Abstract
Although application of intraoperative computer navigation technique had been integrated into placement of pedicle screws (PSs) in thoracic fusion for years, its security and practicability remain controversial. The aim of this study is to evaluate the accuracy, the operative time consumption, the amount of intraoperative blood loss, time of pedicle insertion and the incidence of complications of thoracic pedicle screw placement in patients with thoracic diseases such as scoliosis and kyphosis. Pubmed, Web of Knowledge, and Google scholar were searched to identify comparative studies of thoracic pedicle screw placement between intraoperative computer navigation and fluoroscopy-guided navigation. Outcomes of malposition rate, operative time consumption, insertion time, intraoperative blood loss, and the incidence of complications are evaluated. Fourteen articles including 1723 patients and 9019 PSs were identified matching inclusion criteria. The malposition rate was lower (RR: 0.33, 95 % CI: 0.28–0.38, P < 0.01) in computer navigation group than that in fluoroscopy-guided navigation group; the operative time was significantly longer [weighted mean difference (WMD) = 23.66, 95 % CI: 14.74–32.57, P < 0.01] in computer navigation group than that in fluoroscopy-guided navigation group. The time of insertion was shorter (WMD = −1.88, 95 % CI: −2.25– −1.52, P < 0.01) in computer navigation group than that in fluoroscopy-guided navigation group. The incidence of complications was lower (RR = 0. 23, 95 % CI: 0.12–0.46, P < 0.01) in computer navigation group than that in the other group. The intraoperative blood loss was fewer (WMD = −167.49, 95 % CI: −266.39– −68.58, P < 0.01) in computer navigation group than that in the other. In conclusion, the meta-analysis of thoracic pedicle screw placement studies clearly demonstrated lower malposition rate, less intraoperative blood loss, and fewer complications when using computer navigation. This result provides strong evidence that computer technology could be safer and more reliable than fluoroscopy-guided navigation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Although internal fixation has become a standard procedure for the treatment of thoracic disease especially osteotomies for scoliosis, kyphosis which generally involve multisegmental, multi-screws and multi-rod fixation since pedicle screws were first placed by Harrington, there is still some problems because of the smaller pedicle size than that of other regions, more complex 3D anatomy and osteoporosis especially in thoracic vertebra due to its complex anatomy and decreased pedicle dimensions [22, 35].
Intraoperative computer navigation including ISO-C 3D navigation, CT navigation, and 3D-visual guidance technique as reported by Abe et al. [1] was first performed by Steinmann et al. in the 1990s in Lumbar fusion [29], which provides a good solution to these problems [5, 15, 21, 24, 26]. But like every other techniques, computer navigation has its own disadvantages such as the potential of causing various complications to neurological, vascular and adjacent structures if misplacement [9, 12, 17] and excessively rigid fixation may result in clinically adverse effects, such as device-related osteoporosis [24, 25] which may reduce the fusion rate and adjacent segment degeneration [9, 11, 26]. Once the PSs are accurately placed, the foundation of the procedure was established [34]. Recently, some research [1, 11, 13, 41] have shown that screw placements navigated by computer may have a longer operating time and a shorter length of stay than fluoroscopy-guided navigation. However, the effectiveness, safety, and biomechanics of screws for placement still remain controversial. The purpose of this meta-analysis is to evaluate the malposition rate, operative time consumption, time of insertion, incidence of complications, and intraoperative blood loss of PSs placement in thoracic diseases and provide evidence for clinical practice.
Materials and methods
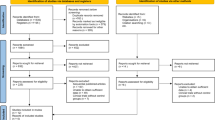
Identification and eligibility of relevant articles.
We searched Pubmed, Medline, Web of Knowledge, and Google scholar for all randomized studies published using “thoracic”, “pedicle screws placement”, “intraoperative computer navigation”, and “fluoroscopy-guided navigation” as key words. One thousand five hundred eighty-four articles were primely screened out and reviewed independently by two authors. We imposed the following inclusion criteria for the meta-analysis: (1) international published randomized controlled trails and rigorous designed prospective studies; (2) the preoperative diagnosis and the indications of posterior pedicle screw fixation in patients with thoracic disease is unmistakable; and (3) data for malposition rate. Exclusion criteria were as follows: (1) retrospective study and case report; (2) cadaver research, animal research, or in vitro research; (3) the navigational location was not the thoracic region or though the location was thoracic region, it did not provide specific cases; and (4) comparison among different navigation technology.
Outcomes
The malposition rate, the incidence of complications, time of insertion, operative time consumption, the incidence of complications, and intraoperative blood loss were sorted successively for further analysis.
Assessment of methodological quality
The methodological quality of the trials was independently assessed by two authors using the Cochrane Handbook for Systematic Reviews of Interventions 5.1. Disagreements were resolved through discussion and consensus. We evaluated the risk of bias of included studies using the Review Manager software (RevMan Version 5.2; The Nordic Cochrane Center, The Cochrane Collaboration, Copenhagen, Denmark), which included the following key domains: random sequence generation; allocation concealment; blinding of participants and personnel; blinding of outcome assessment; incomplete outcome data; and selective reporting.
Meta-analysis
We performed all of the meta-analysis by the Review Manager software (RevMan 5.2). Risk ratios (RRs) and 95 % confidence intervals (CIs) were used to evaluate the dichotomous outcomes, such as the incidence of complications. A P value of <0. 01 was considered statistically significant. The fixed effect model was used when the test for homogeneity was significantly (P > 0.1 and I 2 < 50 %) while the random effect model was used when the test of statistical heterogeneity was significantly (P < 0.1 and I 2 > 50 %). Studies with high statistical heterogeneity were rejected by performing the sensitivity analysis.
Results
Under the guidance of the search strategy, 1584 articles were primely screened out. By following the inclusion and exclusion criterias, we finally obtained 14 satisfactory articles published from 2008 to 2013 [1, 3, 11, 13, 18, 20, 23, 27, 28, 33, 37, 38, 40, 41]. Ten of these studies were RCTs and the other four were prospective studies. The study selection process was presented in Table 1. Funnel plot graph was used to evaluate the publication bias of malposition rate, the incidence of complications, time of insertion, operative time consumption, the incidence of complications and intraoperative blood loss between fluoroscopy-guided, and computer navigation groups, the outcome which shows no obvious distribution of the scatters, which indicated that all selected articles, had no publication bias [Fig. 1].
Meta-results
-
1.
Malposition rate was available in all 14 studies and random effect model (P = 0.01, I 2 = 67 %) was used to analyze the pooled data, the result is significantly difference between the two groups (RR = 0. 33, 95 % CI: 0.28–0.38, P < 0.01) [Fig. 2] which points out that intraoperative computer navigation may significantly lower the malposition rate than fluoroscopy-guided navigation.
-
2.
Operative time consumption was mentioned four studies of all the 14 and fixed effect model (P = 0.63, I 2 = 0 %) was used to analyze the collected date which shows significant difference between computer and fluoroscopy-guided navigation groups (RR = 23.66, 95 % CI: 14.74–32.57, P < 0.01) [Fig. 3] that indicate intraoperative computer navigation had longer operative time consumption than fluoroscopy-guided navigation in thoracic PSs placement.
-
3.
Time of insertion was mentioned four studies of all the 14 and random effect model (P < 0.01, I 2 = 84 %) was used to analyze the collected date which shows significant difference between computer and fluoroscopy-guided navigation groups (RR = −1.88, 95 % CI: −2.25– −1.52, P < 0.01) [Fig. 4] that indicate intraoperative computer navigation can lower operative time consumption than fluoroscopy-guided navigation in thoracic PSs placement.
-
4.
Incidence of complications was available in six of the 14 studies, most of the postoperative complications were cerebrospinal fluid leakage, lower extremity pain, numbness or motor deficit, infection and pneumonia, and complications related to the placement of PSs were lower extremity pain, numbness or motor deficit which may mainly caused by intraoperative nerve injury. The test of heterogeneity shows a P = 1.00, I 2 = 0 %, so fixed effect model was used to analyze the collected date which shows significant difference between computer and fluoroscopy-guided navigation groups (RR = 0.23, 95 % CI: 0.12–0.46, P < 0.01) [Fig. 5].
-
5.
Intraoperative blood loss was mentioned in three studies and fixed effect model (the heterogeneity test showed P = 0.98, I 2 = 0 %) was used to analyze the collected date which shows significant difference between computer and fluoroscopy-guided navigation groups (RR = −167.49, 95 % CI: −266.39– −68.58, P < 0.01) [Fig. 6] that indicate intraoperative computer navigation can lower intraoperative blood loss than fluoroscopy-guided navigation in thoracic PSs placement.
Discussion
This meta-analysis has shown that for patient with thoracic diseases such as scoliosis, kyphosis, or vertebral fracture, the accuracy of pedicle screw insertion was significantly improved under the computer navigation. There have been several meta-analyses [13, 31, 32, 36] since Gelalis [6], who first conducted a systematic review to compare the free-hand, fluoroscopic-guided and navigation techniques and found that the accuracy of screw positioning was improved when navigation assistance was used. However, no meta-analysis was performed to assess the accuracy of thoracic PSs placement under computer guidance.
Interbody fusion for patients using fluoroscopy guidance has achieved a high success rate of 90.3–94.1 % [13, 38]. But place screws accuracy is influenced by multi-factors including an experienced surgeon, complete anatomical knowledge, and a careful preoperative plan. The misplacement of PSs may lead to serious vascular or neurological complications [4, 13] thus made a high malposition rate [19, 30, 39].
Computer navigation technology appears to be helpful for surgeons since Steinmann first performed it in 1990s. Although numbers of studies have demonstrated that place PSs under computer navigation is a safer way in other spinal regions, there is no specific research that conducts systematic analysis in thoracic PSs placement, and the effectiveness, safety, and biomechanics of PS placement in thoracic vertebra under computer guidance still remain controversial, some studies reported that computer navigation has advantages such as higher accuracy and lower blood loss [41], while other studies obtained the opposite conclusion [2, 40]. Hence, a systematic assessment of current studies should be done.
The result of this meta-analysis firstly showed that in thoracic internal fixation, intraoperative computer navigation may significantly lower the malposition rate than fluoroscopy-guided navigation in thoracic diseases by summarizing all 14 articles. However, due to surgeon’s inexperienced, misplacement rate, loose of the instruments, and poor peeling of soft tissue still exists. The prone position of patients during the process of image acquisition also improves the accuracy of PSs [39].
Signally differences about incidence of complications were also shown in this article that the intraoperative computer navigation pedicle screw placement had a lower incidence than the other group. Complications were reported in five of the 14 articles which showed 48 cases [13, 18, 23, 28, 41], the most common one is nerve damage (20 of 38 cases) in the fluoroscopy-guided group and four of ten cases in the computer navigation group and the most serious one is infection (nine of 38 cases) in the fluoroscopy-guided group which caused fatal consequences like pneumonia, and two of ten cases in the other group which leads to deep infection and healed after multiple lavations and removal of the instrumentation [13]. Two independent sample t tests show markedly difference (P < 0.01). Percutaneously small incision and increased accuracy which reduce the damage of juxtaspinal vessels or nerves and the time to re-adjust the trajectories make it possible to lessen the incidence of complications. However, there is a lack of long-term prognosis in the literature currently, the terminal validity still need further verification.
Though a signally difference of operative time consumption is shown by meta-analysis between computer-guided group and fluoroscopy-guided navigation group, it turns out that the operative time may longer in computer navigation group than that in fluoroscopy-guided navigation group in thoracic PSs placement, this result is based on the analysis of four studies in which the time of operation are mentioned and the reasons are as follows: compared with fluoroscopy-guided navigation, operative procedure of computer navigation contains a step of image registration, which may cost a plenty of time, especially in the patient with several degeneration or vertebral instability. In addition, the placement process often requires multiple registrations, which may also increase operative time [10]. As soon as the registration is done, surgeons can accurately place the screws based on intuitive images combined with experiences and feel, thus make repeatedly pause the operation to check the accuracy of screws is not necessary anymore, which reduced the total operative time [8].
Laine et al. (2000) concluded that the computer navigation is somewhat time consuming. Three steps are included in mean preoperative planning time and the second one is the only obligatory one. A surgeon familiar with the system needs 4–6 min per vertebra to perform it [13]. This analysis includes four studies and the outcome shows a longer operative time in computer navigation group, matching problems were the main reason that prolongs operative time [14] and since the introduction of the surface-matching technique such problems are resolved. There were article reports that the average time of insertion of a single screw is lower in computer navigation group [12] and the more familiar the surgeons are with the navigation system, the more accurate the registered process will be, which can reduce the total operated time.
Meanwhile this analysis shows the insertion time was lower in computer navigation group than that in fluoroscopy-guided group, as surgeons become familiar with the navigation system, the registration process will be more accurate, matches among devices will also be more experienced, which lead to the reduction of insertion time, thereby further increases the accuracy of placement.
Only three articles mentioned index about intraoperative blood loss [13, 23, 41], the reasons may as follows: (1) the reduce of total operative time especially time of insertion; (2) the increased accuracy reduces the damage of juxtaspinal vessels or nerves and the time to re-adjust the trajectories; (3) The PSs placement through percutaneously small incision make it possible to avoid intraoperative blood loss.
Four of the 14 articles mentioned the high cost of computer-guided navigation system [7, 11, 18, 33], which limits the promulgation of the system, but detailed data including equipment and materials costs and payment from the patients, were not mentioned, so further studies in this aspect should be conducted.
When performing meta-analysis of the effect of different therapeutic interventions, it is recognized that randomized controlled trials (RCT) as the best type of research that is included. This article brings into 14 studies, ten of which are RCTs and the other four are prospective researches. However, due to ethical and technical issues, it is more difficult to actualize the strict randomization and blinding of the curative effect of surgery in methodology, so bias is difficult to avoid even for the RCTs such as selection bias, sampling bias, and literature search bias. Prospective studies that are rigorously designed were integrated into the meta-analysis to offset the insufficient number of RCT articles. Nonetheless, the problem caused by the combine is the increase of the risk-related bias, such as measurement bias. This is equally inadequate for the article.
Conclusion
Intraoperative computer navigation and fluoroscopy-guided navigation of PSs placement have markedly differences in malposition rate, incidence of complications, time of insertion, and blood loss; operative time as computer-guided can lower four of the above-mentioned indexes except the last one. We inferred that intraoperative computer navigation may be safer in patients who suffer from thoracic diseases such as scoliosis, kyphosis, or vertebral fracture and undergo interbody fusion using PSs. Since the unacceptably high cost of the equipment, the time to be proficient in this technique is long, the radiation exposure of patient or surgeons by some of the devices still cannot be reduced, and computer navigation have a rate of failure, the routinization of computer navigation in thoracic vertebral surgery still need to be treated with caution. Meanwhile, as a new technology, large samples of clinical trial designs are also expected.
References
Abe Y et al (2011) A novel cost-effective computer-assisted imaging technology for accurate placement of thoracic PSs. J Neurosurg Spine 15(5):479–485
Ailawadhi P, Agrawal D, Satyarthee G et al (2011) Use of O-arm for spinal surgery in academic institution in India: experience from JPN apex trauma centre. Neurol India 59(4):590–593
Allam Y et al (2013) Computer tomography assessment of pedicle screw placement in thoracic spine: comparison between free hand and a generic 3D-based navigation techniques. Eur Spine J
Esses SI, Sachs BL, Dreyzin V (1993) Complications associated with the technique of pedicle screw fixation. A selected survey of ABS members. Spine 18:2231–2238
Fu TS, Wong CB, Tsai TT et al (2007) Pedicle screw insertion: computed tomography versus fluoroscopic image guidance. Int Orthop
Gelalis ID, Paschos NK, Pakos EE et al (2012) Accuracy of pedicle screw placement: a systematic review of prospective in vivo studies comparing free hand, fluoroscopy guidance and navigation techniques. Eur Spine J 21:247–255
Haberland N, Ebmeier K, Hliscs R et al (1999) Intraoperative CT in image-guided surgery of the spine. Medicamundi 43:24–31
Hartl R, Lam KS, Wang J et al (2013) Worldwide survey on the use of navigation in spine surgery. World Neurosurg 79(1):162–172
Hicks JM, Singla A, Shen FH et al (2010) Complications of pedicle screw fixation in scoliosis surgery: a systematic review. Spine (Phila Pa 1976) 35(11):E465–E470
Houten JK, Nasser R, Baxi N (2012) Clinical assessment of percutaneous lumbar pedicle screw placement using the O-arm multidimensional surgical imaging system. Neurosurgery 70(4):990–995
Huang Y et al (2009) Application of C-arm X-ray navigation and CT navigation in thoracolumbar pedicle screw fixation, a contrast observation. Shangdong Med 14:5–7
Katonis P, Christoforakis J, Aligizakis AC et al (2003) Complications and problems related to pedicle screw fixation of the spine. Clin Orthop 411:86–94
Kosmopoulos V, Schizas C (2007) Pedicle screw placement accuracy: a meta-analysis. Spine (Phila Pa 1976) 32:E111–E120
Laine T et al (2000) Accuracy of pedicle screw insertion with and without computer assistance: a randomised controlled clinical study in 100 consecutive patients. Eur Spine J 9(3):235–240
Laine T, Schlenzka D, Mäkitalo K et al (1997) Improved accuracy of pedicle screw insertion with computer-assisted surgery. Spine 22:1254–1258
Lekovic GP, Potts EA, Karahalios DG et al (2007) A comparison of two techniques in image-guided thoracic pedicle screw placement: a retrospective study of 37 patients and 277 PSs. J Neurosurg Spine 7(4):393–398
Li Q, Tian Q, Liu B et al (2007) Percutaneous pedicle screw fixation in thoracic-lumbar fracture using mini-invasive pedicle screw system guided by navigation. China Med Mag 87(19):1339–1341
Lonstein JE, Denis F, Perra JH et al (1999) Complications associated with PSs. J Bone Joint Surg Am 81- A:1519–1528
Luther, N et al (2013) Comparison of navigated versus non-navigated pedicle screw placement in 260 patients and 1434 screws: screw accuracy, screw size, and the complexity of surgery. J Spinal Disord Tech
Makino K, Fujiwara H et al Morphometric analysis using multiple anarreconstructed CT of the lumbar pedicle in patients with degenerative lumbar scoliosis is characterized by a Cobb angle of 30 degrees or greater. J Neurosurg Spine 17(3):256–262. 102
Merloz P et al (1998) Computer-assisted surgery: automated screw placement in the vertebral pedicle. Chirurgie 123(5):482–490
Merloz P, Troccaz J, Vouaillat H et al (2007) Fluoroscopy-based navigation system in spine surgery. Proc Inst Mech Eng [H] 221(7):813–820
Panjabi MM, Takata K, Goel V et al (1991) Thoracic human vertebrae. Quantitative three-dimensional anatomy. Spine 16:888–901
Rajasekaran S et al (2007) Randomized clinical study to compare the accuracy of navigated and non-navigated thoracic PSs in deformity correction surgeries. Spine (Phila Pa 1976) 32(2):E56–E64
Ringel F, Stoffel M, Stuer C et al (2006) Minimally invasive transmuscular pedicle screw fixation of the thoracic and lumbar spine. Neurosurgery 59(4 Suppl 2):ONS361-6, discussion ONS366-7
Sahoo MM, Mahapatra SK, Sethi GC et al (2012) Posterior-only approach surgery for fixation and decompression of thoracic lumbar spinal tuberculosis: a retrospective study. J Spinal Disord Tech 25(7):217–223
Sasso RC, Garrido BJ (2007) Computer-assisted spinal navigation versus serial radiography and operative time for posterior spinal fusion at L5-S1. J Spinal Disord Tech 20(2):118–122
Seller K et al (2005) Prospective screw misplacement analysis after fluoroscopy-guided and navigated pedicle screw implantation. Biomed Technol (Berl) 50(9):287–292
Shin MH et al (2012) Accuracy and safety in pedicle screw placement in the thoracic and lumbar spines: comparison study between fluoroscopy-guided C-Arm fluoroscopy and navigation coupled with O-Arm(R) guided methods. J Korean Neurosurg Soc 52(3):204–209
Steinmann JC, Herkowitz HN, ei-Kommons H et al (1993) Spinal pedicle fixation: confirmation of an image-based technique for screw placement[J]. Spine 18(13):1856–1861
Su BW, Kim PD, Cha TD et al (2009) An anatomical study of the mid-lateral pars relative to the pedicle foot print in the lower lumbar spine. Spine (Phila Pa 1976) 34(13):1355–1362
Tian NF, Huang QS, Zhou P, Zhou Y, Wu RK, Lou Y et al (2011) Pedicle screw insertion accuracy with different assisted methods: a systematic review and meta-analysis of comparative studies. Eur Spine J 20:846–859
Tian NF, Xu HZ (2009) Image-guided pedicle screw insertion accuracy: a meta-analysis. Int Orthop 33:895–903
Tormenti MJ et al (2010) Intraoperative computed tomography image-guided navigation for posterior thoracolumbar spinal instrumentation in spinal deformity surgery. Neurosurg Focus 28(3):E11
Torres J et al (2012) Screw placement accuracy for minimally invasive transforaminal lumbar interbody fusion surgery: a study on 3-D neuronavigation-guided surgery. Global Spine J 2(3):143
Vaccaro AR, Rizzolo SJ, Allardyce TJ, Ramsey M, Salvo J, Balderston RA, Cotler JM (1995) Placement of PSs in the thoracic spine. Part I: morphometric analysis of the thoracic vertebrae. J Bone Joint Surg Am 77:1193–1199
Verma R, Krishan S, Haendlmayer K, Mohsen A (2010) Functional outcome of computer-assisted spinal pedicle screw placement: a systematic review and meta-analysis of 23 studies including 5,992 pedicle screws. Eur Spine J 19:370–375
Waschke A et al (2013) CT-navigation versus fluoroscopy-guided placement of PSs at the thoracolumbar spine: single center experience of 4,500 screws. Eur Spine J 22(3):654–660
Wu H et al (2010) Pedicle screw placement in the thoracic spine: a randomized comparison study of computer-assisted navigation and fluoroscopy-guided techniques. Chin J Traumatol Chin Med Assoc 13(4):201–205
Zausinger S, Scheder B, Uhl E et al (2009) Intraoperative computed tomography with integrated navigation system in spinal stabilizations. Spine (Phila Pa1976) 34(26):2919–2926
Zhang B, et al (2006) The application of 3D navigation-assisted thoracic-lumbar PSs placement in interbody fusion. Anhui Med Univ
Zong Z (2009) A comparative study of application between three-dimensional navigation assisted and X-ray fluoroscopy in thoracolumbar pedicle screw fixation. Beijing Univ Chin Med
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Comments
Kiyoshi Ito, Matsumoto, Japan
In recent years, the significant advances of the surgery supporting device is remarkable in the field of the spinal surgery.
Authors showed the significant excellence of computer navigation system from the previous report between two groups. As written in conclusion, I want to know if there is data on the differences of the radiation exposure in both. It is very important to know the difference of the radiation exposure in accordance to the advent of these devices.
Rights and permissions
About this article
Cite this article
Meng, Xt., Guan, Xf., Zhang, Hl. et al. Computer navigation versus fluoroscopy-guided navigation for thoracic pedicle screw placement: a meta-analysis. Neurosurg Rev 39, 385–391 (2016). https://doi.org/10.1007/s10143-015-0679-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-015-0679-2