Abstract
Background
To improve outcomes in patients with chronic kidney disease (CKD), it is important to identify prognostic factors for end-stage renal disease (ESRD) as well as cardiovascular disease (CVD). This study assessed urinary concentrations of albumin, N-acetyl-β-D-glucosaminidase (NAG), and liver-type fatty acid-binding protein (L-FABP), as predictors of ESRD and CVD.
Methods
A prospective, observational, multicenter study, comprising 244 Japanese outpatients with CKD who had a follow-up period of at least 3 months. The primary endpoint was the first onset of a nonfatal or fatal CVD event and progression to ESRD, defined as myocardial infarction, stroke, or artery revascularization (coronary, carotid or peripheral), and initiation of dialysis.
Results
During a median follow-up of 3.8 years, the primary endpoint occurred in 39 (15.8 %) patients. Irrespective of diabetes, high urinary L-FABP correlated with the development of ESRD and CVD. The areas under the receiver-operator characteristic curves (AUCs) for predicting the primary endpoint for urinary concentrations of L-FABP, albumin, and NAG were 0.825, 0.797, and 0.722, respectively. Cox regression analyses, which were adjusted for factors known to influence the primary endpoint, including patient characteristics, and serum and urinary parameters, demonstrated that the primary outcome was associated with high urinary L-FABP and low eGFR [p = 0.049, hazard ratio = 1.341 (95 % CI 1.005–1.790); and p < 0.000, hazard ratio = 0.953 (95 % CI 0.930–0.976), respectively].
Conclusions
Urinary L-FABP may be a useful prognostic marker of progression to ESRD and the onset of CVD in patients with CKD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiovascular disease (CVD) is one of the primary causes of morbidity and mortality in patients with chronic kidney disease (CKD) [1]. To improve clinical outcomes, it is necessary to identify patients with CKD who are not only at a higher risk of progression to end-stage renal disease (ESRD), but also the onset of CVD, with the aim of initiating evidence-based therapy at an early stage.
Liver-type fatty acid-binding protein (L-FABP) is expressed in the proximal tubules [2], and it is an effective endogenous antioxidant during oxidative stress generated in pathophysiologic conditions [3]. Previous studies in kidney transplant recipients demonstrated that an increase in urinary L-FABP concentrations occurred concomitantly with a decrease in peritubular capillary blood flow [4]. This effect was attributed to the presence of a hypoxia responsive element in the promoter region of the L-FABP gene. Thus, urinary L-FABP may be a surrogate marker of microvascular injury and chronic hypoxia [4, 5]. Other reports indicate that urinary L-FABP is a promising biomarker for the diagnosis of various kidney diseases, including acute kidney injury (AKI) [6–9], diabetic nephropathy [3, 10, 11], and CKD [12–14]. Moreover, a recent study suggested that urinary L-FABP concentrations are related to the onset of CVD in patients with type 2 diabetes mellitus (T2DM) [10]. However, few studies have evaluated the relationship between urinary L-FABP in patients with CKD, and the risk of progression to ESRD or CVD onset.
To obtain high-quality data, measurement of clinical research parameters should be performed in a laboratory that is certified by the College of American Pathologists (CAP), an authoritative external organization that verifies accuracy, and the Japan Accreditation Board for Conformity Assessment (ISO15189). The aim of the present study was to evaluate the potential use of urinary clinical parameters, which were measured in a laboratory certified by the CAP and ISO15189 international standards, as biomarkers for progression to ESRD and the incidence of CVD in patients with various types of CKD, including diabetic nephropathy, nephrosclerosis, and glomerulonephritis.
Materials and methods
Study design and patient selection
This was a prospective, observational study, conducted between November 2007 and December 2012. CKD was defined according to guidelines established by Japanese Society of Nephrology [15].
Adult patients with CKD who presented at the outpatient clinic of the Department of Nephrology and Hypertension, Internal Medicine, St. Marianna University School of Medicine Hospital (Kawasaki, Japan) were eligible for enrollment. Inclusion criteria were as follows: (1) a diagnosis of CKD; (2) no history of liver disease, cancer, infectious disease, collagen disease or dialysis; (3) able to perform ambulatory blood pressure monitoring (ABPM); and (4) follow-up period of at least 3 months after enrollment. Patients with a cardiovascular (CV) event during the previous year were excluded. These eligibility criteria were met by a total of 244 patients, and their data were analyzed. The primary endpoint was progression to renal failure and the onset of nonfatal or fatal CV events, defined as myocardial infarction, stroke, revascularization of the coronary, carotid or peripheral artery, and initiation of dialysis. Written informed consent was obtained from all patients. The IRB/Ethics Committees provided approval for this study (IRB approval number: 1156).
Data collection
Hemoglobin in blood, and serum creatinine (Cr), total cholesterol, albumin, and LDL-cholesterol were routinely measured in blood samples collected immediately at the clinical laboratory, and these values were included in the analysis. The glomerular filtration rate (GFR) was estimated using the formula proposed by the Japanese Society of Nephrology, as follows:
eGFR (mL/min/1.73 m2) = 194 × serum Cr−1.094 × age−0.287 × 0.739 (if female) [16].
Spot urine samples were collected and preserved at −80 °C until the time of analyses. The samples were used to determine urinary concentrations of Cr, L-FABP, albumin, and N-acetyl-β-D-glucosaminidase (NAG), which are approved as clinical markers of tubular damage by the Ministry of Health, Labor and Welfare in Japan. Urinary parameters were measured by SRL Co. Research Service (Tokyo, Japan), which is certified by the CAP and ISO15189 standards. Urinary L-FABP was quantified by ELISA. Urinary L-FABP and urinary albumin were expressed as the ratio of the urinary parameter to the urinary Cr concentration. Because urinary NAG was routinely evaluated as the tubular impairment marker at a unit of U/L in the clinical setting, urinary NAG were also expressed in U/L in this study.
Statistical analysis
Results are expressed as median (25–75 % interquartile range (IQR) or mean [±standard deviation (SD)] values. p values <0.05 were considered to denote a statistically significant difference. To evaluate the relationship between urinary parameters at baseline and the primary endpoint, patients were divided into two groups, based on the occurrence of the primary endpoint. Between-group comparisons were made using the Mann–Whitney U test for unpaired data. Patients were then divided into two groups according to urinary parameters being above or below the upper limit of the reference value (upper limits defined as the normal upper limit, 8.4 µg/gCr for L-FABP, 30 mg/gCr for albumin, and 4.2 U/L for NAG), and event-free rate curves were generated for the primary endpoint in each group using the Kaplan–Meier method, and compared with the log-rank test. To determine the area under the receiver-operator characteristic curve (AUC) for baseline urinary concentrations of L-FABP, albumin and NAG as predictors of the primary outcome, receiver-operator characteristic (ROC) curves for clinical parameters were plotted against the occurrence of the primary endpoint. Cox regression analyses were performed to identify independent predictors of the primary endpoint, with adjustment for factors that influence progression to the primary endpoint, including age, ABPM-systolic blood pressure (SBP) and -diastolic blood pressure (DBP), body mass index (BMI), hemoglobin, serum LDL-cholesterol and albumin, presence of diabetes, the presence of prior CVD, estimated GFR, and urinary parameters. Because data on urinary parameters were not normally distributed, theses continuous values were converted into a logarithm for construction of ROC curves and Cox regression analysis. Statistical analyses were performed using SPSS software, version 21 (IBM, Armonk, NY, USA) and Stata MP 13.1 software (StatCorp LP, College Station, TX).
Results
Baseline characteristics
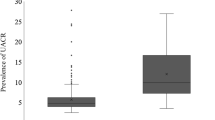
Among the 244 patients, the median follow-up period was 45.9 months (IQR 36.2–53.5 months). The primary outcome occurred in 39 patients (15.8 %), including 20 patients who presented with chronic hemodialysis, 13 with myocardial infarction, 4 with stroke, and 1 each with cerebral hemorrhage and peripheral artery revascularization, respectively. Baseline characteristics for the total patient population, and those with and without primary outcome events are shown in Table 1. Analyses based on age, gender, ABPM-SBP and -DBP, dyslipidemia, diabetes, and cigarette smoking revealed no significant differences in the occurrence of progression to ESRD or CVD onset. In contrast, significant associations with the primary outcome were observed for high serum Cr concentrations, low eGFR, and more severe stages of CKD. Urinary concentrations of L-FABP, albumin and NAG were significantly higher in patients with an event than in those without an event. The frequencies of a history of CVD, and the use of insulin, lipid-lowering and renin-angiotensin-aldosterone system (RAS) blockade treatments were significantly higher in patients with an event than in those without. On the contrary, serum LDL-cholesterol and albumin, hemoglobin, and BMI were significantly lower in patients with an event than in those without.
Survival curve of primary endpoint
As depicted in Fig. 1, the cumulative event-free survival for the primary outcome in patients with urinary concentrations of L-FABP, albumin and NAG above the upper limit reference value was significantly lower than that in the group with concentrations below the upper limit reference value. With regard to urinary L-FABP, patients were divided into two groups according to the presence of diabetes. Irrespective of diabetes (Fig. 2a, b), the cumulative event-free survival rate for the primary outcome in patients with elevated urinary L-FABP was significantly lower than for those with concentrations below the upper limit reference value.
Kaplan–Meier curves for event-free survival of three urinary biomarkers. Patients were divided into two groups based on urinary parameters above or below upper limit of reference value (the upper limit reference value of urinary L-FABP (a) 8.4 µg/gCr; urinary albumin (b), 30 mg/gCr; urinary NAG (c), 4.2 U/L). Above upper limit of reference value for urinary parameters, solid line (high group); below upper limit of reference value of urinary parameters, broken line (low group). Differences between the high and low group were compared by a log-rank test
Kaplan–Meier curves for event-free survival of urinary L-FABP, according to the presence of diabetes. Kaplan–Meier curves for event-free survival of patients with diabetes a and without diabetes, b patients were divided into the two groups depending on urinary L-FABP concentrations above upper limit of reference value (8.4 µg/g creatinine; high group) or below (low group) high urinary L-FABP group, solid line; low urinary L-FABP group, broken line. Differences between the high and low group were compared by a log-rank test
ROC analysis of urinary parameters for predicting the primary endpoint
The AUCs for predicting the primary endpoint using logarithmic-transformed baseline values for L-FABP (log urinary L-FABP), albumin (log urinary albumin) and NAG (log urinary NAG) were 0.825, 0.797 and 0.722, respectively. The parameter with the largest AUC was urinary L-FABP (Fig. 3). The AUC for the primary endpoint for all three urinary parameters was 0.840, which was significantly different from that for NAG (p = 0.001), but not L-FABP (p = 0.606) or albumin (p = 0.165). The cut-off values (sensitivity, specificity) of the primary endpoint for urinary L-FABP, urinary albumin, and urinary NAG, which were determined from the logarithmic-transformed data, were 9.9 µg/gCr (0.80, 0.78), 132.0 mg/gCr (0.74, 0.74), and 4.6 U/L (0.64, 0.63), respectively. Urinary L-FABP concentration had the highest sensitivity of the three urinary parameters.
Receiver-operator characteristics curve for predicting the progression to ESRD and the onset of CVD using urinary parameters. Black circles and solid lines indicate log urinary L-FABP, white circles and broken line indicate log urinary albumin, and white triangles and dotted lines indicate log urinary NAG
Furthermore, patients were divided into the two groups according to the presence of diabetes, and ROC curves were constructed for predicting the primary event according to log urinary concentrations of L-FABP, albumin, and NAG (Fig. 4a, b). Among patients with diabetes (n = 58), 14 (24.1 %) experienced a primary endpoint outcome. AUCs for predicting the primary outcome for log values of urinary L-FABP, albumin and NAG were 0.783, 0.735 and 0.649, respectively. The AUC for predicting the primary endpoint for all three urinary parameters was 0.825, which was significantly different from that for NAG (p = 0.021), but not L-FABP (p = 0.510) or albumin (p = 0.069). Cut-off values (sensitivity, specificity) for predicting the primary outcome for urinary L-FABP, urinary albumin and urinary NAG, which were determined from the logarithmic-transformed data, were 28.7 µg/gCr (0.71, 0.77), 423.0 mg/gCr (0.71, 0.77), and 6.5 U/L (0.57, 0.64), respectively. On the contrary, among patients without diabetes (n = 186), 25 (13.4 %) had a primary outcome event. AUCs for predicting the primary outcome using log values for urinary L-FABP, albumin and NAG were 0.833, 0.823 and 0.725, respectively. The AUC for predicting the primary endpoint for all three urinary parameters was 0.839, which was significantly different from that for NAG (p = 0.012), but not L-FABP (p = 0.850) or albumin (p = 0.643). Cut-off values (sensitivity, specificity) for predicting the primary endpoint for urinary L-FABP, urinary albumin and urinary NAG, which were determined from the logarithmic-transformed data, were 9.3 µg/gCr (0.80 0.82), 105 mg/gCr (0.80, 0.77) and 4.1 U/L (0.64, 0.63), respectively. Although the cut-off values (sensitivity, specificity) for predicting the primary endpoint were different between patients with and without diabetes, urinary L-FABP had the largest AUC, and the highest level of both sensitivity and specificity in both groups. This suggests that it may be sufficient to measure only urinary L-FABP among the three urinary parameters to detect patients at a high risk of ESRD or CVD.
Receiver-operator characteristics curve for predicting the progression to ESRD and the onset of CVD in urinary parameters of the subgroups divided according to the presence of diabetes. Receiver-operator characteristics curve in patients with diabetes a and without diabetes, b black circles and solid lines indicate log urinary L-FABP, white circles and broken line indicate log urinary albumin, and white triangles and dotted lines indicate log urinary NAG
Cox regression analysis for the primary endpoint
Using Cox regression analysis, the onset of ESRD and CVD was directly associated with log urinary L-FABP at baseline, prior CVD event, inversely related to baseline eGFR and age [p = 0.040, hazard ratio = 1.371 (95 % CI 1.014–1.854); p = 0.032, hazard ratio = 2.790 (95 % CI 1.092–7.127); p = 0.018, hazard ratio = 0.967 (95 % CI 0.941–0.994); and p = 0.014, hazard ratio = 0.957 (95 % CI 0.924–0.991), respectively. Table 2). In addition, serum albumin, hemoglobin, log urinary concentrations of albumin and NAG, and the presence of diabetes at baseline, were associated with ESRD and CVD. However, after adjustment for known risk factors, including log urinary L-FABP and eGFR, there were no associations between these variables and the primary endpoint.
Discussion
The present study evaluated the clinical significance of urinary parameters, which were measured according to international standards, as prognostic indicators of the development of ESRD and CVD in patients with CKD. Because the follow-up period was relatively short, and the primary endpoint was hard, patients with advanced stages of CKD, macroalbuminuria, and elevated urinary concentrations of L-FABP and NAG, progressed to the primary endpoint, as expected. In this population, among the three urinary parameters measured, urinary L-FABP had the largest AUC for predicting the onset of the primary endpoint. Multivariate regression analysis demonstrated that elevated urinary L-FABP and low eGFR were associated with the development of ESRD and CVD, irrespective of diabetes. This indicated that urinary L-FABP may be a prognostic marker for progression to ESRD and onset of CVD in patients with CKD.
Progression of CKD in adults is accelerated by comorbidities, for example hypertension [17–19], hyperlipidemia [20], and hyperglycemia [20, 21], as well as aging [22, 23]. These disorders either cause glomerular injury that leads to tubulointerstitial damage, or directly provoke tubulointerstitial damage because of hemodynamic dysfunction. Tubulointerstitial damage is widely known to be the final common pathway in ESRD, and it is strongly related to renal prognosis [24, 25]. Therefore, tubular markers are possible indicators of the severity of CKD. Urinary L-FABP correlated with structural tubulointerstitial damage in renal biopsy specimens [26]. In experiments using L-FABP transgenic mice, urinary L-FABP levels were altered by aggravation and amelioration of tubulointerstitial damage, reflecting the degree of tubulointerstitial degeneration [5, 27]. Recent studies reported that elevated urinary L-FABP concentrations were associated with a reduction in hemoglobin levels, resulting in the development of renal microcirculation dysfunction [28]. These findings suggest that the high sensitivity of urinary L-FABP as a marker of structural changes in tubular cells may contribute to its accuracy in predicting progression to ESRD.
In accordance with the scientific statement from the American Heart Association, ‘‘Kidney Disease as a Risk Factor for the Development of Cardiovascular Disease [28],’’ measurement of urinary parameters may have great value in the prediction of CVD onset as well as renal prognosis. Araki et al. reported that an increase in urinary L-FABP concentration was a risk factor for renal and CV complications in T2DM patients with normoalbuminuria (n = 422) and microalbuminuria (n = 196) in long-term observational studies of 12 years [10, 11]. This result coincides with that of the present study in patients with CKD. A recent cross-sectional study in patients with T2DM demonstrated that the frequency of electrocardiographic abnormalities was significantly higher among those with high urinary L-FABP levels (>8.4 μg/g creatinine; 28.3 %) compared with low urinary L-FABP (<8.4 μg/g creatinine; 9.2 %); however, urinary albumin levels and eGFR levels were similar between the two groups [29]. Urinary L-FABP may reflect the degree of systemic microcirculation injury, and be a predictive marker for the onset of CVD, as well as the development of ESRD.
Proteinuria and albuminuria increased the risk of CVD [30], and even mild albuminuria (~10 mg/day) was an independent predictor of CVD in the general population [31]. It is well established that patients with diabetes have an increased risk of both CVD and CKD compared with non-diabetic individuals. A Canadian epidemiological study with a four-year follow-up period indicated that the rate of myocardial infarction, and all-cause mortality after myocardial infarction was higher in patients with both diabetes and CKD than in those with CKD alone [32]. In the present study, although urinary albumin levels and the proportion of patients with T2DM was higher among patients who experienced a primary outcome event, these variables were not associated with an increased risk of ESRD and CVD after adjustment for factors known to cause progression to the primary endpoint, including patient characteristics, and serum and urinary parameters. Furthermore, although age tended to be higher in the patients with event than in those without it, younger age was an independent risk factor in the multivariate analysis. In the multivariate analysis, several good predictors (urinary albumin, urinary L-FABP, presence of DM, eGFR and age) were correlated with each other. Therefore, such a conflicted finding may be observed in regression output.
This study has some limitations, in particular, measurement of urinary parameters was only performed at baseline, the treatment protocol for patients was not unified, and the cause of CKD was varied. Urinary parameters in preclinical stage, which was measured only in laboratory research and was not used in a clinical diagnosis, were not evaluated because the measurement kits have not yet been approved for urinary parameters by the Ministry of Health, Labor and Welfare in Japan. The follow-up period was also relatively short, and the occurrence of the primary endpoint in patients without advanced renal dysfunction was rare. Therefore, low eGFR was a strong independent risk factor for predicting ESRD and CVD, and the benefit of measuring urinary L-FABP, in addition to eGFR, was not demonstrated.
In conclusion, elevated urinary L-FABP concentrations were found to be associated with progression to ESRD and the incidence of CVD in the patients with CKD. Measurement of urinary FABP may be useful for the detection of patients at greater risk of progression to ESRD and the onset of CVD. To confirm the possibility of urinary L-FABP as a more sensitive marker of ESRD and CVD than eGFR, long-term follow-up studies are necessary in CKD patients without moderate or severe renal dysfunction.
References
Keith DS, Nichols GA, Gullion CM, Brown JB, Smith DH. Longitudinal follow-up and outcomes among a population with chronic kidney disease in a large managed care organization. Arch Intern Med. 2004;164(6):659–63.
Maatman RG, van de Westerlo EM, van Kuppevelt TH, Veerkamp JH. Molecular identification of the liver- and the heart-type fatty acid-binding proteins in human and rat kidney. Use of the reverse transcriptase polymerase chain reaction. Biochem J. 1992;288(Pt 1):285–90.
Kamijo-Ikemori A, Sugaya T, Kimura K. Novel urinary biomarkers in early diabetic kidney disease. Curr Diab Rep. 2014;8(14):1–9 (513-014-0513-1).
Yamamoto T, Noiri E, Ono Y, Doi K, Negishi K, Kamijo A, et al. Renal L-type fatty acid-binding protein in acute ischemic injury. J Am Soc Nephrol. 2007;11(18):2894–902.
Matsui K, Kamijo-Ikemorif A, Sugaya T, Yasuda T, Kimura K. Renal liver-type fatty acid binding protein (L-FABP) attenuates acute kidney injury in aristolochic acid nephrotoxicity. Am J Pathol. 2011;178(3):1021–32.
Matsui K, Kamijo-Ikemori A, Hara M, Sugaya T, Kodama T, Fujitani S, et al. Clinical significance of tubular and podocyte biomarkers in acute kidney injury. Clin Exp Nephrol. 2011;15(2):220–5.
Matsui K, Kamijo-Ikemori A, Sugaya T, Yasuda T, Kimura K. Usefulness of urinary biomarkers in early detection of acute kidney injury after cardiac surgery in adults. Circ J. 2012;76(1):213–20.
Han WK, Wagener G, Zhu Y, Wang S, Lee HT. Urinary biomarkers in the early detection of acute kidney injury after cardiac surgery. Clin J Am Soc Nephrol. 2009;4(5):873–82.
Han WK, Waikar SS, Johnson A, Betensky RA, Dent CL, Devarajan P, et al. Urinary biomarkers in the early diagnosis of acute kidney injury. Kidney Int. 2008;73(7):863–9.
Araki S, Haneda M, Koya D, Sugaya T, Isshiki K, Kume S, et al. Predictive effects of urinary liver-type fatty acid-binding protein for deteriorating renal function and incidence of cardiovascular disease in type 2 diabetic patients without advanced nephropathy. Diabetes Care. 2013;36(5):1248–53.
Kamijo-Ikemori A, Sugaya T, Yasuda T, Kawata T, Ota A, Tatsunami S, et al. Clinical significance of urinary liver-type fatty acid-binding protein in diabetic nephropathy of type 2 diabetic patients. Diabetes Care. 2011;34(3):691–6.
Kamijo A, Sugaya T, Hikawa A, Yamanouchi M, Hirata Y, Ishimitsu T, et al. Clinical evaluation of urinary excretion of liver-type fatty acid-binding protein as a marker for the monitoring of chronic kidney disease: a multicenter trial. J Lab Clin Med. 2005;145(3):125–33.
Kamijo A, Kimura K, Sugaya T, Yamanouchi M, Hikawa A, Hirano N, et al. Urinary fatty acid-binding protein as a new clinical marker of the progression of chronic renal disease. J Lab Clin Med. 2004;143(1):23–30.
Kamijo A, Sugaya T, Hikawa A, Yamanouchi M, Hirata Y, Ishimitsu T, et al. Urinary liver-type fatty acid binding protein as a useful biomarker in chronic kidney disease. Mol Cell Biochem. 2006;284(1–2):175–82.
Japanese Society of Nephrology. Evidence-based practice guideline for the treatment of CKD. Clin Exp Nephrol. 2009;13(6):537–66.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53(6):982–92.
Klag MJ, Whelton PK, Randall BL, Neaton JD, Brancati FL, Ford CE, et al. Blood pressure and end-stage renal disease in men. N Engl J Med. 1996;334(1):13–8.
Klag MJ, Whelton PK, Randall BL, Neaton JD, Brancati FL, Stamler J. End-stage renal disease in African-American and white men: 16-year MRFIT findings. JAMA. 1997;16(277):1293–8.
Tozawa M, Iseki K, Iseki C, Kinjo K, Ikemiya Y, Takishita S. Blood pressure predicts risk of developing end-stage renal disease in men and women. Hypertension. 2003;41(6):1341–5.
Thomas G, Sehgal AR, Kashyap SR, Srinivas TR, Kirwan JP, Navaneethan SD. Metabolic syndrome and kidney disease: a systematic review and meta-analysis. Clin J Am Soc Nephrol. 2011;6(10):2364–73.
Mak RH. Insulin and its role in chronic kidney disease. Pediatr Nephrol. 2008;23(3):355–62.
Poggio ED, Rule AD, Tanchanco R, Arrigain S, Butler RS, Srinivas T, et al. Demographic and clinical characteristics associated with glomerular filtration rates in living kidney donors. Kidney Int. 2009;75(10):1079–87.
Horio M, Imai E, Yasuda Y, Watanabe T, Matsuo S. Performance of GFR equations in Japanese subjects. Clin Exp Nephrol. 2013;17(3):352–8.
Truong LD, Farhood A, Tasby J, Gillum D. Experimental chronic renal ischemia: morphologic and immunologic studies. Kidney Int. 1992;41(6):1676–89.
D’Amico G. Influence of clinical and histological features on actuarial renal survival in adult patients with idiopathic IgA nephropathy, membranous nephropathy, and membranoproliferative glomerulonephritis: survey of the recent literature. Am J Kidney Dis. 1992;20(4):315–23.
Kamijo A, Sugaya T, Hikawa A, Okada M, Okumura F, Yamanouchi M, et al. Urinary excretion of fatty acid-binding protein reflects stress overload on the proximal tubules. Am J Pathol. 2004;165(4):1243–55.
Yokoyama T, Kamijo-Ikemori A, Sugaya T, Hoshino S, Yasuda T, Kimura K. Urinary excretion of liver type fatty acid binding protein accurately reflects the degree of tubulointerstitial damage. Am J Pathol. 2009;174(6):2096–106.
von Eynatten M, Baumann M, Heemann U, Zdunek D, Hess G, Nawroth PP, et al. Urinary L-FABP and anaemia: distinct roles of urinary markers in type 2 diabetes. Eur J Clin Invest. 2010;40(2):95–102.
Maeda Y, Suzuki A, Ishii J, Sekiguchi-Ueda S, Shibata M, Yoshino Y, et al. Level of urinary liver-type fatty acid-binding protein is associated with cardiac markers and electrocardiographic abnormalities in type-2 diabetes with chronic kidney disease stage G1 and G2. Heart Vessel. 2014;3(30):362–8.
Ito S, Nagasawa T, Abe M, Mori T. Strain vessel hypothesis: a viewpoint for linkage of albuminuria and cerebro-cardiovascular risk. Hypertens Res. 2009;32(2):115–21.
Chronic Kidney Disease Prognosis Consortium, Matsushita K, van der Velde M, Astor BC, Woodward M, Levey AS, et al. Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet. 2010;375(9731):2073–81.
Tonelli M, Muntner P, Lloyd A, Manns BJ, Klarenbach S, Pannu N, et al. Risk of coronary events in people with chronic kidney disease compared with those with diabetes: a population-level cohort study. Lancet. 2012;380(9844):807–14.
Acknowledgments
We wish to thank Ms. Kimie Katayama, and Aya Sakamaki, Department of Nephrology and Hypertension, Internal Medicine, St. Marianna University School of Medicine, Ms. Seiko Hoshino, Department of Anatomy, St. Marianna University School of Medicine, for collection of urine. This study was partly supported by Grant-in-Aids for Diabetic Nephropathy Research and for Diabetic Nephropathy and Nephrosclerosis Research, which were provided by the Ministry of Health, Labor and Welfare of Japan and the Ministry of Education, Science, Sports and Culture, Japan.
Conflict of interest
T. Sugaya is the Director and Senior scientist of CMIC Holdings Co., Ltd., the company that produced the kits for L-FABP analysis. None of the other authors have conflicts of interest or financial disclosures of any relevance to the present study.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Matsui, K., Kamijo-Ikemori, A., Imai, N. et al. Clinical significance of urinary liver-type fatty acid-binding protein as a predictor of ESRD and CVD in patients with CKD. Clin Exp Nephrol 20, 195–203 (2016). https://doi.org/10.1007/s10157-015-1144-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-015-1144-9