plus on mouse osteoblast precursor cells [39].
Subcutaneous implantation of Endo CPM in rats resulted in similar tissue reactions as implantation of MTA after 30 days [189] and a stimulated mineralization [190]. Therefore, this sealer was found to be biocompatible [190]. Endo CPM was considered non-cytotoxic on mouse fibroblasts [191]. Perforation treatment with Endo CPM in rat molars showed results similar to MTA after a 60-day period [192]. Contrarily, a histological study in dogs found only an incomplete healing of periapical lesions after 6 months following root canal obturation using Endo CPM [193].
The bioactive potential of CSBS is a consequence of the slight solubility of these materials even after setting. The leaching of calcium hydroxide and the alkalizing potential cause antibacterial and anti-inflammatory effects inducing apical healing [2], and allow the formation of bioactive surfaces on CSBS [27]. Thus, solubility of CSBS seems to be a prerequisite for the positive biological characteristics of these sealers, but on the other hand, solubility of the sealer is compromising the quality of sealing a root canal against regrowth of microorganisms and reinfection. The ISO specification, therefore, demands low solubility with less than 3% of weight loss after immersion in water for 24 h to ensure a durable seal of the root canal system. CSBS have to walk a tightrope between bioactivity on the one and solubility on the other hand. Clinical investigations are much-needed to evaluate the clinical relevance of these factors.
Highlights of biological characteristics
-
CSBS were consistently reported to be biocompatible, non-cytotoxic and non-genotoxic.
-
CSBS display bioactivity with a stimulus to hard tissue formation.
-
Good antibacterial properties, predominantly superior to epoxy resin sealers, were related to CSBS.
Clinical studies
Studies assessing the impact of CSBS on clinical outcome are sparse. Only two studies are available yet (Fig. 3).
Postoperative pain
In a split-mouth randomized controlled trial including 114 teeth, no significant difference regarding postoperative pain was found comparing root canal obturation with either the epoxy resin-based sealer AH Plus or the CSBS iRoot SP [194].
Clinical outcome
A retrospective cohort study investigated the clinical outcome of non-surgical root canal treatment with single-cone gutta-percha obturation and iRoot SP as a sealer. A total of 307 teeth were included with an average follow-up of 30.1 months. The overall success rate was 90.9% [195]. In the same study, sealer extrusion of iRoot SP occurred in 47.4% of the cases and did not significantly affect the treatment outcome [195].
Conclusion and consequences for clinical practice
Much promising in vitro data are currently available for the CSBS iRoot SP, BioRoot RCS, Endo CPM and Endoseal MTA. The majority of in vitro studies are dealing with iRoot SP whilst lesser amount of data exists for the other CSBS. The in vitro results for CSBS mostly display characteristics comparable or in parts even superior to the gold standard AH Plus. When considering the in vitro data, the concept transformation from using endodontic sealers mainly to seal the root canal as prevention against regrowth or reinfection as known from epoxy resin sealers as the current gold standard to a more biological concept becomes clear. CSBS have in addition to their sealing abilities the potential to provide a bioactive surface with a stimulation of hard tissue formation, good antibacterial properties and perform well in the yet-published clinical studies. Therefore, the use of CSBS can be recommended to clinicians and CSBS might display the most important sealer class in the next years.
However, still relevant information for CSBS is missing in the literature, for example, studies concerning the properties of CSBS in warm obturation techniques as the CSBS are mostly recommended for cold obturation techniques by the manufacturers. Furthermore, long-term assessment of physicochemical properties and particularly long-term clinical observations are necessary to evaluate the impact of CSBS on the outcome of root canal treatment.
References
Parirokh M, Torabinejad M, Dummer PMH. Mineral trioxide aggregate and other bioactive endodontic cements: an updated overview—part I: vital pulp therapy. Int Endod J. 2018;51:177–205.
Torabinejad M, Parirokh M, Dummer PMH. Mineral trioxide aggregate and other bioactive endodontic cements: an updated overview—part II: other clinical applications and complications. Int Endod J. 2018;51:284–317.
Thrivikraman G, Madras G, Basu B. In vitro/in vivo assessment and mechanisms of toxicity of bioceramic materials and its wear particulates. RSC Adv. 2014;4:12763–81.
Raghavendra SS, Jadhav GR, Gathani KM, Kotadia P. Bioceramics in endodontics—a review. J Istanb Univ Fac Dent. 2017;51:128–37.
de Oliveira NG, de Souza Araújo PR, da Silveira MT, Veras Sobral AP, Carvalho MV. Comparison of the biocompatibility of calcium silicate-based materials to mineral trioxide aggregate: systematic review. Eur J Dent. 2018;12:317–26.
Nasseh A. The rise of bioceramics. Endod Pract US. 2009;2:17–22.
Koch K, Brave D, Ali Nasseh A. A review of bioceramic technology in endodontics. Roots. 2013;1:10–3.
Al-Haddad A, Ab Aziz C, Zeti A. Bioceramic-based root canal sealers: a review. Int J Biomater. 2016;2016:9753210.
Berzins DW. Chemical properties of MTA. In: Torabinejad M, editor. Mineral trioxide aggregate—properties and clinical applications. 1st ed. Ames: Wiley Blackwell; 2014. pp. 17–36.
Kebudi Benezra M, Schembri Wismayer P, Camilleri J. Influence of environment on testing of hydraulic sealers. Sci Rep. 2017;7:17927.
Prati C, Siboni F, Polimeni A, Bossu M, Gandolfi MG. Use of calcium-containing endodontic sealers as apical barrier in fluid-contaminated wide-open apices. J Appl Biomater Funct Mater. 2014;12:263–70.
Camilleri J, Laurent P, About I. Hydration of biodentine, theracal LC, and a prototype tricalcium silicate-based dentin replacement material after pulp capping in entire tooth cultures. J Endod. 2014;40:1846–54.
Wang Z, Shen Y, Haapasalo M. Dental materials with antibiofilm properties. Dent Mater. 2014;30:e1–16.
Prati C, Gandolfi MG. Calcium silicate bioactive cements: biological perspectives and clinical applications. Dent Mater. 2015;31:351–70.
Jitaru S, Hodisan I, Timis L, Lucian A, Bud M. The use of bioceramics in endodontics—literature review. Clujul Med. 2016;89:470–3.
Tour Savadkouhi S, Fazlyab M. Discoloration potential of endodontic sealers: a brief review. Iran Endod J. 2016;11:250–4.
Silva Almeida LH, Moraes RR, Morgental RD, Pappen FG. Are premixed calcium silicate-based endodontic sealers comparable to conventional materials? A systematic review of in vitro studies. J Endod. 2017;43:527–35.
Jafari F, Jafari S. Composition and physicochemical properties of calcium silicate based sealers: a review article. J Clin Exp Dent. 2017;9:e1249–e1255.
Jafari F, Jafari S, Etesamnia P. Genotoxicity, bioactivity and clinical properties of calcium silicate based sealers: a literature review. Iran Endod J. 2017;12:407–13.
Uzunoglu-Özyürek E, Küçükkaya Eren S, Karahan S. Effect of root canal sealers on the fracture resistance of endodontically treated teeth: a systematic review of in vitro studies. Clin Oral Investig. 2018;22:2475–85.
Dabaj P, Kalender A, Unverdi Eldeniz A. Push-out bond strength and SEM evaluation in roots filled with two different techniques using new and conventional sealers. Materials (Basel). 2018;11:E1620.
Donnermeyer D, Schäfer E, Bürklein S. Real-time intracanal temperature measurement during different obturation techniques. J Endod. 2018;44:1832–6
Gandolfi MG, Van Landuyt K, Taddei P, Modena E, VanMeerbeek B, Prati C. Environmental scanning electron microscopy connected with energy dispersive X-ray analysis and Raman techniques to study ProRoot MTA and calcium–silicate cements in wet conditions and in real-time. J Endod. 2010;36:851–7.
Kebudi Benezra M, Schembri Wismayer P, Camilleri J. Interfacial characteristics and cytocompatibility of hydraulic sealer cements. J Endod. 2018;44:1007–17.
Zamparini F, Siboni F, Prati C, Taddei P, Gandolfi MG. Properties of calcium silicate-monobasic calcium phosphate materials for endodontics containing tantalum pentoxide and zirconium oxide. Clin Oral Investig. 2018. https://doi.org/10.1007/s00784-018-2453-7 (epub ahead of print).
Carvalho CN, Grazziotin-Soares R, de Miranda Candeiro GT, Gallego Martinez L, de Souza JP, Santos Oliveira P, Bauer J, Gavini G. Micro Push-out Bond Strength and bioactivity analysis of a bioceramic root canal sealer. Iran Endod J. 2017;12:343–8.
Prüllage RK, Urban K, Schäfer E, Dammaschke T. Material properties of a tricalcium silicate-containing, a mineral trioxide aggregate-containing, and an epoxy resin-based root canal sealer. J Endod. 2016;42:1784–8.
Camilleri J, Kralj P, Veber M, Sinagra E. Characterization and analyses of acid-extractable and leached trace elements in dental cements. Int Endod J. 2012;45:737–43.
Reszka P, Nowicka A, Lipski M, Dura W, Droździk A, Woźniak K. A Comparative chemical study of calcium silicate-containing and epoxy resin-based root canal sealers. Biomed Res Int. 2016;2016:9808432.
Han L, Okiji T. Bioactivity evaluation of three calcium silicate-based endodontic materials. Int Endod J. 2013;46:808–14.
Borges RP, Sousa-Neto MD, Versiani MA, Rached-Júnior FA, De-Deus G, Miranda CE, Pécora JD. Changes in the surface of four calcium silicate-containing endodontic materials and an epoxy resin-based sealer after a solubility test. Int Endod J. 2012;45:419–28.
Atmeh AR, AlShwaimi E. The effect of heating time and temperature on epoxy resin and calcium silicate-based endodontic sealers. J Endod. 2017;43:2112–8.
Candeiro GT, Correia FC, Duarte MA, Ribeiro-Siqueira DC, Gavini G. Evaluation of radiopacity, pH, release of calcium ions, and flow of a bioceramic root canal sealer. J Endod. 2012;38:842–5.
Hrab D, Chisnoiu AM, Badea ME, Moldovan M, Chisnoiu RM. Comparative radiographic assessment of a new bioceramic-based root canal sealer. Clujul Med. 2017;90:226–30.
Lee JK, Kwak SW, Ha JH, Lee W, Kim HC. Physicochemical properties of epoxy resin-based and bioceramic-based root canal sealers. Bioinorg Chem Appl. 2017;2017:2582849.
Tanomaru-Filho M, Torres FFE, Chávez-Andrade GM, de Almeida M, Navarro LG, Steier L, Guerreiro-Tanomaru JM. Physicochemical properties and volumetric change of silicone/bioactive glass and calcium silicate-based endodontic sealers. J Endod. 2017;43:2097–101.
Khalil I, Naaman A, Camilleri J. Properties of tricalcium silicate sealers. J Endod. 2016;42:1529–35.
Siboni F, Taddei P, Zamparini F, Prati C, Gandolfi MG. Properties of BioRoot RCS, a tricalcium silicate endodontic sealer modified with povidone and polycarboxylate. Int Endod J. 2017;50(Suppl 2):e120-36.
Lim ES, Park YB, Kwon YS, Shon WJ, Lee KW, Min KS. Physical properties and biocompatibility of an injectable calcium-silicate-based root canal sealer: in vitro and in vivo study. BMC Oral Health. 2015;15:129.
Guerreiro-Tanomaru JM, Duarte MA, Gonçalves M, Tanomaru-Filho M. Radiopacity evaluation of root canal sealers containing calcium hydroxide and MTA. Braz Oral Res. 2009;23:119–23.
Tanomaru-Filho M, Bosso R, Viapiana R, Guerreiro-Tanomaru JM. Radiopacity and flow of different endodontic sealers. Acta Odontol Latinoam. 2013;26:121–5.
Cañadas PS, Berástegui E, Gaton-Hernández P, Silva LA, Leite GA, Silva RS. Physicochemical properties and interfacial adaptation of root canal sealers. Braz Dent J. 2014;25:435–41.
Zhou HM, Shen Y, Zheng W, Li L, Zheng YF, Haapasalo M. Physical properties of 5 root canal sealers. J Endod. 2013;39:1281–6.
Qu W, Bai W, Liang YH, Gao XJ. Influence of warm vertical compaction technique on physical properties of root canal sealers. J Endod. 2016;42:1829–33.
Loushine BA, Bryan TE, Looney SW, Gillen BM, Loushine RJ, Weller RN, Pashley DH, Tay FR. Setting properties and cytotoxicity evaluation of a premixed bioceramic root canal sealer. J Endod. 2011;37:673–7.
Ersahan S, Aydin C. Solubility and apical sealing characteristics of a new calcium silicate-based root canal sealer in comparison to calcium hydroxide-, methacrylate resin- and epoxy resin-based sealers. Acta Odontol Scand. 2013;71:857–62.
Poggio C, Dagna A, Ceci M, Meravini MV, Colombo M, Pietrocola G. Solubility and pH of bioceramic root canal sealers: a comparative study. J Clin Exp Dent. 2017;9:e1189-94.
Colombo M, Poggio C, Dagna A, Meravini MV, Riva P, Trovati F, Pietrocola G. Biological and physico-chemical properties of new root canal sealers. J Clin Exp Dent. 2018;10:e120-6.
Urban K, Neuhaus J, Donnermeyer D, Schäfer E, Dammaschke T. Solubility and pH value of 3 different root canal sealers: a long-term investigation. J Endod. 2018. https://doi.org/10.1016/j.joen.2018.07.026 (epub ahead of print).
Yang DK, Kim S, Park JW, Kim E, Shin SJ. Different setting conditions affect surface characteristics and microhardness of calcium silicate-based sealers. Scanning. 2018;2018:7136345.
Dudeja C, Taneja S, Kumari M, Singh N. An in vitro comparison of effect on fracture strength, pH and calcium ion diffusion from various biomimetic materials when used for repair of simulated root resorption defects. J Conserv Dent. 2015;18:279–83.
Tanomaru-Filho M, Chaves Faleiros FB, Saçaki JN, Hungaro Duarte MA, Guerreiro-Tanomaru JM. Evaluation of pH and calcium ion release of root-end filling materials containing calcium hydroxide or mineral trioxide aggregate. J Endod. 2009;35:1418–21.
Xuereb M, Vella P, Damidot D, Sammut CV, Camilleri J. In situ assessment of the setting of tricalcium silicate-based sealers using a dentin pressure model. J Endod. 2015;41:111–24.
Morgental RD, Vier-Pelisser FV, Oliveira SD, Antunes FC, Cogo DM, Kopper PM. Antibacterial activity of two MTA-based root canal sealers. Int Endod J. 2011;44:1128–33.
McMichael GE, Primus CM, Opperman LA. Dentinal tubule penetration of tricalcium silicate sealers. J Endod. 2016;42:632–6.
Akcay M, Arslan H, Durmus N, Mese M, Capar ID. Dentinal tubule penetration of AH Plus, iRoot SP, MTA fillapex, and Guttaflow Bioseal root canal sealers after different final irrigation procedures: a confocal microscopic study. Lasers Surg Med. 2016;48:70–6.
Wang Y, Liu S, Dong Y. In vitro study of dentinal tubule penetration and filling quality of bioceramic sealer. PLoS One. 2018;13:e0192248.
Jardim Del Monaco R, Tavares de Oliveira M, Lima AF, Scarparo Navarro R, Zanetti RV, de Fátima Teixeira da Silva D, Horliana ACRT. Influence of Nd:YAG laser on the penetration of a bioceramic root canal sealer into dentinal tubules: a confocal analysis. PLoS One. 2018;13:e0202295.
Kim H, Kim E, Lee SJ, Shin SJ. Comparisons of the retreatment efficacy of calcium silicate and epoxy resin-based sealers and residual sealer in dentinal tubules. J Endod. 2015;41:2025–30.
Chen H, Zhao X, Qiu Y, Xu D, Cui L, Wu B. The tubular penetration depth and adaption of four sealers: a scanning electron microscopic study. Biomed Res Int. 2017;2017:2946524.
Aydın ZU, Özyürek T, Keskin B, Baran T. Effect of chitosan nanoparticle, QMix, and EDTA on TotalFill BC sealers’ dentinal tubule penetration: a confocal laser scanning microscopy study. Odontology. 2018. https://doi.org/10.1007/s10266-018-0359-0 (epub ahead of print).
Ha JH, Kim HC, Kim YK, Kwon TY. An evaluation of wetting and adhesion of three bioceramic root canal sealers to intraradicular human dentin. Materials (Basel). 2018;11:E1286.
Uzunoglu-Özyürek E, Erdoğan Ö, Aktemur Türker S. Effect of calcium hydroxide dressing on the dentinal tubule penetration of 2 different root canal sealers: a confocal laser scanning microscopic study. J Endod. 2018;44:1018–23.
Arikatla SK, Chalasani U, Mandava J, Yelisela RK. Interfacial adaptation and penetration depth of bioceramic endodontic sealers. J Conserv Dent. 2018;21:373–7.
Yoo YJ, Baek SH, Kum KY, Shon WJ, Woo KM, Lee W. Dynamic intratubular biomineralization following root canal obturation with pozzolan-based mineral trioxide aggregate sealer cement. Scanning. 2016;38:50–6.
Pawar SS, Pujar MA, Makandar SD. Evaluation of the apical sealing ability of bioceramic sealer, AH plus & epiphany: an in vitro study. J Conserv Dent. 2014;17:579–82.
Ballullaya SV, Vinay V, Thumu J, Devalla S, Bollu IP, Balla S. Stereomicroscopic dye leakage measurement of six different root canal sealers. J Clin Diagn Res. 2017;11:ZC65–8.
Sayed ME, Al Husseini MAA. H. Apical dye leakage of two single-cone root canal core materials (hydrophilic core material and gutta-percha) sealed by different types of endodontic sealers: an in vitro study. J Conserv Dent. 2018;21:147–12.
Zhang W, Li Z, Peng B. Assessment of a new root canal sealer’s apical sealing ability. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:e79–82.
Ulusoy OI, Nayir Y, Celik K, Yaman SD. Apical microleakage of different root canal sealers after use of maleic acid and EDTA as final irrigants. Braz Oral Res. 2014;28:1–6.
Deniz Sungur D, Moinzadeh AT, Wesselink PR, Çalt Tarhan S, Özok AR. Sealing efficacy of a single-cone root filling after post space preparation. Clin Oral Investig. 2016;20:1071–7.
Bidar M, Sadeghalhoseini N, Forghani M, Attaran N.. Effect of the smear layer on apical seals produced by two calcium silicate-based endodontic sealers. J Oral Sci. 2014;56:215–9.
Gandhi B, Halebathi-Gowdra R.. Comparative evaluation of the apical sealing ability of a ceramic based sealer and MTA as root-end filling materials—an in-vitro study. J Clin Exp Dent. 2017;9:e901-5.
Yanpiset K, Banomyong D, Chotvorrarak K, Srisatjaluk RL. Bacterial leakage and micro-computed tomography evaluation in round-shaped canals obturated with bioceramic cone and sealer using matched single cone technique. Restor Dent Endod. 2018;43:e30.
Oh S, Cho SI, Perinpanayagam H, You J, Hong SH, Yoo YJ, Chang SW, Shon WJ, Yoo JS, Baek SH, Kum KY. Novel calcium zirconate silicate cement biomineralize and seal root canals. Materials (Basel). 2018;11:E588.
Hwang JH, Chung J, Na HS, Park E, Kwak S, Kim HC. Comparison of bacterial leakage resistance of various root canal filling materials and methods: confocal laser-scanning microscope study. Scanning. 2015;37:422–8.
Gomes-Filho JE, Moreira JV, Watanabe S, Lodi CS, Cintra LT, Dezan Junior E, Bernabé PF, Nery MJ, Otoboni Filho JA. Sealability of MTA and calcium hydroxide containing sealers. J Appl Oral Sci. 2012;20:347–51.
Tanomaru-Filho M, Faleiros FB, Silva GF, Bosso R, Guerreiro-Tanomaru JM. Sealing ability of retrograde obturation materials containing calcium hydroxide or MTA. Acta Odontol Latinoam. 2011;24:110–4.
Bortolini MC, Ferreira dos Santos SS, Habitante SM, Rodrigues JR, Vance R, Jorge AO. Endodontic sealers: intratubular penetration and permeability to Enterococcus faecalis. Indian J Dent Res. 2010;21:40–3.
Oliveira AC, Tanomaru JM, Faria-Junior N, Tanomaru-Filho M.. Bacterial leakage in root canals filled with conventional and MTA-based sealers. Int Endod J. 2011;44:370–5.
Polineni S, Bolla N, Mandava P, Vemuri S, Mallela M, Gandham VM. Marginal adaptation of newer root canal sealers to dentin: a SEM study. J Conserv Dent. 2016;19:360–3.
Huang Y, Orhan K, Celikten B, Orhan AI, Tufenkci P, Sevimay S. Evaluation of the sealing ability of different root canal sealers: a combined SEM and micro-CT study. J Appl Oral Sci. 2018;26:e20160584.
Germain S, Meetu K, Issam K, Alfred N, Carla Z. Impact of the root canal taper on the apical adaptability of sealers used in a single-cone technique: a micro-computed tomography study. J Contemp Dent Pract. 2018;19:808–15.
Celikten B, Uzuntas CF, Orhan AI, Orhan K, Tufenkci P, Kursun S, Demiralp K. Evaluation of root canal sealer filling quality using a single-cone technique in oval shaped canals: an in vitro Micro-CT study. Scanning. 2016;38:133–40.
Al-Haddad A, Abu Kasim NH, Che Ab Aziz ZA. Interfacial adaptation and thickness of bioceramic-based root canal sealers. Dent Mater J. 2015;34:516–21.
Viapiana R, Moinzadeh AT, Camilleri L, Wesselink PR, Tanomaru Filho M, Camilleri J. Porosity and sealing ability of root fillings with gutta-percha and BioRoot RCS or AH Plus sealers. Evaluation by three ex vivo methods. Int Endod J. 2016;49:774–82.
Fernández R, Restrepo JS, Aristizábal DC, Álvarez LG. Evaluation of the filling ability of artificial lateral canals using calcium silicate-based and epoxy resin-based endodontic sealers and two gutta-percha filling techniques. Int Endod J. 2016;49:365–73.
Eltair M, Pitchika V, Hickel R, Kühnisch J, Diegritz C. Evaluation of the interface between gutta-percha and two types of sealers using scanning electron microscopy (SEM). Clin Oral Investig. 2018;22:1631–9.
Kim JA, Hwang YC, Rosa V, Yu MK, Lee KW, Min KS. Root canal filling quality of a premixed calcium silicate endodontic sealer applied using gutta-percha cone-mediated ultrasonic activation. J Endod. 2018;44:133–8.
Nagas E, Uyanik MO, Eymirli A, Cehreli ZC, Vallittu PK, Lassila LV, Durmaz V. Dentin moisture conditions affect the adhesion of root canal sealers. J Endod. 2012;38:240–4.
Madhuri GV, Varri S, Bolla N, Mandava P, Akkala LS, Shaik J. Comparison of bond strength of different endodontic sealers to root dentin: an in vitro push-out test. J Conserv Dent. 2016;19:461–4.
Gokturk H, Bayram E, Bayram HM, Aslan T, Ustun Y. Effect of double antibiotic and calcium hydroxide pastes on dislodgement resistance of an epoxy resin-based and two calcium silicate-based root canal sealers. Clin Oral Investig. 2017;21:1277–82.
Yap WY, Che Ab Aziz ZA, Azami NH, Al-Haddad AY, Khan AA. An in vitro comparison of bond strength of different sealers/obturation systems to root dentin using the push-out test at 2 weeks and 3 months after obturation. Med Princ Pract. 2017;26:464–9.
Gade VJ, Belsare LD, Patil S, Bhede R, Gade JR. Evaluation of push-out bond strength of Endosequence BC sealer with lateral condensation and thermoplasticized technique: an in vitro study. J Conserv Dent. 2015;18:124–7.
Sagsen B, Ustün Y, Demirbuga S, Pala K. Push-out bond strength of two new calcium silicate-based endodontic sealers to root canal dentine. Int Endod J. 2011;44:1088–91.
Amin SA, Seyam RS, El-Samman MA. The effect of prior calcium hydroxide intracanal placement on the bond strength of two calcium silicate-based and an epoxy resin-based endodontic sealer. J Endod. 2012;38:696–9.
Shokouhinejad N, Gorjestani H, Nasseh AA, Hoseini A, Mohammadi M, Shamshiri AR. Push-out bond strength of gutta-percha with a new bioceramic sealer in the presence or absence of smear layer. Aust Endod J. 2013;39:102–6.
Taşdemir T, Er K, Çelik D, Tahan E, Serper A, Ceyhanli KT, Yeşilyurt C. Bond strength of calcium silicate-based sealers to dentine dried with different techniques. Med Princ Pract. 2014;23:373–6.
Gritti GC, Cavalcante SIA, Maia-Filho EM, Bauer J, Bandéca MC, Gavini G, Carvalho CN. Effect of rewetting solutions on micropush-out dentin bond strength of new bioceramic endodontic material. Braz Oral Res. 2017;31:e76.
Razmi H, Bolhari B, Karamzadeh Dashti N, Fazlyab M. The effect of canal dryness on bond strength of bioceramic and epoxy-resin sealers after irrigation with sodium hypochlorite or chlorhexidine. Iran Endod J. 2016;11:129–33.
Nagas E, Cehreli Z, Uyanik MO, Durmaz V. Bond strength of a calcium silicate-based sealer tested in bulk or with different main core materials. Braz Oral Res. 2014;28:1–7 (S1806–83242014000100256).
Al-Haddad AY, Kutty MG, Che Ab Aziz ZA. Push-out bond strength of experimental apatite calcium phosphate based coated gutta-percha. Int J Biomater. 2018;2018:1731857.
Pawar AM, Pawar S, Kfir A, Pawar M, Kokate S. Push-out bond strength of root fillings made with C-Point and BC sealer versus gutta-percha and AH Plus after the instrumentation of oval canals with the self-adjusting file versus WaveOne. Int Endod J. 2016;49:374–81.
DeLong C, He J, Woodmansey KF. The effect of obturation technique on the push-out bond strength of calcium silicate sealers. J Endod. 2015;41:385–8.
Carvalho CN, Martinelli JR, Bauer J, Haapasalo M, Shen Y, Bradaschia-Correa V, Manso AP, Gavini G. Micropush-out dentine bond strength of a new gutta-percha and niobium phosphate glass composite. Int Endod J. 2015;48:451–9.
Ozkocak I, Sonat B. Evaluation of effects on the adhesion of various root canal sealers after Er:YAG laser and irrigants are used on the dentin surface. J Endod. 2015;41:1331–6.
Oliveira DS, Cardoso ML, Queiroz TF, Silva EJ, Souza EM, De-Deus G. Suboptimal push-out bond strengths of calcium silicate-based sealers. Int Endod J. 2016;49:796–801.
Ersahan S, Aydin C. Dislocation resistance of iRoot SP, a calcium silicate-based sealer, from radicular dentine. J Endod. 2010;36:2000–2.
Carvalho NK, Prado MC, Senna PM, Neves AA, Souza EM, Fidel SR, Sassone LM, Silva EJNL. Do smear-layer removal agents affect the push-out bond strength of calcium silicate-based endodontic sealers? Int Endod J. 2017;50:612–19.
Tuncel B, Nagas E, Cehreli Z, Uyanik O, Vallittu P, Lassila L. Effect of endodontic chelating solutions on the bond strength of endodontic sealers. Braz Oral Res. 2015;29:1–6 (S1806–83242015000100256).
Shokouhinejad N, Hoseini A, Gorjestani H, Shamshiri AR. The effect of different irrigation protocols for smear layer removal on bond strength of a new bioceramic sealer. Iran Endod J. 2013;8:10–3.
Ghabraei S, Bolhari B, Yaghoobnejad F, Meraji N. Effect of intra-canal calcium hydroxide remnants on the push-out bond strength of two endodontic sealers. Iran Endod J. 2017;12:168–72.
Hegde V, Arora S. Effect of intracanal medicaments on push-out bond strength of Smart-Seal system. J Conserv Dent. 2015;18:414–8.
Donnermeyer D, Dornseifer P, Schäfer E, Dammaschke T. The push-out bond strength of calcium silicate-based endodontic sealers. Head Face Med. 2018;14:13.
Donnermeyer D, Vahdat-Pajouh N, Schäfer E, Dammaschke T. Influence of the final irrigation solution on the push-out bond strength of calcium silicate-based, epoxy resin-based and silicone-based endodontic sealers. Odontology. 2018. https://doi.org/10.1007/s10266-018-0392-z (epub ahead of print).
Silva EJ, Carvalho NK, Prado MC, Zanon M, Senna PM, Souza EM, De-Deus G. Push-out bond strength of injectable pozzolan-based root canal sealer. J Endod. 2016;42:1656–9.
Assmann E, Scarparo RK, Böttcher DE, Grecca FS. Dentin bond strength of two mineral trioxide aggregate-based and one epoxy resin-based sealers. J Endod. 2012;38:219–21.
Możyńska J, Metlerski M, Lipski M, Nowicka A. Tooth discoloration induced by different calcium silicate-based cements: a systematic review of in vitro studies. J Endod. 2017;43:1593–601.
Berger T, Baratz AZ, Gutmann JL. In vitro investigations into the etiology of mineral trioxide tooth staining. J Conserv Dent. 2014;17:526–30.
Dettwiler CA, Walter M, Zaugg LK, Lenherr P, Weiger R, Krastl G. In vitro assessment of the tooth staining potential of endodontic materials in a bovine tooth model. Dent Traumatol. 2016;32:480–7.
Shokouhinejad N, Nekoofar MH, Pirmoazen S, Shamshiri AR, Dummer PM. Evaluation and comparison of occurrence of tooth discoloration after the application of various calcium silicate-based cements: an ex vivo study. J Endod. 2016;42:140–4.
Camilleri J. Color stability of white mineral trioxide aggregate in contact with hypochlorite solution. J Endod. 2014;40:436–40.
Lenherr P, Allgayer N, Weiger R, Filippi A, Attin T, Krastl G. Tooth discoloration induced by endodontic materials: a laboratory study. Int Endod J. 2012;45:942–9.
Forghani M, Gharechahi M, Karimpour S. In vitro evaluation of tooth discolouration induced by mineral trioxide aggregate Fillapex and iRoot SP endodontic sealers. Aust Endod J. 2016;42:99–103.
Lee DS, Lim MJ, Choi Y, Rosa V, Hong CU, Min KS. Tooth discoloration induced by a novel mineral trioxide aggregate-based root canal sealer. Eur J Dent. 2016;10:403–7.
Sağsen B, Ustün Y, Pala K, Demırbuğa S. Resistance to fracture of roots filled with different sealers. Dent Mater J. 2012;31:528–32.
Topçuoğlu HS, Tuncay Ö, Karataş E, Arslan H, Yeter K. In vitro fracture resistance of roots obturated with epoxy resin-based, mineral trioxide aggregate-based, and bioceramic root canal sealers. J Endod. 2013;39:1630–3.
Ulusoy Öİ, Nayır Y, Darendeliler-Yaman S. Effect of different root canal sealers on fracture strength of simulated immature roots. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:544–7.
Dibaji F, Afkhami F, Bidkhori B, Kharazifard MJ. Fracture resistance of roots after application of different sealers. Iran Endod J. 2017;12:50–4.
Hegde V, Arora S. Fracture resistance of roots obturated with novel hydrophilic obturation systems. J Conserv Dent. 2015;18:261–4.
Patil P, Banga KS, Pawar AM, Pimple S, Ganeshan R. Influence of root canal obturation using gutta-percha with three different sealers on root reinforcement of endodontically treated teeth. An in vitro comparative study of mandibular incisors. J Conserv Dent. 2017;20:241–4.
Ghoneim AG, Lutfy RA, Sabet NE, Fayyad DM. Resistance to fracture of roots obturated with novel canal-filling systems. J Endod. 2011;37:1590–2.
Celikten B, Uzuntas CF, Gulsahi K. Resistance to fracture of dental roots obturated with different materials. Biomed Res Int. 2015;2015:591031.
Khallaf ME. Effect of two contemporary root canal sealers on root canal dentin microhardness. J Clin Exp Dent. 2017;9:e67–70.
Sungur DD, Altundasar E, Uzunoglu E, Yilmaz Z. Influence of different final irrigation regimens and various endodontic filling materials on vertical root fracture resistance. Niger J Clin Pract. 2016;19:267–71.
Özcan E, Çapar İD, Çetin AR, Tunçdemir AR, Aydınbelge HA. The effect of calcium silicate-based sealer on the push-out bond strength of fibre posts. Aust Dent J. 2012;57:166–70.
Vilas-Boas DA, Grazziotin-Soares R, Ardenghi DM, Bauer J, de Souza PO, de Miranda Candeiro GT, Maia-Filho EM, Carvalho CN. Effect of different endodontic sealers and time of cementation on push-out bond strength of fiber posts. Clin Oral Investig. 2018;22:1403–9.
Dibaji F, Mohammadi E, Farid F, Mohammadian F, Sarraf P, Kharrazifard MJ. The effect of BC Sealer, AH-Plus and Dorifill on push-out bond strength of fiber post. Iran Endod J. 2017;12:443–8.
Chen X, Liu H, He Y, Luo T, Zou L. Effects of endodontic sealers and irrigation systems on smear layer removal after post space preparation. J Endod. 2018;44:1293–7.
Uzunoglu E, Yilmaz Z, Sungur DD, Altundasar E. Retreatability of root canals obturated using gutta-percha with bioceramic, mta and resin-based sealers. Iran Endod J. 2015;10:93–8.
de Siqueira Zuolo A, Zuolo ML, da Silveira Bueno CE, Chu R, Cunha RS. Evaluation of the efficacy of TRUShape and Reciproc File Systems in the removal of root filling material: an ex vivo micro-computed tomographic study. J Endod. 2016;42:315–9.
Oltra E, Cox TC, LaCourse MR, Johnson JD, Paranjpe A. Retreatability of two endodontic sealers, EndoSequence BC Sealer and AH Plus: a micro-computed tomographic comparison. Restor Dent Endod. 2017;42:19–26.
Ersev H, Yilmaz B, Dinçol ME, Dağlaroğlu R. The efficacy of ProTaper Universal rotary retreatment instrumentation to remove single gutta-percha cones cemented with several endodontic sealers. Int Endod J. 2012;45:756–62.
Suk M, Bago I, Katić M, Šnjarić D, Munitić M, Anić I. The efficacy of photon-initiated photoacoustic streaming in the removal of calcium silicate-based filling remnants from the root canal after rotary retreatment. Lasers Med Sci. 2017;32:2055–62.
Simsek N, Keles A, Ahmetoglu F, Ocak MS, Yologlu S. Comparison of different retreatment techniques and root canal sealers: a scanning electron microscopic study. Braz Oral Res. 2014;28:1–7 (S1806–83242014000100221).
Hess D, Solomon E, Spears R, He J. Retreatability of a bioceramic root canal sealing material. J Endod. 2011;37:1547–9.
Agrafioti A, Koursoumis AD, Kontakiotis EG. Re-establishing apical patency after obturation with Gutta-percha and two novel calcium silicate-based sealers. Eur J Dent. 2015;9:457–61.
Donnermeyer D, Bunne C, Schäfer E, Dammaschke T. Retreatability of three calcium silicate-containing sealers and one epoxy resin-based root canal sealer with four different root canal instruments. Clin Oral Investig. 2018;22:811–7.
Singh G, Gupta I, Elshamy FM, Boreak N, Homeida HE. In vitro comparison of antibacterial properties of bioceramic-based sealer, resin-based sealer and zinc oxide eugenol based sealer and two mineral trioxide aggregates. Eur J Dent. 2016;10:366–9.
Nirupama DN, Nainan MT, Ramaswamy R, Muralidharan S, Usha HH, Sharma R, Gupta S. In vitro evaluation of the antimicrobial efficacy of four endodontic biomaterials against Enterococcus faecalis, Candida albicans, and Staphylococcus aureus. Int J Biomater. 2014;2014:383756.
Singh G, Elshamy FM, Homeida HE, Boreak N, Gupta I. An in vitro comparison of antimicrobial activity of three endodontic sealers with different composition. J Contemp Dent Pract. 2016;1:17:553–6.
Ozcan E, Yula E, Arslanoğlu Z, Inci M. Antifungal activity of several root canal sealers against Candida albicans. Acta Odontol Scand. 2013;71:1481–5.
Zhang H, Shen Y, Ruse ND, Haapasalo M. Antibacterial activity of endodontic sealers by modified direct contact test against Enterococcus faecalis. J Endod. 2009;35:1051–5.
Willershausen I, Callaway A, Briseño B, Willershausen B. In vitro analysis of the cytotoxicity and the antimicrobial effect of four endodontic sealers. Head Face Med. 2011;7:15.
Candeiro GTM, Moura-Netto C, D’Almeida-Couto RS, Azambuja-Júnior N, Marques MM, Cai S, Gavini G. Cytotoxicity, genotoxicity and antibacterial effectiveness of a bioceramic endodontic sealer. Int Endod J. 2016;49:858–64.
Wang Z, Shen Y, Haapasalo M. Dentin extends the antibacterial effect of endodontic sealers against Enterococcus faecalis biofilms. J Endod. 2014;40:505–8.
Arias-Moliz MT, Camilleri J. The effect of the final irrigant on the antimicrobial activity of root canal sealers. J Dent. 2016;52:30–6.
Tanomaru JM, Tanomaru-Filho M, Hotta J, Watanabe E, Ito IY. Antimicrobial activity of endodontic sealers based on calcium hydroxide and MTA. Acta Odontol Latinoam. 2008;21:147–51.
Zhang W, Peng B. Tissue reactions after subcutaneous and intraosseous implantation of iRoot SP, MTA and AH Plus. Dent Mater J. 2015;34:774–80.
Bósio CC, Felippe GS, Bortoluzzi EA, Felippe MC, Felippe WT, Rivero ER. Subcutaneous connective tissue reactions to iRoot SP, mineral trioxide aggregate (MTA) Fillapex, DiaRoot BioAggregate and MTA. Int Endod J. 2014;47:667–74.
Chang SW, Lee SY, Kang SK, Kum KY, Kim EC. In vitro biocompatibility, inflammatory response, and osteogenic potential of 4 root canal sealers: Sealapex, Sankin apatite root sealer, MTA Fillapex, and iRoot SP root canal sealer. J Endod. 2014;40:1642–8.
Eldeniz AU, Shehata M, Högg C, Reichl FX. DNA double-strand breaks caused by new and contemporary endodontic sealers. Int Endod J. 2016;49:1141–51.
Taraslia V, Anastasiadou E, Lignou C, Keratiotis G, Agrafioti A, Kontakiotis EG. Assessment of cell viability in four novel endodontic sealers. Eur J Dent. 2018;12:287–91.
Rodríguez-Lozano FJ, García-Bernal D, Oñate-Sánchez RE, Ortolani-Seltenerich PS, Forner L, Moraleda JM. Evaluation of cytocompatibility of calcium silicate-based endodontic sealers and their effects on the biological responses of mesenchymal dental stem cells. Int Endod J. 2017;50:67–76.
Mukhtar-Fayyad D. Cytocompatibility of new bioceramic-based materials on human fibroblast cells (MRC-5). Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:e137-42.
Zhou HM, Du TF, Shen Y, Wang ZJ, Zheng YF, Haapasalo M. In vitro cytotoxicity of calcium silicate-containing endodontic sealers. J Endod. 2015;41:56–61.
Poggio C, Riva P, Chiesa M, Colombo M, Pietrocola G. Comparative cytotoxicity evaluation of eight root canal sealers. J Clin Exp Dent. 2017;9:e574-8.
da Silva EJNL, Zaia AA, Peters OA. Cytocompatibility of calcium silicate-based sealers in a three-dimensional cell culture model. Clin Oral Investig. 2017;21:1531–6.
Zhang W, Li Z, Peng B. Ex vivo cytotoxicity of a new calcium silicate-based canal filling material. Int Endod J. 2010;43:769–74.
Baraba A, Pezelj-Ribaric S, Roguljić M, Miletic I. Cytotoxicity of two bioactive root canal sealers. Acta Stomatol Croat. 2016;50:8–13.
Silva EJ, Carvalho NK, Ronconi CT, De-Deus G, Zuolo ML, Zaia AA. Cytotoxicity profile of endodontic sealers provided by 3d cell culture experimental model. Braz Dent J. 2016;27:652–6.
Nair AV, Nayak M, Prasada LK, Shetty V, Kumar CNV, Nair RR. Comparative evaluation of cytotoxicity and genotoxicity of two bioceramic sealers on fibroblast cell line: an in vitro study. J Contemp Dent Pract. 2018;19:656–61.
Güven EP, Yalvaç ME, Kayahan MB, Sunay H, Şahın F, Bayirli G. Human tooth germ stem cell response to calcium-silicate based endodontic cements. J Appl Oral Sci. 2013;21:351–7.
Zhang W, Li Z, Peng B. Effects of iRoot SP on mineralization-related genes expression in MG63 cells. J Endod. 2010;36:1978–82.
Zoufan K, Jiang J, Komabayashi T, Wang YH, Safavi KE, Zhu Q. Cytotoxicity evaluation of Gutta Flow and Endo Sequence BC sealers. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:657–61.
Alsubait SA, Al Ajlan R, Mitwalli H, Aburaisi N, Mahmood A, Muthurangan M, Almadhri R, Alfayez M, Anil S. Cytotoxicity of different concentrations of three root canal sealers on human mesenchymal stem cells. Biomolecules. 2018;1;8:E68.
Er K, Ayar A, Kalkan OF, Canpolat S, Tasdemir T, Ozan U. Neurotoxicity evaluation of three root canal sealers on cultured rat trigeminal ganglion neurons. J Clin Exp Dent. 2017;9:e34-9.
Ruparel NB, Ruparel SB, Chen PB, Ishikawa B, Diogenes A. Direct effect of endodontic sealers on trigeminal neuronal activity. J Endod. 2014;40:683–7.
Zhu X, Yuan Z, Yan P, Li Y, Jiang H, Huang S. Effect of iRoot SP and mineral trioxide aggregate (MTA) on the viability and polarization of macrophages. Arch Oral Biol. 2017;80:27–33.
Yuan Z, Zhu X, Li Y, Yan P, Jiang H. Influence of iRoot SP and mineral trioxide aggregate on the activation and polarization of macrophages induced by lipopolysaccharide. BMC Oral Health. 2018;18:56.
Güven EP, Taşlı PN, Yalvac ME, Sofiev N, Kayahan MB, Sahin F. In vitro comparison of induction capacity and biomineralization ability of mineral trioxide aggregate and a bioceramic root canal sealer. Int Endod J. 2013;46:1173–82.
Zaki DY, Zaazou MH, Khallaf ME, Hamdy TM. In vivo comparative evaluation of periapical healing in response to a calcium silicate and calcium hydroxide based endodontic sealers. Open Access Maced J Med Sci. 2018;6:1475–9.
Jung S, Libricht V, Sielker S, Hanisch MR, Schäfer E, Dammaschke T. Evaluation of the biocompatibility of root canal sealers on human periodontal ligament cells ex vivo. Odontology. 2018. https://doi.org/10.1007/s10266-018-0380-3 (epub ahead of print).
Vouzara T, Dimosiari G, Koulaouzidou EA, Economides N. Cytotoxicity of a new calcium silicate endodontic sealer. J Endod. 2018;44:849–52.
Camps J, Jeanneau C, El Ayachi I, Laurent P, About I. Bioactivity of a calcium silicate-based endodontic cement (BioRoot RCS): interactions with human periodontal ligament cells in vitro. J Endod. 2015;41:1469–73.
Loison-Robert LS, Tassin M, Bonte E, Berbar T, Isaac J, Berdal A, Simon S, Fournier BPJ. In vitro effects of two silicate-based materials, Biodentine and BioRoot RCS, on dental pulp stem cells in models of reactionary and reparative dentinogenesis. PLoS One. 2018;13:e0190014.
Jung S, Sielker S, Hanisch MR, Libricht V, Schäfer E, Dammaschke T. Cytotoxic effects of four different root canal sealers on human osteoblasts. PLoS One. 2018;13:e0194467.
Collado-González M, García-Bernal D, Oñate-Sánchez RE, Ortolani-Seltenerich PS, Lozano A, Forner L, Llena C, Rodríguez-Lozano FJ. Biocompatibility of three new calcium silicate-based endodontic sealers on human periodontal ligament stem cells. Int Endod J. 2017;50:875–84.
Scarparo RK, Haddad D, Acasigua GA, Fossati AC, Fachin EV, Grecca FS. Mineral trioxide aggregate-based sealer: analysis of tissue reactions to a new endodontic material. J Endod. 2010;36:1174–8.
Gomes-Filho JE, Watanabe S, Bernabé PF, de Moraes Costa MT. A mineral trioxide aggregate sealer stimulated mineralization. J Endod. 2009;35:256–60.
Gomes-Filho JE, Watanabe S, Gomes AC, Faria MD, Lodi CS, Penha Oliveira SH. Evaluation of the effects of endodontic materials on fibroblast viability and cytokine production. J Endod. 2009;35:1577–9.
da Silva GF, Guerreiro-Tanomaru JM, Sasso-Cerri E, Tanomaru-Filho M, Cerri PS. Histological and histomorphometrical evaluation of furcation perforations filled with MTA, CPM and ZOE. Int Endod J. 2011;44:100–10.
Gomes-Filho JE, Watanabe S, Cintra LT, Nery MJ, Dezan-Júnior E, Queiroz IO, Lodi CS, Basso MD. Effect of MTA-based sealer on the healing of periapical lesions. J Appl Oral Sci. 2013;21:235–42.
Graunaite I, Skucaite N, Lodiene G, Agentiene I, Machiulskiene V. Effect of resin-based and bioceramic root canal sealers on postoperative pain: a split-mouth randomized controlled trial. J Endod. 2018;44:689–93.
Chybowski EA, Glickman GN, Patel Y, Fleury A, Solomon E, He J. Clinical outcome of non-surgical root canal treatment using a single-cone technique with Endosequence bioceramic sealer: a retrospective analysis. J Endod. 2018;44:941–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Donnermeyer, D., Bürklein, S., Dammaschke, T. et al. Endodontic sealers based on calcium silicates: a systematic review. Odontology 107, 421–436 (2019). https://doi.org/10.1007/s10266-018-0400-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10266-018-0400-3