Abstract
Cholecystectomy is the most performed intra-abdominal surgical procedure in the US, with 1.2 million performed annually, and is predominantly performed laparoscopically. Although largely safe, laparoscopic cholecystectomy results in higher rates of abdominal symptoms consisting of abdominal pain and dyspepsia, which may persist or recur, collectively known as post-cholecystectomy syndrome. This article aims to (1) provide an overview of post-cholecystectomy syndrome with an emphasis on biliary complications and emergent imaging findings, (2) illustrate the spectrum of imaging findings of early and late post-cholecystectomy complications, (3) enumerate the role of various imaging modalities in evaluating post-cholecystectomy complications and address the role of selective trans-catheter coil embolization in managing bile leaks, and (4) discuss pearls and pitfalls in imaging following cholecystectomy. While common first-line imaging modalities for post-cholecystectomy complications include CT and sonography, ERCP and MRCP can delineate the biliary tree with greater detail. Scintigraphy has a higher sensitivity and specificity than CT or sonography for diagnosing bile leak and may preclude the need for ERCP. Post-operative complications include biliary duct injury or leak, biliary obstruction, remnant gallbladder/cystic duct stones and inflammation, biliary dyskinesia, papillary stenosis, and vascular injury. Subtle cases resulting in lethal outcomes, such as hemorrhage from the gallbladder bed without major vessel injury, have also been described. Cases presented will include biliary complications such as post-cholecystectomy stump cholecystitis, nonbiliary complications such as subcapsular hematoma, and normal post-surgical findings such as oxidized regenerated cellulose. Post-operative biliary complications can cause significant morbidity and mortality, and thus familiarity with the expected post-surgical appearance of the gallbladder fossa and biliary tract, as well as understanding the spectrum of complications and associated multimodality imaging findings, are essential for emergency radiologists and those practicing in the acute care setting to direct appropriate patient management. Furthermore, many of the postoperative complications can be managed by noninvasive percutaneous interventional procedures, from drain placement to cystic artery and cystic duct stump embolization.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cholecystectomy is the surgical removal of the gallbladder and has become the mainstay for treating various gallbladder pathologies, including common acute cholecystitis and rare gallbladder carcinoma. It has become one of the most common surgeries in the USA, with 1.2 million cases performed annually [1]. The first open cholecystectomy was described in 1882 by Dr. Carl Langbuch, and later the much less invasive laparoscopic cholecystectomy was first performed by Dr. Med Erich Mühe in 1985 [2]. Laparoscopic surgery became widely adopted over open technique for two main reasons: shorter hospital stays and faster patient recovery to baseline [3].
During a routine cholecystectomy, the gallbladder is dissected away from the liver and removed after double clipping both the cystic duct and cystic artery [4]. However, to achieve surgical success, correctly identifying the biliary anatomy preoperatively and intraoperatively is critical to avoid surgical complications. With only 50–60% of patients having classic biliary anatomy, the risk for iatrogenic injury is not insignificant [5]. Variants such as an aberrant right posterior hepatic duct or long parallel cystic duct are not uncommon, may contribute to biliary injury, and should be considered in patients with biliary leaks [6, 7]. However, cholecystectomies are often performed without prior knowledge of biliary anatomy. If an endoscopic retrograde cholangiopancreaticography (ERCP) or magnetic resonance cholangiopancreaticography (MRCP) is performed pre-operatively, for evaluation of choledocholithiasis or when the diagnosis of cholecystitis is equivocal, reporting anatomic variation is crucial for the surgeon to avoid biliary injury. Unfortunately, approximately 10% of patients undergoing cholecystectomy experience persistent symptoms from gallbladder pathology, including right upper quadrant pain and dyspepsia, known collectively as a post-cholecystectomy syndrome (PCS). These complications may be classified as early, typically in the immediate post-operative period, and late [8].
Imaging plays a crucial role in patients with PCS as it can impact management. The purpose of this article is to review the expected postsurgical appearances after open and laparoscopic cholecystectomy and to illustrate the imaging appearance of biliary, vascular, infectious, and iatrogenic surgical complications on different imaging modalities.
Normal postsurgical appearance after cholecystectomy and pitfalls on imaging
The normal imaging appearance of the post-cholecystectomy state is important to recognize to avoid patient harm and prevent additional unnecessary interventions. Common postsurgical findings include trace pneumoperitoneum, fluid within the gallbladder fossa or surgical bed, and biliary ductal dilation.
Depending on the open versus laparoscopic technique, a trace amount of pneumoperitoneum may be present shortly after surgery; it is typically more common in patients undergoing open cholecystectomy. With laparoscopic approaches, air insufflation of the abdomen with carbon dioxide gas is quickly absorbed through the peritoneal lining [9]. Small volume pneumoperitoneum should not raise suspicion for a hollow viscus perforation, especially in the immediate postoperative period of open cholecystectomy.
A small amount of free fluid in the gallbladder fossa may be a normal finding within the first week after surgery. Seroma, a collection of serous fluid, is common after surgical intervention and may appear as organized usually low attenuation fluid (Fig. 1a and b) on CT imaging. It should be differentiated from a pathologic fluid collection such as a hematoma, biloma, or postoperative abscess [10]. Hematomas can be identified as a complex fluid collection with no discernible surrounding wall. On US, the echogenicity of a hematoma depends on the age of the fluid collection while on CT, hematomas show characteristic hyper-attenuation (Fig. 1c and d) and do not enhance with contrast. Alternatively, an abscess demonstrates a discrete wall that shows enhancement with contrast administration (Fig. 2a and b). Abscess formation can occur as a complication secondary to surgical intervention or secondary to infection of a pre-existing hematoma. A common mimicker of infected hematoma/abscess is an intraoperative hemostatic agent, such as oxidized regenerated cellulose. Classically, this will appear as an air and fluid structure on CT, measuring 40–55 HU, and may prompt a radiologist to raise the concern for a hematoma or abscess (Fig. 2c and d) [11, 12]. A similar dilemma can occur even in sonography, where hemostatic agents can be identified as an echogenic structure with posterior reverberation artifact [10].
Post-cholecystectomy fluid collections in two different patients. Seroma. a NECT axial images show a hypodense fluid collection close to the post-cholecystectomy surgical clips (arrow) on postoperative day 7. b HIDA scan performed subsequently demonstrates no leak of radiopharmaceutical mitigating bile duct injury. Hematoma. c CECT axial image in a different patient on a postoperative day 5 demonstrates hyperdense fluid collection accumulating adjacent to the post-cholecystectomy site (arrow) and encroaching along the falciform ligament and perihepatic region (arrowheads). HIDA scan was performed as the bilirubin was minimally elevated. d Delayed HIDA scan images reveal normal excretion of radiopharmaceutical into the bowel without leak
Abscess vs. oxidized regenerated cellulose. Abscess. a Axial CECT image in a patient with abdominal pain 12 days after cholecystectomy shows a rim-enhancing complex mixed air-fluid collection emanating from the surgical bed (arrow). b Coronal CECT image demonstrates inflammatory stranding (arrow) along the subhepatic region and also inflammatory bowel wall thickening of the duodenum (arrowhead). c Axial CECT images post cholecystectomy day 5 in a different patient show mixed attenuation material in the gallbladder fossa, consistent with oxidized regenerated cellulose (arrow). d Coronal CECT image shows subtle minimal inflammation (arrow) in the subhepatic region when compared to the abscess (image b). Hemostatic material can mimic an abscess and lead to unnecessary procedures. Resorption time is usually 7–14 days
In the postoperative state, the common bile duct and intrahepatic bile ducts may dilate. However, this radiologic finding must always be interpreted in conjunction with the patient’s serum bilirubin levels. If bilirubin is elevated, the finding may represent a retained and obstructing stone within the common bile duct. In the absence of bilirubin elevation, common bile duct dilation may represent persistent dilation from a preoperative obstructing biliary stone that was removed or a postsurgical physiologic change (Fig. 3a, b, and c). Asymptomatic common bile duct dilatation of up to 10 mm can be considered as a normal range in patients after cholecystectomy. However, when the CBD is dilated beyond 10 mm, it may warrant further investigation with MRCP [13].
Asymptomatic long standing biliary ductal dilatation. a and b Axial CECT images in the same patient from 2006 and 2020, respectively, demonstrate dilatation of the common bile duct (arrows) after cholecystectomy. Common bile duct measured 18 mm. c Coronal CECT image of the patient in 2020 shows minimal dilatation of intrahepatic bile ducts (arrow). Bilirubin was in the normal range
Early complications
Biliary complications
Biliary complications are more common and complex after laparoscopy than open cholecystectomy [14]. However, over the past 3 decades, the rate of bile duct injury has decreased from 7 to 0.3–0.6% [15]. Biliary leak after cholecystectomy is usually due to iatrogenic injury to the common bile duct (CBD), cystic duct stump, or anatomical variants, including the accessory ducts of Luschka [15]. Often, the complication is not recognized during the procedure, and it is more challenging if there is surrounding inflammation or chronic fibrosis at the surgical site. Clinical signs and symptoms of bile duct injury are mostly related to bile stasis and leakage [15]. Presenting symptoms include abdominal pain, tenderness, fever, and nausea/emesis [15]. Infection or inflammation of the peritoneal cavity due to bile can present with leukocytosis and bandemia. Though nonspecific, hyperbilirubinemia is usually seen secondary to systemic bile reabsorption by the peritoneal surface; it can also be associated with biloma, cutaneous fistula, and peritonitis [16]. The radiologists should be aware of other differentials for hyperbilirubinemia including CBD obstruction and developing cholangitis in a post-surgical patient.
Various imaging modalities and procedures are available when evaluating patients for post-surgical bile injury. For all stable patients, the primary imaging study is RUQ ultrasound which helps to visualize extrahepatic fluid. Free fluid may extend along the peritoneum, but this is a nonspecific finding in postoperative patients [10]. Contrast-enhanced CT is better than sonography in evaluating uncontained bile leaks, ascites, and assessing the extent of a biloma when present. The term biloma refers to a well-demarcated collection of bile outside the biliary tract, whether intrahepatic or extrahepatic, encapsulated or not (Fig. 4a) [15, 17]. Bilomas measure simple fluid attenuation on CT, as do postoperative seromas. On MRI, bilomas demonstrate variable T1W and high T2W signal intensities similar to the contents of the gallbladder, and seromas demonstrate low signal intensity on T1W and high signal intensity on T2W MR. On both US and CT, attention should also be paid to evaluating CBD caliber to rule out occlusive injuries [16]. A critical imaging pitfall is that the absence of fluid collections does not exclude bile duct injury [18]. US or CT can also be utilized for aspiration of bile for diagnosis and placement of percutaneous drainage, which is also therapeutic.
Bile leak. Abdominal pain 2 weeks after cholecystectomy. a Coronal CECT image shows minimal fluid at the cholecystectomy site (arrowhead). However, there is a moderate volume of intraabdominal free fluid (arrow) and fluid in the pelvis (*), which is more than a physiologic amount. b and c Biliary scintigraphy shows focal tracer activity in the region of the cystic duct (arrow b), and subsequently, on the delayed scan, the tracer extends along the right paracolic gutter into the pelvis, confirming bile leak (arrow c). Percutaneous transhepatic cholangiography was performed, and an internal and external biliary drain was placed
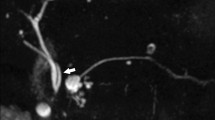
Imaging modalities to confirm the presence of bile leak include MRCP and delayed post-contrast MRI with hepatobiliary contrast material and nuclear scintigraphy HIDA (hepatobiliary iminodiacetic acid) scans. HIDA has increased sensitivity over MRCP and demonstrates extraluminal extravasation (Fig. 4b and c) of the nuclear tracer in the setting of an ongoing bile leak [15]. However, MRCP is superior in delineating ductal anatomy and identifying the precise localization of ductal injury, which is critically important in determining the treatment approach [16]. Using hepatocyte-specific contrast agents that are primarily excreted via bile improves diagnostic confidence [19]. Two liver-specific agents are available in the US and Europe: gadolinium ethoxy benzyl diethylenetriamine penta-acetic acid (Gd-EOB-DTPA) and gadobenate dimeglumine (Gd-BOPTA) [20]. The accuracy, sensitivity, and specificity of dynamic Gd-EOB-DTPA enhanced T1W MR in the detection of biliary leaks are 92.9%, 90.5%, and 100%, respectively [21]. Combining Gd-EOB-DTPA-enhanced MRCP in addition to T2w-MRCP has been shown to significantly increase the sensitivity and accuracy of postoperative bile leak (79% and 84%, respectively), compared to T2w-MRCP alone (59% and 58%) (Fig. 5 a–d) [22]. However, opacification of bile ducts with MR contrast is limited in the presence of obstruction, and the delineation of peripheral intrahepatic bile ducts is limited. Invasive techniques like ERCP (endoscopic retrograde cholangiopancreaticography) not only allow for the evaluation of biliary tree injury/leak but have the option of intervention at the time of diagnosis, such as internal stent placement (Fig. 6a) [15].
Post-cholecystectomy bile leak and role of MR contrast: a Coronal CECT image shows bilobed hypodense fluid collection (arrowhead) around the surgical clips. The following day, MR examination was performed after administering gadolinium ethoxy benzyl diethylenetriamine penta-acetic acid (Gd-EOB-DTPA). b Coronal T2 weighted images of MR show hyperintense fluid collection (arrowhead) corresponding to fluid in the CT image. c Coronal T1 contrast image delayed (20 min) reveals hypointense fluid collection (arrowhead) with no contrast leak. However, d coronal T1 contrast image obtained after 80 min delay reveals hyperintense contrast material within the common bile duct (arrow) and contrast leak into the cholecystectomy site confirming bile leak
Bile leak and intervention. Post-op bile leak after subtotal laparoscopic cholecystectomy for gangrenous cholecystitis. The patient was initially managed with ERCP and stent placement and percutaneous drain. The patient re-presented with sepsis from ongoing bile leak. a Coronal CECT demonstrates organized fluid collection (arrow) in the gallbladder fossa and a biliary stent within the common bile duct (arrowhead). b Coronal CECT image more posteriorly demonstrates mild inflammation in the subhepatic region adjacent to the hepatic flexure (arrowhead). The patient was taken to IR for embolization. c Sinogram demonstrates contrast within the cystic duct stump. d The stump is crossed with a wire into the biliary system and a single helix coil was deployed within the cystic duct (arrow). Followed by an injection of 1.5 cc of n-butyl cyanoacrylate glue (arrowhead)
The classification of bile duct injury is well established in the literature; however, it is beyond the scope of this article. Small and slow leaks may resolve spontaneously, and large leaks may require image-guided percutaneous transhepatic biliary drainage or may warrant endoscopic approaches, including sphincterotomy, transhepatic biliary drainage catheter, and bile duct stenting [23]. In complex cases refractory to stent placement, some authors described selective transcatheter embolization of the cystic stump, replacing surgical management as an alternative (Fig. 6b, c, and d) [23, 24]. Seewald et al. successfully described occlusion of bile leak with the injection of N-butyl-2-cyanoacrylate (NBCA), a tissue glue monomer that solidifies on contact with body fluids at neutral pH, and Schelhammer et al. first described the coil embolization of cystic duct stump after cholecystectomy [24, 25]. A combination of coils and NBCA is favored over NBCA or coils alone [23]. Surgical management may be required in a few cases and includes liver resection, bile duct reconstruction, or bilioenteric anastomosis when radiological and minimally invasive endoscopic techniques fail [23].
Vascular complications
Vascular injuries occur invariably during the creation of a laparoscopic port or the intervention at the surgical bed. They are classified into major and minor vessel injuries [26]. Major vascular injuries most commonly occur within Calot’s triangle involving the hepatic artery, cystic artery, or portal vein; however, injuries involving the abdominal aorta, IVC, and iliac vessels are also reported in the literature [26, 27]. Vascular injuries to epigastric, mesenteric, and omental vessels are classified as minor vascular injuries [26]. Bleeding within the surgical bed can also occur without apparent injury to vessels secondary to surgical factors like improper instrumentation or technique and patient-related factors like hepatic disease and coagulopathy. Subcapsular hematoma and hepatic artery pseudoaneurysm following laparoscopic cholecystectomy are also reported in the literature [28, 29]. Overall, the rate of hemorrhage is 4.1%, with 2.3% occurring intraoperatively and 1.8% postoperatively; variable incidence rates have been shown in different studies [10, 30]. The diagnosis of intraoperative vascular injury is straightforward and can be managed immediately. Postoperative abdominal wall and intraperitoneal bleeding are usually discovered in the early postoperative period.
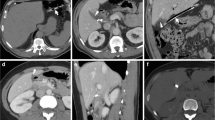
On sonography, hemorrhage appears as free heterogeneously echogenic fluid or a fluid collection in the setting of a formed hematoma [10]. US Doppler evaluation can help diagnose vascular injury [16]. CT identifies hematomas as heterogeneously hyperdense fluid collections with or without surrounding inflammatory stranding, which could be related to expected postoperative changes or surgical complications (Fig. 7a and b). MDCT with IV contrast is an efficient way to demonstrate active contrast extravasation to reveal the focus of bleeding or pseudoaneurysm (Fig. 7c). Hepatic artery pseudoaneurysms can be directly visualized or may only show a surrounding hematoma [10]. This finding on CT warrants selective angiography of the celiac and superior mesenteric arteries with subsequent endovascular treatment (Fig. 7d and e).
Vascular injury: 62-year-old male, post-op day 3 from cholecystectomy for gangrenous cholecystitis, with tachycardia and decreasing hemoglobin. a Axial non-contrast CT image shows hyperdense fluid collection in the surgical bed (*) and along the posterior surface of the liver (*). Note fluid–fluid level (arrow) within the posterior hepatic region hematoma. b Axial CECT image in arterial phase shows replaced right hepatic artery (arrowhead) and hematoma in the surgical bed (*). c Axial CECT image in portal venous phase shows contrast blush next to the cholecystectomy clips (arrowhead), concerning for vascular injury and active extravasation. d Selective angiogram of the replaced right hepatic artery demonstrates contrast blush (arrow) at the expected area of the cystic artery remnant adjacent to surgical clips (arrowhead). Additionally, this angiographic finding correlates to the same finding seen on prior CTA. e A vascular coil was deployed (arrow) with the resolution of contrast blush
On MR, the signal intensity of hemorrhage is based on age and the evolution of the blood products. Subcapsular hemorrhage from liver capsule tears is a rare but severe complication [29, 31]. The onset varies widely from 6 h to 6 weeks post-laparoscopic cholecystectomy and is mostly reported in females [31]. Postulated predisposing factors for subcapsular hematoma include spontaneous hemorrhage of liver parenchyma, damage due to trocar placement, excessive traction of the gallbladder causing injury to the liver capsule, damage to the liver during pulling the gallbladder, anti-inflammatory drugs like ketorolac used in the perioperative pain management, or rarely ruptured hepatic hemangioma [29]. On CT examination with contrast, a subcapsular hematoma is identified as a biconvex hypodense to the heterogeneously dense lesion with or without mass effect on liver parenchyma (Fig. 8a and b). A careful search should be done for bleeding from the gallbladder bed, an intraabdominal extension of bleeding, and for underlying hepatic lesions [29]. The management of hepatic subcapsular hemorrhage depends on the patient’s clinical status and the hematoma size. Subcapsular hematomas are prone to secondary infection (Fig. 8c).
Subcapsular hematoma. Post-op day 10, with abdominal pain. a Axial and b coronal CECT images show subcapsular hematoma (*) along the anterior and lateral perihepatic region with smooth mass effect on the hepatic surface (arrowheads). Initially, the collection subsided (not illustrated), but eventually, the patient was readmitted due to increased abdominal pain and fever. c Repeat CECT axial image shows fluid collection with rim enhancement (arrowhead) along the subcapsular region of the liver, suggesting abscess formation. Under CT guidance pigtail drain catheter was placed in the fluid collection (not shown)
Portal vein thrombosis is an infrequent complication after laparoscopic surgery, including laparoscopic cholecystectomy, with most case reports in patients with preoperatively unknown hypercoagulable conditions; pneumoperitoneum and increased abdominal pressure may also play a role [32].
Late complications
Stump/remnant cholecystitis
Remnant cholecystitis occurs due to a long remnant cystic duct or gallbladder remnant following a subtotal cholecystectomy. Subtotal cholecystectomies are usually performed due to severe inflammation or adhesions obstructing surgical views preventing safe dissection of Calot’s Triangle [33]. It occurs more frequently in laparoscopic approaches due to surgical technique favoring a long cystic duct remnant and poor dexterity, allowing for retained stones [34]. Incomplete surgery can lead to PCS, a recurrence of symptoms resembling the initial cholecystitis [33]. Post-operative incidence of remnant cholecystitis is reported as high as 5% following cholecystectomy, with increased incidence in emergent compared to elective cholecystectomy. It is also more common in middle-aged women [35].
The pathophysiology involves inflammation of the cystic duct or gallbladder remnant following cholecystectomy, with retained or recurrent gallstones, mucoceles, neuromas, or suture granulomas blocking the remnant cystic duct or gallbladder remnant causing obstruction and subsequent inflammation [35]. Ideally, the cystic duct remnant is no longer than 5 mm. A study by Kar et al. with a cohort of patients suffering from PCS secondary to cystic duct remnant stones had stump lengths ranging from 1.3 to 6 cm [36].
Despite a highly suggestive clinical presentation, diagnoses of the stump, or remnant cholecystitis are delayed due to low clinical suspicion in the setting of a history of cholecystectomy. Therefore, it is important for clinicians and radiologists to maintain an awareness of post-cholecystectomy syndrome secondary to remnant cholecystitis and be able to identify radiographic findings.
Abdominal ultrasound is an inexpensive and readily accessible modality for detecting signs of stump or remnant cholecystitis. A cystic duct measuring > 5 mm in diameter is considered abnormal and dilated, especially in a post-cholecystectomy patient, and should result in a low threshold for suspicion for stump or remnant cholecystitis. Signs on ultrasound include a fluid-filled saclike structure within the gallbladder fossa, which may contain shadowing caliculi or direct visualization of caliculi within a remnant cystic duct or dilatation of the cystic duct > 5 mm [33]. One study showed that a primary diagnosis of stump cholecystitis was made with ultrasound in 88.8% of cases [37]. On CT imaging, evidence of stones, microliths, or sludge with wall thickening, enhancement near the cystic duct stump or remnant gallbladder, and adjacent fat stranding are clues to the diagnosis (Fig. 9a, b, c, and d) [27]. CT may also reveal a dilated cystic duct stump, and when pathologically dilated, they are often described as having the appearance of a “flashlight bulb” [38].
Stump cholecystitis. A 33-year-old female presents to ED 5 years after cholecystectomy. No acute abnormality was reported. a Axial CECT images reveal surgical clips and avid wall enhancement of remnant gallbladder/long cystic duct (arrow). b Coronal CECT image reveals dependent stones. Post-cholecystectomy was mentioned in the report, but no definite diagnosis was made. The same patient presented to ED a year later. c Axial CECT image shows remnant gallbladder wall thickening (arrow) and trace pericholecystic stranding (arrowhead). d Coronal CECT image shows cystic duct enhancement and surrounding fluid (arrow). The patient was treated with laparoscopic cholecystectomy
Biliary (CBD stones, pancreatitis, strictures)
Calculi in the common bile duct (CBD) are considered one of the most common causes of PCS. A total of 10 to 18% of patients undergoing cholecystectomy have concomitant stones in the CBD, and up to 3.8% of patients have symptoms as a result of these retained stones [39]. These symptoms usually result from retained CBD stones causing biliary obstruction after laparoscopic cholecystectomy, in which CBD exploration is challenging [4]. Also, small gallbladder stones may migrate into the CBD in patients with a patulous cystic duct when the gallbladder is pulled in a cephalad direction during its dissection [40].
In one study by Lee et al., the prevalence of clinically significant retained CBD stones after laparoscopic cholecystectomy was 1.84%. The median time from laparoscopic cholecystectomy to ERCP was 152 days, ranging from postoperative 2 months to 2 years and 9 months [41]. While a relatively rare occurrence, it is important to be knowledgeable of imaging findings suggestive of CBD stones in the symptomatic post-cholecystectomy patient.
Abdominal US is a first-line imaging modality with limited sensitivity for CBD stones (18–63%) owing to obscuration of the distal CBD by adjacent bowel gas but a high specificity of 70–98% [42]. US findings of CBD stones include echogenic foci that may demonstrate posterior acoustic shadowing within a fluid-filled bile duct. Dilatation of the CBD on US is of limited diagnostic power for identifying CBD stones [42]. US for CBD stones is limited by obfuscation due to artifacts caused by pneumobilia, surgical clips, biliary stents, duodenal diverticula, and calcifying pancreatitis [39].
CT imaging detects CBD stones with a sensitivity of 71–85% and specificity of 88–97% [39]. Detection and appearance of gallstones on CT may vary, with calcified gallstones being readily detected at CT, but noncalcified gallstones are often difficult to visualize particularly if central nitrogen gas from degeneration is absent because they are isoattenuating to the surrounding bile. Stone size can also influence CT detectability, with one study showing that 96% of stones larger than 5 mm were detectable by CT, but only 67% of stones smaller than 5 mm were detectable [43]. An obstructive calculus can present with upstream dilatation of CBD and intrahepatic bile ducts (Fig. 10a).
Acute pancreatitis. A 54-year-old male presented with abdominal pain, lipase > 3000, 6 weeks after cholecystectomy. a Axial CECT image shows mild dilatation of intrahepatic biliary ducts (arrowheads). b Axial CECT image demonstrates thickening and enhancement of common bile duct (arrowhead) and edematous pancreas with peripancreatic inflammatory stranding (arrows). c Coronal CECT image demonstrates impacted stone within the ampulla (arrowhead) and dilated CBD (arrow). ERCP was done on the following day after CT and sphincterotomy was performed
Compared with US and CT, MRCP has the highest sensitivity at 89–95% and specificity at 95–100% for detecting stones in the CBD [42]. CBD stones appear as low-signal-intensity foci surrounded by bright bile on T2-weighted MR images and demonstrate no enhancement. Biliary inflammation that is often associated with symptomatic CBD stones can be seen on MRCP as periductal edema, biliary wall thickening, and enhancement after contrast material administration [42].
Gallstone pancreatitis secondary to retained or recurrent CBD stones is also a common sequela of PCS. While stones less than 5 mm are often clinically silent and pass into the duodenum via the ampulla of Vater, stones greater than 5 mm can obstruct the CBD or ampulla and cause pancreatitis [42] (Fig. 10b and c). In one study of 272 patients diagnosed with post-cholecystectomy syndrome, 15.4% of patients were found to have pancreatitis as the cause [44].
US has little value in diagnosing pancreatitis or its complications; however, US is usually reserved to confirm or exclude the presence of stones or biliary dilatation. Obscuring overlying gas can limit the evaluation of the entire pancreatic parenchyma.
On CT, findings of pancreatitis include an enlarged pancreas with relatively normal enhancement. Peripancreatic fat may be normal or show mild stranding and opacity due to inflammation, with small to varying amounts of non-enhancing peripancreatic fluid (Fig. 10b and c). CT also has moderate sensitivity in identifying inciting gallstones and biliary stones (Fig. 10c) [45].
The sensitivity of MRI exceeds that of CT imaging, emphasizing its role in the evaluation of patients with clinically suspected acute pancreatitis and negative CT imaging findings. Acute interstitial edematous pancreatitis on MRI often shows generalized enlargement of the pancreas, focal swelling due to inflammatory edema of the pancreas, surrounding peripancreatic fat stranding, and relatively homogenous enhancement with contrast. Peripancreatic fluid may also be present [46].
Strictures are a less common complication of cholecystectomy, occurring in 0.6% of patients in months or years following the procedure. They usually result from injury to the CBD during clamping or ligation of the cystic duct [8]. Strictures can be an etiology of PCS causing obstruction and subsequent cholecystitis-like symptoms. The incidence of biliary stricture is reported to be higher in laparoscopic cholecystectomy (0.6%) than open cholecystectomy (0.2%) [47].
While US is the initial diagnostic test of choice and has a sensitivity approaching 100% for the detection of biliary dilatation or obstruction that is commonly present in the setting of biliary strictures, it has a low yield for the detection of the stricture itself [48].
CT imaging helps in the detection of biliary dilatation, the underlying cause of biliary obstruction, and complications such as cholangitis and cholangitic abscess [47]. Studies show that CT demonstrates biliary stricture with a sensitivity of 40–77% and specificity of 57–63% [49]. Strictures are seen on CT as upstream intrahepatic biliary ductal dilatation with focal smooth narrowing of the strictured segment. The most common pattern is the dilatation of ducts in both lobes; however, isolated dilatation of ducts in a single lobe is also possible [49].
MRCP has a sensitivity and specificity of 94% and 97%, respectively, for the diagnosis of biliary strictures [50]. MRCP can demonstrate biliary strictures as narrowing of the lumen and are usually short with smooth, regular margins [8]. Defining the site and extent of a stricture is important to determine management. Notably, MRCP can overestimate the length and extent of the stricture, especially when the duct immediately distal to the stricture is collapsed leading to misinterpretation of the position of the distal end of the stenosis [8].
Post-cholecystectomy clip migration
Post-cholecystectomy clip migration (PCCM) is a rare but notable cause of late post-cholecystectomy complications. The median time between surgery and symptomatic presentation due to PCCM is reported at around 2 years [27, 51]. The number of clips used is cited as an important factor with the median number of clips used being 6 in patients presenting with PCS secondary to PCCM [51]. The use of more than four clips, inaccurate clip placement, localized inflammation, and infection is associated with clip migrations, most commonly migrating into the CBD. The sequelae of clip migration include stone formation, obstructive jaundice, cholangitis, biliary colic, Mirizzi syndrome, fistula, and acute pancreatitis [27]. One study by Chong et al. demonstrated that common diagnoses at presentations of PCCM were obstructive jaundice (37.7%), cholangitis (27.5%), biliary colic (18.8%), and acute pancreatitis (8.7%) [51].
Ultrasound may show secondary findings of PCCM, such as stones, as clips may serve as a nidus for formation or biliary dilatation. CT may show a migrated clip as a high-density metallic focus in the remnant cystic duct remnant, common bile duct, or duodenum (Fig. 11a, b, and c) as well as show evidence of clip migration through secondary findings such as strictures, stone formation around a clip, and biliary dilatation or reactive changes in the duodenum (Fig. 11c) [52]. MRCP can similarly show secondary findings and directly visualize the clip as a susceptibility artifact in an inappropriate location within the biliary tract [27].
Clip migration. A 78-year-old female with duodenitis secondary to erosion of cholecystectomy clips. a axial and b coronal CECT images show surgical clips (arrow) within the first portion of the duodenum. The surgical clips were missed in the initial evaluation due to hyperdense enteric contrast material. c Sagittal CECT image shows diffuse circumferential wall thickening of the duodenum (arrows)
Dropped gallstones (and related complications)
Dropped gallstones are a relatively common complication following laparoscopic cholecystectomy, occurring in 25–30% of cases and presenting several months after surgery [27]. This type of complication is unique to laparoscopic cholecystectomy without reported cases during open/classic surgery in the literature [53]. Effraction of the gallbladder during laparoscopy is well-known, and reported incidence ranges from 10 to 40% [54]. Gallbladder perforation during LC can occur at three stages: during retraction, during the separation of the gallbladder from the liver bed, and during gallbladder extraction from the abdomen via a small incision with high pressure. In the literature, spillage of gallstones after LC was reported as up to 6.9% and 1–2.4% of dropped stones may not be retrieved [55, 56]. Surgeons usually attempt the retrieval of dropped stones; however, some may be fragmented, inaccessible, or overlooked and remain within the peritoneal cavity. Although the incidence of gallbladder perforation and gallstone spillage is high, most dropped gallstones remain asymptomatic and are found incidentally on imaging. Abscess formation is the most common complication reported in literature [27, 57]. Usually, abscess formation occurs within the first year after surgery, but delayed abscess formation has been reported even 15 years after cholecystectomy [54]. Frequent locations of abscess secondary to dropped gallstones are the abdominal wall, subhepatic space, retroperitoneum inferior to subhepatic space, and very rarely within the thoracic cavity [27, 54]. Other known complications secondary to dropped gallstones include fistula formation (enteral, colic, biliary), sinus tracts, and implantation of stones into ovaries, fallopian tubes, and inside an inguinal hernia [53].
US can demonstrate fluid collections within the subhepatic and subdiaphragmatic regions with retained gallstones appearing as hyperechoic lesions [58]. On CT imaging, dropped gallstones are seen as hyperdense rounded structures if calcified (Fig. 12a) [10]. When complicated by abscess, surrounding fluid collection or inflammation can be identified. MRI shows a perihepatic fluid collection with foci of low T2 signal, representative of stones (Fig. 12b, c, d, and e) [59]. The definitive treatment of complicated dropped gallstones consists of pus drainage and stone retrieval; hence, recognizing a stone within the abscess is quintessential. Imaging pitfalls include distinguishing from calcified peritoneal malignant metastases, “peritoneal mice,” contrast filled colonic diverticula, and dropped appendicoliths [27, 59]. Other biliary complications such as cholangitis, biliary cutaneous fistula, or hepatic abscess can also occur.
Dropped gallstones, two different patients, incidental, and complicated. Incidental intraperitoneal gallstones. a Axial CECT image shows a cluster of rounded calcified gallstones along the posterior aspect of the liver (arrowheads). A different patient presents with abdominal pain and fever prior history of cholecystectomy. b Axial T1WI shows dependent low signal collection posterior to the liver (arrow), which contains gallstones (arrowhead). c Coronal T2WI depicts that the fluid is heterogeneously intense. d and e Post-contrast axial and coronal T1WI illustrates rim enhancement (arrow); the collection is inseparable from the liver parenchyma. The patient was managed surgically, and a small portion of the liver was resected
Conclusion
The spectrum of post-op complications and symptoms, such as upper abdominal pain and dyspepsia, are referred to as post-cholecystectomy syndrome (PCS). Post-operative complications of laparoscopic cholecystectomy can occur in the immediate post-operative period and can also have late presentations long after surgery. Complications can be secondary to bile duct injury, including bile leak and stricture formation, vascular injuries, and residual or recurrent biliary stones. These complications can cause significant morbidity and mortality, and thus familiarity with the expected post-surgical appearance of the gallbladder fossa and biliary tract as well as understanding the spectrum of complications and associated multimodality imaging findings are essential for emergency radiologists and those practicing in the acute care setting to direct appropriate patient management.
References
Jones MW GE, Deppen JG Open Cholecystectomy. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK448176/?report=classic. Accessed 24 Oct 2022
Reynolds W Jr (2001) The first laparoscopic cholecystectomy. Jsls 5(1):89–94
Gadacz TR, Talamini MA (1991) Traditional versus laparoscopic cholecystectomy. Am J Surg 161(3):336–338. https://doi.org/10.1016/0002-9610(91)90591-z
Desai NS, Khandelwal A, Virmani V, Kwatra NS, Ricci JA, Saboo SS (2014) Imaging in laparoscopic cholecystectomy–what a radiologist needs to know. Eur J Radiol 83(6):867–879. https://doi.org/10.1016/j.ejrad.2014.02.016
Catalano OA, Singh AH, Uppot RN, Hahn PF, Ferrone CR, Sahani DV (2008) Vascular and biliary variants in the liver: implications for liver surgery. Radiographics 28(2):359–378. https://doi.org/10.1148/rg.282075099
Wojcicki M, Patkowski W, Chmurowicz T, Bialek A, Wiechowska-Kozlowska A, Stankiewicz R, Milkiewicz P, Krawczyk M (2013) Isolated right posterior bile duct injury following cholecystectomy: report of two cases. World J Gastroenterol 19(36):6118–6121. https://doi.org/10.3748/wjg.v19.i36.6118
Mariolis-Sapsakos T, Kalles V, Papatheodorou K, Goutas N, Papapanagiotou I, Flessas I, Kaklamanos I, Arvanitis DL, Konstantinou E, Sgantzos MN (2012) Anatomic variations of the right hepatic duct: results and surgical implications from a cadaveric study. Anat Res Int 2012:838179. https://doi.org/10.1155/2012/838179
Girometti R, Brondani G, Cereser L, Como G, Del Pin M, Bazzocchi M, Zuiani C (2010) Post-cholecystectomy syndrome: spectrum of biliary findings at magnetic resonance cholangiopancreatography. Br J Radiol 83(988):351–361. https://doi.org/10.1259/bjr/99865290
Tonolini M, Ierardi AM, Patella F, Carrafiello G (2018) Early cross-sectional imaging following open and laparoscopic cholecystectomy: a primer for radiologists. Insights Imaging 9(6):925–941. https://doi.org/10.1007/s13244-018-0663-9
Thurley PD, Dhingsa R (2008) Laparoscopic cholecystectomy: postoperative imaging. AJR Am J Roentgenol 191(3):794–801. https://doi.org/10.2214/AJR.07.3485
Turley BR, Taupmann RE, Johnson PL (1994) Postoperative abscess mimicked by surgicel. Abdom Imaging 19(4):345–346. https://doi.org/10.1007/bf00198195
Stringer MD, Dasgupta D, McClean P, Davison S, Ramsden W (2003) “Surgicel abscess” after pediatric liver transplantation: a potential trap. Liver Transpl 9(2):197–198. https://doi.org/10.1053/jlts.2003.50059
Park SM, Kim WS, Bae IH, Kim JH, Ryu DH, Jang LC, Choi JW (2012) Common bile duct dilatation after cholecystectomy: a one-year prospective study. J Korean Surg Soc 83(2):97–101. https://doi.org/10.4174/jkss.2012.83.2.97
Khan MH, Howard TJ, Fogel EL, Sherman S, McHenry L, Watkins JL, Canal DF, Lehman GA (2007) Frequency of biliary complications after laparoscopic cholecystectomy detected by ERCP: experience at a large tertiary referral center. Gastrointest Endosc 65(2):247–252. https://doi.org/10.1016/j.gie.2005.12.037
Copelan A, Bahoura L, Tardy F, Kirsch M, Sokhandon F, Kapoor B (2015) Etiology, diagnosis, and management of bilomas: a current update. Tech Vasc Interv Radiol 18(4):236–243. https://doi.org/10.1053/j.tvir.2015.07.007
Cohen JT, Charpentier KP, Beard RE (2019) An update on iatrogenic biliary injuries: identification, classification, and management. Surg Clin North Am 99(2):283–299. https://doi.org/10.1016/j.suc.2018.11.006
Kuligowska E, Schlesinger A, Miller KB, Lee VW, Grosso D (1983) Bilomas: a new approach to the diagnosis and treatment. Gastrointest Radiol 8(3):237–243. https://doi.org/10.1007/BF01948126
Braghetto I, Bastias J, Csendes A, Debandi A (2000) Intraperitoneal bile collections after laparoscopic cholecystectomy: causes, clinical presentation, diagnosis, and treatment. Surg Endosc 14(11):1037–1041. https://doi.org/10.1007/s004649900029
Aduna M, Larena JA, Martin D, Martinez-Guerenu B, Aguirre I, Astigarraga E (2005) Bile duct leaks after laparoscopic cholecystectomy: value of contrast-enhanced MRCP. Abdom Imaging 30(4):480–487. https://doi.org/10.1007/s00261-004-0276-2
Petrillo M, Ierardi AM, Tofanelli L, Maresca D, Angileri A, Patella F, Carrafiello G (2019) Gd-EOB-DTP-enhanced MRC in the preoperative percutaneous management of intra and extrahepatic biliary leakages: does it matter? Gland Surg 8(2):174–183. https://doi.org/10.21037/gs.2019.03.09
Kul M, Erden A, Dusunceli Atman E (2017) Diagnostic value of Gd-EOB-DTPA-enhanced MR cholangiography in non-invasive detection of postoperative bile leakage. Br J Radiol 90(1072):20160847. https://doi.org/10.1259/bjr.20160847
Kantarci M, Pirimoglu B, Karabulut N, Bayraktutan U, Ogul H, Ozturk G, Aydinli B, Kizrak Y, Eren S, Yilmaz S (2013) Non-invasive detection of biliary leaks using Gd-EOB-DTPA-enhanced MR cholangiography: comparison with T2-weighted MR cholangiography. Eur Radiol 23(10):2713–2722. https://doi.org/10.1007/s00330-013-2880-4
Nezami N, Jarmakani H, Arici M, Latich I, Mojibian H, Ayyagari RR, Pollak JS, Perez Lozada JCL (2019) Selective trans-catheter coil embolization of cystic duct stump in post-cholecystectomy bile leak. Dig Dis Sci 64(11):3314–3320. https://doi.org/10.1007/s10620-019-05677-5
Seewald S, Groth S, Sriram PV, Xikun H, Akaraviputh T, Mendoza G, Brand B, Seitz U, Thonke F, Soehendra N (2002) Endoscopic treatment of biliary leakage with n-butyl-2 cyanoacrylate. Gastrointest Endosc 56(6):916–919. https://doi.org/10.1067/mge.2002.129873
Schelhammer F, Dahl SV, Heintges T, Furst G (2007) A multimodal approach in coil embolization of a bile leak following cholecystectomy. Cardiovasc Intervent Radiol 30(3):529–530. https://doi.org/10.1007/s00270-006-0090-z
Kaushik R (2010) Bleeding complications in laparoscopic cholecystectomy: incidence, mechanisms, prevention and management. J Minim Access Surg 6(3):59–65. https://doi.org/10.4103/0972-9941.68579
Sureka B, Mukund A (2017) Review of imaging in post-laparoscopy cholecystectomy complications. Indian J Radiol Imaging 27(4):470–481. https://doi.org/10.4103/ijri.IJRI_489_16
Yao CA, Arnell TD (2010) Hepatic artery pseudoaneurysm following laparoscopic cholecystectomy. Am J Surg 199(1):e10-11. https://doi.org/10.1016/j.amjsurg.2009.03.014
Moloney BM, Hennessy N, Malley EO, Orefuwa F, McCarthy PA, Collins CG (2017) Subcapsular haematoma following laparoscopic cholecystectomy. BJR Case Rep 3(2):20160118. https://doi.org/10.1259/bjrcr.20160118
Schafer M, Lauper M, Krahenbuhl L (2000) A nation’s experience of bleeding complications during laparoscopy. Am J Surg 180(1):73–77. https://doi.org/10.1016/s0002-9610(00)00416-5
Saad E, O’Connell L, Browne AM, Khan W, Waldron R, Barry K, Khan IZ (2020) Giant intrahepatic subcapsular haematoma: a rare complication following laparoscopic cholecystectomy-a case report and literature review. Case Rep Surg 2020:6410790. https://doi.org/10.1155/2020/6410790
Ikoma N, Anderson CL, Ohanian M, Juneja HS, MacFadyen BV, Shah SK, Bajwa KS (2014) Portal vein thrombosis after laparoscopic cholecystectomy. JSLS 18(1):125–127. https://doi.org/10.4293/108680813X13654754535674
Calhoun SK, Piechowiak RL (2010) Recurrent cholecystitis and cholelithiasis in a gallbladder remnant 14 years after a converted cholecystectomy. Radiol Case Rep 5(1):332. https://doi.org/10.2484/rcr.v5i1.332
Tantia O, Jain M, Khanna S, Sen B (2008) Post cholecystectomy syndrome: role of cystic duct stump and re-intervention by laparoscopic surgery. J Minim Access Surg 4(3):71–75. https://doi.org/10.4103/0972-9941.43090
Cawich SO, Wilson C, Simpson LK, Baker AJ (2014) Stump cholecystitis: laparoscopic completion cholecystectomy with basic laparoscopic equipment in a resource poor setting. Case Rep Med 2014:787631. https://doi.org/10.1155/2014/787631
Kar A, Gulati S, Mohammed S, Valappil MV, Sarala BB, Ghatak S, Bhattacharyya A (2018) Surgical management of cystic duct stump stone or gall bladder remnant stone. Indian J Surg 80(3):284–287. https://doi.org/10.1007/s12262-018-1724-5
Mageed SAA, Omar MA, Redwan AA (2018) Remnant gall bladder and cystic duct stump stone after cholecystectomy: tertiary multicenter experience. Int Surg J
Perera E, Bhatt S, Dogra VS (2011) Cystic duct remnant syndrome. J Clin Imaging Sci 1:2. https://doi.org/10.4103/2156-7514.73500
Almadi MA, Barkun JS, Barkun AN (2012) Management of suspected stones in the common bile duct. CMAJ 184(8):884–892. https://doi.org/10.1503/cmaj.110896
Kim JY, Kim KW, Ahn CS, Hwang S, Lee YJ, Shin YM, Lee MG (2008) Spectrum of biliary and nonbiliary complications after laparoscopic cholecystectomy: radiologic findings. AJR Am J Roentgenol 191(3):783–789. https://doi.org/10.2214/AJR.07.3602
Lee DH, Ahn YJ, Lee HW, Chung JK, Jung IM (2016) Prevalence and characteristics of clinically significant retained common bile duct stones after laparoscopic cholecystectomy for symptomatic cholelithiasis. Ann Surg Treat Res 91(5):239–246. https://doi.org/10.4174/astr.2016.91.5.239
Ratanaprasatporn L, Uyeda JW, Wortman JR, Richardson I, Sodickson AD (2018) Multimodality imaging, including dual-energy CT, in the evaluation of gallbladder disease. Radiographics 38(1):75–89. https://doi.org/10.1148/rg.2018170076
Kim CW, Chang JH, Lim YS, Kim TH, Lee IS, Han SW (2013) Common bile duct stones on multidetector computed tomography: attenuation patterns and detectability. World J Gastroenterol 19(11):1788–1796. https://doi.org/10.3748/wjg.v19.i11.1788
Shirah BH, Shirah HA, Zafar SH, Albeladi KB (2018) Clinical patterns of postcholecystectomy syndrome. Ann Hepatobiliary Pancreat Surg 22(1):52–57. https://doi.org/10.14701/ahbps.2018.22.1.52
Busireddy KK, AlObaidy M, Ramalho M, Kalubowila J, Baodong L, Santagostino I, Semelka RC (2014) Pancreatitis-imaging approach. World J Gastrointest Pathophysiol 5(3):252–270. https://doi.org/10.4291/wjgp.v5.i3.252
Manikkavasakar S, AlObaidy M, Busireddy KK, Ramalho M, Nilmini V, Alagiyawanna M, Semelka RC (2014) Magnetic resonance imaging of pancreatitis: an update. World J Gastroenterol 20(40):14760–14777. https://doi.org/10.3748/wjg.v20.i40.14760
Shanbhogue AK, Tirumani SH, Prasad SR, Fasih N, McInnes M (2011) Benign biliary strictures: a current comprehensive clinical and imaging review. AJR Am J Roentgenol 197(2):W295-306. https://doi.org/10.2214/AJR.10.6002
Singh A, Gelrud A, Agarwal B (2015) Biliary strictures: diagnostic considerations and approach. Gastroenterol Rep (Oxf) 3(1):22–31. https://doi.org/10.1093/gastro/gou072
Gorsi U, Gupta P, Kalra N, Kang M, Singh R, Gupta R, Gupta V, Khandelwal N (2015) Multidetector computed tomography evaluation of post cholecystectomy complications: a tertiary care center experience. Trop Gastroenterol 36(4):236–243. https://doi.org/10.7869/tg.297
Ward J, Sheridan MB, Guthrie JA, Davies MH, Millson CE, Lodge JP, Pollard SG, Prasad KR, Toogood GJ, Robinson PJ (2004) Bile duct strictures after hepatobiliary surgery: assessment with MR cholangiography. Radiology 231(1):101–108. https://doi.org/10.1148/radiol.2311030017
Chong VH, Chong CF (2010) Biliary complications secondary to post-cholecystectomy clip migration: a review of 69 cases. J Gastrointest Surg 14(4):688–696. https://doi.org/10.1007/s11605-009-1131-0
Entel RJ, Peebles MW (1996) Migratory surgical clip in the common bile duct: CT diagnosis. Abdom Imaging 21(4):329–330. https://doi.org/10.1007/s002619900074
Moga D, Perisanu S, Popentiu A, Sora D, Magdu H (2016) Right retroperitoneal and subhepatic abscess; late complications due to spilled stones during laparoscopic cholecystectomy - case report. Chirurgia (Bucur) 111(1):67–70
Robinson JR, Wright JK, Geevarghese SK (2015) Dropped gallstones causing a perihepatic abscess and empyema. Case Rep Surg 2015:629704. https://doi.org/10.1155/2015/629704
Diez J, Arozamena C, Gutierrez L, Bracco J, Mon A, Sanchez Almeyra R, Secchi M (1998) Lost stones during laparoscopic cholecystectomy. HPB Surg 11(2):105–108. https://doi.org/10.1155/1998/95874. (discuss 108-109)
Woodfield JC, Rodgers M, Windsor JA (2004) Peritoneal gallstones following laparoscopic cholecystectomy: incidence, complications, and management. Surg Endosc 18(8):1200–1207. https://doi.org/10.1007/s00464-003-8260-4
Zehetner J, Shamiyeh A, Wayand W (2007) Lost gallstones in laparoscopic cholecystectomy: all possible complications. Am J Surg 193(1):73–78. https://doi.org/10.1016/j.amjsurg.2006.05.015
Viera FT, Armellini E, Rosa L, Ravetta V, Alessiani M, Dionigi P, Rossi S (2006) Abdominal spilled stones: ultrasound findings. Abdom Imaging 31(5):564–567. https://doi.org/10.1007/s00261-005-0241-8
Nayak L, Menias CO, Gayer G (2013) Dropped gallstones: spectrum of imaging findings, complications and diagnostic pitfalls. Br J Radiol 86(1028):20120588. https://doi.org/10.1259/bjr.20120588
Funding
Carrie Hoff received unrelated grant funding from NHTSA/CIREN.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Maddu, K., Polireddy, K., Hsu, D. et al. Do not get stumped: multimodality imaging findings of early and late post-cholecystectomy complications. Emerg Radiol 30, 351–362 (2023). https://doi.org/10.1007/s10140-023-02131-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-023-02131-y