Abstract
Intraoperative MRI (iMRI) allows a more detailed appreciation of the extent of resection than does conventional neurosurgery and results in longer overall survival in patients with malignant glioma. However, it is unknown whether the intraoperative application of contrast agent influences the early postsurgical MRI. The preceding iMRI could alter the signals of MR sequences in the early postsurgical MRI, especially in sequences influenced by T1 contrast. Hereby, we investigate such iMRI-induced influences on the fluid-attenuated inversion recovery (FLAIR) sequence. We retrospectively analyzed postsurgical T2w, T1w, and FLAIR images by visual inspection and by signal measurements in 46 patients with malignant gliomas after tumor resection. Of these, n = 25 patients were operated with conventional microsurgery, and n = 21 patients were operated with contrast-enhanced iMRI-guided microsurgery. We measured signal intensity in the resection cavity, in the cerebrospinal fluid (CSF) of the ventricles, and in the normal brain tissue contralateral to the tumor-bearing hemisphere on axial FLAIR images and T1-weighted and T2-weighted images. In 18 patients, the FLAIR sequence revealed hyperintense signal changes of the CSF in the subarachnoid or ventricular spaces. Seventeen of these 18 patients had received intraoperative MRI. In both FLAIR and T1-weighted images, the signal of the CSF in the ventricles was significantly higher in patients with iMRI than in patients without iMRI. The intraoperative application of contrast agent that is used for iMRI significantly influences postsurgical MRI within the first 72 h. We found hyperintense signal changes of the CSF in the FLAIR sequence in the subarachnoid and intraventricular spaces mimicking subarachnoid hemorrhage. The findings may result in a misdiagnosis of subarachnoid hemorrhage (SAH) in these patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The extent of tumor resection seems to be a predictor for progression-free and overall survival time of patients with high-grade gliomas [25, 26]. Intraoperative MRI (iMRI) allows a more detailed appreciation of the extent of resection than does conventional neurosurgery [22, 23]. IMRI detects residual tumor as an enhancing area after intravenous application of contrast agent and enables immediate further tumor resection. As a result, iMRI is often used in glioma surgery. Many institutions also perform an early MRI within the first 72 h after surgery to determine the extent of tumor resection, irrespective of whether iMRI was used during surgery or not.
To date, no study has analyzed whether the intraoperative application of contrast agent influences the early postsurgical MRI. In the absence of blood–brain barrier (BBB) damage, contrast agent should pass through the cerebral vessels without accumulating in the brain tissue. However, brain tumors themselves and also neurosurgical procedures alter the BBB, causing intracerebral contrast enhancement [8]. Therefore, also the contrast agent administration during preceding iMRI should influence the signals of MR sequences in the early postsurgical MRI, especially in sequences which are influenced by T1 contrast such as T1-weighted sequences and fluid-attenuated inversion recovery (FLAIR). Cerebrospinal fluid (CSF) signal changes in FLAIR imaging after intravenous injection of gadolinium-containing contrast agent have been reported in pathological conditions causing blood–brain barrier disruption or neovascularization [3, 5].
We suggest that also the intraoperative application of contrast agent might influence the signal on FLAIR sequences. To investigate this hypothesis, we retrospectively performed a blinded analysis of postsurgical MR images of patients with malignant brain tumors with and without iMRI-guided surgery.
Methods
The study was approved by the local ethics committee.
We retrospectively analyzed postsurgical MRIs in 46 patients (33/13 male/female, mean age 62.5 years, range 26 to 79 years) with malignant gliomas after tumor resection during an observation period from January 2012 to June 2013. Complete or near-complete surgical resection of the enhancing tumor was intended in all patients.
A subgroup (no-iMRI, n = 25) underwent conventional microsurgery, and a subgroup (iMRI, n = 21) underwent microsurgery guided by contrast-enhanced iMRI with a mobile intraoperative ultra-low-field MRI system (PoleStar N-20, Odin Medical Technologies, Yokneam, Israel and Medtronic, Louisville, CO, USA) after intravenous application of a gadolinium (Gd)-based contrast agent (Gadovist 1.0 mmol/ml, dose 0.1 ml/kg); usually, the contrast agent was applied twice—before starting surgery and for the intraoperative post-resection scan.
All patients underwent contrast-enhanced high-field MRT at 3.0 T (Verio; Siemens, Erlangen, Germany) within 7 days before surgery and within 72 h after surgery using a standard protocol including axial T2-weighted turbo-spin echo sequence (repetition time (TR) = 5.170 ms; echo time (TE) = 92 ms), axial FLAIR sequence (TR = 6.630 ms, TE = 131 ms, TI = 2.140 ms), and T2*-weighted images (TR = 631 ms; TE = 19.9 ms). Axial T1-weighted spin echo sequences (TR = 590 ms, TE = 12 ms) were performed before and after intravenous application of a standard dose of Gd-DTPA (0.1 mmol/kg). Further, coronal and sagittal contrast-enhanced T1-weighted gradient echo sequences were added. In all patients, the FLAIR sequence was performed before intravenous gadolinium injection.
MR signal analysis
One radiologist (with more than 5 years of experience in brain imaging) and one student (instructed and supervised by a neuroradiologist with more than 12 years of experience) independently analyzed the FLAIR sequences by visual inspection. Both observers were blinded for the surgical procedure. Further signal measurements were also done on T1- and T2-weighted images before contrast administration.
-
1.
The visual inspection evaluated the presence of abnormal FLAIR CSF signal considering the location of signal changes (subarachnoid space (SAS) ipsilateral close to the lesion, bilateral SAS, ventricular). In all patients, we also inspected the presurgical FLAIR sequences to exclude preexisting signal changes.
-
2.
The MRI signal intensity was measured in regions of interest (ROI) consensually placed by the two observers in the resection cavity, in the CSF of the ventricles, and in the normal brain tissue contralateral to the tumor-bearing hemisphere on axial FLAIR images and T1-weighted and T2-weighted images. The results of these measurements were compared between the two groups: iMRI versus no-iMRI.
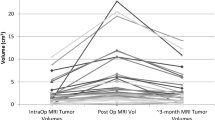
Further, the volumes of the lesions were delineated semi-automatically on the tumor volume on the preoperative contrast-enhanced T1-weighted images.
Statistical analysis
Statistical analysis was performed with R-Statistics 2.15.1 for Windows. We compared signal intensities on FLAIR images, T1-weighted images, and T2-weighted images between patients with iMRI surgery versus patients without iMRI with the Mann–Whitney U test, and we used the correlation between T1 and FLAIR signals with Spearman’s rho correlation coefficient. We used a significance level of p < 0.05.
Spearman’s rho correlation coefficient was also used to test if the signal intensities are influenced by the timing of the postoperative MRI.
Results
Patients
Histopathologically, 44 of the 46 patients had glioblastoma, one patient had a WHO grade III astrocytoma and one patient had gliosarcoma.
Patients who had iMRI (n = 21) had longer surgical time with a median of 54 min compared to patients without (no-iMRI, n = 25) iMRI guidance. There was no difference in the preparation of the surgical site between the patients with iMRI and without iMRI guidance.
Postsurgical MRI (with a standard protocol) was performed within 72 h after surgery in 41 of the 46 patients with an average of 32:29 h for the iMRI group and 33:04 h for the no-iMRI group. The remaining five patients (two from the iMRI group and three from the no-iMRI group) were imaged beyond the “72-h window” with an average of 86:50 h and a range from 73:46 to 107:33 h. There was no significant difference between the groups concerning the timing of the MRI scan after surgery.
Visual inspection of FLAIR signal
In 18 patients, the FLAIR sequence revealed hyperintense signal changes of the CSF in the subarachnoid spaces (Fig. 1) and/or ventricular spaces (Fig. 2). Of these, 17 patients had received intraoperative MRI and only one did not.
Postsurgical MRI after tumor resection with iMRI: Axial T2*-weighted image (a), T2-weighted image (b), T1-weighted image (c), and FLAIR (d) of postsurgical MRI ∼30:00 h after resection of a glioblastoma in the right temporal lobe. Patient had received intravenous contrast media before to control the extent of resection with iMRI. FLAIR sequence revealed untypical hyperintense signal changes of the CSF in the subarachnoid spaces and ventricles yielding very atypical T2-like appearance of the FLAIR (d). Hyperintense FLAIR signal of CSF may also appear in acute SAH, but signal of the T1-weighted image still appears normal (see Fig. 2)
Postsurgical MRI in another patient after resection of a glioblastoma in the right temporal lobe with iMRI: Since postsurgical MRI was suggestive for SAH, patient underwent cranial computed tomography (a) immediately thereafter, showing no abnormality suggestive of SAH. CSF was normal on T2-weighted image (b), while FLAIR (c) showed impressive signal increase of the CSF, suggesting that erroneously another T2-weighted image has sneaked in instead of the FLAIR, but this was not the case. Compared to Fig. 1, the shortening of T1 relaxation time upon preceding intraoperative contrast application was more pronounced yielding abnormal contrast in T1-weighted image before postsurgical contrast application (d), while contrast-enhanced T1-weighted image (e) only shows additional enhancement on the choroid plexus
In the 17 patients with iMRI and hyperintense CSF signal, the interval between brain surgery and postsurgical MRI was 32.04 h (median, range from 24.25 to 80.31 h). One patient with CSF signal changes underwent cranial computed tomography (CCT) immediately after the postsurgical MRI to exclude the presence of subarachnoid hemorrhage (SAH) (Fig. 2). This CCT did not reveal any abnormality suggestive of hemorrhage in the SAS. No patient had suggestive symptoms (headache, meningism) or worsening of clinical status. Therefore, lumbar puncture for CSF diagnostic was not performed in any patient.
In the patient without iMRI and hyperintense CSF signal, postsurgical MRI was performed 51.25 h after surgery. This one patient (with abnormal CSF signal in the absence of iMRI) had alterations of the ipsilateral SAS and in the resection cavity as well as susceptibility changes on T2* imaging and was therefore prescribed a CCT immediately after the postsurgical MRI to exclude SAH. The CCT of this patient, performed immediately after the postsurgical MRI, revealed no hemorrhage in the SAS.
The hyperintense CSF changes were more evident close to the resection cavity and/or in the hemisphere involved by the pathology. Their location was close to the lesion in seven cases, hemispheric in four cases, or ventricular in six cases.
In the patients with hyperintense FLAIR changes, the T1-weighted sequence revealed hyperintense signal changes of the CSF (n = 8), in the resection cavity (n = 3), in the subarachnoid spaces (n = 2), and in the ventricular spaces (n = 3), but the hyperintense signal changes were less intense on the T1-weighted images compared to the FLAIR images.
Susceptibilities in the SAS or ventricles suggesting hemorrhage were not present on T2* images in any patient with iMRI guidance.
Signal measurements
On FLAIR, the CSF signal intensity in the ventricles was significantly higher in patients with iMRI than in patients without iMRI (p < 0.01), but the signal increase was not significant in the resection cavity (p = 0.25) (Table 1 and Fig. 3).
Signal intensities on axial T1-weighted, T2-weighted, and FLAIR images. Comparison of patients with conventional microneurosurgery (no-iMRI) versus patients with iMRI using Mann–Whitney U test. The signal intensities were measured in regions of interest placed in the CSF of the ventricles, in the resection cavity, and in the contralateral brain tissue, respectively. Significance level was p < 0.05
On the T1-weighted sequence, the signal of the CSF in the ventricles was higher in patients with iMRI but without reaching the significance level (p = 0.08). The signal in the resection cavity was not significantly different between the groups on T1-weighted images either.
On T2-weighted images, there was no difference between the signal intensities of patients with and without iMRI.
The patients who had the highest signal intensities of the CSF measured on FLAIR sequence also had the highest values on T1-weighted images (Fig. 4). In the CSF of patients with iMRI, the signal intensity values of the T1-weighted images correlated significantly with the signal values of the FLAIR sequences, with Spearman’s rho 0.65 for the CSF (p < 0.001). In contrast, no correlation was found for the CSF signals in these sequences for patients without iMRI. In both groups, there was a positive correlation between the signal values in the resection cavity between T1-weighted images and FLAIR, with rho of 0.9 for patients with iMRI and 0.7 for patients without iMRI (p < 0.001 both).
Correlation between FLAIR and T1-weighted image intensities in the CSF, in the ventricles (left), and in the resection cavity (right) for the group with conventional surgery (no-iMRI—filled circles) and the group with iMRI (iMRI—open circles). Spearman rho correlation coefficient and P values are provided in the top left corner of each plot
Further, the signal intensity correlated to the timing of the postoperative MRI.
-
1.
The earlier the postoperative MRI was performed, the higher the signal intensity was in the CSF in the FLAIR images in the iMRI group (rho = −0.43, p = 0.05). No correlation was found for the no-iMRI group.
-
2.
With increasing distance to the surgery, the signal intensity in the tumor cavity is declining on T2-weighted images but only in the no-iMRI group (rho = −0.43, p = 0.03).
Table 1 summarizes patients’ characteristics and the results of signal measurements. The preoperative tumor sizes were not significantly different between the iMRI (mean = 68.9 cm3) and the non-iMRI group (54.5 cm3) calculated with the Student’s t test (p = 0.3).
Discussion
Postsurgical MRI within the first 72 h is significantly influenced by the intraoperative application of Gd-based contrast agent which is used for iMRI. We found hyperintense signal changes of the CSF in the FLAIR sequence in the subarachnoid and intraventricular spaces mimicking extended SAH, bearing the risk to result in the misdiagnosis of SAH in these patients. But none of the patients with these SAH-like changes in FLAIR showed any clinical evidence of SAH. We therefore postulate that the T1-shortening effect of Gd-containing contrast agent—in addition to higher protein content in some cases—is responsible for the signal increase in the FLAIR sequence.
In accordance with this hypothesis, we found a strong correlation between the signal on FLAIR and T1-weighted images measured in the CSF of patients with iMRI (in whom Gd-containing contrast agent was applied intraoperatively), but not in patients without iMRI, and also not between FLAIR and T2-weighted images. CSF signal increase was higher close to the lesion and/or ipsilateral hemisphere, which might be explained by the neovascularization close to the SAS or ventricles and the blood–brain barrier breakdown in patients with glioblastoma multiforme (GBM) after surgical tumor resection resulting in leakage of gadolinium chelates into the subarachnoid space. There was also a positive correlation between signal intensities in the resection cavity between FLAIR and T1-weighted images for both groups, probably due to the presence of methemoglobin and proteins, which generally shorten the T1 relaxation time. Additional extravasation of Gd-containing molecules may explain the stronger correlation in patients with iMRI. However, in the T1-weighted images, the CSF signal differences between the groups did not reach significance level, maybe due to the stronger T1 effect of contrast agent on the FLAIR images. Further, no signal differences were observed on T2-weighted images between the patients with and without iMRI.
Animal experiments illustrated the strong sensitivity of FLAIR imaging to changes in the T1 relaxation time of CSF that became apparent even at very low gadolinium concentrations of 0.007 mmol/L [3, 12]. The FLAIR imaging technique uses an inverting pulse to null the signal of CSF as these spins pass through the zero point in their relaxation trajectory. Any shortening of the CSF T1 relaxation time would then make it appear bright with respect to the usual dark CSF [13]. The concept that contrast agent might enter the CSF after IV injection is not new. There are several previous reports of iodinated contrast material entering the SAS [4, 6, 14]. A study by Knutzon et al. of CSF samples taken from dogs after IV injection of gadolinium contrast agent showed T1 shortening effect in vitro [9]. Visualization of this effect on routine MR images has been reported in humans but usually in the setting of extensive disease of the meninges or brain like carcinomatous meningitis [3, 16, 20, 21].
Abnormal enhancement patterns have been reported in early postoperative contrast-enhanced FLAIR sequence in patients after resection of intraparenchymal lesions [3, 5, 13]. Bozzao et al. detected an increased CSF signal 3 h after application of intravenous gadolinium-containing contrast agent in patients with previous surgery and in those with high-grade gliomas abutting to the subarachnoid spaces or ventricles [3]. Dechambre et al. reported that CSF signal changes were particularly evident in patients with pathologies leading to the breakdown of the BBB or with angioneogenesis close to the subarachnoid space or ventricles [5]. Authors concluded that either neovascularization or the breakdown of the BBB results in abnormal enhancement of the subarachnoid spaces in FLAIR sequences [3, 5, 13]. “Hyperintense acute reperfusion marker” or HARM is an abnormal enhancement of the CSF on contrast-enhanced FLAIR due to CNS barrier disruption in acute cerebrovascular diseases [10, 11]. Further potential advantages of FLAIR are the sensitivity to detect acute SAH [5, 18, 19] or other pathologies leading in CSF signal changes such as meningitis [2, 24]. In those cases, findings on all the other routine MR images may be normal, including enhanced T1-weighted images.
So far, there is no report investigating the impact of contrast agent administered during iMRI on the postsurgical MRI.
Another hypothesis discussed in previous studies before is that FLAIR is sensitive to an increase of protein levels in the CSF [5, 15]. A high protein concentration decreases the T1 relaxation time of CSF and causes an offset of the null inversion time, so that CSF appears with high signal intensity. For example, brain ischemia alters the blood–brain barrier causing an increase in vascular permeability to protein resulting in an elevation of CSF protein concentration in about half of patients with stroke [1, 5, 7, 17].
High protein might have caused high CSF signal in FLAIR in the one of our patient without iMRI.
Furthermore, significantly larger tumor volume could have caused larger resection with increased spreading of protein particles in the SAS, which might be a reason for the FLAIR signal changes. However, we could exclude that tumor volume had an influence on these signal changes, since preoperative volume of the lesions in the iMRI did not significantly differ from non-iMRI group.
Bozzao et al. reported that the signal changes of the CSF returned to normal within 2 days [3]. Our study showed that the earlier the postoperative MRI was performed, the higher the signal intensity was in the CSF in the FLAIR images in the iMRI group. The patients who present CSF signal increase underwent postsurgical MRI control with a mean of 32.04 h compared to those with iMRI guidance but without visible signal changes of the CSF with a mean 46.45 h. This suggests that gadolinium diffuses in the SAS during the first hours following its intraoperative application, and thereafter, it is successively resorbed from SAS within the following 1–2 days.
Patients who had intraoperative MRI had longer surgical time with a median of 54 min compared to patients without iMRI guidance. Although we cannot exclude that longer surgical times for iMRI might have influenced FLAIR signal, there is no report supporting such a hypothesis.
Conclusion
In patients with GBM and intraoperative MRI guidance, FLAIR hyperintensity in CSF is likely in postoperative MRI. The signal changes are explained by gadolinium leakage due to the blood–brain barrier breakdown from surgical manipulation and tumor neovascularization.
One should be aware of this phenomenon to avoid the misdiagnosis of subarachnoid hemorrhage in postsurgical MRI.
References
Al-Kassab S, Skyhøj Olsen T, Skriver EB (1981) Blood–brain barrier integrity in patients with cerebral infarction investigated by computed tomography and serum-CSF-albumin. Acta Neurol Scand 64(6):438–445
Bozzao A, Bastianello S, Bozzao L (1997) Superior sagittal sinus thrombosis with high-signal-intensity CSF mimicking subarachnoid hemorrhage on MR FLAIR images. Am J Roentgenol 169(4):1183–1184
Bozzao A, Floris R, Fasoli F, Fantozzi LM, Colonnese C, Simonetti G (2003) Cerebrospinal fluid changes after intravenous injection of gadolinium chelate: assessment by FLAIR MR imaging. Eur Radiol 13(3):592–597
Coin CG, Keranen VJ, Pennink M, Ahmad WD (1979) Evidence of CSF enhancement in the spinal subarachnoid space after intravenous contrast medium administration: is intravenous computer assisted myelography possible? J Comput Assist Tomogr 3:267–269
Dechambre SD, Duprez T, Grandin CB, Lecouvet FE, Peeters A, Cosnard G (2000) High signal in cerebrospinal fluid mimicking subarachnoid haemorrhage on FLAIR following acute stroke and intravenous contrast medium. Neuroradiology 42:608–661
Harnish PP, Northington FK, Samuel KA (1988) Diatrizoate levels in cerebrospinal fluid following intravenous administration: role of fluid production rate. Invest Radiol 23:377–380
Hornig CR, Busse O, Dorndorf W, Kaps M (1983) Changes in CSF blood–brain barrier parameters in ischaemic cerebral infarction. J Neurol 229(1):11–16
Knauth M, Wirtz CR, Tronnier VM, Staubert A, Kunze S, Sartor K (1998) Intraoperative magnetic resonance tomography for control of extent of neurosurgical operations. Radiologe 38(3):218–224
Knutzon RK, Poirier VC, Gerscovich EO, Brock JM, Buonocore M (1991) The effect of intravenous gadolinium on the magnetic resonance appearance of cerebrospinal fluid. Invest Radiol 26:671–673
Köhrmann M, Struffert T, Frenzel T, Schwab S, Doerfler A (2012) The hyperintense acute reperfusion marker on fluid-attenuated inversion recovery magnetic resonance imaging is caused by gadolinium in the cerebrospinal fluid. Stroke 43(1):259–261
Latour LL, Kang DW, Ezzeddine MA, Chalela JA, Warach S (2004) Early blood–brain barrier disruption in human focal brain ischemia. Ann Neurol 56:468–477
Luzzani F, Cipolla P, Pélaprat ML, Robert F, Gotti C, Tirone P, de Haën C (1997) Brain penetration and neurological effects of gadobenate dimeglumine in the rat. Acta Radiol 38(2):268–272
Mamourian AC, Hoopes PJ, Lewis LD (2000) Visualization of intravenously administered contrast material in the CSF on fluid-attenuated inversionrecovery MR images: an in vitro and animal-model investigation. Am J Neuroradiol 21:105–111
McClennan BL, Becker JA (1971) Cerebrospinal fluid transfer of contrast material at urography. Am J Roentgenol 113:427–432
Melhem ER, Jara H, Eustace S (1997) Fluid-attenuated inversion recovery MR imaging: identification of protein concentration thresholds for CSF hyperintensity. Am J Roentgenol 169(3):859–862
Naul LG, Finkenstaedt M (1997) Extensive cerebrospinal fluid enhancement with gadopentetate dimeglumine in a primitive neuroectodermal tumor. Am J Neuroradiol 18:1709–1711
Niebrój-Dobosz I, Mariam AG, Lukasiuk M, Rafałowska J (1992) Blood-cerebrospinal fluid barrier integrity in cerebral infarction. Neuropatol Pol 30(1):29–33
Noguchi K, Ogawa T, Inugami A, Toyoshima H, Sugawara S, Hatazawa J, Fujita H, Shimosegawa E, Kanno I, Okudera T et al (1995) Acute subarachnoid hemorrhage: MR imaging with fluid-attenuated inversion recovery pulse sequences. Radiology 196(3):773–777
Noguchi K, Ogawa T, Seto H, Inugami A, Hadeishi H, Fujita H, Hatazawa J, Shimosegawa E, Okudera T, Uemura K (1997) Subacute and chronic subarachnoid hemorrhage: diagnosis with fluid-attenuated inversion-recovery MR imaging. Radiology 203(1):257–262
Pui MHW, Langston JW, Arai Y (1993) Gd-DTPA enhancement of CSF in meningeal carcinomatosis. J Comput Assist Tomogr 17:940–944
Sakamoto S, Kitagaki H, Ishii K, Yamaji S, Ikejiri Mori E (1997) Gadolinium enhancement of the cerebrospinal fluid in a patient with meningeal fibrosis and cryptococcal infection. Neuroradiology 39:504–505
Senft C, Bink A, Franz K, Vatter H, Gasser T, Seifert V (2011) Intraoperative MRI guidance and extent of resection in glioma surgery: a randomised, controlled trial. Lancet Oncol 12(11):997–1003
Senft C, Franz K, Blasel S (2010) Influence of iMRI-guidance on the extent of resection and survival of patients with glioblastoma multiforme. Technol Cancer Res Treat 9(4):339–346
Singer MB, Atlas SW, Drayer BP (1998) Subarachnoid space disease: diagnosis with fluid-attenuated inversion recovery MR imaging and comparison with gadolinium-enhanced spin-echo MR imaging: blinded reader study. Radiology 208:417–422
Schneider JP, Trantakis C, Rubach M et al (2005) Intraoperative MRI to guide the resection of primary supratentorial glioblastoma multiforme—a quantitative radiological analysis. Neuroradiology 47:489–500
Wirtz CR, Knauth M, Staubert A et al (2000) Clinical evaluation and follow-up results for intraoperative magnetic resonance imaging in neurosurgery. Neurosurgery 46:1112–1122
Conflict of interest
CS has received honoraria as an invited speaker from Medtronic Navigation.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Hussam Metwali, Hannover, Germany
The authors reported about artifacts in the postoperative MRI in the patients who were operated with iMRI for resection of cranial gliomas. These patients received contrast material during the intraoperative MRI. This artifact was mainly in the FLAIR sequence. This could be interpreted as SAH-mimic finding. Accordingly, they described this artifact as a misleading pattern. According to the authors, the reason for these signals in the FLAIR sequence, which could mimic a SAH, is the effect of the contrast material in the presence of defective blood–brain barrier.
In order to test this hypothesis, two groups of patients were analyzed. The first group contains the patients who were operated under iMRI control and received contrast material (Gd-based). The second group includes the patients who were operated on without iMRI. They compared the early postoperative MRI and found that there is a significant difference in the signals and the visual pattern of the FLAIR sequence between both groups. There were no significant differences in T1 and T2 sequences between both groups.
It could be an interesting physical finding, but the clinical value could be questionable. The evaluation of the postoperative MRI is based not only on the FLAIR sequence. The inspector evaluates usually all the sequences of the MRI. Signal change of the CSF after surgery is not a rare postoperative finding, not only due to the effect of the contrast material but also due to the changes in the CSF composition after surgery especially the protein and the cellular content. The subarachnoid hemorrhage is not a common event after glioma surgery unless it is a part of postoperative bleeding in the tumor bed.
If the neurosurgeon considers the clinical state of the patient as well as the other sequences of the MRI, I think the surgeon can differentiate between an artifact and a clinically significant change. In my practice, I did not encounter this dilemma of a misleading FLAIR, till now.
Arya Nabavi, Hannover, Germany
In this article, Misleading FLAIR imaging pattern after glioma surgery with intraoperative MRI, Lescher et al. describe their experience with 46 patients, of which 21 were operated on with the addition of intraoperative imaging. They describe that signal changes in FLAIR after intraoperative contrast application (2× normal dosage) can be misinterpreted as subarachnoid hemorrhage. Taking T2* into account allows the differentiation. They conclude that “intraoperative application of contrast medium significantly influences postsurgical MRI within the first 72 h.”
Reading postoperative images is always a challenge. Changes have to be evaluated by crosschecking effects in different sequences to determine their validity. The authors point to the fact that FLAIR may be misinterpreted, if looked at in a “standalone” fashion. Once pieces of image information from various sequences are combined (i.e., in this case FLAIR and T2*), similar to combining information to determine the cytotoxic or vasogenic nature of signal changes, a serious complication can be ruled out easily. Postoperative imaging is still most often done with 1.5 T units, simply due to its availability. It is questionable if the FLAIR effect described in this article will be as pronounced in that field strength. However, with development to higher fields, we will most likely encounter the described phenomenon and also many more. This issue can be addressed with due diligence and knowledge of MRI sequences.
Another important issue to be reckoned with is field strength. It is common practice in the neurosurgical literature to refer to “intra-” or “postoperative” MRI, as if the method is interchangeable, as long as it is MRI. Since field strength has a major influence, among other aspects, on quality and sensitivity, this represents a major caveat. It is not certain that effects, described for one field strength, will display the same way in another. Usually, there are gradual differences. However, depending on the susceptibility of the sequence, this may differ widely.
The group has to be commended for a very thorough analysis of their data and for raising the awareness of potential “pathologies” following new procedures. Particularly, higher field MRI (3 T) will pick up changes, which ordinarily may not appear on 1.5 T. Residual tumor or “unknown bright objects” may be seen postoperatively, obscuring a definite image-reading. But even more so, it is a reminder to us that with changing technologies, heightened awareness for their specific capacities and weaknesses has to be promoted. MRI does not equal MRI. The sophistication of this imaging technology makes it imperative for us to not just evaluate the images but also look at the information they can provide us with and their potential pitfalls.
Constantin Roder, Tübingen, Germany
Dr. Lescher and co-workers have analyzed specific changes in postoperative MRI after the intraoperative application of gadolinium in iMRI-guided surgery. While a directly postoperatively appearing significant SAH would be a very unusual coincidence of different pathologies, it might nevertheless be important to be aware of such changes to prevent from uncertainty when analyzing the images.
Since iMRI has been used for many years, it now appears to be of an increasing importance to focus more on specific details caused by this technology and to start developing new approaches to broaden possible indications of iMRI.
Rights and permissions
About this article
Cite this article
Lescher, S., Jurcoane, A., Schniewindt, S. et al. Misleading FLAIR imaging pattern after glioma surgery with intraoperative MRI. Neurosurg Rev 39, 79–86 (2016). https://doi.org/10.1007/s10143-015-0653-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-015-0653-z