Abstract
Purpose
Although pediatric spinal deformity correction using pedicle screws has a very low rate of complications, the long-term consequences of screw malposition is unknown. CT navigation has been proposed to improve screw accuracy. The aim of this study was to determine whether intraoperative navigation during pedicle screw placement in pediatric scoliosis makes screw placement more accurate. We also examined radiation exposure, operative time blood loss and complications with and without the use of CT navigation in pediatric spinal deformity surgery.
Methods
A systematic review of the literature was conducted. After screening, 13 articles were qualitatively and quantitatively analyzed to be used for the review. A random effects meta-analysis using REML methodology was employed to compare outcomes of screw accuracy, estimated blood loss, radiation exposure, and surgical duration.
Results
Screws placed with CT navigation surgery were three times as likely to be deemed “acceptable” compared with screws placed with freehand and 2D fluoroscopy assistance, twice as likely to be “perfect”, and only 1/3 as likely to be potentially unsafe (all p value < 0.01). EBL was not significantly different between groups; however, operative time was roughly thirty minutes longer on average. Random effects analysis showed no significant difference in effective dose radiation while using CT navigation (p = 0.06).
Conclusion
This systematic review of the literature demonstrates that intraoperative navigation results in more accurate pedicle screw placement compared to non-navigated techniques. We found that blood loss was similar in navigated and non-navigated surgery. Operative time was found to be approximately a half hour longer on average in navigated compared to non-navigated surgery. Effective radiation dose trended higher in navigated cases compared to non-navigated cases but did not reach statistical significance.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Scoliosis is a common pediatric orthopedic condition affecting 1.0–3.0% of children [1]. There is a strong familial predilection, and approximately 0.2–0.5% of children diagnosed with idiopathic scoliosis will require surgical treatment [2]. Surgical treatment is performed on otherwise healthy children to prevent undesirable outcomes later on in life [3], as such there is much focus on performing surgery in as safe a fashion as is possible. Pediatric spinal deformity surgery using pedicle screw fixation has become the gold standard for correcting spinal deformities in children and adolescents. Although this technique provides excellent correction and is associated with a low complication rate, disturbing accounts exist of pedicle screws abutting nervous tissue or vascular structures [4].
Accurate placement of pedicle screws is paramount to patient safety to minimize immediate and late complications of pedicle screw placement. There is higher risk of screw malposition in the thoracic spine particularly in the apical region on the concave side of a curve due to narrower pedicles that are in closer proximity to vital structures [5, 6]. In addition, congenital spinal deformity and syndromic pathology such as neurofibromatosis involve higher risk instrumentation due to abnormal or difficult anatomy [7]. Currently, the widely used “freehand” technique, with no intraoperative navigation, or freehand with intraoperative fluoroscopy has yielded generally acceptable results. However, due to the danger involved, research has endeavored to find safer ways of placing screws more accurately while still completing the surgery in an efficient fashion. CT-guided navigation has gained traction as the navigation option of choice in many centers. This technique provides real time 3-D imaging and characterization of the spinal anatomy and assists the surgeon in placement of implants. Proponents of the technique argue that it allows consistent accurate placement of pedicle screws, while opponents argue that the increased operative time, blood loss and radiation obviate the value of CT navigation.
The goal of this systematic review is to examine the accuracy of placement of pedicle screws with intraoperative CT guidance compared to placement without such guidance. We hypothesized that there would be increased accuracy of placement of pedicle screws with navigation compared to un navigated screws, but that the technique would be associated with greater blood loss, operative time and radiation as compared to non-navigated placement.
Materials and methods
Data sources
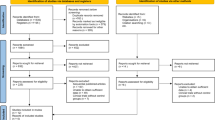
A comprehensive search of the literature databases EMBASE, SCOPUS, PubMed, Web of Science, and Cochrane was conducted. We selected articles from Jan 1, 2007 to June 1 2020 to identify prospective or retrospective comparative studies which looked at pediatric adolescent and young adult patients who underwent posterior spinal fusion for spinal deformity. There were multiple and various medical subject headings (MeSH terms) used for each database. Appendices 1 and 2 and the PRISMA checklist contain the exact inclusion/exclusion criteria and search terms used to identify studies. A summary of the search strategy is detailed in Fig. 1. Thirty full-text articles were then assessed for eligibility; three authors (K.D.B, J.B.A, and M.L.K) reviewed these, and if two of the three reviewers felt that the article should be kept, it was included in the review. 13 total studies were included in the analysis for the systematic review. Details of these articles can be found in Table 1.
Data extraction
Initial data extraction was performed by one author (MLK) and was subsequently verified by another author (KDB) and included the author name(s), title, abstract, date of publication, screw classification, screw malposition, OR return rate, OR time, radiation exposure, EBL, complications, and study limitations. Screw accuracy was defined in each article. Six articles used the Gertzbein classification for pedicle screw accuracy (Table 2). We defined a “optimal” screw as a screw completely within the pedicle, an “acceptable” screw as a screw < 2.0 mm out of the pedicle (Gertzbein grade 0 or 1) and a potentially unsafe screw either as defined in the article of interest or Gertzbein grade 3 (Table 2). Studies which this data could be extracted were used for the purposes of meta-analysis.
Estimated blood loss was extracted from three articles. We extracted mean blood loss and standard deviations. Where ranges were reported instead of standard deviations, we abstracted standard deviations under a normality assumption. EBL was reported in either milliliters or CC. Operative time was defined in three articles and reported in OR minutes. Frequency weighted means were produced for the purposes of reporting averages for these metrics. Effective dose radiation was reported by millisieverts (mSv) in three studies. One study looked at absorbed dose of radiation using mGy-cm as their units of measurement. We converted this data to millisieverts by calculation using a conversion factor of 1.0 mGy/cm = 0.017 mSv [8]. Data from these studies were analyzed using random effects meta-analysis to generate p values and sensitivity analyses were performed using select studies where indicated.
Our study contained 13 studies which encompassed a total of 651 patients. The patient populations were primarily AIS (six studies) [5, 9,10,11,12,13], followed by dystrophic NF1 (one study) [7], and general spinal deformity (one study) [14]. Five studies had mixed populations although the majority were AIS [15,16,17,18,19]. Ten studies used intraoperative navigation using the O-Arm navigation (Medtronic) [5, 7, 9, 12, 15,16,17,18,19,20], two studies used Vector Vision/ Brainlab [10, 13], and one study used GE/Light Speed [14]. Only two studies specified CT radiation settings for their study. Su et al. [20] specified that they used “pediatric” settings of 80 kV, 20 mA, 80 mAs; and Tormenti [14] specified 120 kV and 240 mAs, other studies did not specify settings used.
Data synthesis and analysis
To evaluate between-study variances among the parameters, we calculated I2 statistic and χ2 tests. I2 was found to be high and so A random-effects model with restricted maximum likelihood ratios was generated for our analysis. Continuity correction of 0.5 was applied as applicable when studies had zero cells. We calculated odds ratio or Hedge’s g effect size depending on the distribution of the data. A sensitivity analysis was performed without one study [7] in addition to the main analysis because Jin et al. used a population of NF-1 patients whereas the remainder of the studies used a majority of idiopathic scoliosis patients. All analysis was conducted using Stata 16 (College Station, TX).
Results
Screw classification and accuracy
Nine studies had data on accuracy of screw placement. This constituted 485 patients or 5578 screws. The majority of these (seven studies) used the Gertzbein rating system or a derivative of this system for judgment of screw accuracy (Table 2). Ughwanogho et al. [9] used a system of optimal, acceptable, potentially unsafe, and removed. Cui et al. [10] evaluated screws based on 2.0 mm increments, while Tormenti et al. [14] examined the breach of the pedicle wall and labeled screws as suboptimal or misplaced.
Six studies had sufficient data to compare “optimal” screws versus others. The summative odds in our random effects model showed that placing an optimal screw was twice as high using CT navigation compared to no navigation [OR 2.36 (1.12, 4.99); p value < 0.01] (Fig. 2). In total 75.6% of navigated screws were optimal versus 58.5% of non-navigated screws in these six studies. A sensitivity analysis was performed eliminating the Jin et al. [7] study because NF patients may represent a clinically significant subgroup compared to the remaining studies. This sensitivity analysis also showed CT navigation resulted in more optimally placed screws when the Jin paper was eliminated (p value 0.02).
Six studies had sufficient data to compare “acceptable” screws (Gertzbein 1 or 2). Summative odds of placing an “acceptable” screw (Gertzbein grade 0 or 1) was 3.0 times higher using navigation compared to no navigation [OR 3.17 (1.51, 6.65); p value < 0.01] (Fig. 3). 75.1% of non-navigated screws were acceptable versus 93.9% of navigated screws. A sensitivity analysis was performed eliminating the Jin et al. [7] study once again. The result showed that more acceptable screws were placed with CT navigation (p value < 0.01).
Navigation was 1/3rd as likely to produce a potentially unsafe screw (Gertzbein 3 or equivalent) compared to non-navigated screws [OR 0.35 (0.25, 0.50); p value < 0.001] (Fig. 4). This constituted 7.0% of non-navigated screws and 1.9% of navigated screws. A sensitivity analysis was performed eliminating the Jin et al. [7] study once again. The result still showed less potentially unsafe screws placed with CT navigation (p value 0.01). The navigation group had 2 intraoperative neuromonitoring alerts [9]. The non-navigation cohort reported four CSF leaks during screw insertion [7, 10, 15, 16], 2 radiculopathies and one patient with persistent pain [14, 15, 17], two bilateral pleural effusions [9], one IOMN alert [9], one incomplete paralysis [10], and one asymptomatic screw abutting the aorta [15]. Six patients were taken back to the OR in the freehand group and zero in the navigation group.
EBL and operative time
Estimated blood loss was not significantly different between groups (1131.0 cc vs 1077.0 cc). Random effects meta-analysis showed a non-significant difference between groups (p value 0.91) (Fig. 5). Operative time was longer for CT navigation compared to non-navigated cases [446.0 min navigated vs 412.0 min non-navigated (p value 0.04)] (Fig. 6).
Radiation exposure
All four studies which examined radiation exposure were converted to millisieverts then compared using a random effects model. Although radiation exposure trended higher in the navigated group compared to the non-navigated group the difference was not statistically significant due to the high degree of variance (p value 0.06) (Fig. 7). Of note, three out of four studies [12, 18, 20] showed a significant difference in radiation exposure during CT navigation which favored freehand with fluoroscopic assistance, two of these used effective dose [18, 20] and one used absorbed dose [12] as the metric of measurement. The final study [19] showed no difference in radiation in patients with smaller curves but showed significantly lower radiation using CT navigation when the starting curve was 74.0 degrees or higher. Because one paper used a metric of mGy/cm, we performed a sensitivity analysis without that paper which also showed a non-significant difference between navigated and non-navigated technique in terms of radiation imparted to the patient (p 0.18).
Discussion
Pedicle screw fixation has become standard of care for surgical treatment of pediatric spinal deformity. The technique though widely applied originally in the lumbar spine has also become standard of care for deformity in the thoracic spine. Suk et al. [21] has previously shown this technique to be safe and effective for treating spinal deformities. Pedicle screw fixation allows for a high degree of control of the spinal deformity through three column fixation, allowing for superior three-dimensional correction. Kim et al. [22] subsequently described a “free hand” technique by which spinal anatomy can be used to reliably place pedicle screws in a safe fashion. This may be more difficult in the concave apex of a deformity where the pedicles can be less than 2.0 mm in diameter and the axial plane may not be consistently rotated [23]. In addition, disturbing case reports exist of misplaced pedicle screws abutting visceral, vascular or neurologic structures [24,25,26,27,28,29]. Because the majority of scoliosis surgeries are done in the setting of an asymptomatic child to prevent an adverse outcome in the future, there is an understandable focus on performing surgical procedures in the safest way possible. As such, intra operative CT navigation was developed to improve the accuracy of screw placement in scoliosis surgery. Controversy exists regarding this technique with proponents arguing that the technique allows for more accurate placement of screws whereas detractors argue that utilization of the technology imparts large amounts of radiation to a growing child, results in a longer surgical case with more blood loss, detracts from trainee education, and results in surgeon over reliance on technology. The goal of this systematic review and meta-analysis is to examine the available evidence on intraoperative CT navigation for placement of pedicle screws in pediatric spinal deformity to assess its effect on accuracy of screw placement, radiation exposure, blood loss, surgical time and complications.
Our study found accuracy to be positively affected by usage of intraoperative CT navigation. Random effects analysis showed that overall pedicle screws were nearly twice as likely to be optimally placed, three times as likely to be acceptably placed, and only 1/3rd as likely to be potentially unsafe as screws placed by freehand technique alone or with fluoroscopy. This result was relatively consistent among studies. Not surprisingly, Liu et al. [5] found this difference to be particularly pronounced in very small pedicles (< 2 mm). These authors also [5] found that in the free hand technique, accuracy was correlated negatively with pedicle diameter whereas in the CT navigation group it was not. Tormenti et al. [14] reported a 4.3 times lower rate of pedicle screw breach with navigation compared to non- navigated technique (5.2% compared to 1.2%). Subgroup analysis confirmed even when removing the study with primarily dystrophic NF-1 patients [7] from the analysis the accuracy of screw placement was still significantly improved with CT navigation compared to non-navigated placement. This finding has also been reproduced in early onset, congenital and neuromuscular scoliosis [30,31,32]. The exception to this rule is the paper by Urbanski et al. [12] which showed no increase in accuracy using CT navigation versus freehand, though their freehand group did have four grade 3 screws compared to zero in the navigated group.
Radiation exposure is always a concern in growing children. The stochastic effects of radiation can be magnified in children due to their longer life span and rapidly dividing nature of their tissues [33,34,35]. Our meta-analysis showed that there was no statistically significant increase in radiation between usage of intraoperative CT navigation versus freehand technique. We found a great degree of variance in the effect size between studies. As such, this finding is likely confounded by a number of factors. Radiation imparted by intraoperative CT navigation is a fixed quantity, and varies by the number of scans necessary, and the imaging protocol used which is a function of the length of the patient, and the protocols of the institution, respectively. Urbanski et al. [12] reported using between 1.0 and 4.0 CT scans based on the length of the patient and the length of the fusion necessary; whereas, Richerand et al. [18] used 1.0 or 2.0 CT scans, also dependent on the length of the patient. Number of scans can be reduced in the modern era with navigation through usage of cannulated hardware which eliminates the need for a second CT scan to check final position of screw placement. If a CT is used to routinely check screws placed by freehand use of cannulated instrumentation may eliminate the theoretical radiation advantage freehand technique has over CT navigation by eliminating need for a second CT. Fluoroscopy, on the other hand, has a varying dose which is dependent on total fluoroscopy time. This may change based on the degree difficulty of the operation as shown by Riis et al. [19] or simply the experience level of the surgeon, as with other outcomes of scoliosis surgery [35]. Pediatric dosing protocols are also available that allow for a low level of radiation for CT-based navigation. Second, the wide variance in imparted radiation in the identified studies in this review is an indication of differing protocols. It should be noted that actual settings of the navigation device were only specified by two studies [14, 20], but settings applied can greatly influence the total dose imparted to the patient. This variance is characterized by the Urbanski et al. [12] paper which supplied no detail regarding dosing protocol, or a dose per CT in the manuscript. The average patient in this study received 1071.0 ± 447 mGy-cm versus 391.0 ± 53 mGy-cm or18.4 vs 6.7 mSv which is substantially higher than both the CT navigation and freehand group in any other study examined [12]. Su et al. [20] on the other hand used a pediatric protocol (80 kV–20 mA–80mAs) CT scan which imparted 0.65 mSv per scan for an average of 1–2 scans per patient. Surgeons should be aware of their institutional dosing protocols when using this technology [11, 20]. Third, patient-specific factors are important as Richerand et al. [18] showed very high effective doses of radiation in obese children while using CT navigation. Demographic data, or clinical data such as weight and curve magnitude were inconsistently reported in the studies of radiation but are known confounders in the comparison between CT navigation and freehand in terms of radiation exposure.
Nelson et al. [36] showed that even with a higher dose CT scan, an intraoperative CT imparts similar radiation to 1.3–2.5 spine radiographs or about 54.0 s of live fluoroscopy. Previous studies have shown fluoroscopy times imparting doses up to 2.92 mSv of radiation [37, 38]. As such in spite of variations in practice and likely skill level which characterized the various studies which comprised this meta-analysis, it seems clear that radiation imparted by CT navigation is at the very least more predictable than fluoroscopy, and likely not as operator-dependent [39]. Even working off the assumption that radiation is increased by CT scan, it seems feasible to decrease the number of follow up scoliosis films by one per spin taken particularly since these x-rays have been found not to change management in the first two years post spinal fusion [40]. Riis [19] found that CT assisted navigation became more helpful in terms of relative amounts of radiation with curves larger than 74 degrees, but cautioned that small numbers in his study may limit the generalizability of his results. It stands to reason that there may be differences in patient, curve and technique considerations that may tip the risk benefit ratio in terms of radiation exposure to favor navigation or non-navigation depending on the situation. The data available in this study do not provide enough guidance and future studies should focus on this. At the very least low dose CT protocols allow the operating room staff to stand behind a lead shield or leave the room entirely which can decrease the additive effects of radiation over a career.
Our study found that EBL is similar between navigated and non-navigated groups and navigated groups. The average EBL was close to a liter in all groups. By contrast, operative time averaged about thirty minutes longer in the navigated group. This likely is due to setup time of the navigation system and the time required to obtain and register the CT scan. Though processes can be improved which make obtaining the CT more expeditious, surgeons should be aware that there is a staff-related learning curve that can cause delays at the outset of such a process. Flynn et al. [41] reported in 2018 a protocol to complete two AIS PSF prior to 5 pm in the same OR room using intra-operative CT navigation. This seems to indicate that when a well thought out protocol is employed, the technology is not a rate-limiting factor to surgical completion time. Larson et al. [31] when reporting their experience using the CT-guided navigation stated that while the overall OR time was longer in the navigation compared to the freehand group but when controlling for number of levels fused, the difference was not significant at less than three minutes per level (58.3 vs 61.5 min/level p = 0.63) [15].
The navigated cohort had a very low rate of complications. There were two intraoperative neuromonitoring alerts which both responded to increases in blood pressure. There were no other reported potentially implant related complications. Although we included these neuromonitoring events as potentially implant related, no mention was made of hardware removal or replacement of these screws in this study [9]. Six returns to the operating room were reported in the non-navigation group, one due to a dural leak, two due to pain and medial pedicle screw position, one due to asymptomatic abutment of the aorta, and two due to radicular symptoms caused by screws abutting nerve roots [5, 14, 15]. Zero such returns occurred in the navigation group. Other potentially instrumentation related complications in the non-navigation group were two cases of pleural effusions, one case of intra operative neuromonitoring alert, two additional CSF leaks, and one incomplete paralysis, though it should be noted that authors of this study felt that this complication was not implant-related [7, 9, 10]. Unfortunately, due to the nature and consistency of the reporting in the studies which make up this analysis, CT navigation cannot be directly compared to non-navigated surgery in terms of complications. However, the increased accuracy we found along with the complication data we did identify underscores the importance of accurate placement of pedicle screws. It bears mentioning additionally that many studies utilized intraoperative CT scan to check screws after placement. As such, many more grade 3 screws found in our analysis were likely revised or removed prior to finalizing the spinal fusion surgery likely decreasing the revision rate. Furthermore, the literature supports navigation in decreasing the unplanned return to the operating room (UPROR) rate to a never event (0.0%) in AIS surgery regardless of volume, experience, or training [15, 42]. This suggests that navigation may provide an overall value benefit to the healthcare system, patient, and patient’s family.
This study is not without its limitations. As a collection of retrospective studies, the study is vulnerable to bias confounding and chance of member studies. The findings of increased accuracy of CT navigated surgery are highly consistent, however, throughout the literature with the exception of one study we were able to identify [12]. Secondly, designations of screws as “optimal”, “acceptable”, and “potentially unsafe” though arbitrary, are at least based on a consistent classification. Additionally, we have no reason to suspect that these designations should bias our results in any direction as they are based on the Gertzbein classification. Our radiation results are based on reports from the member studies; however, it was not specifically clear which sources of radiation “counted” towards total radiation. In addition, for studies which examined radiation doses, dosing protocol and even method of measurement varied. After review of these papers, it seems clear that at the very least, CT navigation is associated with more consistent levels of radiation which can be accounted for by changes in post-op protocol to allow similar levels of cumulative radiation. Fluoroscopy is variable, and doses can change with difficulty of the case and experience of the surgeon. Finally, the populations were varied in the identified studies, and though the majority were AIS, it is difficult to say based on this data if some patients may benefit more than others from this technology, although there were data available in this review to suggest that patients with larger deformities and smaller pedicles may show more benefit.
In conclusion, usage of CT navigation results in more accurate screw placement. Member studies indicated that these findings are most pronounced in smaller pedicles, and in the apical region of the curve. Surgeons who wish to improve the accuracy of their screw placement particularly with difficult anatomy should strongly consider employing intraoperative CT navigation. Surgical times are about a half hour longer on average when using CT navigation. Estimated blood loss is comparable, and radiation dosing may be larger but this depends strongly on dosing protocol used and is generally more predictable than fluoroscopy. Utilizing low-dose pediatric CT protocols along with changes in post-operative x-ray documentation of the spinal fusion may be able to yield comparable radiation doses to free hand technique. This type of comprehensive planning may actually be able to decrease radiation by increasing the predictability of the effective radiation dose to the patient. There appear to be fewer implant related complications when using navigation although it is difficult to say for sure with this meta-analysis. Although navigation with CT and other techniques has become more prevalent; based on the data we present here we recommend surgeons consider adding it to their practice if they have not already done so. If surgeons choose to employ free hand technique without CT navigation, we recommend CT documentation of pedicle screws prior to leaving the operating room. We recognize that this may eliminate the radiation benefits that may be seen in freehand technique, however, it may avoid potential issues with screw misplacement and returns to the operating room documented in this meta-analysis.
References
Weinstein SL, Dolan LA, Cheng JC, Danielsson A, Morcuende JA (2008) Adolescent idiopathic scoliosis. Lancet 371(9623):1527–1537. https://doi.org/10.1016/S0140-6736(08)60658-3 (published Online First: Epub Date)
Chan A, Parent E, Narvacan K, San C, Lou E (2017) Intraoperative image guidance compared with free-hand methods in adolescent idiopathic scoliosis posterior spinal surgery: a systematic review on screw-related complications and breach rates. Spine J 17(9):1215–1229. https://doi.org/10.1016/j.spinee.2017.04.001 (published Online First: Epub Date)
Ascani E, Bartolozzi P, Logroscino CA et al (1986) Natural history of untreated idiopathic scoliosis after skeletal maturity. Spine (Phila Pa 1976) 11(8):784–789. https://doi.org/10.1097/00007632-198610000-00007 (published Online First: Epub Date)
Valic M, Zizek D, Span M, Mihalic R, Mohar J (2020) Malpositioned pedicle screw in spine deformity surgery endangering the aorta: report of two cases, review of literature, and proposed management algorithm. Spine Deform 8(4):809–817. https://doi.org/10.1007/s43390-020-00094-5 (published Online First: Epub Date)
Liu Z, Jin M, Qiu Y, Yan H, Han X, Zhu Z (2016) The Superiority of Intraoperative O-arm navigation-assisted surgery in instrumenting extremely small thoracic pedicles of adolescent idiopathic scoliosis: a case-control study. Medicine (Baltimore) 95(18):e3581. https://doi.org/10.1097/MD.0000000000003581 (published Online First: Epub Date)
Heidenreich M, Baghdadi YM, McIntosh AL et al (2015) At what levels are freehand pedicle screws more frequently malpositioned in children? Spine Deform 3(4):332–337. https://doi.org/10.1016/j.jspd.2014.12.003 (published Online First: Epub Date)
Jin M, Liu Z, Liu X et al (2016) Does intraoperative navigation improve the accuracy of pedicle screw placement in the apical region of dystrophic scoliosis secondary to neurofibromatosis type I: comparison between O-arm navigation and free-hand technique. Eur Spine J 25(6):1729–1737. https://doi.org/10.1007/s00586-015-4012-0 (published Online First: Epub Date)
de Broucker T, Pontana F, Santangelo T et al (2012) Single- and dual-source chest CT protocols: levels of radiation dose in routine clinical practice. Diagn Interv Imaging 93(11):852–858. https://doi.org/10.1016/j.diii.2012.07.009 (published Online First: Epub Date)
Ughwanogho E, Patel NM, Baldwin KD, Sampson NR, Flynn JM (2012) Computed tomography-guided navigation of thoracic pedicle screws for adolescent idiopathic scoliosis results in more accurate placement and less screw removal. Spine (Phila Pa 1976) 37(8):E473–E478. https://doi.org/10.1097/BRS.0b013e318238bbd9 (published Online First: Epub Date)
Cui G, Wang Y, Kao TH et al (2012) Application of intraoperative computed tomography with or without navigation system in surgical correction of spinal deformity: a preliminary result of 59 consecutive human cases. Spine (Phila Pa 1976) 37(10):891–900. https://doi.org/10.1097/BRS.0b013e31823aff81 (published Online First: Epub Date)
Su AW, Luo TD, McIntosh AL et al (2016) Switching to a pediatric dose O-arm protocol in spine surgery significantly reduced patient radiation exposure. J Pediatr Orthop 36(6):621–626. https://doi.org/10.1097/BPO.0000000000000504 (published Online First: Epub Date)
Urbanski W, Jurasz W, Wolanczyk M et al (2018) Increased radiation but no benefits in pedicle screw accuracy with navigation versus a freehand technique in scoliosis surgery. Clin Orthop Relat Res 476(5):1020–1027. https://doi.org/10.1007/s11999.0000000000000204 (published Online First: Epub Date)
Sakai Y, Matsuyama Y, Nakamura H et al (2008) Segmental pedicle screwing for idiopathic scoliosis using computer-assisted surgery. J Spinal Disord Tech 21(3):181–186. https://doi.org/10.1097/BSD.0b013e318074d388 (published Online First: Epub Date)
Tormenti MJ, Kostov DB, Gardner PA, Kanter AS, Spiro RM, Okonkwo DO (2010) Intraoperative computed tomography image-guided navigation for posterior thoracolumbar spinal instrumentation in spinal deformity surgery. Neurosurg Focus 28(3):E11. https://doi.org/10.3171/2010.1.FOCUS09275 (published Online First: Epub Date)
Baky FJ, Milbrandt T, Echternacht S, Stans AA, Shaughnessy WJ, Larson AN (2019) Intraoperative computed tomography-guided navigation for pediatric spine patients reduced return to operating room for screw malposition compared with freehand/fluoroscopic techniques. Spine Deform 7(4):577–581. https://doi.org/10.1016/j.jspd.2018.11.012 (published Online First: Epub Date)
Zhao Z, Liu Z, Hu Z et al (2018) Improved accuracy of screw implantation could decrease the incidence of post-operative hydrothorax? O-arm navigation vs. free-hand in thoracic spinal deformity correction surgery. Int Orthop 42(9):2141–2146. https://doi.org/10.1007/s00264-018-3889-8 (published Online First: Epub Date)
Kotani Y, Abumi K, Ito M et al (2007) Accuracy analysis of pedicle screw placement in posterior scoliosis surgery: comparison between conventional fluoroscopic and computer-assisted technique. Spine (Phila Pa 1976) 32(14):1543–1550. https://doi.org/10.1097/BRS.0b013e318068661e (published Online First: Epub Date)
Dabaghi Richerand A, Christodoulou E, Li Y, Caird MS, Jong N, Farley FA (2016) Comparison of effective dose of radiation during pedicle screw placement using intraoperative computed tomography navigation versus fluoroscopy in children with spinal deformities. J Pediatr Orthop 36(5):530–533. https://doi.org/10.1097/BPO.0000000000000493 (published Online First: Epub Date)
Riis J, Lehman RR, Perera RA et al (2017) A retrospective comparison of intraoperative CT and fluoroscopy evaluating radiation exposure in posterior spinal fusions for scoliosis. Patient Saf Surg 11:32. https://doi.org/10.1186/s13037-017-0142-0 (published Online First: Epub Date)
Su AW, McIntosh AL, Schueler BA et al (2017) How does patient radiation exposure compare with low-dose O-arm versus fluoroscopy for pedicle screw placement in idiopathic scoliosis? J Pediatr Orthop 37(3):171–177. https://doi.org/10.1097/BPO.0000000000000608 (published Online First: Epub Date)
Suk SI, Kim WJ, Lee SM, Kim JH, Chung ER (2001) Thoracic pedicle screw fixation in spinal deformities: are they really safe? Spine (Phila Pa 1976) 26(18):2049–2057. https://doi.org/10.1097/00007632-200109150-00022 (published Online First: Epub Date)
Kim YJ, Lenke LG, Bridwell KH, Cho YS, Riew KD (2004) Free hand pedicle screw placement in the thoracic spine: is it safe? Spine (Phila Pa 1976) 29(3):333–342. https://doi.org/10.1097/01.brs.0000109983.12113.9b (discussion 42, published Online First: Epub Date)
Parent S, Labelle H, Skalli W, de Guise J (2004) Thoracic pedicle morphometry in vertebrae from scoliotic spines. Spine (Phila Pa 1976) 29(3):239–248. https://doi.org/10.1097/01.brs.0000109995.64028.fe (published Online First: Epub Date)
Sarwahi V, Suggs W, Wollowick AL et al (2014) Pedicle screws adjacent to the great vessels or viscera: a study of 2132 pedicle screws in pediatric spine deformity. J Spinal Disord Tech 27(2):64–69. https://doi.org/10.1097/BSD.0b013e31825bfecd (published Online First: Epub Date)
Kayaci S, Cakir T, Dolgun M et al (2019) Aortic injury by thoracic pedicle screw. When is aortic repair required? Literature review and three new cases. World Neurosurg 128:216–224. https://doi.org/10.1016/j.wneu.2019.04.173 (published Online First: Epub Date)
Schermann H, Mirovsky Y, Chechik Y (2019) Delayed penetration of the thoracic aorta by pedicle screws: a case report of screws left as-is. Spine (Phila Pa 1976) 44(19):1169–1171. https://doi.org/10.1097/BRS.0000000000003094 (published Online First: Epub Date)
Sevuk U, Mesut A, Kiraz I, Kose K, Ayaz F, Erkul A (2016) Delayed presentation of aortic injury by a thoracic pedicle screw. J Card Surg 31(4):220–230. https://doi.org/10.1111/jocs.12718 (published Online First: Epub Date)
Mirza AK, Alvi MA, Naylor RM et al (2017) Management of major vascular injury during pedicle screw instrumentation of thoracolumbar spine. Clin Neurol Neurosurg 163:53–59. https://doi.org/10.1016/j.clineuro.2017.10.011 (published Online First: Epub Date)
Pesenti S, Bartoli MA, Blondel B, Peltier E, Adetchessi T, Fuentes S (2014) Endovascular aortic injury repair after thoracic pedicle screw placement. Orthop Traumatol Surg Res 100(5):569–573. https://doi.org/10.1016/j.otsr.2014.03.020 (published Online First: Epub Date)
Larson AN, Polly DW Jr, Guidera KJ et al (2012) The accuracy of navigation and 3D image-guided placement for the placement of pedicle screws in congenital spine deformity. J Pediatr Orthop 32(6):e23–e29. https://doi.org/10.1097/BPO.0b013e318263a39e (published Online First: Epub Date)
Larson AN, Santos ER, Polly DW Jr et al (2012) Pediatric pedicle screw placement using intraoperative computed tomography and 3-dimensional image-guided navigation. Spine (Phila Pa 1976) 37(3):E188–E194. https://doi.org/10.1097/BRS.0b013e31822a2e0a (published Online First: Epub Date)
Baghdadi YM, Larson AN, McIntosh AL, Shaughnessy WJ, Dekutoski MB, Stans AA (2013) Complications of pedicle screws in children 10 years or younger: a case control study. Spine (Phila Pa 1976) 38(7):E386–E393. https://doi.org/10.1097/BRS.0b013e318286be5d (published Online First: Epub Date)
UNSCEAR (2006) Effects of ionizing radiation, United Nations Scientific Committee on the effects of atomic radiation. UNSCEAR 2006 report to the general assembly Volume I, with Scientific Annexes. United Nations, New York
Humans IWGotEoCRt (2000) Ionizing radiation, Part 1: X- and Gamma (γ)-radiation, and neutrons. WHO, Lyon
Cahill PJ, Pahys JM, Asghar J et al (2014) The effect of surgeon experience on outcomes of surgery for adolescent idiopathic scoliosis. J Bone Joint Surg Am 96(16):1333–1339. https://doi.org/10.2106/JBJS.M.01265 (published Online First: Epub Date)
Nelson EM, Monazzam SM, Kim KD, Seibert JA, Klineberg EO (2014) Intraoperative fluoroscopy, portable X-ray, and CT: patient and operating room personnel radiation exposure in spinal surgery. Spine J 14(12):2985–2991. https://doi.org/10.1016/j.spinee.2014.06.003 (published Online First: Epub Date)
Perisinakis K, Theocharopoulos N, Damilakis J et al (2004) Estimation of patient dose and associated radiogenic risks from fluoroscopically guided pedicle screw insertion. Spine (Phila Pa 1976) 29(14):1555–15560. https://doi.org/10.1097/01.brs.0000131214.57597.21 (published Online First: Epub Date)
Slomczykowski M, Roberto M, Schneeberger P, Ozdoba C, Vock P (1999) Radiation dose for pedicle screw insertion. Fluoroscopic method versus computer-assisted surgery. Spine (Phila Pa 1976) 24(10):975–982. https://doi.org/10.1097/00007632-199905150-00009 (discussion 83, published Online First: Epub Date)
Malik AT, Rai HH, Lakdawala RH, Noordin S (2019) Does surgeon experience influence the amount of radiation exposure during orthopedic procedures? A systematic review. Orthop Rev (Pavia) 11(1):7667. https://doi.org/10.4081/or.2019.7667 (published Online First: Epub Date)
Garcia GH, Park MJ, Baldwin K, Flynn J, Spiegel DA (2013) Do routine radiographs within the first two years following pediatric posterior spinal fusion prompt revision surgery? Spine (Phila Pa 1976) 38(25):2216–2220. https://doi.org/10.1097/BRS.0000000000000018 (published Online First: Epub Date)
Flynn JM, Striano BM, Muhly WT et al (2018) A dedicated pediatric spine deformity team significantly reduces surgical time and cost. J Bone Joint Surg Am 100(18):1574–1580. https://doi.org/10.2106/JBJS.17.01584 (published Online First: Epub Date)
Bauer JM, Moore JA, Rangarajan R et al (2018) Intraoperative CT scan verification of pedicle screw placement in AIS to prevent malpositioned screws: safety benefit and cost. Spine Deform 6(6):662–668. https://doi.org/10.1016/j.jspd.2018.04.010 (published Online First: Epub Date)
Funding
No funds, grants, or other support was received.
Author information
Authors and Affiliations
Contributions
KDB, MK, DT, WNS, JMF, JBA: conception or design of work; Acquisition, analysis, or interpretation of data for the work; Drafting of work or revising it critically for important intellectual content; Final approval of version to be published.
Corresponding author
Ethics declarations
Conflict of interest
KDB owns stock in Pfizer, Inc. JMF reports royalties or other material support from Wolters Kluwer Health and Biomet and serves as a board member of the American Board of Orthopaedic Surgery. All other authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This study did not require IRB approval as no subject data was accessed.
Informed consent
This study did not require informed consent as no subject data was accessed.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Baldwin, K.D., Kadiyala, M., Talwar, D. et al. Does intraoperative CT navigation increase the accuracy of pedicle screw placement in pediatric spinal deformity surgery? A systematic review and meta-analysis. Spine Deform 10, 19–29 (2022). https://doi.org/10.1007/s43390-021-00385-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-021-00385-5