Abstract
The objective of this study was to assess the bonding performance of a new universal self-adhesive cement RelyX Unicem (RXU) to dentin and enamel compared to four currently used luting systems, using a shear bond strength test with and without thermocycling. Median bond strengths were determined after 24 h storage, and after thermocycling (6,000 cycles, 5–55°C) for RXU and compared to Syntac/Variolink II (SynC/V) as a standard for luting conventional ceramics, ED-Primer II/Panavia F2.0 (EDII/PF2), Prime&Bond NT/Dyract Cem Plus (PBNT/DyCP), and a glass ionomer cement, Ketac Cem (KetC), as a standard for luting high-strength ceramic and metal-based restorations. Data (n=10 per group) were statistically analyzed using the Mann–Whitney–Wilcoxon test at the 0.05 level of significance. The bond strength (MPa) of RXU to dentin (10.8) was not statistically different from those of SynC/V (15.1), EDII/PF2 (10.5) or PBNT/DyCP (10.1), and statistically higher than KetC (4.1). The bond strength of RXU to enamel (14.5) was significantly lower than those of SynC/V (32.8), EDII/PF2 (23.6), and PBNT/DyCP (17.8), but higher than KetC (6.1). After thermocycling, the bond strength of RXU to enamel significantly decreased, but was still significantly higher than that of KetC. RelyX Unicem may be considered an alternative to Ketac Cem for high-strength ceramic or metal-based restorations, and may be used for luting conventional ceramic crowns with little or no enamel left.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The spectrum of materials for indirectly restoring lost tooth structures has been extended during recent decades to ceramics being used without any metal support, mainly because of their superior esthetical properties. Silica-based ceramics, one of the first ceramics used metal-free, require, however, an adhesive bond to tooth structures to prevent fracturing and, therefore, special luting procedures and luting materials are necessary [2–4]. This bonding/luting procedure requires several sequential steps and the use of rubber dam is highly recommended. Therefore, the whole method is regarded as technique-sensitive [7, 33].
Furthermore, new ceramics with improved mechanical properties based on alumina and zirconia, extending the indications of ceramic materials from crowns or inlays to small fixed prostheses, require again a different luting procedure and different luting materials. Procedures known for silica-based ceramics cannot be applied to these materials due to the reduced solubility and different chemical structure [14]. Acid etching; e.g., by hydrofluoric acid (HF), and silanization, which leads to high bond values between silica-based ceramics and the luting material, does not provide any bond with alumina or zirconia ceramic [14]. Conventional cements; e.g., glass ionomer cements, have been recommended for luting these ceramics [21]. However, the bonding forces of these cements to tooth structures are lower than using an adhesive system together with a resin-based luting material [23]. Compomer luting materials with higher bond strengths to dentin (12.5 MPa) than those of resin-modified glass ionomer cements (7.6 MPa) [19] have been recommended, but these materials are still recommended to be used with an adhesive system.
Thus, the clinician faces the problem of technique sensitivity of luting procedures as well as the problem that different luting materials/procedures have to be applied, depending on the restoration material chosen with the ideal luting material not yet available. In order to help solve these problems, a new resin luting material RelyX Unicem, 3M ESPE (RXU), has been marketed to be used in one step, thereby avoiding technique sensitivity, and which is claimed by the manufacturer to be suitable for all restorative materials. The self-adhesive properties are claimed to be based upon phosphoric-acid methacrylates that demineralize and infiltrate the tooth substrate, resulting in micromechanical retention. Secondary reactions have been suggested to provide chemical adhesion to hydroxyapatite [31]. The basic inorganic fillers are able to undergo a cement reaction with the phosphoric-acid methacrylates. The dominant setting reaction starts with free radical polymerization, which can be initiated either by light or by a redox system (dual-curing composite materials) [31].
Successful bonding of the luting material to both the restorative material and the tooth structures is imperative for the retention of the restoration [25] and for good marginal adaptation [18]. Bonding has also to withstand the contraction forces of the luting resin during polymerization [26]. Bond strengths to sandblasted alumina-based high-strength ceramic (Procera AllCeram) have been reported to be higher for RXU (5.9 MPa) and Panavia F (PF) (8.0 MPa) than for Variolink II (V) (0.9 MPa) [24]. Similarly, bond strength values to high-gold-content alloys were higher for RXU (9.2 MPa) and PF (10.0 MPa) than V (5.4 MPa) [24]. On the other hand, bond strength values to the HF-etched and silanized lithium disilicate ceramic (IPS Empress 2) were higher for V (17.2 MPa) and RXU (16.8 MPa) than PF (10 MPa) [24]. These data show that RXU may be considered a suitable luting material for both types of ceramic, if bond strength data to the tooth substrate are in the range of the standard luting procedures described earlier.
First microtensile bond strength tests of RXU to enamel after 24 h water storage have shown that values in enamel (19.6 MPa) were significantly lower compared to PF, whereas no significant difference was found in dentin (16.9 MPa) [6].
No long term clinical experience exists with this new luting material. However, it is known that with time bonding to restorative materials as well as to tooth structures may undergo hydrolytical degradation resulting in bond failure [29]. A widely-used method to accelerate this degradation process in vitro is to submit test samples to a thermocycling treatment stress [9, 10].
The objective of this study was to test the following hypotheses: 1. The use of RelyX Unicem with its simplified application procedure can be considered an alternative to the currently used systems for luting conventional ceramics and those for luting metal-based and high-strength ceramic restorations. Therefore, the shear bond strengths of RelyX Unicem to both dentin and enamel with and without thermocycling were compared to those of three current resin-based luting systems, with their corresponding smear-layer removing or smear-layer dissolving adhesive systems, and one glass ionomer cement; 2. Thermal stress influences the bond strength between a luting material and different tooth structures.
Materials and methods
Preparation of the specimens
200 non-carious human third molars were collected in 0.5% Chloramine solution, cleaned and stored in distilled water (4°C) for a maximum of 6 months until use. The teeth were embedded in chemically cured acrylic resin (Sampl Kwick, Buehler, Lake Bluff, Ill, USA). They were ground flat with a series of SiC-papers ending with 600 grit used on a polisher (Polimet, Buehler) to either obtain about a 4 mm diameter flat buccal dentin surface at 1.5–2.0 mm distance from the pulp, or a flat enamel surface. For each type of substrate, the specimens (n=100) were randomly divided into ten groups of ten specimens each (with and without thermocycling for each of the five luting systems).
Bonding procedure
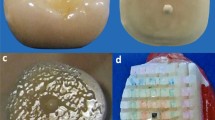
Four resin-based luting systems (RelyX Unicem (RXU) [3M ESPE, Seefeld, Germany], Syntac/Variolink II (SynC/V) [Vivadent, Schaan, Liechtenstein], ED-Primer II/Panavia F 2.0 (EDII/PF2) [Kuraray Medical, Okayama, Japan], the compomer system Prime&Bond NT/Dyract Cem Plus (PBNT/DyCP) [DeTrey Dentsply, Konstanz, Germany]), and one glass ionomer cement (Ketac Cem Maxicap (KetC) [3M ESPE]) were investigated. The compositions of the materials are listed in Table 1, and their application protocols are listed in Table 2. After appropriate surface treatment, a polytetrafluoroethylene mold was used to create a rod of luting cement (3 mm bonding diameter, 4 mm height) on all pretreated tooth surfaces. The composite resin luting materials were placed in two increments and each increment was light-cured for 40 s (Spectrum TM curing light, Dentsply, USA). The intensity of the light (500 mW/cm2) was controlled by a radiometer (Caulk Dentsply, Milford, DE, USA). Before shear bond-strength measurement, the specimens of each luting system and for each type of substrate, were either stored at 37°C in distilled water for 24 h, or underwent thermocycling (TC) for a total of 6,000 cycles (5–55°C, dwell time: 2 min) [10].
Shear bond strength test
Shear bond strength was determined according to ISO/TS 11405:2003 [10] using a Universal Testing Machine (Zwick 010, Ulm, Germany) at a cross head speed of 0.75 mm/min. A chisel-shaped rod was placed at a distance of 200 μm from and parallel to the tooth substrate–adhesive interface. Bond strength was calculated in megapascals (MPa). Bond failure sites were inspected visually under a stereomicroscope (Wild M420, Leica Heerbrugg, Switzerland) at ×32 magnification to determine fracture modes. The fracture mode of each specimen was observed and classified into one of three categories:
-
Adh/Padh: Complete adhesive fracture at the resin–tooth substrate interface and/or partial adhesive fracture, where remnants of the luting material remained adherent to the substrate surface.
-
CohC: cohesive fracture in the luting material.
-
Adh/CohC: mixed fracture mode; adhesive fracture at the resin–tooth substrate interface combined with cohesive fracture in the luting material.
Statistical analysis
Medians and 25% and 75% quartiles were determined from ten replications of each experimental group and pairwise comparisons between groups were performed using the Mann–Whitney–Wilcoxon rank sum test (SPSS PC+, version 5.01, SPSS Inc, Chicago, Ill, USA) at the 0.05 level of significance (α). In order to assess the influence of thermocycling and the tooth substrate in general and irrespective of all other parameters, the levels of significance were adjusted to α*(k)=1−(1−α)1/k (k=number of performed pairwise tests) using the error rates method [16].
Results
Shear bond strength to dentin
The median shear bond strengths of different luting systems to dentin, either with or without thermocycling, as well as the corresponding 25% to 75% quartiles are shown in Fig. 1 as well as the results of pairwise comparisons for the luting systems vs. each other.
Regarding the bond strength to dentin without thermocycling, RXU produced a median bond strength to dentin (10.8 MPa), which was not significantly different from SynC/V (15.1 MPa), EDII/PF2 (10.5 MPa) or PBNT/DyCP (10.1 MPa) and significantly higher than for KetC (4.1 MPa). The bond strength of SynC/V was statistically higher than that of EDII/PF2. After thermocycling, RXU (14.9 MPa) showed significantly higher bond strength data than EDII/PF2 (7.4 MPa) and KetC (4.6 MPa), but the data were significantly lower than that of SynC/V (19.8 MPa).
Shear bond strength to enamel
The median shear bond strengths of different luting systems to enamel, either with or without thermocycling, as well as the corresponding 25% to 75% quartiles are shown in Fig. 2 as well as the results of pairwise comparisons for the luting systems vs. each other.
Median (with 25–75% percentiles) shear bond strength values of different luting systems to enamel, with and without thermocycling. Lines indicate significant differences between groups (P≤0.05). ― without TC, --- with TC, TC effect. *Ketac Cem was statistically lower than all other luting cements either with or without TC and it was not indicated with lines
Regarding the bond strength to enamel without thermocycling, RXU produced a bond strength to enamel (14.5 MPa), which was significantly lower than all other resin luting systems, but higher than KetC (6.1 MPa). SynC/V showed the statistically highest bond strength (32.8 MPa), followed by EDII/PF2 (23.6 MPa), and PBNT/DyCP (17.8 MPa). After thermocycling, RXU still produced a statistically lower bond strength value (6.6 MPa) than all other resin luting systems, SynC/V (27 MPa), EDII/PF2 (21.2 MPa), PBNT/DyCP (17 MPa), but higher than KetC (1.9 MPa).
Effect of the tooth substrate on the bond strength
For each luting system (without thermocycling), the bond strength to enamel was statistically higher than that of dentin except for RXU, where there was no significant difference. After thermocycling, the bond strengths to enamel were statistically higher than those of dentin except for RXU and KetC, where bond strengths to enamel were significantly lower than those to dentin. In general, the error rates method indicated that the type of the tooth substrate significantly affected the bond strength to tooth structure, irrespective of the thermocycling treatment or the type of the luting system.
Effect of thermocycling on the shear bond strength
Results of pairwise comparisons for no thermocycling vs. thermocycling are shown in Figs. 1 and 2. Regarding the bond strength to dentin, thermocycling had no significant effect on the bond strength of any of the luting systems to dentin except SynC/V. The bond strength of SynC/V to dentin was significantly increased after thermocycling. On the other hand, thermocycling significantly decreased the bond strength of only RXU and KetC to enamel. In general, the error-rates method indicated that thermocycling did not significantly affect the bond strength to dentin, whereas it significantly affected the bond strength to enamel, irrespective of the type of the luting system.
The recorded fracture modes are listed in Table 3. Regarding bonding to dentin, the fracture mode of all the luting systems to dentin was mostly Adh/Padh. Regarding bonding to enamel, most of the specimens of RXU, KetC and PBNT/DyrCP had an adhesive fracture (Adh/Padh), whereas the mixed fracture mode (Adh/CohC) was mostly observed for SynC/V and EDII/PF2.
Discussion
The stresses at the restoration–tooth interface are complex, but they can be identified as mainly a tensile or shear type of stress [22]. Therefore, the shear bond strength test was used in this study according to ISO/TS 11405:2003 [10]. The luting systems were applied on the dentin and enamel surfaces without any restorative materials in order to get pure bond strength data to the tooth structure without any interacting bonding effects of the restorative materials.
Bond strength to dentin
The results of the present study (Fig. 1) showed that RXU produced a bond strength to dentin, which was not statistically different from the other resin based luting materials and statistically higher than that of KetC. These results are in line with the data from literature. Using the microtensile bond strength test, Johnson et al. observed no statistically significant difference between EDII/PF2 (17.2 MPa) and RXU (16.1 MPa) [12]. Similar data were found in another study [6].
The results of the present study showed that the bond strength of EDII/PF2 to dentin was significantly lower than for SynC/V, which is again in accordance with the literature [6, 11, 15, 20]. One reason may be the high filler content and viscosity of the PF2 luting resin, which may decrease the depth of penetration into the primed dentin [15, 17]. There may have also been an increased adhesive permeability of one-step and two-step adhesive systems. The slow rate of polymerization in the dual cured mode allows water to diffuse from the dentin across the ED Primer, and form water droplets along the primer–composite interface [5]. Additionally, the remaining acids of ED primer may have inhibited the chemical curing of the cement [27].
The results of the present study (Fig. 1) showed that the bond strength of compomer-based luting cement PBNT/DyCP to dentin without thermocycling was not statistically different from any other resin-based luting cement but higher than KetC. However, after thermocycling, a high variation of data was found. This may be explained by, firstly, the technique sensitivity of total etch systems especially with absence of water in the solvent [7], secondly, the increased adhesive permeability for water of simplified adhesive systems, when used with chemically cured resins [30] and, thirdly, the possible acid–base reaction between the uncured acidic resin monomers of the PBNT adhesive inhibition layer and the initiator components of the chemically cured Dyract Cem Plus [27].
Bond strength to enamel
The results of the present study (Fig. 2) showed that the bond strength of RXU to enamel was statistically lower than all other luting resins, but higher than KetC. After thermocycling, the bond strength of RXU significantly decreased, but was still significantly higher than that of KetC. Our results are in line with the findings of other studies. Using the microtensile bond strength test, De Munck et al. found that the bond strength of RXU to enamel (19.6 MPa) was statistically lower than for ED/PF (35.4 MPa) [6]. In another study, the microtensile bond strength of RXU to enamel (16.1 MPa) was statistically lower than for EDII/PF2 (31.0 MPa) [12].
On the other hand, SynC/V, without thermocycling, produced the statistically highest bond strength to enamel, followed by EDII/PF2. It is well reported that acid etching provides the most reliable bond strength to enamel [28]. When phosphoric acid is applied, the preferential etching of interprismatic enamel permits creation of 1 μm wide resin tags as well as resin infiltration within the surface of prisms to produce enamel hybrid layers. In contrast, the self-etching primer adhesive systems only produced resin infiltration into enamel to a depth of 0.6–0.7 μm [1, 8]. However, this shallow resin penetration (nanometer-sized resin tags) provided good resin–enamel bond strengths. The microtensile bond strength to enamel of the total etch adhesive system One step, Bisco, USA (46.2 MPa) was not significantly different from that of the self-etching primer adhesive system Clearfil SE Bond, Kuraray Medical, Japan (39.8 MPa) [8].
The results of the present study showed that bond strength of compomer-based luting cement, PBNT/DyCP to enamel, without thermocycling, was statistically lower than SynC/V, EDII/PF2 and higher than RXU. Although the enamel was acid-etched by De Trey conditioner 36, the bond strength was statistically lower than that of SynC/V. This may be due to the possible chemical interaction as mentioned above in the case of dentin [27].
Effect of tooth substrate on bond strength
The error-rates method showed that the type of the tooth substrate affected the bond strength of the tested luting systems. Therefore, our data suggest that RXU may be used for luting conventional all-ceramic crowns, if a large dentin surface [13] and no or little enamel is left. Looking upon the bond strength data to enamel, RXU may not be the ideal material for luting inlays and partial crowns, where a considerable enamel surface area is present. However, it has to be considered that RXU, at least without thermocycling, seems to be the only material which provides similar bond strength values to dentin and to enamel and, which was shown in former studies [24], to both types of ceramics. This may cause a more uniform stress distribution in the clinical situation than that caused by large differences in bond strengths between the different substrates. Future research is needed on this topic.
Influence of thermocycling on bond strength
The error-rates method showed that thermocycling, in general, did not affect bond strength to dentin, whereas it affected bond strength to enamel. Thermocycling and the resulting thermal stresses significantly decreased the bond strength of RXU and KetC to enamel. Apparently, the bonding between these materials and enamel is not sufficient to withstand the thermocycling stress. A combination of factors may have contributed to the magnitude of this effect. For example, the difference in thermal conductivity and the coefficient of thermal expansion between the tooth structure and each restorative material versus the initial bond strength between luting material and tooth substrate to withstand the fatigue created by any developed thermal stresses. It has been reported that the enamel and dentin thermal conductivities (×10−3) are 0.22 and 0.15 cal/mm s °C and their coefficients of thermal expansion (×10−6) are 10 and 11.4 l/°C, respectively [32]. Regarding RXU and KetC, the values of these properties were not reported in the literature, however, the coefficients of thermal expansion of composites and glass ionomer cements have been reported to be generally higher than those of enamel and dentin (e.g. 81×10−6 and 35×10−61/°C) [32].
Conclusions
Within the limitations of this in vitro study, the use of RelyX Unicem with its simplified application procedure may be considered an alternative to the currently used systems for luting conventional ceramics, high-strength ceramics and metal-based restorations, when no or little enamel is left. Thermocycling does not significantly affect the bond strength of the tested luting systems to dentin, whereas it significantly affects their bond strengths to enamel.
References
Asmussen E (1977) Penetration of restorative resins into acid etched enamel: I. Viscosity, surface tension and contact angle of restorative resin monomers. Acta Odontol Scand 35:175–182
Burke FJ (1995) The effect of variations in bonding procedure on fracture resistance of dentin-bonded all-ceramic crowns. Quintessence Int 26:293–300
Burke FJ (1996) Fracture resistance of teeth restored with dentin-bonded crowns: the effect of increased tooth preparation. Quintessence Int 27:115–121
Burke FJ, Fleming GJ, Nathanson D, Marquis PM (2002) Are adhesive technologies needed to support ceramics? An assessment of the current evidence. J Adhes Dent 4:7–22
Carvalho RM, Pegoraro TA, Tay FR, Pegoraro LF, Silva NRFA, Pashley DH (2004) Adhesive permeability affects coupling of resin cements that utilise self-etching primers to dentine. J Dent 32:55–65
De Munck J, Vargas M, Van Landuyt K, Hikitaa K, Lambrechts P, Van Meerbeek B (2004) Bonding of an auto-adhesive luting material to enamel and dentin. Dent Mater 20:963–971
Frankenberger R, Kramer N, Petschelt A (2000) Technique sensitivity of dentin bonding: effect of application mistakes on bond strength and marginal adaptation. Oper Dent 25:324–330
Hashimoto M, Ohno H, Yoshida E, Hori M, Sano H, Kaga M, Oguchi H (2003) Resin–enamel bonds made with self-etching primers on ground enamel. Eur J Oral Sci 111:447–453
Helvatjoglu-Antoniades M, Koliniotou-Kubia E, Dionyssopoulos P (2004) The effect of thermal cycling on the bovine dentine shear bond strength of current adhesive systems. J Oral Rehabil 31:911–917
ISO (International Organization for Standardization): ISO/TS 11405: 2003, Dental Materials-Testing of adhesion to tooth structure
Jayasooriya PR, Pereira PN, Nikaido T, Tagami J (2003) Efficacy of a resin coating on bond strengths of resin cement to dentin. J Esthet Restor Dent 15:105–113
Johnson JC, Burgess JO, Blatz MB (2004) Bond of new resin cements to enamel, dentin, and alumina. J Dent Res 83(Spec Issue A): abstract #474
Kantorowicz GF (1993) Inlays, crowns & bridges–a clinical handbook, 5th edn. Butterworth-Heinemann Ltd, Oxford
Kern M, Wegner SM (1998) Bonding to zirconia ceramic: adhesion methods and their durability. Dent Mater 14:64–71
Mak YF, Lai SC, Cheung GS, Chan AW, Tay FR, Pashley DH (2002) Micro-tensile bond testing of resin cements to dentin and an indirect resin composite. Dent Mater 18:609–621
Miller RG (1981) Simultaneous statistical inference. Springer, Berlin Heidelberg New York
Miyazaki M, Ando S, Hinoura K, Onose H, Moore BK (1995) Influence of filler addition to bonding agents on shear bond strength to bovine dentin. Dent Mater 11:234–238
Mota CS, Demarco FF, Camacho GB, Powers JM (2003) Microleakage in ceramic inlays luted with different resin cements. J Adhes Dent 5:63–70
Mujdeci A, Gokay O (2004) The effect of airborne-particle abrasion on the shear bond strength of four restorative materials to enamel and dentin. J Prosthet Dent 92:245–249
Nikaido T, Cho E, Nakajima M, Tashiro H, Toba S, Burrow MF, Tagami J (2003) Tensile bond strengths of resin cements to bovine dentin using resin coating. Am J Dent 16:41A–46A
Oden A, Andersson M, Krystek-Ondracek I, Magnusson D (1998) Five year clinical evaluation of Procera All Ceram crowns. J Prosthet Dent 80:450–456
Oilo G (1993) Bond strength testing—what does it mean? Inter Dent J 43:492–498
Pereira LC, Nunes MC, Dibb RG, Powers JM, Roulet JF, Navarro MF (2002) Mechanical properties and bond strength of glass-ionomer cements. J Adhes Dent 4:73–80
Piwowarczyk A, Lauer HC, Sorensen JA (2004) In vitro shear bond strength of cementing agents to fixed prosthodontic restorative materials. J Prosthet Dent 92:265–273
Rosenstiel SF, Land MF, Crispin BJ (1998) Dental luting agents: a review of the current literature. J Prosthet Dent 80:280–301
Sakaguchi RL, Peters MC, Nelson SR, Douglas WH, Poort HW (1992) Effects of polymerization contraction in composite restorations. J Dent 20:178–182
Sanares AM, Itthagarun A, King NM, Tay FR, Pashley DH (2001) Adverse surface interactions between one-bottle light-cured adhesives and chemical-cured composites. Dent Mater 17:542–556
Swift EJ, Perdigao J, Heymann HO (1995) Bonding to enamel and dentin: a brief history and state of the art. Quintessence Int 26:95–110
Tay FR, Hashimoto M, Pashley DH, Peters MC, Lai SC, Yiu CK, Cheong C (2003) Aging affects two modes of nanoleakage expression in bonded dentin. J Dent Res 82:537–541
Tay FR, Frankenberger R, Krejcic I, Bouillaguet S, Pashley DH, Carvalho RM, Laia CNS (2004) Single-bottle adhesives behave as permeable membranes after polymerization: I. In vivo evidence. J Dent 32:611–621
Technical data sheet: Espertise RelyX Unicem (2002) 3M ESPE, Seefeld Germany
Toparli M, Gokay N, Aksoy T (2000) An investigation of temperature and stress distribution on a restored maxillary second premolar tooth using a three-dimensional finite element method. J Oral Rehabil 27:1077–1081
Van Meerbeek B, De Munck J, Yoshida Y, Inoue S, Vargas M, Vijay P, Van Landuyt K, Lambrechts P, Vanherle G (2003) Buonocore memorial lecture. Adhesion to enamel and dentin: current status and future challenges. Oper Dent 28:215–235
Wada T (1986) Development of a new adhesive material and its properties. In: Gettleman L, Vrijhoef MMA, Uchiyama Y (eds) Proceedings of the International Symposium on Adhesive Prosthodontics, Amsterdam, Netherlands. Academy of Dental Materials, Chicago, pp 9–18
Williams D (1997) Ceramics transformed: manipulating crystal structures to toughen bioceramics. Med Device Technol 8:6–8
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Abo-Hamar, S.E., Hiller, KA., Jung, H. et al. Bond strength of a new universal self-adhesive resin luting cement to dentin and enamel. Clin Oral Invest 9, 161–167 (2005). https://doi.org/10.1007/s00784-005-0308-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-005-0308-5