Abstract
A number of studies have shown increased accuracy of pedicle screw placement in spine with the help of computer-assisted navigation. The literature is lacking in regard to functional benefit derived from this technique. The aim of this systematic review was to look at the functional outcomes following computer-assisted pedicle screw placement in spine. A ‘Dialog Datastar’ search was used using optimized search strategy covering the period from 1950 to July 2009; 23 papers were finally included which met our inclusion criteria. We report on a total of 1,288 patients with 5,992 pedicle screws. The comparison of neurological complications in two groups demonstrated an odds ratio of 0.25 (95% CI 0.06, 1.14) in favour of using navigation for pedicle screw insertion (p = 0.07). Comparative trials demonstrated a significant advantage in terms of accuracy of navigation over conventional pedicle screw insertion with a relative risk of 1.12 (95% CI 1.09, 1.15) (p < 0.00001). Navigation does not show statistically significant benefit in reducing neurological complications and there was insufficient data in the literature to infer a conclusion in terms of fusion rate, pain relief and health outcome scores.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The reported pedicle screw misplacement in historical spinal literature can be as high as 20–39.8% [1–3], but only a small number leads to complications (neurological, vascular or visceral injuries). But these complications can be potentially life and limb threatening. Computer-assisted navigation allows for simultaneous and multi-planar visualization of spinal anatomy which helps in virtually tracking surgical instruments in relation to displayed anatomy in real time [4]. This has led to its utilisation in pedicle screw placement thus increasing the accuracy of screw positioning in cadavers and patients [5–9].
The question then arises, that does this increased accuracy in screw placement lead to a significant decrease in the complication rates from the misplacement of pedicle screws or increased functional outcomes in terms of better fusion rates, improved pain scores and superior health outcome measures?
The primary research objective for this systematic review was to investigate whether accurate placement of pedicle screws, with the help of navigation, gives benefits in terms of avoidance of neurological complications, improved pain relief, improved fusion rates and better health outcome scores such as Oswestry disability index, SF-36 or SF-12 scores. Our secondary aim was to look at the accuracy of pedicle screw placement with navigation.
Materials and methods
We conducted a systematic review and meta-analysis of the available studies of computer-assisted pedicle screw insertion using the quality of reporting of meta-analysis (QUOROM) guidelines for synthesis of information from the relevant existing literature [10].
Literature identification and inclusion/exclusion criteria
The abstracts and titles of all the articles in: MEDLINE (1950 to July 2009), EMBASE (1974 to July 2009) and CINAHL (1982 to July 2009) were searched via ‘Dialog Datastar’ with the following key words: pedicle screw and navigation. Thesaurus mapping was then used to explode this search with “spine” and combining these searches with the Boolean linkage terms AND and OR to identify relevant publications.
The complete articles identified by the above search methodology were retrieved and assessed against the inclusion/exclusion criteria outlined in Table 1. Additionally, the cross-references in the trials retrieved electronically were hand searched.
Data collection
The data collected from the qualifying articles was: indication for surgery, number of patients, vertebral level(s) instrumented, number of pedicle screws, neurological loss and patient-based outcome measures (fusion rates, Oswestry disability index, SF-36, SF-12, and pain scores) where available. Data was extracted independently by two reviewers, R.V. and S.K. except for articles in German language which was done by K.H. Any discrepancy was resolved mutually and if necessary by third party agreement (A.M.). In view of paucity of randomised controlled trials and heterogeneous nature of trials, we did not use a formal scoring method for assessing quality of studies. Instead, we critically appraised the studies using a checklist designed to assess the methodological quality of both randomised and non-randomised studies [11].
Statistical methodology
Data was pooled separately for studies with control group and for those studies without control group.
Randomised and case–control studies
Summary statistics was created by calculating odds ratio with 95% confidence interval for the various functional outcomes. Heterogeneity was tested using I2 statistics. As there was high heterogeneity in the studies, random effects model was used. Data was entered and analysed in Revman 4.2 [http://www.cochrane.org/ (2008)].
Case series
The case series data was pooled using an inverse variance method weighted for the size of the study. This pooled data was analysed by random effects model.
Results
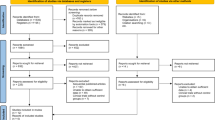
The electronic search methodology identified 67 possibly relevant publications, while the hand search of the references of these 67 articles identified a further four articles resulting in 71 papers being reviewed. At review, 48 papers were excluded as they did not meet the inclusion criteria (Table 1). Thus, 23 publications [5, 6, 8, 9, 12–30] were analysed in this paper (Table 2; 2 randomised controlled trials, 12 case–control studies and 9 case series). Three studies were in German language and remaining 20 studies were in English.
These 23 studies in essence include: 719 patients (3,555 pedicle screws inserted with the help of navigation techniques) with an age range of 13–61.2 years and 569 patients (2,437 pedicle screws inserted without the help of navigation techniques) with an age range of 15.4–60.2. The indication for surgery varied widely across the different studies including correction for kyphosis and scoliosis, treatment for metastasis, rheumatoid arthritis and trauma. The surgery was performed at all levels and did not exclude any particular level.
Neurological complication
All of the analysed studies reported about presence or absence of neurological complications as a result of pedicle screw insertion. Navigational techniques were used to insert pedicle screws in 327 patients (9 case series) and 392 patients (2 RCT’s and 12 case–control studies). There were no reported cases of neurological complications in navigational group in either series. On the other hand, conventional pedicle screws were inserted in 569 patients (2 RCT’s, 12 case–control studies) leading to 13 cases of neurological complications (2.3%). The meta-analysis undertaken (Fig. 1) demonstrated relative odds ratio of 0.25 (95% CI of 0.06–1.14) in favour of using navigation for pedicle screw insertion; however, this result was not statistically significant (p = 0.07).
Forest plot showing neurological complications in comparative trials. Individual studies are plotted on y-axis with a summary estimate at the bottom. The point estimates (blue squares) are shown on a line that represents their associated 95% confidence interval. The odds ratio (OR) is shown towards the right of the diagram with the pooled estimate calculated with the random-effects model at the bottom. The pooled estimate suggests that risk of neurological complications decreases with navigation
Kotani et al. [29] reported a girl in the non-navigational group, developing a neurological loss after 4 years. She was included in the analysis as the cause was found to be screw perforation and symptoms resolved with screw removal. Seichi et al. [16] reported a case of neurological loss (cervical myelopathy) which was due to tumour re-growth thus this was not included in the analysis.
Fusion rate
Six studies [12, 13, 19, 24, 26, 30] reported follow-up period ranging from 15 to 34 months, while one study followed the patients to clinical and radiological bony fusion [16], but none reported on rate of fusion achieved.
Pain relief and health outcome scores
Amiot et al. reported that two of their patients in the navigation group had dysesthesia in the post-operative period but a conservative approach was followed with symptom resolution at 6 months. While, Ito et al. reported that the Ranawat’s pain score in their ten rheumatoid arthritis patients improved from 1.4 to 1 in the navigation group and from 1.6 to 1.2 in non-navigational group.
No study gave the health outcome scores like the Oswestry disability index or SF-36/12 scores.
Accuracy
All 23 studies (n = 5,992 screws) provided accuracy data. Amiot et al. and Seller et al. used magnetic resonance imaging (MRI) for grading post-operative accuracy while other authors used computerised tomography techniques (CT scan) [5, 6, 8, 9, 12–30].
A total of 93.3% (n/N = 3,316/3,555) of the pedicle screws were inserted accurately with navigational techniques, whereas 84.7% (n/N = 2,064/2,437) were inserted accurately with non-navigational techniques. Meta analysis of the 14 studies with control group (RCT = 2, case–control studies = 12), i.e. 1,838 pedicle screws from the navigation group and 2,437 from the non-navigational group showed a significant advantage (p < 0.00001) of navigation over non-navigation (conventional) pedicle screw insertion with a relative risk of 1.12, with a 95% CI 1.09, 1.15 (see Fig. 2). Pooled data from the nine case series (1,717 screws, 48%) that used navigational techniques also showed accurate placement of pedicle screws (risk ratio was 0.92 with 95% CI 0.88, 0.96).
Forest plot showing accuracy of placement of pedicle screws in comparative trials. The relative risk (RR) is shown towards the right of the diagram with the pooled estimate calculated with the random-effects model at the bottom. The diagrammatic pooled estimate (diamond) and numerical relative risk both shows that navigation helps in more accurate placement of pedicle screws
Discussion
Pedicle screws have become the favoured method of posterior spinal fixation since being popularised by Roy-Camille [31]. Biomechanical studies have shown that pedicle screws provide increased rigidity and construct stiffness compared to other posterior fixation techniques [32, 33]. It is a technically demanding procedure and studies have shown an alarmingly high rate of screw misplacement varying between 21 and 39.8% with conventional insertion techniques [1–3]. The misplaced screws can cause three types of complications, namely neurological, vascular and mechanical.
Neurological complication while inserting pedicle screws is a rare but serious complication, which can be avoided by careful planning of the surgery. Theoretically, image-guided navigation techniques can help the surgeon in preventing the complication by providing accurate anatomic guidance for the procedure. However, Schulze et al. [34] have argued that experienced surgeons can accurately place pedicle screws in 80% of cases with conventional techniques and neurological symptoms are rarely affected by an inaccurate pedicle screw even if the penetration of the pedicle wall is more than 6 mm. In our meta-analysis, pedicle screw insertion by navigational techniques have caused fewer incidences of neurological complications than conventional methods though this was not statistically significant (p = 0.07). We think this could be due to lack of big randomised trials as the incidence of neurological complications is low and none of our studies had big numbers required for narrow confidence intervals.
We were unable to make conclusions regarding the fusion rates after computer-assisted surgery because of the paucity of information provided by many authors. None of the studies in our meta-analysis reported any vascular complications and none of them used patient-based outcome measures like Oswestry disability index, SF-36 or SF-12 scores.
Limitations
These results must be interpreted with caution as there were various potential sources of heterogeneity. Insertion of pedicle screws are complex interventions and it is difficult to avoid bias in comparison groups. Our a priori hypothesis for heterogeneity included diverse nature of studies, different indications for surgery and varying complexity of surgery as well as different levels of spine. Randomised controlled trials provide the strongest evidence for meta-analysis. Our study had only 2 RCT’s and the rest were controlled trials, some of which were retrospective. Inherent biases and confounding factors in non-RCT studies sometimes are unavoidable. Meta-analysis and systematic reviews are not without its flaws, but it is not our intention to discuss them here. For a review of the criticisms, the reader is directed to papers by Greenland [35, 36].
Conclusion
Does computer navigation provide better clinical outcome than conventional techniques? We did not find any statistically significant difference in the available clinical outcomes between two techniques. Current evidence does not favour computer-assisted navigation over conventional techniques.
In this context it is useful to remember that ‘absence of evidence is not evidence of absence’ [37]. Further research in this area should include randomised controlled trials with well-planned methodology to limit bias and report on validated patient-based outcome measures.
References
Gertzbein SD, Robbins SE (1990) Accuracy of pedicular screw placement in vivo. Spine 15:11–14
Castro WH, Halm H, Jerosch J, Malms J, Steinbeck J, Blasius S (1996) Accuracy of pedicle screw placement in lumbar vertebrae. Spine 21:1320–1324
Laine T, Makitalo K, Schlenzka D, Tallroth K, Poussa M, Alho A (1997) Accuracy of pedicle screw insertion: a prospective CT study in 30 low back patients. Eur Spine J 6:402–405
Holly LT, Foley KT (2007) Image guidance in spine surgery. Orthop Clin North Am 38:451–461 (abstract viii)
Youkilis AS, Quint DJ, McGillicuddy JE, Papadopoulos SM (2001) Stereotactic navigation for placement of pedicle screws in the thoracic spine. Neurosurgery 48:771–778 (discussion 778–779)
Richter M, Amiot LP, Neller S, Kluger P, Puhl W (2000) Computer-assisted surgery in posterior instrumentation of the cervical spine: an in vitro feasibility study. Eur Spine J 9:S65–S70
Kosmopoulos V, Schizas C (2007) Pedicle screw placement accuracy: a meta-analysis. Spine 32:E111–E120. doi:10.1097/01.brs.0000254048.79024.8b
Laine T, Schlenzka D, Makitalo K, Tallroth K, Nolte LP, Visarius H (1997) Improved accuracy of pedicle screw insertion with computer-assisted surgery. A prospective clinical trial of 30 patients. Spine 22:1254–1258
Schwarzenbach O, Berlemann U, Jost B, Visarius H, Arm E, Langlotz F, Nolte LP, Ozdoba C (1997) Accuracy of computer-assisted pedicle screw placement. An in vivo computed tomography analysis. Spine 22:452–458
Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF (1999) Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Quality of reporting of meta-analyses. Lancet 354:1896–1900
Downs SH, Black N (1998) The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 52:377–384
Bostelmann R, Benini A (2004) Computer-assisted surgery (CAS) in transpedicular lumbar fusion. Experiences of the Spinal Neurosurgery Department. Schweiz Rundsch Med Prax 93:96–102
Amiot LP, Lang K, Putzier M, Zippel H, Labelle H (2000) Comparative results between conventional and computer-assisted pedicle screw installation in the thoracic, lumbar, and sacral spine. Spine 25:606–614
Girardi FP, Cammisa FP Jr, Sandhu HS, Alvarez L (1999) The placement of lumbar pedicle screws using computerised stereotactic guidance. J Bone Jt Surg Br 81:825–829
Schnake KJ, Konig B, Berth U, Schroeder RJ, Kandziora F, Stockle U, Raschke M, Haas NP (2004) Accuracy of CT-based navigation of pedicle screws in the thoracic spine compared with conventional technique. Unfallchirurg 107:104–112. doi:10.1007/s00113-003-0720-8
Seichi A, Takeshita K, Nakajima S, Akune T, Kawaguchi H, Nakamura K (2005) Revision cervical spine surgery using transarticular or pedicle screws under a computer-assisted image-guidance system. J Orthop Sci 10:385–390. doi:10.1007/s00776-005-0902-z
Rajasekaran S, Perumal Ramesh SV, Shetty AP (2007) Randomized clinical study to compare the accuracy of navigated and non-navigated thoracic pedicle screws in deformity correction surgeries. Spine 32:E56–E64
Seller K, Wild A, Urselmann L, Krauspe R (2005) Prospective screw misplacement analysis after conventional and navigated pedicle screw implantation. Biomed Tech (Berl) 50:287–292
Kotani Y, Abumi K, Ito M, Minami A (2003) Improved accuracy of computer-assisted cervical pedicle screw insertion. J Neurosurg 99:257–263
Merloz P, Troccaz J, Vouaillat H, Vasile C, Tonetti J, Eid A, Plaweski S (2007) Fluoroscopy-based navigation system in spine surgery. Proc Inst Mech Eng [H] 221:813–820
Ito H, Neo M, Yoshida M, Fujibayashi S, Yoshitomi H, Nakamura T (2007) Efficacy of computer-assisted pedicle screw insertion for cervical instability in RA patients. Rheumatol Int 27:567–574. doi:10.1007/s00296-006-0256-7
Schlenzka D, Laine T, Lund T (2000) Computer-assisted spine surgery. Eur Spine J 9(Suppl 1):S57–S64
Merloz P, Tonetti J, Pittet L, Coulomb M, Lavallee S, Troccaz J, Cinquin P, Sautot P (1998) Computer-assisted spine surgery. Comput Aided Surg 3:297–305. doi:10.1002/(SICI)1097-0150(1998)3:6<297:AID-IGS3>3.0.CO;2-8
Richter M, Mattes T, Cakir B (2004) Computer-assisted posterior instrumentation of the cervical and cervico-thoracic spine. Eur Spine J 13:50–59. doi:10.1007/s00586-003-0604-1
Rampersaud YR, Pik JH, Salonen D, Farooq S (2005) Clinical accuracy of fluoroscopic computer-assisted pedicle screw fixation: a CT analysis. Spine 30:E183–E190
Richter M, Cakir B, Schmidt R (2005) Cervical pedicle screws: conventional versus computer-assisted placement of cannulated screws. Spine 30:2280–2287
Kamimura M, Ebara S, Itoh H, Tateiwa Y, Kinoshita T, Takaoka K (1999) Accurate pedicle screw insertion under the control of a computer-assisted image guiding system: laboratory test and clinical study. J Orthop Sci 4:197–206
Laine T, Lund T, Ylikoski M, Lohikoski J, Schlenzka D (2000) Accuracy of pedicle screw insertion with and without computer assistance: a randomised controlled clinical study in 100 consecutive patients. Eur Spine J 9:235–240
Kotani Y, Abumi K, Ito M, Takahata M, Sudo H, Ohshima S, Minami A (2007) Accuracy analysis of pedicle screw placement in posterior scoliosis surgery: comparison between conventional fluoroscopic and computer-assisted technique. Spine 32:1543–1550. doi:10.1097/BRS.0b013e318068661e
Lee GY, Massicotte EM, Rampersaud YR (2007) Clinical accuracy of cervicothoracic pedicle screw placement: a comparison of the “open” lamino-foraminotomy and computer-assisted techniques. J Spinal Disord Tech 20:25–32. doi:10.1097/01.bsd.0000211239.21835.ad
Roy-Camille R, Saillant G, Mazel C (1986) Internal fixation of the lumbar spine with pedicle screw plating. Clin Orthop Relat Res, pp 7–17
Ludwig SC, Kramer DL, Vaccaro AR, Albert TJ (1999) Transpedicle screw fixation of the cervical spine. Clin Orthop Relat Res, pp 77–88
Ferguson RL, Tencer AF, Woodard P, Allen BL Jr (1988) Biomechanical comparisons of spinal fracture models and the stabilizing effects of posterior instrumentations. Spine 13:453–460
Schulze CJ, Munzinger E, Weber U (1998) Clinical relevance of accuracy of pedicle screw placement. A computed tomographic-supported analysis. Spine 23:2215–2220 (discussion 2220–2211)
Greenland S (1994) Can meta-analysis be salvaged? Am J Epidemiol 140:783–787
Greenland S (1994) Invited commentary: a critical look at some popular meta-analytic methods. Am J Epidemiol 140:290–296
Altman DG, Bland JM (1995) Absence of evidence is not evidence of absence. BMJ 311:485
Arand M, Hartwig E, Hebold D, Kinz L, Gebhard F (2007) Precision analysis of naviagation assisted implanted thoracic and lumbar pedicled screws. A prospective clinical study. Unfallchirurg 104(11):1076–1081
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Verma, R., Krishan, S., Haendlmayer, K. et al. Functional outcome of computer-assisted spinal pedicle screw placement: a systematic review and meta-analysis of 23 studies including 5,992 pedicle screws. Eur Spine J 19, 370–375 (2010). https://doi.org/10.1007/s00586-009-1258-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-009-1258-4