Abstract
The authors aimed to conduct a systematic review to assess data from the current literature on the effectiveness of low-level laser therapy (LLLT) in preventing tooth sensitivity (TS) after tooth whitening (DB). PRISMA guidelines for systematic reviews were followed. Clinical trials evaluating the treatment of LLLT in patients with sensitivity after tooth whitening were selected. A full bibliographic search was performed on May 4, 2021, in the following databases: Embase, MEDLINE via PubMed, SciELO, VHL Regional Portal, Web of Science, Gray Literature, Scopus, ClinicalTrials.gov and Cochrane Library. This study followed Cochrane’s recommendations for analyzing risk of bias. A total of 1054 studies were found (255 studies were excluded because they were duplicates and 785 because of titles and abstracts). Only 14 articles were selected for analysis, of which eight were excluded because they had one or more exclusion criteria, resulting in six articles included in this systematic review, the vast majority being classified as low risk of bias. The studies reviewed indicated that LLLT showed promise in preventing TS after TB. However, evidence is limited and more clinical trials with low risk of bias are needed to reach a definitive conclusion on the action of LLLT in pain control after TB.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The mechanism of dental bleaching (DB) involves the degradation of the extracellular matrix and the oxidation of chromophores located precisely in dentin and enamel [1, 2], breaking one or more double bonds of organic chemical dyes that stain teeth [1, 3, 4]. Colour-producing stains within tooth structures are often organic compounds that contain conjugated double bonds. In this way, stain molecules are oxidized into colourless [4], lighter-coloured compounds [1]. It should be taken into account that the time of treatment required to reach the saturation point of DB depends on the exposure time and the concentration of the bleaching compound [1].
However, like any procedure, there are risks that require care. Tooth sensitivity (TS) is the most common clinical consequence resulting from in-office DB [1, 5,6,7,8] performed with 35% H2O2 [8]. This TS usually occurs at the time of treatment and can last for several days [1], followed by mild gingival irritation [1, 5]. Bleaching agents can release substances that lead to changes in cell metabolism and/or inflammation of the dental pulp [2]. Inflammatory mediators released by the penetration of bleaching agents into dental tissues can sensitize nociceptors, leading to TS [9]. The degrees of these side effects are directly related to the concentrations of peroxide, the duration of treatment and the composition of the products used [1].
Recent studies have indicated treatments intended to reduce these effects caused by TS [7, 10,11,12,13]. Likewise, laser therapy has recently been presented as a treatment method for reducing TS after DB [3]. Low-level laser therapy (LLLT) has been increasingly used in various areas of dentistry and medicine [2, 8, 14, 15] for pain reduction [8, 14], due to its analgesic, anti-inflammatory and biostimulant effects [8]. These excellent properties suggest that LLLT may be able to attenuate the damage and inflammation caused in pulp tissue by in-office bleaching agents. Also, it can possibly reduce the risk and intensity of TS due to DB [8], restoring the integrity of the dental pulp after the procedure and promoting, in this way, the regeneration of the injured tissues, mainly for the control of the postoperative symptoms [2].
A previous systematic review assessed the effects of LLLT on dentin hypersensitivity [16]; however, no review was performed addressing TS after DB. Therefore, the present review condensed the existing evidence in order to clarify this important issue. Thus, the goal of the present study was to perform a systematic review in order to assess the effectiveness of LLLT in preventing TS after DB.
Materials and methods
Protocol and registration
The registration protocol for the present study was obtained from the International Prospective Register of Systematic Reviews (PROSPERO 2020, CRD42020206317). The study also followed the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA), stated in the systematic reviews report [17].
Eligibility criteria
In the search strategy, the terms, synonyms and free terms (keywords) of the Medical Subject Heading (MeSH) were defined using the PICO guidelines [18]:
-
1.
Population (P): Patients who underwent DB.
-
2.
Intervention (I): Low-level laser therapy/photobiomodulation.
-
3.
Comparison (C): Control, placebo, or other treatment.
-
4.
Outcomes (O): Primary outcomes: Relief of TS after bleaching; Secondary outcomes: Relief of TS after bleaching over time.
This systematic review only included randomized controlled trials (RCTs) to observe the clinical efficacy of LLLT in preventing ST in permanent teeth of adult patients (men and women) undergoing BD, compared to other desensitization treatments or placebo. In vitro studies, cohort studies, editorial letters, historical reviews and pilot studies, observational studies and descriptive studies such as case reports and case series were excluded.
Information sources
The electronic search was performed to find the articles that would be included in the present review. In order to find all studies published in the area, the search was performed on 4th May 2021 (with an alert requesting recently published articles) in the following databases: Embase; MEDLINE database via PubMed; SciELO; VHL Regional Portal; Web of Science; Gray Literature; Scopus; ClinicalTrials.gov and Cochrane Library. There were no restrictions regarding language or publication dates.
Search strategy
Search strategies were precisely designed for each database (Table 1). The search strategy was reviewed by colleagues experienced in developing and conducting systematic reviews. The identified studies were imported into a reference management software (EndNoteWeb) for automatic removal of duplicates.
Selection process
Titles and abstracts of all studies identified by the search strategy were independently read and reviewed by two authors (AMPC and RPO) to locate eligible studies, and disagreements were resolved by discussion or involving the third reviewer (CMA). The search resulted in full-text versions of studies eligible for evaluation and data extraction. Subsequently, a manual search was performed in the reference lists of the included articles to detect additional relevant studies that had not been found during the searches in the databases. If the articles were found in more than one database, that is, duplicates, they were excluded from one of the databases, so that only one article remained, without repetition. In cases where the same study had different follow-up periods in relation to outcome assessments, only the most recent versions were accepted. Eligible studies were read in full, as well as those that did not contain sufficient information in the titles and abstracts, in order to make a final decision on whether or not to include these studies.
Data collection process
Data from the included articles were independently recorded and recorded in duplicate by two researchers (AMPC and RPO). Reviewers must enter the data in an Excel format spreadsheet (Microsoft Corporation, Redmond, WA, USA).
Data items
Eligible studies were classified by first author’s name and year of publication. Details considered important, such as study designs, participants, interventions and outcomes, were extracted using custom extraction forms. If there were different follow-up periods in the same studies, data extraction would have been performed using longer follow-up periods. When the study did not present data of interest, the authors were contacted by e-mail.
Study risk of bias assessment
The Cochrane Collaboration tool was used by two independent reviewers (AMPC and RPO) to assess the risk of bias in the RCTs. The following items were among the evaluation criteria: sequence generation; allocation concealment; patient blindness; masking the results evaluator; incomplete results data and selective result report. There was no disagreement between reviewers during data selection and assessment of bias. However, if necessary, a third reviewer would help reach consensus (CMA).
Scoring according to the recommendations outlined in the Cochrane Handbook for Systematic Reviews of Interventions 5.1.0 (http://handbook.cochrane.org) was used to assess the risk of bias for each item in the studies and relate to their quality. All items analyzed were considered essential to assess the risk of bias. Therefore, for each item, we chose to record “yes” indicating low risk of bias, “no” indicating high risk of bias and “not clear” indicating lack of information or uncertainty about the potential for bias. Thus, we sought to communicate with the authors in the case of studies considered “unclear” in any of the items, in order to obtain the necessary information for a definitive decision on the study. When at least one of the items was judged to be vague or at high risk of bias, the entire study was conceptualized, respectively, as unclear or at high risk of bias. To classify studies as being of good quality, all items must be at low risk of bias.
Meta-analysis
An attempt was made to perform a meta-analysis to assess the effectiveness of LLLT in preventing TS after DB; however, it was not successfully performed in this systematic review. In order to clarify the reasons, they are specified below:
-
1.
About the sensitivity test data, two studies [12, 19] presented mean and SD for both groups = 0. In the MA software, this finding does not produce any effect size for the study nor lead (obviously) to any result. In addition, another selected study [20] did not present SD.
-
2.
For the questionnaire data, they exhibited the same problem in the analysis of several days (mean and SD for both groups = 0), in addition to the difference in the scales used, and also the difference in the time of laser use between some studies.
-
3.
Due to the high heterogeneity between the studies, greater than 50% (I2 = 87%).
Results
Research-study selection
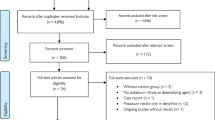
The electronic search performed in the databases (Embase, MEDLINE database via PubMed, SciELO, VHL Regional Portal, Web of Science, Gray Literature; Scopus, ClinicalTrials.gov and Cochrane Library) resulted in 1054 articles. Among these studies, 255 were excluded because they were duplicates, and 785 were excluded after reading the titles and abstracts, either because they used another type of laser or because they addressed other types of treatments, i.e. they did not use LLLT for treating TS after DB. Of the 14 articles selected for analysis, eight were excluded because they were non-randomized clinical studies, had been recorded in Clinical Trials and the Brazilian Registry of Clinical Trials (ReBEC) without the outcomes. This way, the sample for analysis was composed of six studies. The flowchart of the complete study process is illustrated in Fig. 1.
Description of included studies
Table 2 presents data from the six studies selected for the present systematic review, according to the inclusion and exclusion criteria. In order to detail the selected articles with respect to the type of DB, all of them used in-office DB to assess TS [3, 8, 12, 19,20,21]. However, all worked with the same product concentration (35% H2O2) [3, 12, 19,20,21], with the exception of Moosavi et al., who used 40% H2O2 [8], and Dias et al., who, in addition to 35% H2O2, used H2O2 in combination with titanium dioxide with 6% nitrogen (6% H2O2 / TiO2 with N) [20].
Another issue to describe is that some of the selected articles used laser before DB [12, 19, 21], others after [3, 8, 20, 21], and one of the studies used it before and after DB [21]. All studies worked with infrared laser [3, 8, 12, 19,20,21] for controlling TS. However, one study compared low-level infrared laser (LLIL) with low-level red laser (LLRL) to determine which would be the most viable and with the most promising effect in comparison with placebo [8]. Some studies worked with infrared spectrum laser at 808 nm, 60 J/cm2 for 16 s [3, 12, 19], and others at 780 nm, 40 mW, 10 J/cm2 for 10 s [20, 21]. Regarding the study that used both types of lasers, the LLRL was used at 660 nm, 12 J/cm2 for 15 s, and the LLIL at 810 nm, 12 J/cm2 for 15 s [8].
Regarding treatments, Alencar et al. [12] used LLLT associated with fluoride toothpaste (5000 ppm), and compared this procedure with the application of fluoride. De Silva et al. [19] assessed the use of laser in comparison with placebo. De Paula et al. [3] and Dias et al. [20] assessed the laser in isolation, comparing it with a control group. In addition, the first article mentioned also used the laser associated with KNO3 [3]. Moosavi et al. [8] used the two types of lasers (LLRL and LLIL) alone, comparing them with each other and with a placebo group. Finally, Calheiros et al. [21] assessed the laser in isolation and compared the outcomes with those of control and placebo groups.
With respect to the assessment criteria, half of the studies used the modified visual analog scale (MVAS), [3, 12, 19] some used the visual analog scale (VAS) [8, 20], and one study worked with the verbal rating scale (VRS) [21]. The methods of assessments varied between studies. Three studies used only a daily pain questionnaire, in which the patients reported the intensity of the sensitivity they felt [3, 8, 21]. In addition to the daily pain questionnaire, two studies used evaporative stimulus [12, 19], and one study used mechanical and evaporative stimuli [20]. The studies indicated great variation with respect to the assessment periods, i.e. one performed the assessment for 28 days [12], others for 21 days [3, 19], 15 days [21] and 7 days [20], and another for up to 48 h after each bleaching session, which totalled two [8]. Another issue was that most studies used the split-mouth design [3, 12, 19, 20], whereas the minority worked with parallel studies [8, 21].
All studies included were RCTs that compared LLLT with placebo-based treatments or other treatments to treat TS after DB. Only one study did not assess a placebo treatment group [20]. None of the studies reported adverse effects of the treatments used. All publications were written in English.
In this systematic review, most studies were classified as low risk of bias [3, 8, 12, 19]. One of the articles could not be classified due to the lack of information and the unsuccessful attempt to contact the authors by email [20], and another study was classified as high risk [21] (Figs. 2 and 3).
Due to the high heterogeneity in terms of different types, forms and periods of assessments, in addition to the different moments in which lasers were used, two studies [12, 19] had means and SD equal to zero for the groups used, which did not produce any effect size for the studies, and did not refer to any outcome. These two studies also presented the same problem regarding the questionnaire data in the assessment of several days (mean and SD = zero). Furthermore, one of the studies [20] did not report SD, and it was not possible to contact any of the authors for a period of 1 month by means of weekly emails. Therefore, the performance of a meta-analysis with the selected studies was not considered possible.
Discussion
The present systematic review was performed to assess the material provided by the literature about the effectiveness of LLLT in preventing TS after DB. The vast majority of the studies assessed in this qualitative analysis indicated that there was a promising effect of LLLT to treat this condition.
After detailed research on the subject, six RCTs were included for the analysis, given that they had assessed the efficacy of LLLT, alone or in combination with another type of treatment, in the prevention or control of TS caused by the action of DB. The majority of the studies assessed (five) indicated that LLLT had reduced or even avoided TS [3, 8, 12, 19, 20]. On the other hand, one study did not indicate efficient outcomes [21].
LLLT therapy has been widely used to treat this condition, because it is used in many biomedical sciences to promote tissue regeneration. In recent years, many researchers have described several important biological effects associated with LLLT [22]. The term “laser therapy” has been widely referred to the therapeutic effects of lasers. Other terms, such as laser biomodulation, laser bioactivation, laser biostimulation, laser irradiation and laser photostimulation, have often been used instead of laser therapy [15].
Considering TS as a condition caused by the action of DB, the analysis of the studies, addressing the type of DB used, found that all of them had used in-office DB [3, 8, 12, 19,20,21] and worked with the same product concentration (35% H2O2) [3, 12, 19,20,21] with the exception of two studies, one that used 40% H2O2 [8] and another that, in addition to 35% H2O2, used H2O2 in combination with titanium dioxide with 6% nitrogen (6% H2O2 / TiO2 with N) [20]. Even though the literature reports that the available bleaching techniques and agents are effective and have demonstrated similar behaviours [23], in-office DB generates greater intensity of TS [23,24,25].
Bleaching agents are mainly based on hydrogen peroxide (H2O2) or carbamide peroxide (PC), [1, 26, 27] the latter being a stable complex that decomposes in contact with water and releases H2O2. As PC releases H2O2, the chemistry of most tooth whiteners is that of H2O2 [1]. Both bleaching agents (PC and H2O2) can change the inherent colour of teeth; however, different safety and efficacy factors should be taken into consideration [27]. On the other hand, DB is a conservative approach compared to restorative options when tooth discolouration is of great concern. It is also considered to be one of the most conservative and cost-effective dental treatments to improve a person’s smile [27]. This way, the literature has reported DB effectiveness in some clinical trials [23,24,25, 28].
Although the pain and discomfort caused by DB are generally mild and transient, in some cases they can be severe and irritating, leading to the interruption of the bleaching treatment [8]. A previous study concluded that peroxides penetrate the coronal wall of the teeth and enter the pulp chambers in significant amounts, and the greater the concentration of peroxide, the greater the penetration power [26]. In line with this finding, an in vivo study conducted with rats demonstrated that the concentrations of H2O2 influenced the effects on pulp tissue, and higher concentrations of H2O2 could cause necrosis in the pulp and prolonged effect on the apoptotic process. Also, lower concentrations of H2O2 produced moderate inflammation, cell proliferation and apoptosis, with reduction of these processes over time [29]. Likewise, the number of DB sessions directly influenced the extent and intensity of pulp damage, as reported in a study whose findings indicated necrotic tissue in the pulp horns and underlying inflammatory changes after a DB session [30]. After five sessions, changes included necrotic areas in the pulp tissue, involving the second third of the root pulp, and producing intense inflammation in the apical third of rat teeth [30].
According to a previous study, LLLT used with specific parameters was able to compensate for the cytotoxic effects of the bleaching gel, which may have resulted from the maintenance of partial or even total cell viability, or by stimulating the proliferation of surviving cells [2]. The increase in cell activity due to increased metabolism or proliferation in the irradiated groups can be considered a beneficial effect of the therapy, even if these outcomes cannot be extrapolated to in vivo studies [2]. Regarding the moment of laser use, in some studies, the lasers were used before the DB [12, 19, 21], others after [3, 8, 20, 21] and one of the studies used it before and after the DB [21]. In addition, all studies worked with infrared laser [3, 8, 12, 19,20,21] for controlling TS; however, one study used LLIL and LLRL [8], also with different wavelengths of the devices used. The literature does not establish a standard to follow the ideal moment of laser use, as well as the wavelength, which directly depends on the LLLT device used. When we assessed what science made available with respect to the type of laser, the infrared beam was more used to treat not only this condition [3, 8, 12, 19,20,21] but also dentine hypersensitivity [31, 32]. Post-bleaching TS differs from dentine hypersensitivity for being directly related to the penetration of bleaching gel by-products into dentin and pulp tissue through the enamel. This fact causes reversible pulpitis, which results in thermal sensitivity of the teeth, not causing permanent damage to the pulp [33].
Some therapies used did not result in sufficient effects or evidence, as shown by some systematic reviews with meta-analyses, regarding the administration of anti-inflammatory drugs [9, 34] and analgesics for the prevention of TS [34]. In addition, the incorporation of desensitizers in the bleaching gel did not reduce the risk of TS [35]. Likewise, the use of desensitizing gel before or after DB did not reduce the incidence or intensity of TS in RCTs [7]. In opposition to these findings, a meta-analysis indicated that potassium nitrate and sodium fluoride had reduced TS caused by DB [36]. Along the same lines, the application of calcium phosphate [11] and the use of CPP-ACP paste also had a beneficial effect by reducing TS caused by DB [37]. However, despite the range of treatments on the market, a gold standard for treating this condition has not yet been found. The studies assessed used LLLT in different ways; one used LLLT associated with 5000 ppm fluoride dentifrice and compared it with the application only of fluoride dentifrice [12]. Another study assessed the use of laser in comparison with placebo [19]. Two studies assessed the laser alone or in combination with KNO3 in comparison with a control group [3, 20]. One of the studies used two types of lasers in isolation, i.e. LLRL and LLIL, comparing them with each other and with a placebo group [8]. One study assessed the laser in isolation in comparison with control and placebo groups [21]. These different methods are due to the search for the best way to use LLLT to treat TS and determine the gold standard to treat this condition.
Thus, to measure TS after DB, half of the studies used the modified VAS [3, 12, 19], followed by the VAS used by two studies [8, 20] and the VRS [21]. The VAS offers the advantage of being a continuous scale, and has been widely used in clinical studies of dentine hypersensitivity [38,39,40,41,42]. However, despite being the most used method, due to its subjective nature, there has been great variation in the outcomes obtained. With respect to stimuli, three studies used only a daily pain questionnaire, in which the patients reported the intensity of the sensitivity they felt [3, 8, 21]. In addition to the daily pain questionnaire, two studies used the evaporative stimulus [12, 19], and one used mechanical and evaporative stimulation [20]. There are several ways to assess patients’ pain, as indicated by some studies; however, the most common manners were evaporative [38,39,40,41,42,43] and mechanical [38, 39, 41,42,43] stimuli.
In addition, several assessment periods were found, which ranged from a short period, corresponding to 1 week [8, 20], to a long period of treatment [12], i.e. 28 days. However, regardless of the time assessed, the studies found favourable outcomes resulting from the use of LLLT [3, 8, 12, 19, 20]. The literature shows that, in general, in the first hours (24 and 48 h after DB), a lower degree of TS can be observed when LLIL is used, in comparison with another type of laser and placebo, indicating that LLLT should be considered an effective strategy to alleviate the pain and discomfort caused by in-office DB procedures [8].
With respect to study design, most of the selected studies had a split-mouth design [3, 8, 12, 20], which results in smaller and more conservative samples. This way, oral health researchers and statisticians should carefully consider the implications and limitations of this study design in oral health clinical trials, as the effect of transport will be negative on the estimated difference with respect to treatment outcomes. One treatment may affect the response of the other, leading to a conservative estimate of treatment effect in one trial [44]. However, laser is an electromagnetic wave [3, 15] with a monochromatic, coherent and collimated light [15] and there is no consistent evidence that dental laser therapy can produce any systemic effect [3].
Despite the impossibility of performing a meta-analysis, we can observe that the vast majority of studies supported the use of LLLT to treat DB-related sensitivity, even though the number of studies on this topic was scarce. Alencar et al. [12] assessed the efficacy of LLLT associated with the use of 5000 ppm fluoride toothpaste for TS after DB in teeth exposed to 35% H2O2 for 4 weeks. These authors compared that efficacy with the application of the fluoride toothpaste associated with laser simulation, using a daily pain questionnaire for 28 days and evaporative stimulation, through baseline assessment and during the four DB sessions. In both study groups, LLLT and placebo were used before DB, whereas toothpaste was applied after DB. Given the outcomes obtained, the study supported the use of therapy with LLLT in combination with the topical use of 5000 ppm sodium fluoride in each bleaching session, as it demonstrated lower TS in comparison to that caused by the other treatment.
This result is in agreement with those of other studies, such as that conducted by De Silva et al. [19]. These authors found that photobiomodulation was effective in preventing TS after DB with 35% H2O2, in comparison with a placebo group, in which the authors performed the simulation of laser before the DB. They assessed pain through a daily questionnaire, but during a shorter period (21 days) and through evaporative stimulation, with baseline assessment during three DB sessions.
Similarly, De Paula et al. [3] also reached the same conclusion regarding LLLT efficacy, assessing the use of photobiomodulation with low-level laser therapy (PBM-LLLT) combined with 5% potassium nitrate (KNO3) for TS control after in-office DB. In that study, the use of PBM-LLLT occurred after DB, and pain was assessed only through a daily pain questionnaire for a period of 21 days.
Also in accordance with those studies, the literature provides the studies conducted by Dias et al. [20] and Moosavi et al. [8], who also reached the same conclusion. The first study assessed TS by means of evaporative and tactile tests after DB with 35% H2O2 (one session with two 12-min applications) and 6% of H2O2 / TiO2 with N (one session of three 12-min applications), followed by the application of LLLT and control using the split-mouth model, with the tests performed before DB, immediately after, 24, 48, 72 h and 1 week after laser application [20]. The last study used 40% H2O2 and assessed TS after DB with the irradiation LLRL and LLIL, making a comparison between them, and comparing them to the placebo group, registered using a pain questionnaire 1, 24 and 48 h after DB [8].
Contradicting the reported studies, Calheiros et al. used laser in various situations, such as before, after, and before and after DB with 35% H2O2, in addition to using a control and a placebo groups. These authors assessed their patients using a daily pain questionnaire for 15 days, and did not observe any advantage in the use of laser for preventing TS after in-office DB [21]; however, this study was classified as having high risk of bias, which reduced the safety of the outcomes.
Pain is subjective and varies among individuals, which was responsible for the outcomes obtained in the studies selected for this systematic review. Based on an overview of the studies, in which a variety of assessment types was found (some used a questionnaire, others different stimuli), we could observe different periods of assessments, which ranged from 1 week to 28 days. In addition, there were different times of laser use. Some worked with the laser at the initial moment and others after DB. As a result, it was impossible to perform a meta-analysis to better determine the action of LLLT. This fact was a limitation of the present study.
Thus, this systematic review sought to assess the real evidence of the use of LLLT for treating TS caused by DB, since the literature did not provide any review on this subject. However, despite the fact that it was not possible to perform a meta-analysis, the present study may have probably been able to clarify the action of LLLT in the treatment of TS caused by DB, in order to prevent the discomfort caused. Further studies on this subject should be conducted with an assessment standard, for a better interpretation of the outcomes, since high heterogeneity was observed in the studies assessed.
Conclusion
The literature indicates that LLLT has a promising effect in preventing post-bleaching sensitivity. However, evidence is still very limited, and further clinical studies with a high standard of methodological assessment are needed in order to reach an adequate conclusion on the topic addressed in the present study.
References
Clifton MC (2014) Tooth whitening: what we now know. J Evid Based Dent Pract 14:70–76
Dantas CMG, Vivan CL, Ferreira LS et al (2010) In vitro effect of low intensity laser on the cytotoxicity produced by substances released by bleaching gel. Braz Oral Res 24:460–466
De Paula B, Alencar A, Ortiz M et al (2019) Effect of photobiomodulation with low-level laser therapy combined with potassium nitrate on controlling post-bleaching tooth sensitivity: clinical, randomized, controlled, double-blind, and split-mouth study. Clin Oral Investig 23:2723–2732. https://doi.org/10.1007/s00784-018-2715-4
Kwon SR, Wertz PW (2015) Review of the mechanism of tooth whitening. J Esthet Restor Dent 27:240–257. https://doi.org/10.1111/jerd.12152
Haywood VB, Sword RJ (2017) Tooth bleaching questions answered. Br Dent J 223:369–380. https://doi.org/10.1038/sj.bdj.2017.767
Kielbassa AM, Maier M, Gieren AK et al (2015) Tooth sensitivity during and after vital tooth bleaching: a systematic review on an unsolved problem. Quintessence Int 46:881–897. https://doi.org/10.3290/j.qi.a34700
Martini EC, Parreiras SO, Szesz AL et al (2020) Bleaching-induced tooth sensitivity with application of a desensitizing gel before and after in-office bleaching: a triple-blind randomized clinical trial. Clin Oral Investig 24:385–394. https://doi.org/10.1007/s00784-019-02942-9
Moosavi H, Arjmand N, Ahrari F et al (2016) Effect of low-level laser therapy on tooth sensitivity induced by in-office bleaching. Lasers Med Sci 31:713–719. https://doi.org/10.1007/s10103-016-1913-z
Faria ESAL, Nahsan FP, Fernandes MT et al (2015) Effect of preventive use of nonsteroidal anti-inflammatory drugs on sensitivity after dental bleaching: a systematic review and metaanalysis. J Am Dent Assoc 146:87–93. https://doi.org/10.1016/j.adaj.2014.10.007
Parreiras SO, Szesz AL, Coppla FM et al (2018) Effect of an experimental desensitizing agent on reduction of bleaching-induced tooth sensitivity: a triple-blind randomized clinical trial. J Am Dent Assoc 149:281–290. https://doi.org/10.1016/j.adaj.2017.10.025
Mehta D, Jyothi S, Moogi P et al (2018) Novel treatment of in-office tooth bleaching sensitivity: a randomized, placebo-controlled clinical study. J Esthet Restor Dent 30:254–258. https://doi.org/10.1111/jerd.12374
Alencar CM, De Paula BLF, Araújo JLN et al (2018) Effect of low-level laser therapy combined with 5000 parts per million fluoride dentifrice on postbleaching sensitivity: a clinical, randomized, and double-blind study. J Esthet Restor Dent 30:352–359. https://doi.org/10.1111/jerd.12386
Alexandrino LD, Alencar CM, Silveira ADSD et al (2017) Randomized clinical trial of the effect of novamin and CPP-ACPF in combination with dental bleaching. J Appl Oral Sci 25:335–340. https://doi.org/10.1590/1678-7757-2016-0408
Yıldız ED, Arslan H (2018) Effect of low-level laser therapy on postoperative pain in molars with symptomatic apical periodontitis: a randomized placebo-controlled clinical trial. J Endod 44:1610–1615. https://doi.org/10.1016/j.joen.2018.07.002
Reddy GK (2004) Photobiological basis and clinical role of low intensity lasers in biology and medicine. J Clin Laser Med Surg 22:141–150. https://doi.org/10.1089/104454704774076208
Rezazadeh F, Dehghanian P, Jafarpour D (2019) Laser effects on the prevention and treatment of dentinal hypersensitivity: a systematic review. J Lasers Med Sci 10:1–11. https://doi.org/10.15171/jlms.2019.01
Moher D, Liberati A, Tetzlaff J et al (2010) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 8:336–341. https://doi.org/10.1016/j.ijsu.2010.02.007
Maia LC, Antonio AG (2012) Systematic reviews in dental research A guideline. J Clin Pediatr Dent 37:117–124. https://doi.org/10.17796/jcpd.37.2.h606137vj3826v61
De Silva CC, Alencar CM, de Paula BLF et al (2020) Photobiomodulation vs. placebo on post-bleaching sensitivity and color change: a split-mouth clinical study. Open dent J 14:267–274. https://doi.org/10.2174/1874210602014010267
Dias HB, Carrera ET, Bortolatto JF et al (2016) LED and low level laser therapy association in tooth bleaching using a novel low concentration H2O2/N-doped TiO2 bleaching agent. Laser Phys 26:15–60. https://doi.org/10.1088/1054-660X/26/1/015602
Calheiros APC, Moreira MS, Gonçalves F et al (2017) Photobiomodulation in the prevention of tooth sensitivity caused by in-office dental bleaching. A randomized placebo preliminary study. Photomedicine Laser Surg 35:415–420. https://doi.org/10.1089/pho.2017.4282
Silveira PC, Streck EL, Pinho RA (2007) Evaluation of mitochondrial respiratory chain activity in wound healing by low-level laser therapy. J Photochem Photobiol B 86:279–282. https://doi.org/10.1016/j.jphotobiol.2006.10.002
Mondelli RF, Azevedo JF, Francisconi AC et al (2012) Comparative clinical study of the effectiveness of different dental bleaching methods-two year follow-up. J Appl Oral Sci 20:435–443. https://doi.org/10.1590/S1678-77572012000400008
Tay LY, Kose C, Herrera DR et al (2012) Long-term efficacy of in-office and at-home bleaching: a 2-year double-blind randomized clinical trial. Am J Dent 25:199–204
Mounika A, Mandava J, Roopesh B et al (2018) Clinical evaluation of color change and tooth sensitivity with in-office and home bleaching treatments. Indian J Dent Res 29:423–427. https://doi.org/10.4103/ijdr.IJDR_688_16
Gokay OM, Ujdeci A, Algn E (2004) Peroxide penetration into the pulp from whitening strips. J Endod 30:887–889
American DA (2009) Council on Scientific Affairs, Tooth whitening/bleaching: treatment considerations for dentists and their patients, 3ª. ADA Council on Scientific Affairs, Chicago, pp 230–257
Zekonis R, Matis BA, Cochran MA et al (2003) Clinical evaluation of in-office and at-home bleaching treatments. Oper Dent 28:114–121
Benetti F, Gomes-Filho JE, Ferreira LL et al (2017) Hydrogen peroxide induces cell proliferation and apoptosis in pulp of rats after dental bleaching in vivo. Arch Oral Biol 81:103–109. https://doi.org/10.1016/j.archoralbio.2017.04.013
Cintra LT, Benetti F, Facundo ACS et al (2013) The number of bleaching sessions influences pulp tissue damage in rat teeth. J Endod 39:1576–1580. https://doi.org/10.1016/j.joen.2013.08.007
Narayanan R, Prabhuji MLV, Paramashivaiah L et al (2019) Low-level laser therapy in combination with desensitising agent reduces dentin hypersensitivity in fluorotic and non-fluorotic teeth - a randomised, controlled, double-blind clinical trial. Oral Health Prev Dent 17:547–556. https://doi.org/10.3290/j.ohpd.a43567
Lopes AO, Eduardo CP, Aranha ACC (2017) Evaluation of different treatment protocols for dentin hypersensitivity: an 18-month randomized clinical trial. Lasers Med Sci 32:1023–1030. https://doi.org/10.1007/s10103-017-2203-0
Roberts RB (1991) Passive tooth bleaching: the cosmetic revolution. 2ª ed. Chicago, La Mesa: R.B. Roberts, 19–91.
Santana MLC, Leal PC, Reis A et al (2019) Effect of anti-inflammatory and analgesic drugs for the prevention of bleaching-induced tooth sensitivity. J Am Dent Assoc 150:818–829. https://doi.org/10.1016/j.adaj.2019.05.004
Rezende M, Coppla FM, Chemin K et al (2019) Tooth sensitivity after dental bleaching with a desensitizer-containing and a desensitizer-free bleaching gel: a systematic review and meta-analysis. Oper Dent 44:E58–E74. https://doi.org/10.2341/17-253-L
Wang Y, Gao J, Jiang T et al (2015) Evaluation of the efficacy of potassium nitrate and sodium fluoride as desensitizing agents during tooth bleaching treatment—a systematic review and meta-analysis. J Dent 43:913–923. https://doi.org/10.1016/j.jdent.2015.03.015
Yassin O, Milly H (2019) Effect of CPP-ACP on efficacy and postoperative sensitivity associated with at-home vital tooth bleaching using 20% carbamide peroxide. Clin Oral Investig 23:1555–1559. https://doi.org/10.1007/s00784-018-2574-z
Madruga MM, da Silva AF, da Rosa WLO et al (2017) Evaluation of dentin hypersensitivity treatment with glass ionomer cements: a randomized clinical trial. Braz Oral Res 31:3. https://doi.org/10.1590/1807-3107BOR-2017.vol31.0003
Parkinson C, Constantin P, Goyal C (2017) An exploratory clinical trial to evaluate the efficacy of an experimental dentifrice formulation in the relief of dentine hypersensitivity. J Dent 56:39–44. https://doi.org/10.1016/j.jdent.2016.10.013
Wang L, Magalhães AC, Francisconi-Dos-Rios LF et al (2016) Treatment of dentin hypersensitivity using nano-hydroxyapatite pastes: a randomized three-month clinical trial. Oper Dent 41:E93–E101. https://doi.org/10.2341/15-145-C
Gopinath NM, John J, Nagappan N et al (2015) Evaluation of dentifrice containing nano-hydroxyapatite for dentinal hypersensitivity: a randomized controlled trial. J Int Oral Health 7:118–122
Vano M, Derchi G, Barone A et al (2018) Reducing dentine hypersensitivity with nano-hydroxyapatite toothpaste: a double-blind randomized controlled trial. Clin Oral Investig 22:313–320. https://doi.org/10.1007/s00784-017-2113-3
Torwane NA, Hongal S, Goel P et al (2013) Effect of two desensitizing agents in reducing dentin hypersensitivity: an in-vivo comparative clinical trial. J Clin Diagn Res 7:2042–2046. https://doi.org/10.7860/jcdr/2013/6005.3401
Pihlstrom BL, Barnett ML (2010) Design, operation, and interpretation of clinical trials. J Dent Res 89:759–772. https://doi.org/10.1177/0022034510374737
Funding
We have to thank the Coordination for the Improvement of Higher Education Personnel (CAPES) for the support and the National Council for Scientific and Technological Development (CNPq) under no 130961/2019–1.
Author information
Authors and Affiliations
Contributions
Alexandra Melo Pingarilho Carneiro was the principal investigator and an important contribution to the conceptual framework, data collection, data entry, manuscript writing and bibliographic research. Antonia Patricia Oliveira Barros and Roberta Pimentel de Oliveira were co-researchers assisting in the selection of the title, conceptual structure, study design, manuscript writing and data analysis. Aryvelto Miranda Silva and Brennda Lucy Freitas de Paula were co-researchers assisting in data acquisition and writing of the article. Cristiane de Melo Alencar and Cecy Martins Silva were co-investigators and a major contributor to statistics and critical review of important intellectual content. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Carneiro, A.M.P., Barros, A.P.O., de Oliveira, R.P. et al. The effect of photobiomodulation using low-level laser therapy on tooth sensitivity after dental bleaching: a systematic review. Lasers Med Sci 37, 2791–2804 (2022). https://doi.org/10.1007/s10103-022-03578-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-022-03578-0