Abstract
Hyperthermia is an anti-cancer treatment in which the temperature of the malignant tumor is increased more than other adjacent normal tissues. Microwave, ultrasound, laser, and radiofrequency sources have been used for hyperthermia of cancerous tissues. In the past decade, near-infrared (NIR) laser for cancer therapy, known as photo-thermal therapy (PTT), was expanded in which the photo-sensitizer agent converts the light photon energy to heat. The heat following PTT can destroy cancer cells. There are some photo-sensitizer agents which have been used for PTT; however, owing to recent advances in nanotechnology, noble metal nanoparticles like gold (Au) nanoparticles (GNPs) have been used successfully in PTT. GNPs have some desirable specifications, including simple and controlled synthesis, small size, high level of biocompatibility, and surface plasmon resonance (SPR). The SPR effect of the GNPs increases the radiative properties like absorption and scattering; therefore, they can be used in PTT. In this article, we reviewed recent in vitro studies of PTT using GNPs in literature. At first, we focus on the physical properties of GNPs, their interaction with infrared radiation, and physical parameters governing the interaction of infrared radiation with the GNPs. Then, we review the passive and active targeting of GNPs using the different coating to induce the thermal damage in cancer cells using low-level laser PPT. The GNPs’ cellular internalization into cancer cells is a challenge which is consequently considered. In this review, we also summarize the results of synergistic cancer therapy studies on the combination of radiation therapy as a routine cancer treatment and PTT: in which significant improvement occurs in treatment efficacy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Photo-thermal therapy (PTT) is a non-invasive and relatively new method of cancer treatment [1]. In PTT, the absorbed light turns into heat and cancer cells are destroyed due to their high temperature, which results in photoablation followed by cell death [2]. PTT is simply functional and has a great potential to improve the recovery time and providing a better output of cancer treatment [3]. It also reduces the cure complexity and time spent on treatment [1].
Studies have shown that the temperature over 40 °C causes irreversible damage to proteins and an inefficiency of DNA double-strand break repair [4, 5]. Other studies have shown that increasing temperature to 43 °C destroys cancer cells due to lack of glucose [1]. PTT includes enhancing the cancer cell temperature in the range of 42–46 °C in which most of the structures and enzymatic proteins change and eventually causes cell death [6, 7]. In addition to the low thermal threshold of the cancer cells [7], low pH and hypoxic conditions in cancer cells make them more vulnerable to PTT compared to normal cells [8].
Different sources, including laser, microwave, ultrasound, and radiofrequency waves, have been studied for PTT [3, 9]. Damage to normal cells surrounding the tumor limits use of conventional sources of heat production [10]. Low absorption of radiation in tumors is another limitation on the use of these sources; for example, radiofrequency waves have less absorption with gold nanoparticles (GNPs) [11]. On the other hand, PTT by laser has advantages like reduced expense, fewer side effects, and suitable wavelength for biological applications [6, 12]. The use of two windows of laser for PTT results in minimum absorption in the peripheral tissues: the first window at the wavelength range of 650–940 nm corresponds to near-infrared (NIR) region, and the second window is in the range of 1000–1350 nm called infrared (IR) region [3]. In the first window, absorption and scattering of the light take place in water molecules which leads to the higher efficiency of penetration of the radiation [4]. However, PTT with NIR wavelengths has disadvantages such as limited penetration for deep tumors (deeper than 3–5 cm) [4, 11]. Enhancing the laser power results in more reduction in the normal cells’ viability [10] as well as an inhomogeneous and non-selective distribution of the heat especially in deep tumors [13]. Nanotechnology in medicine plays an important role which can aid to solve these problems [14].
Gold nanoparticles in PTT
The efficacy of PTT has been improved by nanotechnology [15, 16]; in which different nanoparticles (NPs) have been used as intermediary for converting the light to heat and consequently local temperature enhancement [4, 17,18,19]. NPs used in thermal therapy have mainly included two categories: (1) thermal-magnetic NPs; these NPs under an alternating magnetic field with high frequency are involved in heat production. (2) Thermal-light NPs; in PTT using these NPs, the light turns into heat by the plasmonic effect of the NPs [3, 20]. Among the various non-organic plasmonic nanoparticles, GNPs possess unique properties such as large surface to volume ratio, simple synthesis, and low toxicity or high biocompatibility [8] which have been widely used in nanomedicine researches [14, 18]. It is possible to adjust maximum absorption spectrum of the GNPs in the NIR region by modifying their size and shape [21]. Therefore, GNPs can be effectively used to absorb NIR light and efficiently transform into heat in PTT [8, 21, 22]. In addition, plasmonic GNPs have considerable thermal stability and good pre-clinical tolerance without significant side effects [8]. GNPs can more aggregate in cancer cells through a passively accumulation in tumors because of the enhanced permeability and retention (EPR) effect [23]. This phenomenon occurs, since administrated NPs can leak out from tumor blood vessels, but not from normal vessels. Tumor blood vessels possess a high number of pores; hence, when NPs are injected into the bloodstream, they could extravasate through these pores and aggregate in the tumor interstitial fluid [24]. Due to the fast growth of tumor cells, they have ineffective lymphatic drainage. Therefore, the extravasated NPs can retain within the tissue for long times [25]. The higher level of the NPs in tumor cells compared to the normal cells provides an enhancement of radiation absorption in them; consequently, an effective treatment with fewer side effects occurs [2, 17, 22].
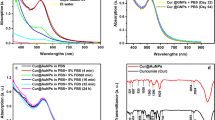
The mechanism of treatment PTT by GNPs includes the collision of laser radiation to GNPs and electron excitation of the NPs; then during energy redistribution, the electrons reach to new equilibrium Fermi electron distribution [17]. Hot electrons give their energy to the lattice and through phonon-phonon scattering, heat is transferred to the environment in picoseconds, and GNPs are rapidly getting cold [17, 26, 27]. In other words, as a result of excitation, fast local heat is generated [18]; hot electron temperature rises to thousands of degrees Kelvin and lattice temperature reaches to 10° when GNPs irradiated by NIR [26]. This property makes GNPs suitable for cancer treatment through PTT [26]. In fact, a low-power laser can be used in GNP-mediated PTT in which damage in surrounding normal tissue and consequent side effects in normal cells decrease while cancer cell death increases [2, 10, 28]. Due to changes in temperature, different physical and biological responses take place depending on the laser power which include phase alteration in lipid membrane that followed by membrane melting in nanoscale, denaturation of the proteins surrounding GNPs, fast melting of DNA, releasing molecules of the GNPs surface, and evaporation of water around the nanoparticles [17]. Figure 1 shows the combination of the unique properties of GNPs with PTT which causes cancer cell death.
PTT efficacy using GNPs depends on several factors [17], e.g., size of the GNPs is an important factor, so that increasing the GNPs’ size reduces the ability of converting light into heat and as a result, the efficiency of PTT is decreased [29]. In another study, the comparison between the gold-silica nanoshells with different thicknesses of gold revealed that GNPs with a higher thickness of gold exhibited a stronger absorption band but the lower heat therapeutic effect [30]. The second factor is the distribution of laser flux; it has been shown that some parameters including duration and intensity of laser influence on the cell death in PTT [10]. Also, lasers in pulsed mode (and especially with a high pulse energy) can be associated with strong heating effects which can have many consequences. The pulsed laser with short pulse duration relative to continuous wave lasers delivers a greater amount of energy to tissue [10]. Also, due to heat transfer to water, pulsed lasers cause the phase change in the water, and therefore, bubbles are formed in the biological system [17]. It has been reported that bubbles are significantly formed by GNPs irradiated with pulsed laser in the cytoplasm [10]. Therefore, use of pulsed lasers in the presence of GNPs has the advantage, so that one can reduce the pulse laser energy while having the same effects [17].
Studies have shown a positive relationship between laser power density and cellular dysfunction in which cell death rate increases with increasing the laser power density [4]. Although the PTT effect of high-energy laser irradiation is highly considerable, it also causes non-specific cell killing [30]. These results indicate the importance of choosing the appropriate power to minimize damage in the normal tissue adjacent the tumor. The laser power is suitable if it will be less than the skin tolerance threshold. To fulfill this aim, the maximum exposure can be applied to the skin at a wavelength in the range of 808–980 nm, is about 330–350 mW/cm2 with a radiant time of 10 to 100 s [20]. The power of lasers used in PTT studies is less than the threshold level of cell damage [22]. The laser irradiation time is also another effective parameter, so that increasing the infrared radiation time increases the temperature and consequently cell killing is increased [30].
The fourth factor which affects on the efficacy of GNPs-mediated PTT is the amount of GNPs within the cancer cells [10, 15, 30]. Some parameters such as the GNPs’ size, morphology, and surface modification as well as incubation time can alter the amount of internalized GNPs into the cancer cells [1, 3, 31, 32]; for example, increasing the incubation time of GNPs with cancer cells increases the GNPs’ internalization into the cells and therefore increases the efficiency of thermal therapy [6]. The parameters used in GNPs-mediated PTT in some in vitro studies and also their results are tabulated in Table 1.
Coating the GNPs for PTT
Nanoparticles used in PTT are mainly composed of two parts: (1) the core, which acts as a heat-to-light conversion agent; (2) the peripheral part that is responsible for stability of the NPs in complex physiological environments; also loading the targeting agents on the NPs increases their identification and consequently their uptake by cancer cells [29]. Although GNPs can passively, without targeting agent on their surface, accumulate in cancer cells [1, 22], they have a non-specific connection with the cells’ membrane [35, 36]. Due to the GNPs accumulation in normal cells, an undesirable damage associated with non-targeted GNPs can be increased [37]. Therefore, without the differential effect of the GNPs’ uptake between tumoral and normal tissues, effective treatment of the tumor is not achievable through PTT [21]. Targeted GNP is the best strategy for having more effective and also selective treatment with minimal side effects as well as reducing the laser power and consequently increasing safety in NP-mediated PPT [29, 30].
Due to the surface characteristics of GNPs, it is possible to connect through the thiol (-SH) and amine (-NH2) groups [20, 38] for various ligands such as antibodies, peptides, nucleic acid aptamers, and small molecules with the aim of identifying and connecting to a particular cell [1,2,3,4]. The ligands have good biocompatibility after binding to the GNPs surfaces [32] and sustain their biological activity [31, 32]. Therefore, by active targeting, bounded ligands to the GNP surface increase their concentration on a specific cell membrane [32]. For example, using GNPs bounded to the CD44 agent under irradiation with NIR light, a significant therapeutic effect has been shown in comparison to naked GNPs [4]. It has been reported that conjugating an appropriate targeting agent to the surface of GNPs, the therapeutic efficacy of PPT can be five times greater than without conjugation [29]. Other recent studies have confirmed the role of binding GNPs with specific biological molecules for active targeting of cancer cells [7, 39,40,41].
Different agents have been used for surface modification of GNPs: one of them is polyethylene glycol (PEG); PEGylation of GNPs surface not only increases their hydrophilicity but also as a passive targeting [4] improves their biocompatibility [12, 21]. Folic acid (folate) is used as an active targeting agent and widely used to help in detection of cancer cells [16, 41]; it is a water-soluble vitamin and non-immunogenic agent [42]. Some cancer cells in ovarian, fallopian tube, kidney, lung, and thyroid cancerous tissues tend to overexpress the folate receptors (about ten times more than the normal cells) on their cell membrane; folate serves as a co-factor in the synthesis of nucleic acid and amino acids [40]. By targeting the folate receptors on the surface of such cancer cells, normal cells can be protected from damage of PTT due to the differential effect of uptake in them [42].
Aptamer is a targeting agent that can be attached to the surface of the GNPs by the thiol group [43]. The aptamer is an oligonucleotide of DNA or RNA, which can be attached to specific cell membrane proteins with a three-dimensional structure [31]. The aptamer is chemically synthesized in an in vitro environment through the SELEX (Systematic Evolution of Ligands by EXponential Enrichment) method [43]. Advantages of using aptamer as a targeting agent are its simple synthesis, small size, ease of modification, alteration, and storage [6]; due to these advantages, some other targeting agents such as antibodies have been replaced by aptamer in recent years [28]. Therefore, these specifications have made aptamer suitable for active targeting of cancer cells [6]. Aptamer has been also used to detect low-density cancer cells with a high sensitivity [31]. The high affinity of aptamers for binding to the GNPs’ surface is the other advantage [28], in which high level of ligand density increases the therapeutic efficacy [29].
Conjugating NPs with antibodies provides an effective and selective targeting [35]. Accumulation of antibody conjugated GNPs in cancer cells causes these cells to be sensitive to PTT [7]. Antibodies have specific binding to cancer cells; also by blocking the signal path, they kill the cancer cells [30]. Despite the specific antibody binding to the cancer cell, they can potentially be immunogenic [28]. Large hydrodynamic size of antibody-conjugated NPs reduces their cellular uptake [28, 44].
Peptides, short polymeric amino acid sequence, can be used for identifying specific cells [44]. Less immunization, high biocompatibility, and more internalization into cells are the advantages of peptides over antibodies [1, 45]. A study has shown that GNPs conjugated with peptides effectively reduce cancer cell survival in PTT [31].
Cellular uptake of GNPs for PTT
In addition to the advances in developing appropriate GNPs, their destination for treatment, as a determinative factor in light to heat conversion efficiency, needs to be investigated [3]. The therapeutic effects of GNPs depend on their location inside or outside of cells [46]. GNPs can either remain on the cell surface or induce biological responses through different cellular uptake pathways. The cell membrane is the main barrier to entering the GNPs into the cell [17]. Damage to the cell membrane through the PTT is a non-invasive and irreversible technique for destroying the cancer cells [10, 31]. It also has been demonstrated that for photo-thermolysis induction, GNPs attached to the cells’ membrane need lower laser power than the internalized GNPs into the cells [17, 31]. On the other hand, it has been shown that cancer cells just are damaged due to the presence of GNPs in the cells’ membrane, for which GNPs cannot enter the cells through endocytosis; while the necrotic process occurs during PTT by their entrance into the cells [10]. Another advantage of entrancing the GNPs into cancer cells in PTT is reducing the side effects, because it reduces the need for high amounts of GNPs [47]. Therefore, investigating the intracellular events may help for better understanding of the GNP-mediated PTT mechanism.
NPs endocytosis is mainly accomplished with the phagocyte mechanism, which is an energetic process and non-phagocytic mechanisms (pinocytosis) which include several mechanisms such caveolae-mediated endocytosis [48]. Therefore, the mechanism of the NPs’ entrance into cells may be different in different cells. Also, cancer cells have a higher capacity for endocytosis due to their high metabolic activity compared to normal cells [49]. The internalization of NPs into cells plays a major role in causing cytotoxicity and therefore irreversible damages [17, 18]. The internalization potential of GNPs into a cell depends on several factors [48] including the GNPs’ size, shape (morphology), surface modification, concentration, the time duration that GNPs are exposed to the cancer cells as well as cell type and ligand type [17, 39, 49,50,51]. The NPs’ size is an important factor which affects on their cellular uptake, intracellular distribution, and cytotoxicity [52]. Also, it has been shown that cellular responses to PTT depend on the size of NPs; a comparison between different sizes of the spherical GNPs has revealed that the size of 50 nm has the greatest efficiency in entering into the cell [17, 49]. Different shapes of NPs show the different level of interaction with the cells’ membrane and consequently a different cellular uptake occurs [18]. The positive charge on the NPs’ surface increases the cellular uptake due to electrostatic interactions with cell surface [29, 47, 49]. Adding ligand on GNPs surface may increase the positive charge on the NP surface [31]. So that the NPs’ internalization into the cells increases. In addition, to increase the stability of NPs, PEGylation also increases cellular uptake [14, 22]. Also, functionalized NPs can connect to receptors on the membrane surface and usually enter into the cells through the receptor-mediated endocytosis [37, 53]. Cellular uptake also depends on the incubation time of the cells with NPs as well as the kind of cell [22, 47, 51]. Probably, the longer the GNPs are incubated, the more NPs will enter the cell [46]. These properties also affect the intracellular location of NPs [18]. Use of high-intensity laser can increase the cells’ membrane permeability so that more GNPs could enter into the cells [17].
Cellular uptake of GNPs is prerequisite for GNP-mediated PTT using NIR light, and also targeting the specific intracellular organelles can improve the PTT efficacy [41]. If GNPs accumulate in the subcellular components, the mechanical damage and consequently the efficacy of PTT will increase [47]. Targeting the lysosomes and mitochondria as two intracellular organelles plays a key role in the induction of cell apoptosis [46]. As mentioned, functionalized GNPs can connect to the cells’ surface receptors, and the receptor-mediated endocytosis process occurs [39]. The formed endosome can eventually be merged with lysosomes [53]. Lysosome has acidic pH and various hydrolytic enzymes, which is a stable environment for GNPs [48]. In common practice, stability in the lysosome membrane of normal cells prevents lysosomal damage in the presence or absence of GNPs [46]. While the lysosomal membrane of cancer cells is relatively vulnerable, and as a result of its degradation by GNPs, hydrolytic materials release and may be transmitted to other organelles such as mitochondria [46]. By accumulation of GNPs in lysosomes, the production of hydrolytic enzyme increases which leads to increase in lysosomal activity and eventually results in rupture of the lysosomal membrane [52, 53].
Mitochondria, as the main site of energy production [19, 47], is an appropriate target for cancer treatment [54]. Cancer cells have shown an extensive metabolic activity, resulting in mitochondrial damage compared to normal cells [27]. NIR excites GNP electrons, and consequently, the phonon-phonon mechanism interacts with the mitochondria electron transfer chain [27]. Therefore, the mitochondria encounter oxygen deficiency [27]. This reduction in oxygen level and the other GNPs’ effects on mitochondria, including the release of enzyme cytochrome c and active oxygen species, activate apoptosis in the cell [46, 47]. In other words, GNPs can cause heat deterioration during PTT via local accumulation in mitochondria [47]. The remaining problems in mitochondrial treatment are cavities smaller than 2 nm in the mitochondrial internal membrane which prevent the GNPs’ cellular uptake to the mitochondrial matrix [47, 54]. A study [46] has investigated the mechanism of apoptosis in cancer cells in the presence of GNPs and has demonstrated that unlike lysosomes, only a small number of GNPs were participated in mitochondrial damage. This non-selective accumulation showed that GNPs could not directly participate in damage to the mitochondria; thus, the damage may be due to lysosomal protease [46]. It has been reported that GNPs with some specific ligands [54] move toward lysosomes and other ligands make GNPs move toward the mitochondria; in other words, surface ligands of GNPs play an important role in the movement of NPs within cells.
Since the cell nucleus is important organelle respect to others within the cells for survival and proliferation, so that considering the GNPs’ effect on the nucleus is essential [55], and can be selected as a suitable target for GNPs-mediated PTT. As mentioned before, the GNPs firstly are localized in other organelles including endosomes and lysosomes after internalized into the cells. So, they have to escape from these organelles into the cytoplasm to enter the nucleus [56]. Also, the size of the transport channels of the nuclear pore complex (NPC) has to be considered if GNPs are destined to the nucleus [47]. The number of NPCs varies depending on the activity level of a cell [56] and also the nuclear transport machinery is often altered in different cancer cells, there is no standard protocol for the NPs’ internalization into the nucleus in different tumoral cells [47]. However, the internalization mechanism is not yet well known, the GNPs can alter the nuclear morphology, reorganize nuclear laminae, and finally inhibit nuclear functions; In particular, they can reduce the subnuclear compartments that produce ribosomes [55]. It has been reported that PTT can further increase some of these results so that cancer cell death will be increased [55].
Synergistic effect of photo-thermal therapy and radiation therapy
Although PTT has been widely used as a single treatment [4], it is hard to eradicate the tumor with minimal side effects only by PTT even with optimized NPs [15]. In order to cancer treatment, PTT can stop cell proliferation through cell destruction, or overly sensitize them for other therapies [7]. Drug delivery, drug release, and radiation therapy (RT) are examples of these treatments [4].
New therapeutic approaches in which PTT is used along with other treatments, the treatment output has been improved and the recurrence rate of the tumor has been reduced [4]. PTT has been used as an adjunct to RT in cancer treatment [13]. Ionizing radiation produces free radicals that can damage macromolecules such as DNA, proteins, etc. in irradiated cells [12, 23] which results in cancer cell death [37]. The main goal of RT is to deliver a lethal dose to the cancer cells while minimizing exposure to adjacent normal cells [12, 36, 57]. Various factors can affect RT efficacy [5]. Using radiation sensitizers in cancer cells during RT can increase the effectiveness of RT without increasing the absorbed dose of normal cells [23].
PTT can be used with RT to increase the effectiveness of cancer treatment; in this regard, studies have tried to develop proper NPs as an optical absorption agents to have the necessary efficacy in PTT and also as radiation sensitizers agents to improve the RT efficacy [4, 12, 13]. According to former studies, GNPs and especially functionalized GNPs are the best candidates for this purpose; they are suitable radiosensitizers in RT [9, 36, 41, 58, 59] and also increase the light absorption in cancer cells in PTT [4, 23]. As mentioned previously, heat is generated due to absorption of NIR radiation by GNPs [17] and is transferred to the environment [27]. Moreover, when GNPs are irradiated in RT, they can increase the microscopic absorbed dose [58]; as a result, the delivered dose to tumoral tissue is increased using GNPs. In vitro studies have reported the synergistic effect of RT and PTT using GNPs for cancer treatment [4, 5, 12]. Table 2 shows that the combination of PTT and RT in the presence of GNPs significantly reduces the cell survival rate in comparison with PTT or RT alone.
RT has low efficiency in destroying hypoxic cells so that hypoxia is a major limitation in RT [12]. Hypoxia by eliminating the effect of oxygen [57] induces resistance to ionizing radiation in the hypoxic cells [36]. Cancer cells are more sensitive to high temperature in hypoxia condition [58]; also, use of PTT in a combination therapy improves the oxygen level of tumor [5]. As a result, hypoxic cells of the tumor are sensitized to ionizing radiation [12]. Cell cycle has been used to demonstrate the synergistic effect of RT and PTT [13]. RT considerably kills the tumoral cells in G2/M phase, which is a sensitive phase of the cell cycle to ionizing radiation [5] and has the least effect in S phase in which the cells have lower radiosensitivity [23]. On the other hand, PTT mainly affects cells in the S phase and results in a concentration of cells in the G2/M phase by inducing the G2/M phase cell cycle arrest [13]; consequently, PTT can put cells in a radiosensitive phase of the cell cycle. Therefore, a combination of these treatment modalities can increase the efficiency of cancer treatment. The third mechanism in inducing synergistic effects can be related to proteins [5]. PTT increases the effects of RT by attenuating the repair mechanism of DNA double-strand break induced by RT [4]. PTT with induction of protein denaturation in enzymes, which are responsible for DNA repair, causes DNA irreversible damage in cancer cells [13, 16].
Moreover, to increase in treatment efficacy, the combination of RT and PTT has another advantage that is the possibility of reducing the prescribed radiation dose to the tumor so that received dose by normal tissues adjacent to the tumor can be decreased. For example, it has been reported [12] that to achieve specific cell survival reduction, about 20% radiation dose can be reduced due to the synergistic effect of RT and PTT in the presence of GNPs relative to RT alone. So that, the increased radiosensitivity level of 1.38 in the presence of GNPs in the single treatment (RT) reached to 1.63 in combination therapy (RT plus PTT).
Summary and future perspectives
GNP-mediated PTT is a hopeful treatment modality, in which heat is generated through the interaction of NIR light with GNPs, to kill cancer cells or suppress their growth [18]. Some effective factors such as size, concentration, and surface modification of NPs, pulse duration, and laser power as well as the time of irradiation can be optimized to increase the efficacy of the treatment. However, further studies are needed to improve our understanding of the dominant mechanisms of this treatment.
The uniform and efficient NPs’ delivery to cancer cells are often problematic due to non-specific targeting in PTT in the presence of GNPs [34]. The biological differences between cancer and normal cells have led to specific targeting [51] so that dramatically, cell death occurs in cancer cells compared to normal cells in PTT using functionalized GNPs [34]. In other words, by targeting GNPs against cancer cells, it is possible to accumulate selectively them within or on the surface of these cells [17]. In this way, the cells will be susceptible to the PTT and the treatment efficacy increases and also side effects of the PTT decreases [7]. The challenges of using GNPs in PTT of cancer cells include their cellular uptake, and the escape from specific subcellular sites such as lysosome, endosome, and mitochondria [47]. Also, targeting of intracellular organelles is difficult due to the cumulative behavior of GNPs [54] and their accumulation in a non-biological colloid destroys the photo-thermal-heating effect of the GNPs [11]. The properly functionalizing of GNPs could facilitate the escape from lysosomes and endosomes, or promote cellular uptake in a path other than endocytosis [47]. However, it remains unclear to identify the induced effects associated with an intracellular interaction between GNPs and subcellular components [46]. Also, the need for powerful lasers and the change in absorption curve of NPs are other problems that require further investigations in PTT. The use of PTT in accompany with RT on hypoxic cells reduces the possibility of tumor recurrence. The effect of PTT on hypoxic cells is increasing the radiosensitivity of these cells to RT which can lead to a decrease in required lethal dose to the tumor, and consequently, RT sessions reduce in the fractionated radiation regimen. On the other hand, reducing the dose to the patient will reduce the side effects of ionizing radiation in these patients. Despite the studies of the synergistic effect of PTT and RT, the lack of adequate clinical studies is one of the factors that restricts the development of this strategy for the clinical application.
References
Liu SY, Liang ZS, Gao F, Luo SF, Lu GQ (2010) In vitro photothermal study of gold nanoshells functionalized with small targeting peptides to liver cancer cells. J Mater Sci Mater Med 21(2):665–674. https://doi.org/10.1007/s10856-009-3895-x
Wu P, Gao Y, Zhang H, Cai C (2012) Aptamer-guided silver-gold bimetallic nanostructures with highly active surface-enhanced Raman scattering for specific detection and near-infrared photothermal therapy of human breast cancer cells. Anal Chem 84(18):7692–7699. https://doi.org/10.1021/ac3015164
Espinosa A, Silva AK, Sanchez-Iglesias A, Grzelczak M, Pechoux C, Desboeufs K, Liz-Marzan LM, Wilhelm C (2016) Cancer cell internalization of gold nanostars impacts their photothermal efficiency in vitro and in vivo: toward a plasmonic thermal fingerprint in tumoral environment. Adv Healthc Mater 5(9):1040–1048. https://doi.org/10.1002/adhm.201501035
Zhang AW, Guo WH, Qi YF, Wang JZ, Ma XX, Yu DX (2016) Synergistic effects of gold nanocages in hyperthermia and radiotherapy treatment. Nanoscale Res Lett 11(1):279. https://doi.org/10.1186/s11671-016-1501-y
Paunesku T, Gutiontov S, Brown K, Woloschak GE (2015) Radiosensitization and nanoparticles. Cancer Treat Res 166:151–171. https://doi.org/10.1007/978-3-319-16555-4_7
Yang L, Tseng YT, Suo G, Chen L, Yu J, Chiu WJ, Huang CC, Lin CH (2015) Photothermal therapeutic response of cancer cells to aptamer-gold nanoparticle-hybridized graphene oxide under NIR illumination. ACS Appl Mater Interfaces 7(9):5097–5106. https://doi.org/10.1021/am508117e
Fernandez-Cabada T, de Pablo CSL, Pisarchyk L, Serrano-Olmedo JJ, Ramos-Gomez M (2016) Optical hyperthermia using anti-epidermal growth factor receptor-conjugated gold nanorods to induce cell death in glioblastoma cell lines. J Nanosci Nanotechnol 16(7):7689–7695. https://doi.org/10.1166/jnn.2016.12570
Banu H, Stanley B, Faheem SM, Seenivasan R, Premkumar K, Vasanthakumar G (2014) Thermal chemosensitization of breast cancer cells to cyclophosphamide treatment using folate receptor targeted gold nanoparticles. Plasmonics 9(6):1341–1349. https://doi.org/10.1007/s11468-014-9747-7
Jubb AM, Buffa FM, Harris AL (2010) Assessment of tumour hypoxia for prediction of response to therapy and cancer prognosis. J Cell Mol Med 14(1–2):18–29. https://doi.org/10.1111/j.1582-4934.2009.00944.x
Rau LR, Huang WY, Liaw JW, Tsai SW (2016) Photothermal effects of laser-activated surface plasmonic gold nanoparticles on the apoptosis and osteogenesis of osteoblast-like cells. Int J Nanomedicine 11:3461–3473. https://doi.org/10.2147/ijn.s108152
Raoof M, Corr SJ, Kaluarachchi WD, Massey KL, Briggs K, Zhu C, Cheney MA, Wilson LJ, Curley SA (2012) Stability of antibody-conjugated gold nanoparticles in the endolysosomal nanoenvironment: implications for noninvasive radiofrequency-based cancer therapy. Nanomedicine 8(7):1096–1105. https://doi.org/10.1016/j.nano.2012.02.001
Ma N, Jiang YW, Zhang X, Wu H, Myers JN, Liu P, Jin H, Gu N, He N, Wu FG, Chen Z (2016) Enhanced radiosensitization of gold nanospikes via hyperthermia in combined cancer radiation and photothermal therapy. ACS Appl Mater Interfaces 8(42):28480–28494. https://doi.org/10.1021/acsami.6b10132
Li P, Shi YW, Li BX, Xu WC, Shi ZL, Zhou C, Fu S (2015) Photo-thermal effect enhances the efficiency of radiotherapy using Arg-Gly-Asp peptides-conjugated gold nanorods that target alphavbeta3 in melanoma cancer cells. J Nanobiotechnol 13:52. https://doi.org/10.1186/s12951-015-0113-5
Mousavi M, Nedaei HA, Khoei S, Eynali S, Khoshgard K, Robatjazi M, Iraji Rad R (2017) Enhancement of radiosensitivity of melanoma cells by pegylated gold nanoparticles under irradiation of megavoltage electrons. Int J Radiat Biol 93(2):214–221. https://doi.org/10.1080/09553002.2017.1231944
Wang H, Zhao R, Li Y, Liu H, Li F, Zhao Y, Nie G (2016) Aspect ratios of gold nanoshell capsules mediated melanoma ablation by synergistic photothermal therapy and chemotherapy. Nanomedicine 12(2):439–448. https://doi.org/10.1016/j.nano.2015.11.013
Chen CW, Lee PH, Chan YC, Hsiao M, Chen CH, Wu PC, Wu PR, Tsai DP, Tu D, Chen XY, Liu RS (2015) Plasmon-induced hyperthermia: hybrid upconversion NaYF4:Yb/Er and gold nanomaterials for oral cancer photothermal therapy. J Mater Chem B 3(42):8293–8302. https://doi.org/10.1039/c5tb01393c
Qin Z, Bischof JC (2012) Thermophysical and biological responses of gold nanoparticle laser heating. Chem Soc Rev 41(3):1191–1217. https://doi.org/10.1039/c1cs15184c
Alfranca G, Artiga A, Stepien G, Moros M, Mitchell SG, de la Fuente JM (2016) Gold nanoprism-nanorod face off: comparing the heating efficiency, cellular internalization and thermoablation capacity. Nanomedicine (Lond) 11(22):2903–2916. https://doi.org/10.2217/nnm-2016-0257
Wang X, Zhou J, Chen B, Tang Z, Zhang J, Li L, Tang J (2016) Enhanced intracellular hyperthermia efficiency by magnetic nanoparticles modified with nucleus and mitochondria targeting peptides. J Nanosci Nanotechnol 16(6):6560–6566
Vankayala R, Lin CC, Kalluru P, Chiang CS, Hwang KC (2014) Gold nanoshells-mediated bimodal photodynamic and photothermal cancer treatment using ultra-low doses of near infra-red light. Biomaterials 35(21):5527–5538. https://doi.org/10.1016/j.biomaterials.2014.03.065
Zhan T, Li P, Bi S, Dong B, Song H, Ren H, Wang L (2012) 12P-conjugated PEG-modified gold nanorods combined with near-infrared laser for tumor targeting and photothermal therapy. J Nanosci Nanotechnol 12(9):7198–7205
Park J, Park J, Ju EJ, Park SS, Choi J, Lee JH, Lee KJ, Shin SH, Ko EJ, Park I, Kim C, Hwang JJ, Lee JS, Song SY, Jeong SY, Choi EK (2015) Multifunctional hollow gold nanoparticles designed for triple combination therapy and CT imaging. J Control Release 207:77–85. https://doi.org/10.1016/j.jconrel.2015.04.007
Her S, Jaffray DA, Allen C (2017) Gold nanoparticles for applications in cancer radiotherapy: mechanisms and recent advancements. Adv Drug Deliv Rev 109:84–101. https://doi.org/10.1016/j.addr.2015.12.012
Baeza A, Manzano M, Colilla M, Vallet-Regi M (2016) Recent advances in mesoporous silica nanoparticles for antitumor therapy: our contribution. Biomater Sci 4(5):803–813. https://doi.org/10.1039/c6bm00039h
Hill TK, Mohs AM (2016) Image-guided tumor surgery: will there be a role for fluorescent nanoparticles? Wiley Interdiscip Rev Nanomed Nanobiotechnol 8(4):498–511. https://doi.org/10.1002/wnan.1381
Huang X, Jain PK, El-Sayed IH, El-Sayed MA (2008) Plasmonic photothermal therapy (PPTT) using gold nanoparticles. Lasers Med Sci 23(3):217–228. https://doi.org/10.1007/s10103-007-0470-x
Mocan L, Ilie I, Tabaran FA, Dana B, Zaharie F, Zdrehus C, Puia C, Mocan T, Muntean V, Teodora P, Ofelia M, Marcel T, Iancu C (2013) Surface plasmon resonance-induced photoactivation of gold nanoparticles as mitochondria-targeted therapeutic agents for pancreatic cancer. Expert Opin Ther Targets 17(12):1383–1393. https://doi.org/10.1517/14728222.2013.855200
Azhdarzadeh M, Atyabi F, Saei AA, Varnamkhasti BS, Omidi Y, Fateh M, Ghavami M, Shanehsazzadeh S, Dinarvand R (2016) Theranostic MUC-1 aptamer targeted gold coated superparamagnetic iron oxide nanoparticles for magnetic resonance imaging and photothermal therapy of colon cancer. Colloids Surf B Biointerfaces 143:224–232. https://doi.org/10.1016/j.colsurfb.2016.02.058
Du B, Ma C, Ding G, Han X, Li D, Wang E, Wang J (2017) Cooperative strategies for enhancing performance of photothermal therapy (PTT) agent: optimizing its photothermal conversion and cell internalization ability. Small 13(13). https://doi.org/10.1002/smll.201603275
Park SE, Lee J, Lee T, Bae SB, Kang B, Huh YM, Lee SW, Haam S (2015) Comparative hyperthermia effects of silica-gold nanoshells with different surface coverage of gold clusters on epithelial tumor cells. Int J Nanomedicine 10(Spec Iss):261–271. https://doi.org/10.2147/ijn.s88309
Sun X, Zhang G, Keynton RS, O'Toole MG, Patel D, Gobin AM (2013) Enhanced drug delivery via hyperthermal membrane disruption using targeted gold nanoparticles with PEGylated protein-G as a cofactor. Nanomedicine 9(8):1214–1222. https://doi.org/10.1016/j.nano.2013.04.002
Liu J, Liang Y, Liu T, Li D, Yang X (2015) Anti-EGFR-conjugated hollow gold nanospheres enhance radiocytotoxic targeting of cervical cancer at megavoltage radiation energies. Nanoscale Res Lett 10:218. https://doi.org/10.1186/s11671-015-0923-2
Huang X, El-Sayed IH, Qian W, El-Sayed MA (2006) Cancer cell imaging and photothermal therapy in the near-infrared region by using gold nanorods. J Am Chem Soc 128(6):2115–2120. https://doi.org/10.1021/ja057254a
Huang HC, Rege K, Heys JJ (2010) Spatiotemporal temperature distribution and cancer cell death in response to extracellular hyperthermia induced by gold nanorods. ACS Nano 4(5):2892–2900. https://doi.org/10.1021/nn901884d
Fay F, Scott CJ (2011) Antibody-targeted nanoparticles for cancer therapy. Immunotherapy 3(3):381–394. https://doi.org/10.2217/imt.11.5
Douglass M, Bezak E, Penfold S (2013) Monte Carlo investigation of the increased radiation deposition due to gold nanoparticles using kilovoltage and megavoltage photons in a 3D randomized cell model. Med Phys 40(7):071710. https://doi.org/10.1118/1.4808150
Li X, Zhou H, Yang L, Du G, Pai-Panandiker AS, Huang X, Yan B (2011) Enhancement of cell recognition in vitro by dual-ligand cancer targeting gold nanoparticles. Biomaterials 32(10):2540–2545. https://doi.org/10.1016/j.biomaterials.2010.12.031
Mendoza-Nava H, Ferro-Flores G, Ocampo-Garcia B, Serment-Guerrero J, Santos-Cuevas C, Jimenez-Mancilla N, Luna-Gutierrez M, Camacho-Lopez MA (2013) Laser heating of gold nanospheres functionalized with octreotide: in vitro effect on HeLa cell viability. Photomed Laser Surg 31(1):17–22. https://doi.org/10.1089/pho.2012.3320
Wang M, Thanou M (2010) Targeting nanoparticles to cancer. Pharmacol Res 62(2):90–99. https://doi.org/10.1016/j.phrs.2010.03.005
Mansoori GA, Brandenburg KS, Shakeri-Zadeh A (2010) A comparative study of two folate-conjugated gold nanoparticles for cancer nanotechnology applications. Cancers (Basel) 2(4):1911–1928. https://doi.org/10.3390/cancers2041911
Khoshgard K, Hashemi B, Arbabi A, Rasaee MJ, Soleimani M (2014) Radiosensitization effect of folate-conjugated gold nanoparticles on HeLa cancer cells under orthovoltage superficial radiotherapy techniques. Phys Med Biol 59(9):2249–2263. https://doi.org/10.1088/0031-9155/59/9/2249
Yasun E, Li C, Barut I, Janvier D, Qiu L, Cui C, Tan W (2015) BSA modification to reduce CTAB induced nonspecificity and cytotoxicity of aptamer-conjugated gold nanorods. Nano 7(22):10240–10248. https://doi.org/10.1039/c5nr01704a
Huang YF, Chang HT, Tan W (2008) Cancer cell targeting using multiple aptamers conjugated on nanorods. Anal Chem 80(3):567–572. https://doi.org/10.1021/ac702322j
Raha S, Paunesku T, Woloschak G (2011) Peptide-mediated cancer targeting of nanoconjugates. Wiley Interdiscip Rev Nanomed Nanobiotechnol 3(3):269–281. https://doi.org/10.1002/wnan.121
Heidari Z, Salouti M, Sariri R (2015) Breast cancer photothermal therapy based on gold nanorods targeted by covalently-coupled bombesin peptide. Nanotechnology 26(19):195101. https://doi.org/10.1088/0957-4484/26/19/195101
Zhang F, Zhu X, Gong J, Sun Y, Chen D, Wang J, Wang Y, Guo M, Li W (2016) Lysosome-mitochondria-mediated apoptosis specifically evoked in cancer cells induced by gold nanorods. Nanomedicine (London) 11(15):1993–2006. https://doi.org/10.2217/nnm-2016-0139
Kodiha M, Wang YM, Hutter E, Maysinger D, Stochaj U (2015) Off to the organelles—killing cancer cells with targeted gold nanoparticles. Theranostics 5(4):357–370. https://doi.org/10.7150/thno.10657
Stern ST, Adiseshaiah PP, Crist RM (2012) Autophagy and lysosomal dysfunction as emerging mechanisms of nanomaterial toxicity. Part Fibre Toxicol 9:20. https://doi.org/10.1186/1743-8977-9-20
Asik E, Akpinar Y, Guray T, Iscan M, Demircigil GC, Volkan M (2016) Cellular uptake, genotoxicity and cytotoxicity of cobalt ferrite magnetic nanoparticles in human breast cells. Toxicol Res 5(6):1649–1662. https://doi.org/10.1039/c6tx00211k
Sabella S, Carney RP, Brunetti V, Malvindi MA, Al-Juffali N, Vecchio G, Janes SM, Bakr OM, Cingolani R, Stellacci F, Pompa PP (2014) A general mechanism for intracellular toxicity of metal-containing nanoparticles. Nano 6(12):7052–7061. https://doi.org/10.1039/c4nr01234h
Wang L, Liu Y, Li W, Jiang X, Ji Y, Wu X, Xu L, Qiu Y, Zhao K, Wei T, Li Y, Zhao Y, Chen C (2011) Selective targeting of gold nanorods at the mitochondria of cancer cells: implications for cancer therapy. Nano Lett 11(2):772–780. https://doi.org/10.1021/nl103992v
Li Y, Yu Y, Duan JC, Li ZL, Geng WJ, Jiang LZ, Wang J, Jin MH, Liu XM, Sun ZW (2016) The internalization, distribution, and ultrastructure damage of silica nanoparticles in human hepatic L-02 cells. Part Part Syst Charact 33(9):664–674. https://doi.org/10.1002/ppsc.201600043
Lee H, Dam DH, Ha JW, Yue J, Odom TW (2015) Enhanced human epidermal growth factor receptor 2 degradation in breast cancer cells by lysosome-targeting gold nanoconstructs. ACS Nano 9(10):9859–9867. https://doi.org/10.1021/acsnano.5b05138
Mkandawire MM, Lakatos M, Springer A, Clemens A, Appelhans D, Krause-Buchholz U, Pompe W, Rodel G, Mkandawire M (2015) Induction of apoptosis in human cancer cells by targeting mitochondria with gold nanoparticles. Nano 7(24):10634–10640. https://doi.org/10.1039/c5nr01483b
Kodiha M, Hutter E, Boridy S, Juhas M, Maysinger D, Stochaj U (2014) Gold nanoparticles induce nuclear damage in breast cancer cells, which is further amplified by hyperthermia. Cell Mol Life Sci 71(21):4259–4273. https://doi.org/10.1007/s00018-014-1622-3
Yang C, Uertz J, Yohan D, Chithrani BD (2014) Peptide modified gold nanoparticles for improved cellular uptake, nuclear transport, and intracellular retention. Nano 6(20):12026–12033. https://doi.org/10.1039/c4nr02535k
Khoshgard K, Kiani P, Haghparast A, Hosseinzadeh L, Eivazi MT (2017) Radiation dose rate affects the radiosensitization of MCF-7 and HeLa cell lines to X-rays induced by dextran-coated iron oxide nanoparticles. Int J Radiat Biol 93(8):757–763. https://doi.org/10.1080/09553002.2017.1321806
Lin Y, McMahon SJ, Scarpelli M, Paganetti H, Schuemann J (2014) Comparing gold nano-particle enhanced radiotherapy with protons, megavoltage photons and kilovoltage photons: a Monte Carlo simulation. Phys Med Biol 59(24):7675–7689. https://doi.org/10.1088/0031-9155/59/24/7675
Jain S, Coulter JA, Butterworth KT, Hounsell AR, McMahon SJ, Hyland WB, Muir MF, Dickson GR, Prise KM, Currell FJ, Hirst DG, O'Sullivan JM (2014) Gold nanoparticle cellular uptake, toxicity and radiosensitisation in hypoxic conditions. Radiother Oncol 110(2):342–347. https://doi.org/10.1016/j.radonc.2013.12.013
Author information
Authors and Affiliations
Contributions
Hasan Norouzi and Karim Khoshgard conceived the idea, made plan for the review, contributed text, provided tables, and finalized the manuscript; Hasan Norouzi and Fatemeh Akbarzadeh collected data and made the figure; all authors reviewed the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study does not contain any articles from the authors in the photo-thermal therapy.
Informed consent
Informed consent was not needed for this review.
Rights and permissions
About this article
Cite this article
Norouzi, H., Khoshgard, K. & Akbarzadeh, F. In vitro outlook of gold nanoparticles in photo-thermal therapy: a literature review. Lasers Med Sci 33, 917–926 (2018). https://doi.org/10.1007/s10103-018-2467-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-018-2467-z