Abstract
Bile leak is a well-known complication of cholecystectomy. Endoscopic drainage and decompression of the biliary system including temporary insertion of a biliary stent is generally considered the treatment of choice. We report the successful obliteration of a bile leak using fibered platinum coils placed under fluoroscopic guidance after stent treatment had failed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Bile leak is a recognized complication of endoscopic and open cholecystectomy [1]. Endoscopic intervention is the generally agreed treatment of choice, obviating the need for surgical re-exploration [2]. However, in some situations endoscopic drainage and decompression of the biliary system may not be sufficient. We report a multimodal approach, placing vascular coils via endoscopic access.
Case Report
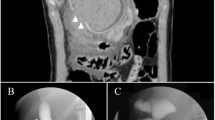
A 77-year-old man received subtotal colectomy because of colonic carcinoma (pT3, N1, M0, R0). Four months later, open cholecystectomy was performed due to acute cholecystitis. During the early postoperative period the patient developed jaundice and an elevation of the plasma bilirubin level. Endoscopic retrograde cholangiography (ERC) on day 6 disclosed insufficiency of the cystic stump, which was treated by temporary stent insertion through the papilla of Vater in the main bile duct. Furthermore, percutaneous drainage of a perihepatic biloma was performed. However, the patient developed high-flow leakage with an output of 800–1,600 ml/day. Follow-up ERCP confirmed persistent, broadly based leakage due to cystic duct insufficiency (Fig. 1A, B).
Fluoroscopy of a multimodal approach in the treatment of a bile leak following cholecystectomy. A, B Endoscopic retrograde opacification of the biliary tree demonstrating leakage from the cystic stump. C Placement of one fibered platinum coil through the working canal of an endoscope under fluoroscopic guidance. D Endoscopic control demonstrating immediate occlusion of the bile leak after placement of two coils.
After removal of the biliary stent a microcatheter (Prograde, Terumo, Tokyo, Japan) was advanced into the remaining cystic stump under fluoroscopic guidance through the working canal of a duodenoscope. Subsequently, two fibered platinum coils (5/50/4; Boston Scientific, Cork, Ireland) were inserted and tightly packed together (Fig. 1C). The leak resolved immediately after coil placement (Fig. 1D). Intravenous antibiotics were given for 10 days due to microbiologically proven Escherichia faecium contamination of the bile. The patient recovered well.
Control-ERCP 2 months later revealed persistent occlusion of the cystic duct. No recurrence of a bile leak was observed during a 1 year follow-up.
Discussion
Postoperative bile leakage is among the most common complications of cholecystectomy and can be observed after laparoscopic (0.9%) as well as in open surgical (2.4%) procedures. The incidence of a leakage increases to 3.2% following laparoscopic cholecystectomy in the case of acute cholecystitis [3]. The severity of bile leaks can be classified by ERCP into low-grade and high-grade, depending on the necessity of intrahepatic opacification for the identification of the leakage [4]. Sandha et al. proposed biliary sphincterotomy alone in low-grade leaks and temporary insertion of a plastic biliary stent in high-grade leaks [4]. Others have proposed percutaneous transhepatic biliary drainage [5] or nasobiliary tubes respectively. The latter can be easily removed and allow access for cholangiographic control imaging [6]. The rationale of drainage is to eliminate intraductal pressure and to divert bile from the site of the leakage in order to allow passive healing.
In cases of failed treatment n-butyl cyanoacrylate (NBCA) has been successfully injected to obliterate bile ducts [7, 8]. Endoscopic embolization with micropledgets has also been described [9]. Tsukamoto et al. percutaneously implanted an expandable metallic biliary endoprosthesis for the treatment of a biliary leakage [10]. Following bile duct disruption due to radiofrequency ablation Thompson et al. successfully inserted a covered metallic stent [11].
Because of the high-output leakage present in our case (Fig. 1A, B) neither injection of NBCA nor a bare metallic stent seemed suitable. We therefore decided to place fibered platinum coils for maximum reduction of bile flow. The mechanism of occlusion is presumably entirely mechanical. Furthermore, the viscous bile may adhere to the coil fibers. The combination of these phenomena probably occluded the cystic duct and led to immediate subsidence of the bile leak. Oliva et al. and Hunt et al. successfully treated biliary fistulas by coil placement [12, 13]. Both proposed percutaneous access. However, when ERCP is technically feasible, as in our case, the endoscopic approach seems to be less traumatic.
To our knowledge only one case of a late complication following coil embolization (due to migration of coils) has been reported in the literature [14]. As this technique has only been used in a small number of patients, the incidence of short- or long-term complications remains unclear. Further studies would seem to be mandatory. However, endoscopic placement of coils may be an important addition to the interventional armamentarium in the treatment of bile leakage.
References
Buanes T, Waage A, Mjaland O, Solheim K (1996) Bile leak after cholecystectomy significance and treatment: Results from the national Norwegian Cholecystectomy Registry. Int Surg 181:276–279
Kaffee AJ, Hourigan L, De Luca N, Byth K, Williams SJ, Bourke MJ (2005) Impact of endoscopic intervention in 100 patients with suspected postcholecystectomy bile leak. Gastrointest Endosc 61:269–275
Prakash K, Jacob G, Lekha V, Venugopal A, Venugopal B, Ramesh H (2002) Laparoscopic cholecystectomy in acute cholecystitis. Surg Endosc 16:180–183
Sandha GS, Bourke MJ, Haber GB, Kortan PP (2004) Endoscopic therapy for bile leak based on a new classification: Results in 207 patients. Gastrointest Endosc 60:567–574
Cozzi G, Severini A, Civelli E, Milella M, Pulvirenti A, Salvetti M, Romito R, Suman L, Chiaraviglio F, Mazzaferro V (2006) Percutaneous transhepatic biliary drainage in the management of postsurgical biliary leaks in patients with nondilated intrahepatic bile ducts. Cardiovasc Intervent Radiol 29:380–388
Elmi F, Silvermann WB (2005) Nasobiliary tube management of postcholecystectomy bile leaks. J Clin Gastroenterol 39:441–444
Vu DN, Strub WM, Nguyen PM (2006) Biliary duct ablation with n-butyl cyanoacrylate. J Vasc Interv Radiol 17:63–69
Kiltz U, Baier J, Adamek RJ (1999) Selective embolisation of a bile leak after operative resection of an echinococcal cyst. Dtsch Med Wochenschr 124:650–652
Krige JEJ, Bornman PC, Beningfield SJ, Nieuwoudt JH, Terblanche J (1990) Endoscopic embolisation of external biliary fistulae. Br J Surg 77:581–583
Tsukamoto T, Hirohashi K, Osugi H, Kubo S, Tanaka H, Shuto T, Takemaura S, Kinoshita H (2002) Percutaneous management of bile duct injuries after cholecystectomy. Hepatogastroenterology 49:113–115
Thompson PhM, Hare ChMB, Lees WR (2004) Bile duct disruption following radiofrequency ablation: Successful repair using covered stent. Cardiovasc Intervent Radiol 27:383–385
Oliva VL, Nicolet V, Soulez G, Falardeau M, Daloze P, Jaoude MA, Carignan L (1997) Bilomas developing after laparoscopic biliary surgery: Percutaneous management with embolisation of biliary leaks. J Vasc Interv Radiol 8:469–473
Hunt JA, Gallagher PJ, Heintze SWDF, Waugh R, Shiel AGR (1997) Percutaneous microcoil embolization of intraperitoneal intrahepatic and extrahepatic biliary fistulas. ANZ J Surg 67:424–427
Sandroussi Ch, Lemech LD, Grunewald B, Abraham N, Gallagher PJ (2005) Late complication following coil embolization of a biliary leak. ANZ J Surg 75:614–615
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schelhammer, F., Dahl, S.v., Heintges, T. et al. A Multimodal Approach in Coil Embolization of a Bile Leak Following Cholecystectomy. Cardiovasc Intervent Radiol 30, 529–530 (2007). https://doi.org/10.1007/s00270-006-0090-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-006-0090-z