Abstract
The aim of the present study was to assess whether different dentin conditioning protocols with different acids [phosphoric acid, ethylene diamine tetra acetic acid (EDTA), and polyacrylic acid (PAA)] influence the bond strength of fiber posts along the radicular depth when luted with self-adhesive resin cement. Twenty single-rooted teeth were randomly divided into four experimental groups (n = 5) according to dentin treatment: Group 1: no treatment; Group 2: etching with 35 % phosphoric acid for 10 s; Group 3: 17 % EDTA application for 60 s; and Group 4: conditioning with 25 % PAA for 30 s. RelyX Fiber Posts were luted with the self-adhesive resin cement RelyX Unicem 2 Automix (3M ESPE). Roots were transversally sectioned into nine 1-mm thick specimens, three corresponding to each root third and a push-out test was performed. Data were analyzed by two-way ANOVA and Tukey test (p < 0.05). Failure mode was determined and specimens with representative failures for each group were observed under scanning electron microscopy. According to the results, dentin treatment influenced the bond strength (p < 0.001), whereas the root third did not (p > 0.05). Fiber posts luted after treating dentin with phosphoric acid, and PAA exhibited the highest push-out bond strength values, while the lowest were obtained after EDTA application. Intermediate results were obtained when dentin was not conditioned. In conclusion, the bond strength of the self-adhesive resin cement RelyX Unicem 2 improves when root dentin is treated with 35 % phosphoric acid or 25 % PAA, before fiber posts luting irrespective of the root depth.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fiber reinforced composite (FRC) posts have become the first choice to restore endodontically treated teeth with an important loss of structure due to extensive carious lesions, fractures, defective restorations, or excessive access preparations [1–3].
Several advantages of FRC posts have contributed to their widespread use. Their modulus of elasticity is similar to dentin, allowing a uniform distribution of occlusal stresses in the root dentin and reducing the risk of catastrophic failures, such as root fractures [4]. Moreover, shade and partial translucency of FRC posts confer them favorable optical properties to reproduce the natural aspect in the restored teeth and enable light curing of dual-cure resin cements [5].
Presently, there are numerous dual-cured resin cements available to lute FRC posts, with self-adhesive resin cements (SARCs) being preferably chosen by clinicians [6]. Their attractiveness is based on their simplicity of use and their reduced technique and operator sensitivity, because no etching or denting bonding is required [6, 7]. Moreover, literature suggests that SARCs improve fiber posts retention in comparison with those resin cements that require more bonding steps [3, 6].
Self-adhesive resin cements contain an organic matrix and inorganic fillers as composites do. The organic matrix consists of multi-functional phosphoric acidic methacrylates or other acidic monomers. The inorganic fillers are composed of combinations selected from barium fluoroaluminoborosilicate glass, strontium calcium aluminosilicate glass, quartz, colloidal silica, and ytterbium fluoride among other glass fillers [8].
Their mechanism of adhesion consists of an initial redox reaction that starts after the acidic monomers are activated by light or self-curing mechanisms. Thus, the monomers demineralize the dentin hydroxyapatite and the infiltration within dentin and the polymerization of the monomers take place [8, 9]. In addition, an acid–base reaction occurs, where phosphoric acidic methacrylates in the organic matrix react with the basic fillers and the hydroxyapatite of root dentin [8, 10]. As a result of this reaction, the pH of SARC increases progressively, and the neutralization is accelerated by water, the by-product of the acid–base reaction [11].
The first SARC, RelyX Unicem, was launched into the market in 2002; thus, it is the most tested in literature and the so-called gold standard for SARCs [8]. A new version was available in 2010, RelyX Unicem 2 with improved fluidity according to manufacturer without changes in the mechanism of adhesion. RelyX Unicem demineralizes dentin very superficially without a distinct hybrid layer or resin tags formation [12, 13]. However, RelyX Unicem has been reported to achieve high and stable bond strength values despite this superficial interaction with dentin substrate, being attributed to its chemical interaction with the calcium from hydroxyapatite [14–16].
However, the main cause of failure for teeth restored with FRC posts is still post debonding [17]. Post space preparation generates a thick smear layer that contains rough debris and remnants of gutta-percha and sealers [18]. Moreover, the mineralized components of this smear layer are able to buffer the pH of the acidic monomers, limiting its diffusion and impairing a proper demineralization of the underlying dentin [19, 20].
Therefore, total or partial removal of the smear layer by different acidic solutions has been proposed to enhance the interaction between resin cement and dentin, and increase the SARCs bond strength [21–24]. However, a few studies have evaluated the effectiveness of the application of these acidic solutions before SARCs insertion in the post space and, according to the results, this effectiveness, seems to be SARC dependent [24, 25].
The aim of this study was to determine the push-out bond strength of RelyX Unicem 2 along the radicular depth after treating the root dentin with a strong acid, such as 35 % phosphoric acid, or mild acids, such as 17 % EDTA and 25 % PAA. Thus, the first null hypothesis was that the bond strength of RelyX Unicem 2 is the same regardless of the acid applied on the root canal dentin. The second null hypothesis was that this bond strength is similar along the radicular depth.
Materials and methods
Twenty single-rooted human teeth with fully developed apices and extracted for periodontal or orthodontic reasons were selected. The inclusion criteria were absence of caries or root cracks, and previous endodontic treatments, posts, or crowns. Teeth were stored in 0.1 % thymol at 4 °C for a maximum of 3 months.
Roots were sectioned perpendicularly to the long axis of the teeth to a length of 16 mm from the apex using a diamond bur at high speed under copious water cooling.
Specimen preparation
Root canals were endodontically instrumented at a working length of 1 mm from the apex. All root canals were instrumented by the same operator. Canals were treated using a crown-down preparation technique with ProTaper rotatory instruments (Dentsply-Maillefer, Ballaigues, Switzerland) to size F1 or F2. Irrigation was performed using 5.25 % sodium hypochlorite between files and 17 % EDTA solution (Ultradent, South Jordan, UT, USA) for 1 min as a final rinse. Root canals were rinsed with distilled water for 1 min and then dried with ISO–standardized paper points (Dentsply-Maillefer). Afterwards, they were filled with gutta-percha cones (Dentsply DeTrey, Konstanz, Germany) and AH-Plus cement (Dentsply DeTrey, Zurich, Switzerland) with the lateral condensation technique. Once the endodontic treatment was completed, cervical root canal openings were filled with a resin-modified glass-ionomer cement (Vitrebond Plus, 3M ESPE, St Paul, MN, USA) that was light-cured for 40 s (LED Elipar curing light, light intensity of 1200 mW/cm2, 3M ESPE, Seefeld, Germany). Specimens were then stored in distilled water for 7 days at 37 °C.
Post luting procedures
Post spaces were prepared to a depth of 10 mm by removing the gutta-percha with Gates-Glidden drills size 2 and 3 (Dentsply-Maillefer), leaving a minimum apical seal of 5 mm.
Dowel spaces were drilled using calibrated drills corresponding to the conical RelyX glass Fiber Post size #1 or #2 (3M ESPE). A final flush of the canal spaces was accomplished using sterile water, and they were dried with paper points (Dentsply–Maillefer).
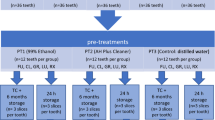
The prepared roots were equally and randomly divided into four experimental groups (n = 5) [26], according to the dentin treatment performed before RelyX Unicem 2 (3M ESPE) application (Table 1): Group 1: No dentin treatment; Group 2: etching with 35 % phosphoric acid (Ultra-Etch, Ultradent) for 10 s; Group 3: treatment with 17 % EDTA gel (SlickGel ES, SybronEndo, Orange, CA, USA.) for 60 s; and Group 4: conditioning with 25 % PAA (Ketac Conditioner, 3M ESPE) for 30 s.
FRC posts were tried-in, cleaned with alcohol, and then luted. The post was seated with constant finger pressure and stabilized under a 750-g static load [23]. This seating force was applied for the first 2 min, leaving the material to set in the self-curing mode and, then, it was light-cured for 40 s.
After the luting procedure, the coronal part of the posts was completely covered with the resin-modified glass-ionomer cement Vitrebond Plus (3M ESPE), and the roots were stored in distilled water for 7 days at 37 °C.
Push-out bond strength test
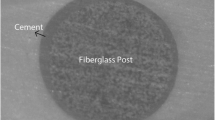
Roots were embedded in epoxy resin and transversally sectioned with a high precision digitally programmed machine (Isomet 5000, Buehler, Lake Buff, IL, USA). It was pre-set to serially obtain nine specimens 1-mm thick by means of a water-cooled diamond saw. Three sections corresponded to each root third: apical, middle, and coronal. Each specimen was marked on its coronal side with an indelible marker, and the exact thickness of each segment was measured using a digital caliper of 0.001-mm accuracy (Mitutoyo, Tokyo, Japan).
Before testing, all sections were observed under a stereomicroscope (Olympus SZX7, Olympus Optical Co., Ltd, London, UK) at 30× to detect potential defects caused by cutting. Photographs of both sides of each specimen were taken to calculate the coronal and apical post radius using the software Image J software, v. 1.44, (National Institutes of Health, Bethesda, MD, USA). The coronal dentin surface of each specimen was secured face down with cyanoacrylate adhesive (Loctite Gel, Henkel, Düsseldorf, Germany) to a horizontal stainless steel platform with a central circular perforation. A vertical static load was applied in the apical-to-cervical direction via a metal rod to the post section in each specimen, using a universal load testing machine (Instron 3345, Instron Corp., Canton, MA, USA) at a crosshead speed of 0.5 mm/min. The maximum push-out force (N) for bond failure was recorded. The retentive strength of the post segment was expressed in MPa, by dividing the load at failure in Newtons by the interfacial area (A) of the post fragment, which corresponded to the bonded area, in square millimeters (mm2). The interfacial area was calculated as the lateral surface of a truncated cone using the following formula: A = (R + r) [h 2 + (R − r)2] 0.5, where = 3.14, R = coronal post radius, r = apical post radius, and h = root slice thickness.
The failure mode of each debonded specimen was evaluated under the stereomicroscope at 30× magnification and classified as adhesive (between dentin and resin cement or between resin cement and the post), cohesive (within the resin cement or within the post), or mixed failure (a combination of adhesive and cohesive failures). Representative specimens from each experimental group were sputter-coated with gold (Bal-Tec Sputter Coater SCD 005, Bal-Tec GmbH, Witten, Germany) and observed under a scanning electron microscope (SEM) (Phillips XL30 ESEM, FEI Company, Hillsboro, OR, USA) at 100×.
Micromorphological analysis
Eight additional teeth (2 per experimental group) were instrumented and obturated as previously described for the push-out test. Then, the gutta-percha was removed and root dentin was treated as described before for each experimental group. Afterwards, two longitudinal grooves were made on both sides of each root using a diamond disk (Horico GmbH, Berlin, Germany) and with the help of a wax knife positioned into the grooves previously carved the roots were sectioned longitudinally. The specimens were subjected to a drying process by increasingly alcohol immersion dilutions in distilled water for 20 min each (25, 50, 75, 95, and 100 %) according to Perdigão et al. [27] and were gold-sputtered. The surfaces were morphologically analyzed under the same scanning electron microscope at 5000×.
Statistical analysis
Two-way ANOVA was carried out to determine the influence of the independent variables dentin treatment and root depth on the dependent variable bond strength of the resin cement used to lute fiber posts, and posterior comparisons were analyzed by Tukey’s test. Statistical analysis was performed by means of the IBM SPSS 19 software (IBM Company, Armonk, NY, USA) with a pre-set alpha of 0.05.
Results
Two-way ANOVA test showed that the variable dentin treatment influenced on the dependent variable bond strength (p < 0.001), while the root depth and the interaction between dentin treatment and root depth did not (p > 0.05).
Mean and standard deviations determined for each experimental group are shown in Table 2. The posterior comparisons detected that the specimens treated with phosphoric acid or PAA showed similar and higher bond strength values than those obtained for the untreated group. The lowest bond strengths were achieved when root dentin was conditioned with EDTA.
Failure mode analysis
Figure 1 summarizes the percentage of each failure mode determined for the experimental groups tested.
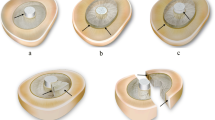
The most representative failure for the group without dentin treatment was the adhesive failure between the resin cement and the root dentin. As it can be observed in Fig. 2a, after post debonding, the cement remained mainly attached to the post and, thus, no remnants of resin cement were found around dentin walls.
SEM images of representative failure modes for each experimental group. a Adhesive failure of a specimen cemented with no dentin treatment (group 1). b Cohesive failure of a specimen luted after dentin treatment with phosphoric acid (group 2). c Cohesive failure of a specimen cemented after dentin treatment with EDTA (group 3). d Cohesive failure of a specimen luted after treatment with PAA (group 4)
Conversely, the cohesive failure within the cement was the most frequently found when root dentin was conditioned with phosphoric acid, EDTA, and PAA. After push-out test, specimens showed a break within the resin cement mass and consequently, resin cement remnants were clearly visible surrounding the post space walls and also the post (Fig. 2b–d).
Micromorphological analysis
The acidic solutions tested produced distinct effects on root canal dentin. When no acid solution was applied, the dentin walls appeared covered by smear layer and dentinal tubules could not be observed (Fig. 3a). The etching with phosphoric acid completely removed the smear layer and the smear plugs, dentinal tubules could be clearly identified, and peritubular dentin was selectively removed at the tubules entrance (Fig. 3b). By contrast, EDTA (Fig. 3c) was not able to remove the smear layer created after preparing the post space, and therefore, failed to expose dentine tubules resembling untreated dentin. Regarding PAA, this mild acid created a substrate where the smear layer and smear plugs were partially removed (Fig. 3d).
Discussion
According to the results obtained, the first null hypothesis must be rejected, as the dentin treatment influenced the push-out bond strength of FRC posts luted with RelyX Unicem 2. Nevertheless, the second hypothesis has to be accepted, as the root third did not affect the bond strength values achieved.
The push-out bond strength of FRC posts luted with RelyX Unicem 2 increased when smear layer was completely removed after treating dentin with a strong acid like 35 % phosphoric acid or if partially dissolved by a mild acid like 25 % PAA. Conversely, treatment with the mild acid 17 % EDTA produced significantly lower bond strength values.
Previous studies have reported an adequate performance of RelyX Unicem in comparison with total-etch or self-etching adhesives with the conventional resin cements, even when no dentin treatment was performed [28, 29]. However, in vivo reports have concluded that post debonding is still the main reason for clinical failure [17, 30].
In the present study, the application of phosphoric acid on root canal dentin completely removed the thick smear layer, and smear plugs created during post space preparation and demineralized the underlying dentin (Fig. 3a, b). This would help the infiltration of the resin cement and improve the micromechanical interlocking, yielding higher bond strengths than an untreated substrate. The improved performance of the application of phosphoric acid can also be related with the high percentage of cohesive failures (61.8 %) within the cement registered in the present study in comparison with the untreated group which showed mainly adhesive failures (27.13 %). In fact, RelyX Unicem has been reported to perform better in terms of microtensile bond strength on a free smear layer surface in comparison with other SARCs [31].
The bonding mechanism of SARCs is considered to be similar to that of mild self-etching adhesives based on the adhesion-decalcification concept [12]. According to this, chemical reaction between the phosphoric acidic methacrylates and the hydroxyapatite of root dentin would be relevant [12, 32], as the chemical interaction has been reported to provide hydrolytic stability to this SARC after thermomechanical aging [33], being impaired by the demineralization produced by phosphoric acid. However, in the root canal, the bonding effectiveness of RelyX Unicem 2 would be mainly compromised by the presence of a thick smear layer. According to this, some reports described lower push-out bond strengths for self-etching adhesives when compared with total-etch ones [34, 35], although other reports concluded similar results for both depending mainly on the adhesive tested [13, 33, 36].
Regarding PAA, the application of this mild acid before luting FRC posts with RelyX Unicem 2 was related with higher bond strength values. These results are in accordance with previous studies on radicular dentin [37, 38], although Tonial et al. reported an improvement of bond strength only for Maxcem Elite resin cement with no influence for RelyX Unicem. Furthermore, Faria-e-Silva et al. did not find differences between treating dentin with PAA or not before luting with RelyX Unicem. However, PAA was used in a lower concentration (11.5 %), half of the one used in the present study which could explain the differences found with our results [24]. PAA partially removes the smear layer and the smear plugs (Fig. 3d), and according to Mazzitelli et al. and Pavan et al. [21, 37], it creates an intermediate surface layer that may activate calcium and phosphate ions promoting a stronger chemical interaction between resin cement and dentin. RelyX Unicem 2 contents glass-ionomer filler particles in its composition [39] and mild acids, such as PAA, have been recommended to remove or modify the smear layer prior to GICs cementation to enhance their bond strength to dentin [40]. This improvement in bond strength could be related, similarly to phosphoric acid application, with the low percentage of adhesives failures between dentin and cement (5.1 %) and the high prevalence of cohesive failures within cement (69.2 %) when compared to untreated specimens.
By contrast, specimens treated with EDTA achieved the lowest bond strength values despite EDTA being also a mild acid. SEM images showed that after EDTA application, the dentin surface was still covered by the smear layer (Fig. 3c). However, EDTA is a chelating agent that depletes Ca levels, modifying the smear layer [41, 42]. Consequently, EDTA would not enhance micromechanical interlocking with the underlying dentin and would also hamper the chemical reaction produced between dentin hydroxyapatite and RelyX Unicem 2, according to previous studies [23, 24].
Regarding the influence of root dentin depth, push-out bond strength values of RelyX Unicem 2 were similar along the root canal depth. The bond strength of resin cements have been described to decrease from the coronal to the apical third [43, 44]. The main reasons described are the light attenuation through the fiber post and the histological characteristics of the root canal, as the number of dentinal tubules decreases along the radicular depth and the presence of sclerotic dentine increases with age [45, 46]. Notwithstanding, literature shows controversial results when RelyX Unicem 2 or its previous version has been tested. Some authors reported higher bond strength values at the coronal and middle thirds than at the apical one [14, 47], whereas others reported that RelyX Unicem behaved homogenously along the radicular length as found in the current study [26, 48]. The main reason that could explain this homogenous behavior is its dual-cured nature, which allows polymerization where light does not reach [49].
According to the results aforementioned, the application of phosphoric acid or PAA improves the bond strength of RelyX Unicem 2 when luting fiber posts. Notwithstanding, SARCs are not a homogenous group neither in composition nor in adhesion mechanism [8, 50]; thus, other SARCs should also be tested. In addition, it would be interesting to evaluate how these improved results endure the test of time.
Finally, under the experimental conditions of this study, the following conclusions can be drawn:
-
The bond strength of the self-adhesive resin cement RelyX Unicem 2 is increased by treating the root canal dentin with 35 % phosphoric acid or with 25 % PAA before luting fiber post, whereas the conditioning with 17 % EDTA is not beneficial.
-
The root depth did not influence the push-out bond strength of this self-adhesive resin cement.
References
Goracci C, Ferrari M. Current perspectives on post systems: a literature review. Aust Dent J. 2011;56:77–83.
Cagidiaco MC, Goracci C, Garcia-Godoy F, Ferrari M. Clinical studies of fiber posts: a literature review. Int J Prosthodont. 2008;21:328–36.
Sterzenbach G, Karajouli G, Naumann M, Peroz I, Bitter K. Fiber post placement with core build-up materials or resin cements-an evaluation of different adhesive approaches. Acta Odontol Scand. 2012;70:368–76.
Chieruzzi M, Pagano S, Pennacchi M, Lombardo G, D’Errico P, Kenny JM. Compressive and flexural behaviour of fibre reinforced endodontic posts. J Dent. 2012;40:968–78.
Kim YK, Kim SK, Kim KH, Kwon TY. Degree of conversion of dual-cured resin cement light-cured through three fibre posts within human root canals: an ex vivo study. Int Endod J. 2009;42:667–74.
Sarkis-Onofre R, Skupien JA, Cenci MS, Moraes RR, Pereira-Cenci T. The role of resin cement on bond strength of glass-fiber posts luted into root canals: a systematic review and meta-analysis of in vitro studies. Oper Dent. 2014;39:E31–44.
Silva RA, Coutinho M, Cardozo PI, Silva LA, Zorzatto JR. Conventional dual-cure versus self-adhesive resin cements in dentin bond integrity. J Appl Oral Sci. 2011;19:355–62.
Ferracane JL, Stansbury JW, Burke FJ. Self-adhesive resin cements—chemistry, properties and clinical considerations. J Oral Rehabil. 2011;38:295–314.
Abo-Hamar SE, Hiller KA, Jung H, Federlin M, Friedl KH, Schmalz G. Bond strength of a new universal self-adhesive resin luting cement to dentin and enamel. Clin Oral Investig. 2005;9:161–7.
Gerth HU, Dammaschke T, Zuchner H, Schafer E. Chemical analysis and bonding reaction of RelyX unicem and bifix composites–a comparative study. Dent Mater. 2006;22:934–41.
Zorzin J, Petschelt A, Ebert J, Lohbauer U. pH neutralization and influence on mechanical strength in self-adhesive resin luting agents. Dent Mater. 2012;28:672–9.
Monticelli F, Osorio R, Mazzitelli C, Ferrari M, Toledano M. Limited decalcification/diffusion of self-adhesive cements into dentin. J Dent Res. 2008;87:974–9.
Bitter K, Paris S, Pfuertner C, Neumann K, Kielbassa AM. Morphological and bond strength evaluation of different resin cements to root dentin. Eur J Oral Sci. 2009;117:326–33.
de Durao Mauricio PJ, Gonzalez-Lopez S, Aguilar-Mendoza JA, Felix S, Gonzalez-Rodriguez MP. Comparison of regional bond strength in root thirds among fiber-reinforced posts luted with different cements. J Biomed Mater Res B Appl Biomater. 2007;83:364–72.
Mazzitelli C, Monticelli F, Toledano M, Ferrari M, Osorio R. Effect of thermal cycling on the bond strength of self-adhesive cements to fiber posts. Clin Oral Investig. 2012;16:909–15.
Pereira JR, Lins do Valle A, Ghizoni JS, Lorenzoni FC, Ramos MB, Dos Reis So MV. Push-out bond strengths of different dental cements used to cement glass fiber posts. J Prosthet Dent. 2013; 110:134–40.
Rasimick BJ, Wan J, Musikant BL, Deutsch AS. A review of failure modes in teeth restored with adhesively luted endodontic dowels. J Prosthodont. 2010;19:639–46.
Perdigao J, Gomes G, Augusto V. The effect of dowel space on the bond strengths of fiber posts. J Prosthodont. 2007;16:154–64.
Erhardt MC, Cavalcante LM, Pimenta LA. Influence of phosphoric acid pretreatment on self-etching bond strengths. J Esthet Restor Dent. 2004; 16:33,40 (discussion 41).
Tay FR, Pashley DH. Aggressiveness of contemporary self-etching systems. I: depth of penetration beyond dentin smear layers. Dent Mater. 2001;17:296–308.
Mazzitelli C, Monticelli F, Toledano M, Ferrari M, Osorio R. Dentin treatment effects on the bonding performance of self-adhesive resin cements. Eur J Oral Sci. 2010;118:80–6.
Tonial D, Ghiggi PC, Lise AA, Burnett LH Jr, Oshima HM, Spohr AM. Effect of conditioner on microtensile bond strength of self-adhesive resin cements to dentin. Stomatologija. 2010;12:73–9.
Pisani-Proenca J, Erhardt MC, Amaral R, Valandro LF, Bottino MA, Del Castillo-Salmeron R. Influence of different surface conditioning protocols on microtensile bond strength of self-adhesive resin cements to dentin. J Prosthet Dent. 2011;105:227–35.
Faria-e-Silva AL, Menezes Mde S, Silva FP, Reis GR, Moraes RR. Intra-radicular dentin treatments and retention of fiber posts with self-adhesive resin cements. Braz Oral Res. 2013; 27:14–9.
Demiryürek EÖ, Külünk Ş, Saraç D, Yüksel G, Bulucu B. Effect of different surface treatments on the push-out bond strength of fiber post to root canal dentin. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:e74–80.
Cantoro A, Goracci C, Vichi A, Mazzoni A, Fadda GM, Ferrari M. Retentive strength and sealing ability of new self-adhesive resin cements in fiber post luting. Dent Mater. 2011;27:e197–204.
Perdigao J, Lambrechts P, Van Meerbeek B, Vanherle G, Lopes AL. Field emission SEM comparison of four postfixation drying techniques for human dentin. J Biomed Mater Res. 1995;29:1111–20.
Leme AA, Coutinho M, Insaurralde AF, Scaffa PM, da Silva LM. The influence of time and cement type on push-out bond strength of fiber posts to root dentin. Oper Dent. 2011;36:643–8.
Bitter K, Eirich W, Neumann K, Weiger R, Krastl G. Effect of cleaning method, luting agent and preparation procedure on the retention of fibre posts. Int Endod J. 2012;45:1116–26.
Naumann M, Koelpin M, Beuer F, Meyer-Lueckel H. 10-year survival evaluation for glass-fiber-supported postendodontic restoration: a prospective observational clinical study. J Endod. 2012;38:432–5.
Suyama Y, de Munck J, Cardoso MV, Yamada T, Van Meerbeek B. Bond durability of self-adhesive composite cements to dentine. J Dent. 2013;41:908–17.
Viotti RG, Kasaz A, Pena CE, Alexandre RS, Arrais CA, Reis AF. Microtensile bond strength of new self-adhesive luting agents and conventional multistep systems. J Prosthet Dent. 2009;102:306–12.
Bitter K, Perdigao J, Exner M, Neumann K, Kielbassa A, Sterzenbach G. Reliability of fiber post bonding to root canal dentin after simulated clinical function in vitro. Oper Dent. 2012;37:397–405.
Kadam A, Pujar M, Patil C. Evaluation of push-out bond strength of two fiber-reinforced composite posts systems using two luting cements in vitro. J Conserv Dent. 2013;16:444–8.
Rathke A, Tymina Y, Haller B. Effect of different surface treatments on the composite-composite repair bond strength. Clin Oral Investig. 2009;13:317–23.
Calixto LR, Bandeca MC, Clavijo V, Andrade MF, Vaz LG, Campos EA. Effect of resin cement system and root region on the push-out bond strength of a translucent fiber post. Oper Dent. 2012;37:80–6.
Pavan S, dos Santos PH, Berger S, Bedran-Russo AK. The effect of dentin pretreatment on the microtensile bond strength of self-adhesive resin cements. J Prosthet Dent. 2010;104:258–64.
Stona P, Borges GA, Montes MA, Junior LH, Weber JB, Spohr AM. Effect of polyacrylic acid on the interface and bond strength of self-adhesive resin cements to dentin. J Adhes Dent. 2013;15:221–7.
Han L, Okamoto A, Fukushima M, Okiji T. Evaluation of physical properties and surface degradation of self-adhesive resin cements. Dent Mater J. 2007;26:906–14.
Tanumiharja M, Burrow MF, Tyas MJ. Microtensile bond strengths of glass ionomer (polyalkenoate) cements to dentine using four conditioners. J Dent. 2000;28:361–6.
Ballal NV, Mala K, Bhat KS. Evaluation of decalcifying effect of maleic acid and EDTA on root canal dentin using energy dispersive spectrometer. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:e78–84.
Cobankara FK, Erdogan H, Hamurcu M. Effects of chelating agents on the mineral content of root canal dentin. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:e149–54.
Montanari M, Prati C, Piana G. Differential hydrolytic degradation of dentin bonds when luting carbon fiber posts to the root canal. Med Oral Patol Oral Cir Bucal. 2011;16:e411–7.
Lopes GC, Ballarin A, Baratieri LN. Bond strength and fracture analysis between resin cements and root canal dentin. Aust Endod J. 2012;38:14–20.
Ryou H, Romberg E, Pashley DH, Tay FR, Arola D. Importance of age on the dynamic mechanical behavior of intertubular and peritubular dentin. J Mech Behav Biomed Mater. 2015;42:229–42.
Ho YC, Lai YL, Chou IC, Yang SF, Lee SY. Effects of light attenuation by fibre posts on polymerization of a dual-cured resin cement and microleakage of post-restored teeth. J Dent. 2011;39:309–15.
Wang VJ, Chen YM, Yip KH, Smales RJ, Meng QF, Chen L. Effect of two fiber post types and two luting cement systems on regional post retention using the push-out test. Dent Mater. 2008;24:372–7.
Zicari F, Couthino E, De Munck J, Poitevin A, Scotti R, Naert I, Van Meerbeek B. Bonding effectiveness and sealing ability of fiber-post bonding. Dent Mater. 2008;24:967–77.
Haddad MF, Rocha EP, Assuncao WG. Cementation of prosthetic restorations: from conventional cementation to dental bonding concept. J Craniofac Surg. 2011;22:952–8.
Makkar S, Malhotra N. Self-adhesive resin cements: a new perspective in luting technology. Dent Update. 2013; 40:758–60, 763–4, 767–8.
Acknowledgments
The authors would like to thank 3M ESPE for the donation of the materials used in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Baena, E., Flores, A. & Ceballos, L. Influence of root dentin treatment on the push-out bond strength of fiber posts. Odontology 105, 170–177 (2017). https://doi.org/10.1007/s10266-016-0252-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10266-016-0252-7