Abstract
Objectives
This study aims to evaluate the effect of different endodontic sealers (epoxy resin, eugenol, and bioceramic/calcium silicate-based) and the time of cementation (immediately or 7 days after canal obturation) on the bond strength of a fiberglass post cemented with RelyX™ ARC.
Material and methods
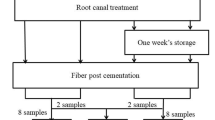
Eighty-four premolars were instrumented and divided into groups (n = 12) according to the sealer and the time of post cementation: Endofill (EN), Endosequence BC Sealer (BC), and AH Plus (AH) had immediately fiber post cementation; EN7, BC7, and AH7 had post cementation after 7 days; and control group (C) had fiber post cementation without endodontic sealer. Each post space of the root was cut into slices and submitted to push-out test. Failure mode was assessed. Two-way ANOVA, Tukey’s, and Dunnett’s tests were used for statistical analysis (α = 5%).
Results
The type of endodontic sealer (p < 0.001), the time of post cementation (p = 0.038), and the interaction sealer time (p = 0.002) had negative influence on bond strength of fiberglass posts cemented with RelyX™ ARC. AH promoted the highest bond strength mean values (21.20 MPa immediately and 15.54 MPa at 7 days). EN (9.75 MPa immediately and 13.15 MPa at 7 days) and BC (10.43 MPa immediately and 5.73 MPa at 7 days) had lower bond strength than AH, regardless the time of cementation.
Conclusions
AH was the best sealer to obturate the root canal when fiberglass cementation with resin-based cement is planned.
Clinical relevance
The correct choice of an endodontic sealer and the adequate time of post cementation may avoid post dislocation caused by low bond strength to dentin.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The longevity of endodontically treated teeth depends on several factors, including the ones related to (1) the tooth (the amount of remaining tooth structure, for example); (2) the root canal treatment procedures (the ability to promote optimal disinfection); and (3) the intracanal post cementation technique. When resin cements are chosen to cement fiberglass posts, one of the main concerns is the gradual loss of retention, which is closely related to, among other factors, the high sensitivity of the adhesive technique cementation and to the polymerization shrinkage of the resin cements [1]. Thus, to prevent the loss of retention of a fiberglass post, it is necessary to have adequate bond strength between post and dentin.
RelyX™ ARC (3 M ESPE, St Paul, MN, USA) is a dual cure adhesive resin cement used for the cementation of endodontic posts and other types of restoration such as metal, porcelain or resin crowns, and bridges. For many years, it has been questioned which is the most appropriate endodontic sealer to fill the root canal before post cementation with adhesive resin-based cements. It is clinically accepted that the use of eugenol-based sealers [such as Endofill (EN; Dentsply Maillefer, Ballaigues, Switzerland)] should be avoided before post cementation with an adhesive resin-based cement because the eugenol may inhibit the polymerization process in the resin-based cement [2].
Although former studies had shown the contrary [3, 4], recent and strong evidences confirmed that eugenol reduces the immediate bond strength of fiberglass posts cemented with adhesive resin-based sealers [5]. Therefore, other types of endodontic sealers have been indicated and developed as alternatives to be used before the post cementation with a resin cement, such as epoxy-amine resin-based sealers [for example, AH Plus (AH; Dentsply Maillefer, Ballaigues, Switzerland)] and calcium silicate-based/bioceramic sealers [for example, Endosequence BC (BC; Brasseler USA, Savannah, GA)]. AH is used as a gold standard in research [6,7,8,9,10,11] because of its excellent properties related to adhesion [12], sealing ability [13], and non-interference with the bond strength of fiberglass posts cemented with adhesive resin cements [6]. BC is a sealer mainly composed of calcium silicate and calcium phosphate. Among other advantages, BC sealer is able to form hydroxyapatite during its setting process, consequently producing a bond between the dentin and the filling material [14].
It has been demonstrated that bond strength to dentin of gutta-percha/BC is similar to that of gutta-percha/AH [8], a sealer that have higher bond strength than most of other sealers [15]. As BC sealer is a relatively new material available, the information about a possible interference with bond strength of fiberglass posts cemented with resin-based cements is still scarce.
In addition to the type of endodontic sealer, the time of post cementation is another factor that could affect the bond strength of fiberglass posts cemented with adhesive resin cements. Currently, there is no consensus in the literature if posts should be cemented immediately after root canal treatment or during a later stage after canal obturation. Some studies recommend that post space preparation and cementation should not be done immediately after root canal obturation with eugenol-based sealers, because the eugenol contamination is reduced if the sealer is allowed to set completely [16]. On the other hand, authors state that eugenol continues to penetrate into dentinal tubules over time; thus, if using a resin cement, it would be better to cement a fiberglass post in a time interval of 24 h (early stage) instead of after 2 weeks (delayed) [17]. There is little evidence to guide clinicians in relation to the best time for cementation of a fiberglass post using resin-based cement on canals sealed with non-eugenol sealers such as AH and BC. Delayed cementation of different fiber posts in root canal previously obturated with AH resulted in higher retentive strengths [18]. Conversely, authors observed no influence of the time of fiber post cementation on bovine dentin adhesion after endodontic obturation with different sealers [7].
Considering the clinical relevance of avoiding fiber posts displacement because of the reduced bond strength to dentin, the aim of this present study was to assess the effect of different endodontic sealers (eugenol-based, amine-epoxy resin-based, and calcium silicate-based/bioceramic) and the time of post cementation (immediately or 7 days after root canal obturation) on the bond strength of a fiberglass post cemented with an adhesive resin cement system (RelyX™ ARC).
The null hypothesis was that neither the type of endodontic sealer nor the time of post cementation would negatively interfere on the bond strength between the fiberglass post/adhesive cement and the root dentine.
Materials and methods
Sample preparation
This study was approved by the local ethics committee of the university where the experiment was conducted (CAAE 34892514.0.0000.5084).
Eighty-four single-rooted mandibular premolars extracted for orthodontic reasons were used. Teeth included in the study had straight roots, no caries or root cracks, and a root length of at least 15 mm. After cleaning, teeth were decoronated below the cementoenamel junction perpendicularly to their longitudinal axis using a water-cooled diamond disc. The coronal surface was flattened using slow-speed diamond burs. The length of the root was standardized at 15 mm.
A single operator, specialist in endodontics and who experienced all of the techniques used in this study, performed the root canal preparation, obturation, and post cementation procedures. Root canals were prepared 1 mm shorter of the apical foramen with Reciproc R40 (VDW München, Germany) with irrigation using 2.5% sodium hypochlorite (10 mL on total). Subsequently, smear layer was removed using 5 mL of 17% EDTA for 3 min [7] and a final flush with 10 mL of distilled water. Canals were dried with absorbent paper points (VDW München, Germany). All sealers were used in conjunction with gutta-percha points R40 (VDW München, Germany). The AH and EN sealers, used to fill the root canals, were prepared according to the manufacturers’ recommendations, and the gutta-percha cone was covered with a layer of sealer and inserted into the canal (with gentle brushing movements against the root canal walls). After that, the gutta-percha cone was slowly positioned. To fill the root canals with BC sealer, it was used with the syringe provided by the manufacturer. The sealer was inserted with the intracanal tips in the coronal third of the canal, and, then, the gutta-percha cone was covered with a thin layer of sealer and slowly inserted. Finally, for all specimens, a McSpadden compactor (Dentsply Maillefer Ballaigues Switzerland) was used for thermo filling and the gutta-percha was vertically compacted using a size-fitted plugger at the root canal orifice.
Teeth were then randomly divided in groups (n = 12) accordingly to the endodontic sealer and time of fiber post cementation: EN, BC, and AH had the fiber post cemented immediately after the completion of the obturation. EN7, BC7, and AH7 had the fiber post cemented 7 days post obturation. Additionally, in control group (C), fiber post was cemented without using an endodontic sealer.
Fiber post cementation
The filling material was removed on the first 10 mm of the canal (leaving 5 mm of gutta-percha on the apical third of the root) using size 3 Largo burs (Dentsply Mailefer). Subsequently, post spaces were prepared using the size 1 drill, provided in the White Post DC kit (FGM, Joinville, SC, Brazil) and attached to a low-speed handpiece. Post spaces were then irrigated with 10 mL of distilled water and dried with absorbent paper points.
The effectiveness of the removal of the root filling material was assessed using magnification loupes ×3.5 (Carl Zeiss, Jena, Germany). Double-tapered fiberglass posts no. 1 (White Post DC, FGM, Joinville, SC, Brazil) were selected by positioning them into the root canal and subsequently stored until cementation. Samples from EN7, BC7, and AH7 were maintained for 7 days in distilled water at 37° C before post space preparation and fiberglass post cementation. Silano (Prosil FGM, Joinville SC, Brazil) was applied on the post surface using a micro-brush for 1 min and, then, dried by blowing compressed air for 20 s. After post preparation, the post space was etched with 35% phosphoric acid, rinsed with water for 30 s, and dried with absorbent paper points. Subsequently, two layers of Primer (Adapter Scotchbond Multi Purpose 3 M) were applied for 10 s, and the post space was dried using absorbent paper points. Adhesive (Adapter Scotchbond Multi Purpose 3 M) was applied for 10 s and its excess was removed using absorbent paper points. Finally, the adhesive resin cement system RelyX™ ARC (3 M ESPE) was manipulated and placed into the post space with a Centrix syringe (DFL, Rio de Janeiro RJ, Brazil). The endodontic post was also covered with sealer and seated to full depth using finger pressure for 20 s. Light curing was carried out for 40 s using halogen light (Radii Cal; SDI, Melbourne, Australia). The specimens were kept humid for 7 days at 37° C.
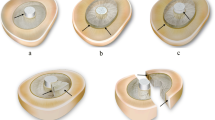
Obtaining and measuring the specimens
Each root post space was cut into four slices of 1.5 mm thickness in a cutting machine (Isomet 100 Precision Saw (Buehler Ltd., Lake Bluff, IL, USA)) under constant water irrigation. Apical and coronal ends were disposed. Images of both sides (cervical and apical) of the slices were captured with a digital camera (Q-Color 5; Olympus, America Inc., PA, USA) attached to a stereomicroscopic loupe (SZ61; Olympus America Inc., PA, USA), at ×40 magnification. The lumen diameters of both sides of the slices were measured using the Image J software (National Institute of Health, Maryland, USA http:/rsb.info.nih.gov/ij/). Figure 1 shows one of the root slices where it is possible to notice the complete internal surface of the root covered with cement, as well as the absence of air bubbles. The slices with evident bubbles or voids were discarded from the study to achieve the standardization of the specimens.
Micropush-out bond strengths
Micropush-out test measured bond strength of fiber post/RelyX™ ARC to dentin. The cervical side of each test specimen was placed in contact to a support (Odeme, Joaçaba, SC, Brazil), which was coupled to the base of a universal test machine (Instron, 3342, Canton, MA, USA). Loading was performed at a crosshead speed of 0.5 mm min−1 until the post was completely dislodged from the root slice. The value obtained in Kgf (kilogram-force) was used to calculate the bond strength in MPa (Mega Pascal) using the following formula: A = π (R + r) √h 2 + (R − r)2; where π is the constant 3.14, r 1 and r 2 are the smaller and larger post space radii, respectively, and h is the height of the section in mm.
Failure mode analysis
The pushed-out specimens were cleaved longitudinally and the root segments were observed under ×40 magnification with a stereomicroscope loupe (SZ61, Olympus America Inc., PA, USA) to categorize the failure mode into six types: (1) adhesive: at post/cement interface, (2) adhesive: at cement/dentin interface, (3) adhesive-mixed: at post/cement/dentin, (4) cohesive into dentin, (5) cohesive into cement, and (6) cohesive into post.
Data analysis
Mean bond strength (MPa) of fiber posts and standard deviation were calculated for each group. Data normality was confirmed by Shapiro-Wilk test (α = 5%). To investigate the influence of the endodontic sealer and the time of cementation on the fiber posts/RelyX™ ARC, bond strength two-way ANOVA was used. Additionally, the effect size (partial η2) of the variables (type of endodontic sealer and time of cementation) on the bond strength was also calculated. Multiple comparisons were achieved using one-way ANOVA, post hoc Tukey’s, and post hoc Dunnett’s tests. Significance level was set at α = 5% (SPSS version 21.0 IBM, Armonk, NY, USA).
Results
Figure 2 shows the mean bond strength values (MPa) and standard deviation for fiber posts cemented in the root canals that had been previously obturated with different endodontic sealers, immediately and 7 days after root canal obturation. For the control group, the value was 19.31 (± 6.00). Graph 1 shows the variation in fiber posts bond strength for each endodontic sealer.
Two-way ANOVA showed that the endodontic sealer (p < 0.001), time of post cementation (p = 0.038), and the interaction between sealer time (p = 0.002) had a negative influence on bond strength, with values of partial η2 of 0.480 for sealer and 0.064 for time of cementation. In addition, it was observed that the type of endodontic sealer was the main factor responsible for the variation on the bond strength of fiber posts cemented with RelyX™ ARC (48%).
Post hoc Tukey’s and Dunnett’s tests were used for multiple comparisons (α = 5%). Figure 3 shows the interaction (mean and confidence intervals) between the endodontic sealers, time of cementation, and bond strength of fiber posts. AH group had the highest bond strength values regardless of the time of cementation (preferable when the post was cemented immediately, but also acceptable when the post was cemented after 7 days). The time of post cementation also did not influence on the bond strength for either BC group (p ≥ 0.05) or EN group (p ≥ 0.05), and both sealers presented lower bond strength values when compared with AH [statistically significant (p ≤ 0.05) for the following comparisons: BC and AH; BC7 and AH; BC7 and AH7; EN and AH; EN and AH7; EN7 and AH] , and when compared with the control group (p ≤ 0.05).
Bond strength mean values (Mpa) and confidence intervals (95%) of fiber posts cemented in the root canals that had been previously obturated with Endofill (EN), AH Plus (AH), Endosequence BC Sealer (BC), and control group/no sealer (C), immediately and 7 days after root canal obturation. *Post hoc Tukey test (p < 0.05); the different superscript letters indicate statistically significant difference. *Post hoc Dunnett (p < 0.05); asterisk indicates statistically significant difference in relation to the control group
Table 1 presents the results of the predominating types of failures in each group. The prevalence of adhesive failures on the cement-dentin interface was verified in all of the groups, except for the AH group.
Discussion
The type of endodontic sealer, the time of post cementation, and the interaction between sealer time had a negative influence on the bond strength of fiber posts cemented with RelyX™ ARC. The most important factor responsible for the variation on the bond strength was the sealer. These results reject, therefore, the null hypothesis.
In this present study, the procedures performed during post space preparation were carefully conducted and were standardized for all groups. This step apparently removed the excess of the endodontic filling material (sealer/gutta-percha) from the prepared root canal space. Nevertheless, remnants of sealer might have been left attached to the canal walls and also located in the entrance of the dentinal tubules. Therefore, the remnants of previous sealers may be present even after post space preparation and cleaning, and this would change the wettability, permeability, and reactivity of the dentin, affecting the resin-dentin bond strength [19, 20]. Moreover, the use of RelyX™ ARC and the post cementation technique was also carefully conducted to guarantee the complete involvement of the post and the root surfaces with cement. All these steps were standardized to avoid a negative impact in the push-out test.
Push-out test was used in this study in accordance with other relevant studies published in the dental literature [21, 22]. One advantage of the push-out test, when investigating bond strength, is its ability to create a uniform stress concentration and adhesive failure pattern on the specimens [23]. However, as the push-out is essentially a laboratorial test [24], it should not be used as a single guideline for clinical decision-making [25].
The results of this in vitro study showed that, aiming to have higher bond strength, the best endodontic sealer to fill the root canal before fiber post cementation with RelyX™ ARC is AH. Theoretically, the results for AH pointed that it is better to cement the post as soon as the root canal obturation is completed. However, since both experimental times of post cementation (immediately and 7 days post obturation) had similar values of bond strength when compared to the control group (post cementation without endodontic sealer), both options of time for post cementation might be adequate choices when using AH sealer to obturate the root canal. The inexistence of difference with the control group means that AH did not interfere with the fiber post bond strength.
Regarding the root canals obturated with BC or EN, the results showed that it does not matter if the post cementation is performed immediately or after 7 days of the root canal obturation. For both sealers, the fiberglass post bond strength values were lower than those values observed on the AH and the control group.
This present research emphasized what have been already reported in other studies regarding the superiority of AH [12, 13] and its non-interference with the bond strength of fiberglass post cementation when using adhesive resin cements [6]. The 5 mm of gutta-percha/AH that remained in the apical third might have provided a good adaptation to the dentin due to the sealer’s ability to form a chemical bond to the dentin collagen network [11]. Therefore, the apical root canal obturation with gutta-percha/AH provided an optimal environment to the fiber post cementation with RelyX™ ARC, resulting, consequently, in adequate fiber post bond strength.
The findings of this current study reinforced the idea that zinc oxide eugenol-based sealers (EN) should be avoided when it is planned to use resin cement. This suggestion is in accordance with and can be supported by a recent meta-analysis that indicated that eugenol reduced bond strength even when different eugenol contact times were measured (ranging from immediate to 15 days) [5].
The poor results of fiber post bond strength when BC sealer was used to fill the root canal [immediately 10.43 MPa (± 5.89) and 7 days 5.73 MPa (± 2.82)], when compared to AH [immediately 21.20 MPa (± 5.79) and 7 days 15.54 MPa (± 4.98)], can be attributed to the presence of a high amount of residual BC left inside the tubules after post space preparation. According to Oltra et al. [26], in a micro-CT study investigating the percentage of residual filling material after root canal obturation, the authors showed that BC sealer remained significantly more into the dentinal tubules than AH. In our study, this excess of residual material could be responsible for impairing the correct penetration of the resin cement inside the tubules. Another explanation for this finding might be related with the potential of BC sealer to form tag-like structures consisting of either cement itself or crystals, suggesting intratubular precipitation [27]. This precipitation (rich in calcium and phosphate), due to its high alkalinity, could decrease the effectiveness of etching (phosphoric acid) and prevent the formation of an effective hybrid layer with resinous tags.
Overall, the failure mode analysis showed that for all endodontic sealers, and also for the control group, the majority of failures were adhesive on cement/dentin interface. This fact can demonstrate an adequate (and strong) bonding between the endodontic post and RelyX™ ARC. After using EN as an endodontic sealer, the post cementation at 7 days presented an increase in adhesive (cement/dentin) failures and, also, a considerable increase in adhesive (post/cement) failures when compared to immediate post cementation. Although the push-out tests have showed that EN impaired the fiber post bond strength regardless of the time of post cementation, these results could suggest that eugenol remains on the dentin over time and, consequently, it might be worse to have the post cemented after 7 days post root canal obturation. Nevertheless, it is important to bear in mind that failure mode analysis is a complementary test and it should not be analyzed independently.
Conclusion
In sum, within the limitations of this in vitro study, it was concluded that before fiberglass post cementation with an adhesive resin-based cement (RelyX™ ARC), the best endodontic sealer to obturate the root canal is AH (epoxy resin-based sealer), immediately or 7 days after the completion of endodontic procedures. EN (zinc oxide eugenol-based) should be avoided. BC (bioceramic/calcium silicate-based) may not be a good alternative.
References
Pulido CA, de Oliveira Franco AP, Gomes GM, Bittencourt BF, Kalinowski HJ, Gomes JC, Gomes OM (2016) An in situ evaluation of the polymerization shrinkage, degree of conversion, and bond strength of resin cements used for luting fiber posts. J Prosthet Dent 116:570–576
Fujisawa S, Kadoma Y (1992) Effect of phenolic compounds on the polymerization of methyl methacrylate. Dent Mater 8:324–326
Schwartz RS, Murchison DF, Walker WA 3rd (1998) Effects of eugenol and noneugenol endodontic sealer cements on post retention. J Endod 24:564–567
Aggarwal V, Singla M, Miglani S et al (2012) Effect of different root canal obturating materials on push-out bond strength of a fiber dowel. J Prosthodont 21:389–392
Altmann AS, Leitune VC, Collares FM (2015) Influence of eugenol-based sealers on push out bond strength of fiber post luted with resin cement: systematic review and meta-analysis. J Endod 41:1418–1423
Cecchin D, Farina AP, Souza MA, Carlini-Júnior B, Ferraz CC (2011) Effect of root canal sealers on bond strength of fibreglass posts cemented with self-adhesive resin cements. Int Endod J 44:314–320
Rosa RA, Barreto MS, Moraes Rdo A et al (2013) Influence of endodontic sealer composition and time of fiber post cementation on sealer adhesiveness to bovine root dentin. Braz Dent J 24:241–246
Shokouhinejad N, Gorjestani H, Nasseh AA, Hoseini A, Mohammadi M, Shamshiri AR (2013) Push-out bond strength of gutta-percha with a new bioceramic sealer in the presence or absence of smear layer. Aust Endod J 39:102–106
Carvalho CN, Martinelli JR, Bauer J, Haapasalo M, Shen Y, Bradaschia-Correa V, Manso AP, Gavini G (2015) Micropush-out dentine bond strength of a new gutta-percha and niobium phosphate glass composite. Int Endod J 48:451–459
Forough Reyhani M, Ghasemi N, Rahimi S, Milani AS, Omrani E (2016) Effect of different endodontic sealers on the push-out bond strength of fiber posts. Iran Endod J 11:119–123
Oliveira DS, Cardoso ML, Queiroz TF, Silva EJ, Souza EM, De-Deus G (2016) Suboptimal push-out bond strengths of calcium silicate-based sealers. Int Endod J 49:796–801
De-Deus G, Di Giorgi K, Fidel S, Fidel RA, Paciornik S (2009) Push-out bond strength of Resilon/Epiphany and Resilon/Epiphany self-etch to root dentin. J Endod 35:1048–1050
Santos J, Tjäderhane L, Ferraz C, Zaia A, Alves M, De Goes M, Carrilho M (2010) Long-term sealing ability of resin-based root canal fillings. Int Endod J 43:455–460
Loushine BA, Bryan TE, Looney SW et al (2011) Setting properties and cytotoxicity evaluation of a premixed bioceramic root canal sealer. J Endod 37:673–677
Gettleman BH, Messer HH, ElDeeb ME (1991) Adhesion of sealer cements to dentin with and without the smear layer. J Endod 17:15–20
Vano M, Cury AH, Goracci C et al (2006) The effect of immediate versus delayed cementation on the retention of different types of fiber post in canals obturated using a eugenol sealer. J Endod 32:882–885
Aleisa K, Al-Dwairi ZN, Alsubait SA, Morgano SM (2016) Pull-out retentive strength of fiber posts cemented at different times in canals obturated with a eugenol-based sealer. J Prosthet Dent 116:85–90
Vano M, Cury AH, Goracci C, Chieffi N, Gabriele M, Tay FR, Ferrari M (2008) Retention of fiber posts cemented at different time intervals in canals obturated using an epoxy resin sealer. J Dent 36:801–807
Schwartzer E, Collares FM, Ogliari FA et al (2007) Influence of zinc oxide-eugenol temporary cement on bond strength of an all-in-one adhesive system to bovine dentin. Braz J Oral Sci 6:6
Ribeiro JC, Coelho PG, Janal MN et al (2011) The influence of temporary cements on dental adhesive systems for luting cementation. J Dent 39:255–262
Aggarwal V, Singla M, Miglani S, Kohli S (2013) Comparative evaluation of push-out bond strength of ProRoot MTA, Biodentine, and MTA Plus in furcation perforation repair. J Conserv Dent 16:462–465
Nagas E, Cehreli ZC, Uyanik MO, Vallittu PK, Lassila LV (2016) Effect of several intracanal medicaments on the push-out bond strength of ProRoot MTA and Biodentine. Int Endod J 49:184–188
Campos RE, Santos Filho PCF, de O Júnior OB, Ambrosano GMB, Pereira CA (2017) Comparative evaluation of 3 microbond strength tests using 4 adhesive systems: mechanical, finite element, and failure analysis. J Prosthet Dent. https://doi.org/10.1016/j.prosdent.2017.02.024
Chen WP, Chen YY, Huang SH, Lin CP (2013 Feb) Limitations of push-out test in bond strength measurement. J Endod 39(2):283–287
De-Deus G, Souza E, Versiani M (2015) Methodological considerations on push-out tests in endodontics. Int Endod J 48:501–503
Oltra E, Cox TC, LaCourse MR, Johnson JD, Paranjpe A (2017) Retreatability of two endodontic sealers, EndoSequence BC Sealer and AH Plus: a micro-computed tomographic comparison. Restor Dent Endod 42:19–26
Han L, Okiji T (2013) Bioactivity evaluation of three calcium silicate-based endodontic materials. Int Endod J 46:808–814
Funding
The work was supported by Foundation for Research and Scientific and Technological Development of Maranhão-FAPEMA, Brazil.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Vilas-Boas, D.A., Grazziotin-Soares, R., Ardenghi, D.M. et al. Effect of different endodontic sealers and time of cementation on push-out bond strength of fiber posts. Clin Oral Invest 22, 1403–1409 (2018). https://doi.org/10.1007/s00784-017-2230-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-017-2230-z