Abstract
Background
Few epidemiologic studies on acute kidney injury (AKI) have focused on the older adult population. This study aimed to clarify the characteristics and risk factors for AKI in this population.
Methods
This retrospective observational study was performed with the clinical data of all outpatients and inpatients aged ≥ 65 years at the time of enrolment at Kochi Medical School Hospital between 1 January 1981 and 31 December 2021. The primary cohort was divided into those aged 65–74 and ≥ 75 years. The primary outcome was the occurrence of AKI.
Results
Of 83,822 patients, 38,333 were included in the 65–74-year-old group, whereas 45,489 were included in the ≥ 75-year-old group. Prevalences of the first AKI event in the 65–74-year-old and ≥ 75-year-old groups were 11.9% and 12.4%, respectively. Overall, lower estimated glomerular filtration rate, lower albumin level, lower or higher level of serum uric acid, and histories of diabetes mellitus, chronic heart failure, ischaemic heart disease, non-ischaemic heart disease, cerebrovascular disease, cancer, and liver disease were independent risk factors for an AKI event. The risk factors for AKI unique to each cohort were using non-steroidal anti-inflammatory drugs (NSAIDs) and loop diuretics (L-DI), and histories of hypertension (HT) and vascular diseases (VD) in men aged 65–74 years; using NSAIDs, angiotensin-converting enzyme inhibitors (ACEIs), L-DI and other diuretics (O-DI), and histories of HT and VD in men aged ≥ 75 years; using NSAIDs and O-DI and not using angiotensin-receptor blockers (ARBs), and a history of HT in women aged 65–74 years; and use of L-DI and a history of VD in women aged ≥ 75 years. Presence of proteinuria was a risk factor for developing AKI.
Conclusions
Many AKI risk factors reported thus far are associated with AKI development. However, there are differences in the effects of the renin-angiotensin system inhibitors, ACEIs, and ARBs (ARBs may be protective). Additionally, the U-shaped relationship between AKI onset and uric acid levels differs between sexes in the elderly population, similar to other age groups, but this sex difference disappears in the very elderly population. Pre-existing chronic kidney disease is a risk factor for the development of AKI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute kidney injury (AKI) is a heterogeneous group of serious conditions characterised by a rapid decrease in the glomerular filtration rate (GFR) and/or renal output [1, 2]. AKI affects approximately 10–15% of adults admitted to hospital [1, 2] and is associated with high morbidity, mortality, and health care costs [3]. The diagnostic and staging criteria for AKI were first standardised in 2004, and our understanding of the epidemiology of AKI has since improved [2, 4, 5]. Despite this progress, AKI continues to be associated with high morbidity and mortality independent of other severe conditions. Since there is currently no treatment for AKI, it is important to identify exposure and susceptibility factors [1, 2]. When identified, prevention or modification of the respective risk factors may reduce the AKI rate and severity, as recently demonstrated [1, 2].
Older age has been associated with particularly high AKI rates and has been identified as an independent risk factor for AKI [2, 6,7,8]. The decreased ability to compensate for renal insults and increased GFR reduction may cause excessive vulnerability to AKI in older persons [8, 9]. Furthermore, AKI increases the rates of chronic kidney disease (CKD) and mortality, especially in this age group [7,8,9]. However, the age cut-off for “elderly” has conventionally been deemed ≥ 65 years [10]. Therefore, the current data are limited, as participants are usually categorised as elderly persons in a single age group ≥ 65 years. Worldwide, increased life expectancy has resulted in a continuous, disproportionate and rapid growth in the population of individuals aged ≥ 75 years. Presently, people aged ≥ 75 years are considered very elderly. Additionally, most existing studies on AKI involving very elderly persons are small, and few studies have applied the current definitions of AKI and reported risk factors and outcomes. The epidemiology of AKI in the population aged ≥ 75 years is of particular interest, as interventions in this age group may be the most rewarding for the prevention of AKI.
This study aimed to clarify the characteristics and risk factors for AKI in the elderly population, with the purpose of determining whether there is a difference between the population aged 65–74 years and that aged ≥ 75 years.
Materials and methods
Ethics statements
All procedures were performed in accordance with the ethical standards of the institutional and/or national research committee at which the studies were conducted (institutional review board approval number: 23–15) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent to record and analyse data for research purposes was obtained from all study participants. Data were obtained from patients who completed a general consent form based on the opt-out policy of Kochi Medical School Hospital.
Study design and population
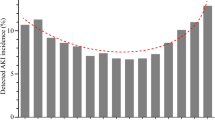
We conducted a retrospective review of data from the Retrieval system for Open Medical Analysis (RYOMA 2) data warehouse at Kochi Medical School Hospital, a 600-bed tertiary care and academic hospital in Kochi Prefecture (western Japan) [11,12,13]. All outpatients and inpatients aged ≥ 65 years at the time of enrolment at our hospital between 1 January 1981 and 31 December 2021 were evaluated for eligibility. The estimated glomerular filtration rates (eGFRs) were calculated on the basis of the patients’ serum creatinine (SCr) data using the Japanese equation for eGFR [14]. The inclusion criteria were as follows: eGFR of ≥ 30 mL/min/1.73 m2 calculated on the basis of the SCr level and measured up to 1 year before the enrolment date, and SCr level measured at least twice within 2 years from the enrolment date. We excluded patients who were aged < 65 years, who had not undergone SCr level measurement or had undergone it only once after the enrolment date, who had an eGFR of < 30 mL/min/1.73 m2 or received maintenance dialysis, and for whom accurate data on death outcomes were unavailable. In Cohort 1, we also excluded patients who had an eGFR of > 160 mL/min/1.73 m2 because a histogram plot of eGFR levels indicated that the majority of patients in our study had an eGFR of ≤ 160 mL/min/1.73 m2 (Supplementary Fig. 1). In Cohort 2, to evaluate the influence of pre-existing CKD with proteinuria on the development of AKI, we extracted patients from Cohort 1 who had a urine test result for proteinuria.
Outcomes
The primary outcome was the occurrence of AKI. The groups were divided according to the events that met the inclusion criteria. Because urine output data were not available, we defined and staged AKI according to the Kidney Disease: Improving Global Outcomes SCr-based criteria as follows: increase in SCr by ≥ 0.3 mg/dL (≥ 26.5 μmol/L) within 48 h or increase in SCr to ≥ 1.5 times baseline, which is known or presumed to have occurred within the previous 7 days [2]. All available SCr values obtained from blood tests were used to define AKI.
Data collection and covariates
Data were collected retrospectively. All data were obtained from electronic medical records. Trained doctors and research nurses completed the data input. They were unaware of the study and did not participate in the patient management or care. The following variables were considered as covariates: sex; eGFR; serum albumin (Alb); serum uric acid (SUA); presence of proteinuria (U-Prot), coded as ( −), ( ±), (1 +), (2 +), and (≥ 3 +); use of fluid infusion, non-steroidal anti-inflammatory drugs (NSAIDs), contrast agents (CAs), angiotensin-converting enzyme inhibitors (ACEIs), angiotensin-receptor blockers (ARBs), antibiotics, anticancer drugs (ACDs), loop diuretics (L-DI), thiazide diuretics (T-DI), and other diuretics (O-DI); and history of diabetes mellitus (DM), hypertension (HT), hyperlipidaemia (HL), chronic heart failure (CHF), ischaemic heart disease (IHD), non-ischaemic heart disease (non-IHD), cerebrovascular disease (CVD), other vascular diseases (VDs), cancer, liver disease, cardiac surgery (CS), thoracic surgery (TS), and vascular surgery (VS).
Statistical analysis
We conducted a descriptive analysis of AKI occurrences in the 65–74-year-old and ≥ 75-year-old groups. The Mann–Whitney U and Fisher’s exact tests were used to compare the variables. Logistic regression analysis was performed with AKI onset as the objective variable. The 65–74-year-old and ≥ 75-year-old groups were stratified on the basis of sex, and the regression analysis was performed on the four groups. Items with fewer than 10 patients were excluded from the covariates in the regression analysis. The level of significance was set at p = 0.05. All analyses were performed using R software (version 4.1.2; R Foundation for Statistical Computing, Vienna, Austria).
Results
A total of 83,822 patients satisfied the inclusion criteria. Of these, 38,333 patients did not have SCr data measured when they were ≥ 75 years of age (65–74-year-old group), whereas 45,489 patients had SCr data measured when they were ≥ 75 years of age (≥ 75-year-old group). In the 65–74-year-old group, 17,402 patients had SCr data measured twice within 1 week (Fig. 1). Of these patients, 226 experienced AKI before 65 years of age. Of the remaining patients, 2044 (11.9%) had their first AKI event between 65 and 74 years of age, and 15,132 (88.1%) did not have an AKI event. There were 1782 patients with AKI events and 12,821 patients without AKI events who had measured Alb and SUA data. Finally, in Cohort 1, there were 1742 patients with AKI events and 12,756 patients without AKI events who had an eGFR of ≤ 160 mL/min/1.73 m2. In Cohort 2, there were 1431 patients with AKI events and 10,930 patients without AKI events who had a urine test result for proteinuria. In patients aged ≥ 75 years, 23,632 had SCr data measured twice within 1 week. Of these patients, 470 developed AKI before 75 years of age. Of the remaining patients, 2862 (12.4%) had their first AKI event at ≥ 75 years of age, and 20,300 (87.6%) did not have an AKI event. There were 2632 patients with AKI events and 17,668 patients without AKI events who had measured Alb and SUA data. Finally, in Cohort 1, there were 2605 patients with AKI events and 17,618 patients without AKI events who had an eGFR of ≤ 160 mL/min/1.73 m2. In Cohort 2, there were 2096 patients with AKI events and 14,912 patients without AKI events who had a urine test result for proteinuria.
In the 65–74-year-old group of Cohort 1, the frequencies of men; VS; CS; fluid infusion; use of NSAIDs, ACEIs, ARBs, antibiotics, L-DI, T-DI, and O-DI; and histories of DM, HT, HL, CHF, IHD, non-IHD, CVD, VD, cancer, and liver disease were higher in the AKI group than in the non-AKI group (Table 1). The eGFR and Alb levels and the frequency of TS were lower and age and the SUA level was higher in the AKI group than in the non-AKI group. In the ≥ 75-year-old group, although the trends were similar to those in the 65–74-year-old group, use of NSAIDs was not a risk factor for AKI events and the frequency of TS was not statistically different between the AKI and non-AKI groups (Table 1).
As shown in Fig. 2, in men aged 65–74 years, the risks of developing AKI were lower eGFR, lower Alb level, use of NSAIDs and L-DI, and histories of DM, HT, CHF, IHD, non-IHD, CVD, VD, cancer, and liver disease. The risk of developing AKI increased when the uric acid levels were < 4 mg/dL (SUA < 2, SUA 2–3, and SUA 3–4) and ≥ 7 mg/dL (SUA > 7) compared with the reference of 5–6 mg/dL.
Risk of AKI in men aged 65–74 years in Cohort 1. The primary endpoint was AKI occurrence, which was quantified as the ratio of the serum creatinine level during the follow-up period to the baseline serum creatinine level at enrolment. The analysis was conducted using age, eGFR, Alb level, SUA level, use of drugs, and presence of comorbid diseases as covariates. The reference values for age, eGFR, Alb level, and SUA level were < 65 years, G3a, > 3.0 g/dL, and 5–6 mg/dL, respectively. AKI acute kidney injury, eGFR estimated glomerular filtration rate, Alb serum albumin, SUA serum uric acid, NSAIDs non-steroidal anti-inflammatory drugs, CA contrast agent, ACEI angiotensin-converting enzyme inhibitor, ARB angiotensin-receptor blocker, ACD anticancer drugs, L-DI loop diuretics, T-DI thiazide diuretics, O-DI other diuretics, DM diabetes mellitus, HT hypertension, HL hyperlipidaemia, CHF chronic heart failure, IHD ischaemic heart disease, non-IHD non-ischaemic heart disease, CVD cerebrovascular disease, VD other vascular disease, OR odds ratio, 95% CI 95% confidence interval
As shown in Fig. 3, in men aged ≥ 75 years, the risks of developing AKI were lower eGFR; lower Alb level; use of NSAIDs, ACEIs, L-DI, and O-DI; and histories of DM, HT, CHF, IHD, non-IHD, CVD, VD, cancer, and liver disease. The risk of developing AKI increased when the uric acid levels were < 3 mg/dL (SUA < 2 and SUA 2–3) and ≥ 6 mg/dL (SUA 6–7 and SUA > 7) compared with the reference of 5–6 mg/dL.
Risk of AKI in men aged ≥ 75 years in Cohort 1. The primary endpoint was AKI occurrence, which was quantified as the ratio of the serum creatinine level during the follow-up period to the baseline serum creatinine level at enrolment. The analysis was conducted using age, eGFR, Alb level, SUA level, use of drugs, and presence of comorbid diseases as covariates. The reference values for age, eGFR, Alb level, and SUA level were < 65 years, G3a, > 3.0 g/dL, and 5–6 mg/dL, respectively. AKI acute kidney injury, eGFR estimated glomerular filtration rate, Alb serum albumin, SUA serum uric acid, NSAIDs non-steroidal anti-inflammatory drugs, ACEI angiotensin-converting enzyme inhibitor, ARB angiotensin-receptor blocker, ACD anticancer drug, L-DI loop diuretics, T-DI thiazide diuretics, O-DI other diuretics, DM diabetes mellitus, HT hypertension, HL hyperlipidaemia, CHF chronic heart failure, IHD ischaemic heart disease, non-IHD non-ischaemic heart disease, CVD cerebrovascular disease, VD other vascular disease, OR odds ratio, 95% CI: 95% confidence interval
As shown in Fig. 4, in women aged 65–74 years, the risks of developing AKI were lower eGFR, lower Alb level, use of NSAIDs and O-DI, not using ARBs, and histories of DM, HT, CHF, IHD, non-IHD, CVD, cancer, and liver disease. The risk of developing AKI increased when the uric acid levels were < 2 mg/dL (SUA < 2), 4–5 mg/dL (SUA 4–5), and ≥ 4 mg/dL (SUA 6–7 and SUA > 7) compared with the reference of 5–6 mg/dL.
Risk of AKI in women aged 65–74 years in Cohort 1. The primary endpoint was AKI occurrence, which was quantified as the ratio of the serum creatinine level during the follow-up period to the baseline serum creatinine level at enrolment. The analysis was conducted using age, eGFR, Alb level, SUA level, use of drugs, and presence of comorbid diseases as covariates. The reference values for age, eGFR, Alb level, and SUA level were < 65 years, G3a, > 3.0 g/dL, and 5–6 mg/dL, respectively. AKI acute kidney injury, eGFR estimated glomerular filtration rate, Alb serum albumin, SUA serum uric acid, NSAIDs non-steroidal anti-inflammatory drugs, CA contrast agent, ACEI angiotensin-converting enzyme inhibitor, ARB angiotensin-receptor blocker, ACD anticancer drug, L-DI loop diuretics, T-DI thiazide diuretics, O-DI other diuretics, DM diabetes mellitus, HT hypertension, HL hyperlipidaemia, CHF chronic heart failure, IHD ischaemic heart disease, non-IHD non-ischaemic heart disease, CVD cerebrovascular disease, VD other vascular disease, OR odds ratio, 95% CI 95% confidence interval
As shown in Fig. 5, in women aged ≥ 75 years, the risks of developing AKI were lower eGFR, lower Alb level, use of L-DI, and histories of DM, CHF, IHD, non-IHD, CVD, VD, cancer, and liver disease. The risk of developing AKI increased when the uric acid levels were < 3 mg/dL (SUA < 2 and SUA 2–3) and ≥ 6 mg/dL (SUA 6–7 and SUA > 7) compared with the reference of 5–6 mg/dL.
Risk of AKI in women aged ≥ 75 years in Cohort 1. The primary endpoint was AKI occurrence, which was quantified as the ratio of the serum creatinine level during the follow-up period to the baseline serum creatinine level at enrolment. The analysis was conducted using age, eGFR, Alb level, SUA level, use of drugs, and presence of comorbid diseases as covariates. The reference values for age, eGFR, Alb level, and SUA level were < 65 years, G3a, > 3.0 g/dL, and 5–6 mg/dL, respectively. AKI acute kidney injury, eGFR estimated glomerular filtration rate, Alb serum albumin, SUA serum uric acid, NSAIDs non-steroidal anti-inflammatory drugs, ACEI angiotensin-converting enzyme inhibitor, ARB angiotensin-receptor blocker, ACD anticancer drug, L-DI loop diuretics, T-DI thiazide diuretics, O-DI other diuretics, DM diabetes mellitus, HT hypertension, HL hyperlipidaemia, CHF chronic heart failure, IHD ischaemic heart disease, non-IHD non-ischaemic heart disease, CVD cerebrovascular disease, VD other vascular disease, OR odds ratio, 95% CI 95% confidence interval
Characteristics of Cohort 2 are similar to those of Cohort 1, except for use of antibiotics in the ≥ 75-year-old group (Table 2). In Cohort 2, absence of proteinuria, U-Prot (−), was higher in the non-AKI group than in the AKI group, whereas presence of proteinuria, U-Prot (1 +), (2 +), and (≥ 3 +), was higher in the AKI group than in the non-AKI group (Table 2). Although the risks of developing AKI in Cohort 2 were similar to those in Cohort 1, there were some changes over tie. As shown in Fig. 6, in men aged 65–74 years, not using ARBs added to the risks of developing AKI in Cohort 2 compared with Cohort 1. As shown in Fig. 7, in men aged ≥ 75 years, there was no differences in the risks of developing AKI between Cohorts 1 and 2. As shown in Fig. 8, in women aged 65–74 years, not using ARBs added to the risks of developing AKI in Cohort 2 compared with Cohort 1, while a history of HT and uric acid levels of 4–5 mg/dL (SUA 4–5) were no longer associated with the risk of developing AKI. As shown in Fig. 9, in women aged ≥ 75 years, uric acid levels of 2–3 mg/dL (SUA 2–3) were no longer associated with the risk of developing AKI. Of note, when comparing proteinuria (−) as a reference in Cohort 2, proteinuria ( ±), (1 +), and (2 +) in men and proteinuria ( ±), (1 +), (2 +), and (≥ 3 +) in women were risk factors for developing AKI.
Risk of AKI in men aged 65–74 years in Cohort 2. The primary endpoint was AKI occurrence, which was quantified as the ratio of the serum creatinine level during the follow-up period to the baseline serum creatinine level at enrolment. The analysis was conducted using age, eGFR, Alb level, SUA level, U-Prot, use of drugs, and presence of comorbid diseases as covariates. The reference values for age, eGFR, Alb level, SUA level, and U-Prot were < 65 years, G3a, > 3.0 g/dL, 5–6 mg/dL, and (−), respectively. AKI acute kidney injury, eGFR estimated glomerular filtration rate, Alb serum albumin, SUA serum uric acid, NSAIDs non-steroidal anti-inflammatory drugs, CA contrast agent, ACEI angiotensin-converting enzyme inhibitor, ARB angiotensin-receptor blocker, ACD anticancer drugs, L-DI loop diuretics, T-DI thiazide diuretics, O-DI other diuretics, DM diabetes mellitus, HT hypertension, HL hyperlipidaemia, CHF chronic heart failure, IHD ischaemic heart disease, non-IHD non-ischaemic heart disease, CVD cerebrovascular disease, VD other vascular disease, U-Prot proteinuria, OR odds ratio, 95% CI 95% confidence interval
Risk of AKI in men aged ≥ 75 years in Cohort 2. The primary endpoint was AKI occurrence, which was quantified as the ratio of the serum creatinine level during the follow-up period to the baseline serum creatinine level at enrolment. The analysis was conducted using age, eGFR, Alb level, SUA level, U-Prot, use of drugs, and presence of comorbid diseases as covariates. The reference values for age, eGFR, Alb level, SUA level, and U-Prot were < 65 years, G3a, > 3.0 g/dL, 5–6 mg/dL, and (−), respectively. AKI acute kidney injury, eGFR estimated glomerular filtration rate, Alb serum albumin, SUA serum uric acid, NSAIDs non-steroidal anti-inflammatory drugs, ACEI angiotensin-converting enzyme inhibitor, ARB angiotensin-receptor blocker, ACD anticancer drug, L-DI loop diuretics, T-DI thiazide diuretics, O-DI other diuretics, DM diabetes mellitus, HT hypertension, HL hyperlipidaemia, CHF chronic heart failure, IHD ischaemic heart disease, non-IHD non-ischaemic heart disease, CVD cerebrovascular disease, VD other vascular disease, U-Prot proteinuria, OR odds ratio, 95% CI 95% confidence interval
Risk of AKI in women aged 65–74 years in Cohort 2. The primary endpoint was AKI occurrence, which was quantified as the ratio of the serum creatinine level during the follow-up period to the baseline serum creatinine level at enrolment. The analysis was conducted using age, eGFR, Alb level, SUA level, U-Prot, use of drugs, and presence of comorbid diseases as covariates. The reference values for age, eGFR, Alb level, SUA level, and U-Prot were < 65 years, G3a, > 3.0 g/dL, 5–6 mg/dL, and (−), respectively. AKI acute kidney injury, eGFR estimated glomerular filtration rate, Alb serum albumin, SUA serum uric acid, NSAIDs non-steroidal anti-inflammatory drugs, CA contrast agent, ACEI angiotensin-converting enzyme inhibitor, ARB angiotensin-receptor blocker, ACD anticancer drug, L-DI loop diuretics, T-DI thiazide diuretics, O-DI other diuretics, DM diabetes mellitus, HT hypertension, HL hyperlipidaemia, CHF chronic heart failure, IHD ischaemic heart disease, non-IHD non-ischaemic heart disease, CVD cerebrovascular disease, VD other vascular disease, U-Prot proteinuria, OR odds ratio, 95% CI 95% confidence interval
Risk of AKI in women aged ≥ 75 years in Cohort 2. The primary endpoint was AKI occurrence, which was quantified as the ratio of the serum creatinine level during the follow-up period to the baseline serum creatinine level at enrolment. The analysis was conducted using age, eGFR, Alb level, SUA level, U-Prot, use of drugs, and presence of comorbid diseases as covariates. The reference values for age, eGFR, Alb level, SUA level and U-Prot were < 65 years, G3a, > 3.0 g/dL, 5–6 mg/dL, and (−), respectively. AKI acute kidney injury, eGFR estimated glomerular filtration rate, Alb serum albumin, SUA serum uric acid, NSAIDs non-steroidal anti-inflammatory drugs, ACEI angiotensin-converting enzyme inhibitor, ARB angiotensin-receptor blocker, ACD anticancer drug, L-DI loop diuretics, T-DI thiazide diuretics, O-DI other diuretics, DM diabetes mellitus, HT hypertension, HL hyperlipidaemia, CHF chronic heart failure, IHD ischaemic heart disease, non-IHD non-ischaemic heart disease, CVD cerebrovascular disease, VD other vascular disease, U-Prot proteinuria, OR odds ratio, 95% CI 95% confidence interval
Discussion
Our study revealed that lower eGFR, lower Alb level, lower or higher levels of SUA, and histories of DM, CHF, IHD, non-IHD, CVD, cancer, and liver disease are independent risk factors for AKI events in all cohorts aged ≥ 65 years. The risk factors for AKI unique to each cohort were as follows: use of NSAIDs and L-DI, and histories of HT and VD in men aged 65–74 years; use of NSAIDs, ACEIs, L-DI, and O-DI, and histories of HT and VD in men aged ≥ 75 years; use of NSAIDs and O-DI, not using ARBs, and a history of HT in women aged 65–74 years; and use of L-DI, and a history of VD in women aged ≥ 75 years. Contrary to expectations, the use of CAs, ARBs, ACDs, and T-DI, and a history of HL were not risk factors for AKI events in any cohort.
AKI is more common in older individuals than in younger individuals [15, 16], and many studies have demonstrated a clear relationship between AKI and older age [6, 16]. Elderly patients with pre-existing AKI are at the highest risk of end-stage renal disease and death [7, 17]. AKI events in elderly and very elderly patients are a critical problem for short- and long-term outcomes compared with those in younger patients. In our study, the prevalences of AKI events in elderly and very elderly patients were 11.9% and 12.4%, respectively. These results show that more than 10% of patients aged 65 years or older had AKI, and in very elderly patients aged 75 years or older, AKI occurred even more frequently than in those aged 65–74 years. An age-dependent relationship for AKI was observed in both the elderly and very elderly patients in our study.
The higher incidence of AKI in elderly persons can be attributed to the age-dependent structural and functional alterations of the kidney over time and the comorbidities that accumulate with age [6, 15, 16]. The results of the age-dependent structural and functional alterations of the kidney are a reduced GFR at baseline and a diminished kidney reserve in the setting of pathophysiological challenges, making elderly patients highly vulnerable to acute stress and more likely to develop clinically relevant AKI. Additionally, elderly individuals are also more likely to suffer from CKD, congestive heart failure, HT, renovascular disease, and diabetes, and are more likely to undergo surgery (especially CS and VS). Combined with these conditions and risks, elderly patients are more likely to be exposed to nephrotoxic CAs (during cardiac or vascular arteriography), ACEIs or ARBs, and NSAIDs for osteoarthritis [10]. The combination of changes in the ageing kidney, abnormalities in other organ systems, and exposure to various pharmaceutical agents make elderly individuals more susceptible to AKI [10]. Our study showed that use of NSAIDs is a risk factor for AKI in elderly and very elderly patients, as reported previously [10]. Furthermore, our study also revealed that use of L-DI but not T-DI is a risk factor for AKI in elderly and very elderly patients. However, our study showed that, although use of ACEIs is a risk for AKI in men aged ≥ 75 years and tends to be a risk for AKI even in women aged ≥ 75 years, unexpectedly, use of ARBs is not a risk for AKI events in all cohorts aged ≥ 65 years protects against AKI in women aged 65–74 years, and tends to be protective even in men aged 65–74 years.
AKI is highly frequent in patients aged ≥ 75 years, which is the age group with the most rapid growth worldwide, i.e. the so-called “very elderly” population [18]. In the elderly population, reduced renal function at baseline and CKD were consistently and strongly associated with the development of AKI, followed by HT and CHF [18]. Renin-angiotensin system (RAS) inhibitors are used as therapies for HT or CHF. Notably, RAS inhibitors may protect elderly individuals from AKI [18]. A previous study showed that NSAID use was the only exposure associated with AKI development in the very elderly population [18]. Many studies have shown that age-related and pathologically decreased renal function and HT may be the most important risk factors for AKI development, which is consistent with previous data and current concepts of susceptibility to AKI in older persons [8, 9, 19]. CHF has the strongest association with AKI [18]. This underscores the importance of heart failure as a risk factor for the development of AKI [2, 20, 21]. These findings may be of clinical relevance, as adequate treatment for CHF, CKD, and HT, and treatment with RAS inhibitors, when indicated for other diseases, could prevent AKI in older persons. As a strong and consistent finding, previous investigators have suggested that RAS inhibitors could potentially protect against AKI in individuals aged ≥ 75 years [18]. Although experimental data indicate activation of RAS during ischaemic AKI and mitigation of AKI by RAS inhibitors, there are also concerns about hypotension or vasoplegia caused by RAS inhibitors, which may aggravate AKI [22,23,24]. Most clinical studies and meta-analyses are consistent with our data showing that the use of RAS inhibitors is associated with less frequent AKI; however, other studies have demonstrated no association between these parameters or even an adverse effect on AKI [24,25,26,27,28,29]. Therefore, the prevention of AKI using RAS inhibitors remains controversial. Our study showed that the effects of RAS inhibitors on the onset of AKI differed depending on age and sex; the impression was that ACEIs are a risk for AKI, especially in very elderly individuals and that ARBs protect against AKI, especially in elderly individuals. These results may be due to differences in the mechanisms of action on the RAS between ACEIs and ARBs, but further research is required.
In our previous study, we had observed a U-shaped relationship between SUA levels and odds ratios (ORs) of AKI risk in the population aged 18 years and older; that is, ORs were higher in both high- and low-SUA strata [30]. Furthermore, our previous study had shown that using the stratum with an SUA level of 3.5–4.0 mg/dL for women as the reference, statistical significance was found at SUA levels > 6.0 or ≤ 3.0 mg/dL, and that using the stratum with an SUA level of 5.5–6.0 mg/dL for men as the reference, statistical significance was found at SUA levels > 6.5 or ≤ 4.5 mg/dL [30]. The present study shows that a U-shaped relationship was also observed between SUA levels and ORs of AKI risk in elderly and very elderly patients. Furthermore, using the stratum with an SUA level of 5.0–6.0 mg/dL for both women and men as the reference, among elderly patients, a significant difference was observed in the OR of AKI depending on SUA level in men when the SUA level was ≤ 4 or > 7 mg/dL, and a significant difference was observed in women when the SUA level was ≤ 2 or > 4 mg/dL. However, in the very elderly group, there was a significant difference in the OR of AKI depending on SUA level in both men and women when the SUA level was ≤ 3 or > 6 mg/dL. In other words, this study reveals that the same sex-related differences in AKI risk depending on SUA level as in our previous study were observed in the elderly patients but not in the very elderly patients.
This study also demonstrated that pre-existing CKD significantly increases the incidence of AKI in both elderly and very elderly patients. We showed that the eGFR at entry was significantly lower in patients who developed AKI than in those who did not. Furthermore, our study revealed that patients with proteinuria have a high risk of developing AKI, and that the risk of developing AKI tends to increase as the level of proteinuria increases. Therefore, our study has been proven that it is important to be cautious in elderly and very elderly people with CKD who are more likely to develop AKI.
This study had several strengths and limitations. First, our comprehensive study with a large sample size may provide representative results for AKI not only in the elderly population but also in the very elderly population, as characterised by current definitions. Particularly, there are very few similar epidemiological studies on the risk of developing AKI in the very elderly population, which is expected to attract increasing attention in the future. Therefore, our study’s results are expected to have a large impact on this research field. Second, because our study was a single-centre, retrospective observational study, there may have been potential confounding factors, confounding information, and selection biases. In particular, in Cohort 2, approximately one-third of patients with AKI did not have a urine test performed; thus, we suspected that the results of Cohort 2 were likely to be more influenced by selection bias than those of Cohort 1. Additionally, in Cohort 2, men with U-Prot (≥ 3 +) were no longer at risk for AKI progression, but it cannot be ruled out whether the very lower number of men with U-Prot (≥ 3 +) influenced this result. Finally, our study used only SCr levels, but not urine output criteria, to define AKI, which may have resulted in an underestimation of AKI [31].
Conclusions
AKI is highly frequent and severe in individuals aged ≥ 65 years. Many risk factors reported thus far, such as reduced renal function at baseline, DM, and cancer, are associated with AKI development. Our study showed that elderly and very elderly individuals share many of the same risks of AKI as other age groups in previous studies. However, we revealed that there are differences in the effects of the RAS inhibitors, ACEIs and ARBs (ARBs may be protective), and that the U-shaped relationship between AKI onset and uric acid levels differs between sexes in the elderly population, similar to other age groups, but this sex difference disappears in the very elderly population. Further research is required to collect more meaningful clinical outcomes and identify more modifiable risk factors to design future strategies for AKI prevention in elderly and very elderly persons who are likely to have AKI and will account for a high proportion of the future population. Pre-existing CKD is a risk factor for the development of AKI in elderly and very elderly persons.
Data availability
Data and analysis methods for this study are included in this article. Further information may be obtained upon request to the authors.
References
Ronco C, Bellomo R, Kellum JA. Acute kidney injury. Lancet. 2019;394:1949–64.
Disease K. Improving global outcomes (KDIGO) acute kidney injury work group: KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl. 2012;2:1–138.
Xu X, Nie S, Liu Z, Chen C, Xu G, Zha Y, et al. Epidemiology and clinical correlates of AKI in Chinese hospitalized adults. Clin J Am Soc Nephrol. 2015;10:1510–8.
Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P. Acute renal failure—definition, outcome measures, animal models, fluid therapy and information technology needs: the second international consensus conference of the Acute Dialysis Quality Initiative Group. Crit Care. 2004;8:R204–12.
Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, et al. Acute kidney injury network: report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007;11:R31.
Xue JL, Daniels F, Star RA, Kimmel PL, Eggers PW, Molitoris BA, et al. Incidence and mortality of acute renal failure in medicare beneficiaries, 1992 to 2001. J Am Soc Nephrol. 2006;17:1135–42.
Ishani A, Xue JL, Himmelfarb J, Eggers PW, Kimmel PL, Molitoris BA, et al. Acute kidney injury increases risk of ESRD among elderly. J Am Soc Nephrol. 2009;20:223–8.
Anderson S, Eldadah B, Halter JB, Hazzard WR, Himmelfarb J, Horne FM, et al. Acute kidney injury in older adults. J Am Soc Nephrol. 2011;22:28–38.
Rosner MH, La Manna G, Ronco C. Acute kidney injury in the geriatric population. Contrib Nephrol. 2018;193:149–60.
Coca SG. Acute kidney injury in elderly persons. Am J Kidney Dis. 2010;56:122–31.
Hatakeyama Y, Horino T, Nagata K, Matsumoto T, Terada Y, Okuhara Y. Transition from acute kidney injury to chronic kidney disease: a single-centre cohort study. Clin Exp Nephrol. 2018;22:1281–93.
Nagata K, Horino T, Hatakeyama Y, Matsumoto T, Terada Y, Okuhara Y. Effects of transient acute kidney injury, persistent acute kidney injury and acute kidney disease on the long-term renal prognosis after an initial acute kidney injury event. Nephrol (Carlton). 2021;26:312–8.
Hatakeyama Y, Horino T, Yasui S, Komori M, Terada Y, Okuhara Y. Incidence of acute kidney injury and decreased estimated glomerular filtration rate according to the site of cancer. Clin Exp Nephrol. 2023;27:262–71.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92.
Ali T, Khan I, Simpson W, Prescott G, Townend J, Smith W, et al. Incidence and outcomes in acute kidney injury: a comprehensive population-based study. J Am Soc Nephrol. 2007;18:1292–8.
Hsu CY, McCulloch CE, Fan D, Ordonez JD, Chertow GM, Go AS. Community-based incidence of acute renal failure. Kidney Int. 2007;72:208–12.
Chertow GM, Burdick E, Honour M, Bonventre JV, Bates DW. Acute kidney injury, mortality, length of stay, and costs in hospitalized patients. J Am Soc Nephrol. 2005;16:3365–70.
Stille K, Kribben A, Herget-Rosenthal S. Incidence, severity, risk factors and outcomes of acute kidney injury in older adults: systematic review and meta-analysis. J Nephrol. 2022;35:2237–50.
Liao YB, Deng XX, Meng Y, Zhao ZG, Xiong TY, Meng XJ, et al. Predictors and outcome of acute kidney injury after transcatheter aortic valve implantation: a systematic review and meta-analysis. EuroIntervention. 2017;12:2067–74.
Ronco C, Bellasi A, Di Lullo L. Implication of acute kidney injury in heart failure. Heart Fail Clin. 2019;15:463–76.
Holgado JL, Lopez C, Fernandez A, Sauri I, Uso R, Trillo JL, et al. Acute kidney injury in heart failure: a population study. ESC Heart Fail. 2020;7:415–22.
Kontogiannis J, Burns KD. Role of AT1 angiotensin II receptors in renal ischaemic injury. Am J Physiol. 1998;274:F79–90.
Cheng SY, Chou YH, Liao FL, Lin CC, Chang FC, Liu CH, et al. Losartan reduces ensuing chronic kidney disease and mortality after acute kidney injury. Sci Rep. 2016;6:34265.
Yacoub R, Patel N, Lohr JW, Rajagopalan S, Nader N, Arora P. Acute kidney injury and death associated with renin angiotensin system blockade in cardiothoracic surgery: a meta-analysis of observational studies. Am J Kidney Dis. 2013;62:1077–86.
Cheungpasitporn W, Thongprayoon C, Srivali N, O’Corragain OA, Edmonds PJ, Ungprasert P, et al. Preoperative renin-angiotensin system inhibitors use linked to reduced acute kidney injury: a systematic review and meta-analysis. Nephrol Dial Transplant. 2015;30:978–88.
Chou YH, Huang TM, Wu VC, Chen WS, Wang CH, Chou NK, et al. Associations between preoperative continuation of renin-angiotensin system inhibitor and cardiac surgery-associated acute kidney injury: a propensity score-matching analysis. J Nephrol. 2019;32:957–66.
Whiting P, Morden A, Tomlinson LA, Caskey F, Blakeman T, Tomson C, et al. What are the risks and benefits of temporarily discontinuing medications to prevent acute kidney injury? A systematic review and meta-analysis. BMJ Open. 2017;7:e012674.
Hollmann C, Fernandes NL, Biccard BM. A systematic review of outcomes associated with withholding or continuing angiotensin-converting enzyme inhibitors and angiotensin receptor blockers before noncardiac surgery. Anesth Anal. 2018;127:678–87.
Bell S, Dekker FW, Vadiveloo T, Marwick C, Deshmukh H, Donnan PT, et al. Risk of postoperative acute kidney injury in patients undergoing orthopaedic surgery—development and validation of a risk score and effect of acute kidney injury on survival: observational cohort study. BMJ. 2015;351:h5639.
Otomo K, Horino T, Miki T, Kataoka H, Hatakeyama Y, Matsumoto T, et al. Serum uric acid level as a risk factor for acute kidney injury in hospitalized patients: a retrospective database analysis using the integrated medical information system at Kochi Medical School hospital. Clin Exp Nephrol. 2016;20:235–43.
Quan S, Pannu N, Wilson T, Ball C, Tan Z, Tonelli M, et al. Prognostic implications of adding urine output to serum creatinine measurements for staging of acute kidney injury after major surgery: a cohort study. Nephrol Dial Transplant. 2016;31:2049–56.
Author information
Authors and Affiliations
Contributions
YH, TH, and SY conceptualised and designed the study and performed the literature search. All authors collected and interpreted the data and wrote and revised the manuscript. All authors had full access to all the data in the study and accept responsibility for submitting the manuscript for publication. YH, TH, and SY had access to the raw data and verified them. Each author contributed important intellectual content during manuscript drafting or revision and agrees to be personally accountable for the individual's own contributions and to ensure that questions pertaining to the accuracy or integrity of any portion of the work, even one in which the author was not directly involved, are appropriately investigated and resolved, including with documentation in the literature if appropriate.
Corresponding author
Ethics declarations
Ethical approval
All procedures were performed in accordance with the ethical standards of the institutional and/or national research committee at which the studies were conducted (institutional review board approval number 23–15) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent to record and analyse data for research purposes was obtained from all study participants. Data were obtained from patients who completed a general consent form based on an opt-out policy at Kochi Medical School Hospital.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Hatakeyama, Y., Horino, T., Yasui, S. et al. Differences in characteristics and risk factors for acute kidney injury between elderly and very elderly patients: a retrospective review. Clin Exp Nephrol (2024). https://doi.org/10.1007/s10157-024-02512-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10157-024-02512-8