Abstract
Vancomycin (VAN) minimum inhibitory concentrations (MICs) at the upper end of the susceptible range for Staphylococcus aureus (S. aureus), as measured by the Etest method, have been associated with poor clinical outcomes of S. aureus bloodstream infections, as has the isolate’s genetic background. Here, we assessed the impact of VAN MICs, as determined by a broth microdilution method (BMD) that incorporates incremental VAN concentrations between the conventional log2 dilutions, isolate susceptibility to killing by human phagocytes, acting as a surrogate marker for bacterial cell wall thickness, and S. aureus genetic composition, on the development of complicated S. aureus bacteremia (SAB). We carried out a retrospective, observational single-center cohort study of 148 consecutive patients with SAB caused by methicillin-susceptible (MSSA) isolates (n = 113) or methicillin-resistant (MRSA) isolates (n = 35). S. aureus isolates were genotyped using a commercially available DNA microarray. Overall, VAN MICs of S. aureus isolates taken from complicated and uncomplicated SAB were comparable, irrespective of the testing method (P = 0.19 with BMD, and P = 0.94 with Etest). Likewise, S. aureus isolates in both comparison groups had the same susceptibility to killing by human phagocytes (P = 0.5). Among the genes screened by the S. aureus DNA array, only Sec and Sel were differentially present among S. aureus isolates in both groups (overrepresented in those causing complications) and their presence was associated independently with complicated SAB in multivariate models adjusted for potentially relevant clinical covariates. Separate analysis of MSSA SAB episodes yielded similar results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The debate as to whether or not Staphylococcus aureus (S. aureus) vancomycin (VAN) minimum inhibitory concentration (MIC) at the upper end of the susceptible range impacts adversely on clinical outcomes of methicillin-resistant (MRSA) and methicillin-susceptible (MSSA) S. aureus bloodstream infections remains unsettled [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20]. Most studies supporting this assumption used the Etest method for VAN MIC assessment, uniformly showing that bacteremic infections caused by S. aureus isolates displaying MICs ≥ 1.5 mg/L are associated with an increased risk of complications, mortality, or both [1, 3, 4, 6, 8, 16, 18]. Nevertheless, S. aureus VAN MICs provided by the Etest method are poorly reproducible and lack precision [21], potentially hampering comparison of experiences across centers. In this context, we recently developed a broth microdilution method (BMD) that incorporates incremental VAN concentrations within the susceptible range, not only between the conventional log2 dilutions, but also between those on the Etest scale, which permits robust and precise measurement of VAN MIC [22], and in our view may contribute toward elucidating the true relevance of this S. aureus phenotypic trait in clinical outcomes.
The possibility that high S. aureus VAN MICs, as measured by Etest, reflect a phenotypic advantage in terms of virulence has been postulated [4, 6]. In this sense, hVISA and S. aureus VAN-resistant strains exhibit a thicker cell wall and as a result may be suboptimally phagocytosed [23, 24]. In line with this, we previously found an inverse relationship between the susceptibility of the isolates to killing by human phagocytes and cell wall thickness for VAN-susceptible S. aureus isolates [25], thus suggesting that the killing index may be used as a surrogate marker for this structural bacterial phenotypic feature. Furthermore, a number of studies suggest that the ability of S. aureus to cause complicated bacteremia is notably influenced by the isolate’s genetic background [26,27,28,29]. In this context, a number of specific resistance and virulence genes have been linked to elevated VAN MICs in the Etest [26,27,28,29]. Here, we assessed the impact of VAN MICs as measured by our BMD method, as well as isolate susceptibility to killing by human phagocytes and bacterial genetic characteristics, on the development of complicated S. aureus bacteremia (SAB).
Patients and methods
Study population
We carried out a retrospective, observational single-center cohort study of 148 consecutive patients (median age, 66.5 years; range, 1 to 91 years), of which 139 were adults (≥ 18 years old) and 9 children, with bloodstream infections caused by S. aureus within the period January 2013 to May 2018. Only patients with first episodes of SAB were considered. An infectious disease specialist (RO) reviewed all chart information focusing on demographics and relevant clinical data including age, sex, source of bacteremia, co-morbid conditions, antibiotic treatment, and outcome. The study was approved by the Ethics Committee of the Hospital Clínico Universitario INCLIVA, which waived requirement of informed consent.
Bacterial isolates
A total of 148 S. aureus isolates (MSSA, n = 113; MRSA, n = 35) recovered from first positive blood cultures (BACTEC™ FX Instrument; Beckton Dickinson-BD-, Sparks, MD) from unique patients at the Microbiology Service of the Hospital Clínico Universitario of Valencia were evaluated in this study. S. aureus were primarily identified by colony morphology, Gram staining, and a positive slide coagulase test [21]. Bacterial identity was confirmed by MALDi-TOF MS analysis. MRSA were detected by the standard disc diffusion method using a 30-mg cefoxitin disc (BBL Microbiology Systems, Cockeysville, MD, USA). All primary isolates had been cryopreserved at − 70 °C in glycerol containing Bacto-Brain Heart Infusion broth-BHI- (BD) and were retrieved for the analyses described herein.
Determining Staphylococcus aureus vancomycin MIC values
Frozen stocks were thawed and the isolates were subcultured overnight on trypticase soy agar plates with 5% sheep’s blood (BD). VAN MICs were measured using in-house prepared BMD panels that included the following antibiotic concentrations: 0.50, 0.62, 0.75, 0.87, 1.0, 1.25, 1.40, 1.50, 1.60, 1.75, and 2.0 μg/ml in cation-adjusted Mueller-Hinton broth [22], and by Etest, which was performed using a standard procedure as previously reported [21]. All isolates were screened for VAN heteroresistance (hVISA) at time of isolation using the Etest macromethod, performed using a 2.0 McFarland inoculum on BHI agar plates (BD), using vancomycin and teicoplanin Etest strips (bioMérieux) [21]. Heteroresistance by the Etest macromethod was defined as MICs for vancomycin and teicoplanin of ≥ 8 mg/L or a teicoplanin MIC of ≥ 12 mg/L regardless of the vancomycin MIC.
Staphylococcus aureus killing assay
These experiments were performed following a published protocol [23]. Briefly, whole blood was obtained from healthy volunteers by venipuncture using heparinized syringes (Lithium Heparin, BD). An aliquot of heparinized blood was centrifuged 5 min at 3000×g to obtain the plasma fraction. Primary subcultures of the isolates were made on sheep’s blood agar plates (BD). Bacterial cells were grown at 37 °C to the exponential growth phase and then collected, washed in phosphate-buffered saline pH, 7.4 (PBS), and resuspended in RPMI 1640 culture medium (Gibco, Barcelona, Spain). Cells (0.5 × 106) were inoculated in parallel into 100 μl of human whole blood or plasma and incubated for 1 h at 37 °C. At the desired times (t0 and t1), samples were diluted in pyrogen-free distilled water (pH 4.5–6.5), left for 5 min at room temperature, and vortexed vigorously for ∼ 5 s. Viable bacterial cells were determined by plating serial dilutions (in triplicate) on Mueller Hinton agar followed by overnight incubation at 37 °C. The survival percentage was calculated as follows: % CFU in blood = [CFU blood (1 h) / CFU blood (0 h)] × 100; % CFU in plasma = [CFU plasma (1 h) / CFU plasma (0 h)] × 100; % survival = (% CFU in blood/% CFU plasma) × 100; % killing=: 100 - % survival. Low and high susceptibility to killing were defined as % killing < 60% and > 70%, respectively [25].
Staphylococcus aureus genetic composition analysis
S. aureus isolates were genotyped using the S. aureus DNA microarray from Clondiag (S. aureus Genotyping Kit 2.0 Jena, Germany), strictly following the manufacturer’s recommendations, and as previously detailed [23]. Extraction of bacterial DNA from primary subcultures on sheep’s blood agar plates (BD) was performed using DNA extraction reagents and the EZ1 automated device (Qiagen, CA, USA).
Clinical outcomes
The main outcome variable was the development of complicated SAB, which was defined by the following events, as previously reported [4, 6, 11, 28]: (i) endocarditis, (ii) septic thrombophlebitis, (iii) metastatic infection, (iv) persistent bacteremia for > 72 h after initiating active antimicrobial drug therapy, and (v) recurrent bacteremia, defined as the presence of subsequent blood cultures positive for S. aureus within 30 days of the index blood culture after initial clearance of bacteremia. Nosocomial and community SAB were those diagnosed after at least or within 48 h after hospital admission, respectively. Empirical (first-line) treatment was defined as any antibiotic regimen administered within 48 h after bloodstream infection diagnosis in the absence of antimicrobial susceptibility data.
Statistical analysis
The Mann-Whitney U test was used to compare continuous variables with non-normal distribution. Correlation between variables was assessed by the Spearman Rank test. The chi-square test was used to compare proportions. All statistical tests were two-tailed and the threshold for statistical significance was P = <0.05. To analyze the risk factors for developing complicated bacteremia, we performed a multivariate forward stepwise logistic regression model including all the clinically relevant variables with a P value of < 0.05 and possible confounding factors with a P value of < 0.1 detected in the univariate analysis. All the statistical analyses were performed using SPSS version 20.0 (SPSS, Chicago, IL, USA).
Results
Staphylococcus aureus bacteremia episodes
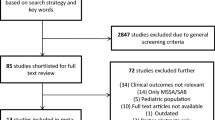
A total of 148 episodes of SAB were included in the current study. Of these, 113 were caused by MSSA and 35 by MRSA. There were 104 community-acquired episodes and 44 nosocomial episodes. The probable sources of SAB were low respiratory tract infection (n = 34; 22.3%), skin and soft tissues (n = 26; 17.6%), vascular catheter (n = 25; 16.9%), intra-abdominal (n = 15; 10.1%), urinary tract (n = 15; 10.1%), and osteoarticular (n = 13; 8.8%) and surgical site infection (n = 5; 3.4%). The primary site of infection was unknown in the remaining 15 patients (10.1%). Thirty-seven patients (25%) developed complicated SAB; in detail, 11 patients had suppurative thrombophlebitis, 10 metastatic osteoarticular infection, 7 persistent bacteremia, 4 recurrent bacteremia, 4 endocarditis, and 1 embolic infection.
Staphylococcus aureus vancomycin MIC values
All S. aureus isolates were susceptible to vancomycin (≤ 2 mg/L). No isolate was categorized as hVISA. VAN MIC values of the isolates as determined by BMD and Etest are shown in Fig. 1. Modal vancomycin BMD MIC was 0.63 mg/L for both MSSA and MRSA isolates. Modal Etest MIC value was 1 mg/L for both MSSA and MRSA isolates. Poor correlation was seen between VAN MIC values measured by BMD and Etest (rho = 0.291). S. aureus isolates in our series were genetically diverse, as inferred by the wide variety of clonal complex (CC) types documented (21 types). The most prevalent clonal types were CC5 (n = 39), CC30 (n = 19), CC8 (n = 15), CC22 (n = 12), CC45 (n = 9), and CC398 (n = 8). As shown in Fig. 2, S. aureus VAN MIC values were comparable across the clonal complex types, regardless of the method employed for VAN MIC determination (P = 0.61 with BMD and P = 0.51 with Etest).
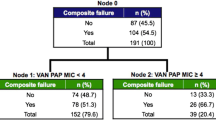
Phenotypic and genotypic features of Staphylococcus aureus isolates and development of complicated bacteremia
Overall, VAN MICs of S. aureus isolates recovered from complicated and uncomplicated bacteremia episodes were comparable (Fig. 3), irrespective of the testing method (P = 0.19 for BMD and P = 0.94 for Etest). Likewise, as shown in Fig. 4, S. aureus isolates in both comparison groups had the same susceptibility to killing by human phagocytes (P = 0.5). In fact, ROC curve analyses failed to identify a cut-off value for both parameters to discriminate reliably between S. aureus isolates either involved or not involved in complicated bacteremic episodes (not shown). These observations stood when MSSA isolates were analyzed separately (P = 0.68 with BMD and P = 0.77 with Etest; P = 0.71 for the killing index). S. aureus isolates in the comparison groups were not significantly different regarding clonal complex type, capsular type, or accessory gene regulator (agr) group (Table 1). Among the genes screened by the S. aureus DNA array, only Sec and Sel were differentially present among S. aureus isolates in both groups (overrepresented in those causing complications; P = 0.01) (Table 1 and Supplementary Table 1).
Staphylococcus aureus (S. aureus) vancomycin (VAN) MIC values measured by broth microdilution (BMD) (panel a) and Etest (panel b) in isolates either involved or not involved in complicated bacteremia episodes (SAB). Data restricted to methicillin-susceptible (MSSA) isolates are shown in panels c and d
Risk factors for developing complicated Staphylococcus aureus bacteremia
In addition to S. aureus phenotypic features (VAN MIC value and killing index) and genetic traits found to be associated with complications in frequency comparison analyses (Table 1), several clinical covariates with potential relevance were recorded in order to assess differences between comparison groups, as well as to control for potential confounding factors by logistic regression modeling. Clinical covariates included patient’s demographics, acquisition category (community vs. nosocomial) co-morbidities (measured by the Charlson comorbidity index), severity of illness (presence of septic shock at bacteremia onset), source of bacteremia, suitability of first-line antibiotic therapy, overall antibiotic use, and clinical management of the primary source of bacteremia. Note that (i) initial antibiotic therapy was deemed appropriate in 50% of episodes and the median delay in starting it was 1.5 days (IQR, 0–3 days); (ii) β-lactam antibiotics were administered in 86 episodes (52.8%) and glycopeptides in 50 episodes (33.7%). As shown in Table 2, the presence of Sec and Sel genes was the only factor independently associated with the occurrence of complicated SAB (OR, 3.45; 95% CI 1.26–9.45; P = 0.02). When considering only MSSA isolates for the analyses, both the presence of sec and sel genes and the use of non β-lactam agents were associated with increased risk of complicated SAB (Supplementary Table 2).
Discussion
Elucidation of the true impact of glycopeptide-susceptible S. aureus VAN MIC values on SAB outcomes is of indisputable relevance, as it may critically influence therapeutic management of this clinical entity. VAN MIC values at the upper end of the susceptibility range (≥ 1.5 mg/L), using the Etest method, have been associated with higher morbimortality rates than those caused by highly susceptible strains (MIC ≤ 1 mg/mL) [1, 3, 4, 6, 8, 16, 18], although this assumption has been disputed [11, 12]. In our view, the Etest method is inappropriate for evaluating the attributable impact of S. aureus VAN MICs on outcomes in any clinical setting, owing to the method’s low reproducibility and lack of precision [21]; in fact, S. aureus VAN MIC values measured by Etest correlate poorly with those determined by BMD and agar dilution assays, the methods of choice according to international agencies (i.e., Clinical Laboratory Standard Institute-CLSI, and the European Committee on Antimicrobial Susceptibility Testing-EUCAST-) [30,31,32] and are uniformly reported to be higher. We recently developed a BMD method incorporating several “inter log2 dilution” concentrations of VAN, which permits a robust and precise determination of VAN MICs with intra- and inter-assay CVs below 20%, which could be instrumental for shedding light on the above issue [22]. Here, we found that S. aureus VAN MIC values within the susceptible range measured with our BMD method were not predictive of complicated SAB as defined herein, either as a continuous or dichotomous variable, in a series including mostly community-acquired episodes originating from a highly heterogeneous source and caused by clonally diverse isolates. In our experience, S. aureus VAN MIC values measured by Etest (≥ 1.5 mg/L vs. ≤ 1 mg/mL) were also not associated with developing SAB complications, in line with previous reports [11, 12]. The limited number of death events in this series precluded any statistically meaningful analysis as to the potential effect of S. aureus VAN MIC values on mortality.
A few studies have assessed the relationship between S. aureus VAN MICs, as measured by BMD methods, and complicated SAB, most failing to find an association. Specifically, Rojas and colleagues [11] found no correlation between VAN MIC values (high, > 1 mg/L; low, ≤ 1 mg/L), measured by an in-house BMD method, and the development of metastatic infection or persistent bacteremia caused by MRSA isolates. Adani et al. [15] reported that VAN MIC values (high levels 2 mg/L; low levels ≤ 2 mg/L), as determined by a commercially available automated BMD method (MicroScan; Beckman Coulter, West Sacramento, CA, USA) were not predictive of persistent or recurrent bacteremia due to MRSA. Baxi et al. [33] reported that high (2 mg/L vs. low, ≤ 2 mg/L) VAN MIC values determined by Microscan were not associated with greater risk of a composite outcome of mortality, readmission, and recurrence in a series including cases due to MSSA and MRSA. Likewise, San-Juan et al. [18], in a study including catheter-related MSSA bacteremia episodes, found no significant differences between isolates either involved or not involved in the development of endocarditis when VAN susceptibility testing was performed using commercial BMD panels (ESTEN 2009, Sensititre™, Izasa, Barcelona, Spain), irrespective of whether VAN MIC values were analyzed as a continuous or dichotomized (> 1.0 ≤ 1.0 mg/L) variable. In contrast, Sullivan et al. [20] reported that SAB due to reduced VAN susceptibility, as defined by Microscan MIC of 2 mg/L, was associated with increased risk of complications in adjusted analyses. The above studies used either commercially available or in-house prepared panels, and all employed conventional BMD methods using serial twofold doubling dilutions of antimicrobials. Between- and within-run variation of 1 log2 dilution is considered acceptable for BMD methods by international agencies (CLSI and EUCAST). Thus, the lack of margin for VAN MIC thresholds defining low vs. high susceptibility in these studies makes the possibility of isolate miscategorization relatively high.
Based on previous observations [23, 24], Aguado and colleagues hypothesized that high S. aureus VAN MIC levels, as determined by Etest, may reflect certain structural modifications (i.e., thicker cell wall), which may result in increased bacterial pathogenicity [4]. In this respect, we previously showed that S. aureus isolates’ susceptibility to killing by human phagocytes in a relatively simple in vitro assay may be used as a surrogate marker for S. aureus cell wall thickness, which requires a rather elaborate measurement protocol involving the use of electronic microscopy [25]. We specifically found the cell wall to be significantly thicker in isolates displaying low killing indices (< 60%) than in ones exhibiting high killing indices (> 70%), irrespective of their susceptibility to methicillin [25]. In this study, we found no association between the killing group to which the isolates belonged and the development of complicated SAB, thus indirectly suggesting that cell wall thickness might not be a relevant pathogenetic factor accounting for increased risk of these clinical events. Naturally, the true relevance of cell wall thickness as a virulence trait in this clinical setting can only be elucidated by electronic microscopy assessment.
The isolate’s genetic background has been suggested as modulating the ability of S. aureus to cause complicated bacteremia; namely, S. aureus isolates belonging to certain genotypic (clonal) types, such as CC5, CC8, CC12, CC15, CC20, CC30, or CC45, have been shown to exhibit a significant trend toward increasing levels of persistent bacteremia or endocarditis [17, 26, 28, 29, 34,35,36,37,38]. Nevertheless, in line with previous reports [12, 19, 27, 39, 40], we failed to find any such associations. Of interest, CCs associated with complicated SAB in the aforementioned studies were well represented in our panel (almost 50%). In addition to substantial differences among cohorts in terms of patients’ clinical characteristics and distribution of MSSA and MRSA isolates, a variety of genotypic typing methods were used in these studies, which may account, at least in part, for the discrepant findings.
Conflicting data have been published on the potential association between S. aureus genotypic traits including the agr type, capsular type, and a wide variety of bacterial genes and the development of complicated SAB [11, 12, 17, 19, 26,27,28,29, 34, 35, 37, 38, 40]. Here, only sec and sel genes (coding for enterotoxin C and L, respectively) were found to be differentially present among S. aureus isolates depending on whether they caused complicated SAB or not (overrepresented in the former isolates). Furthermore, the presence of Sec and Sel genes was the only factor independently associated with complicated SAB in multivariate models adjusted for potentially clinical relevant covariates including patient’s demographics and co-morbidities, severity of illness, source of bacteremia, management of the primary source of bacteremia, suitability of first-line antibiotic therapy, and overall antibiotic use. As for the latter variable, as expected, use of antibiotics other than β-lactams and glycopeptides was also independently associated with complicated SAB caused by MSSA. Enterotoxins C and L exhibit superantigenic properties [41]. Superantigens bind simultaneously to MHC class II (MHC-II) and TCRs, outside their antigen-binding groove, resulting in an excessive inflammatory response that can lead to toxic shock, multiorgan failure, and death [42]. The pathogenetic relevance of S. aureus enterotoxins in the development of endocartidis has also recently been suggested [43]. Notably, S. aureus VAN MIC values were significantly lower in isolates harboring the sec and sel genes than ones in which these genes were absent (not shown), further reinforcing our assumption that VAN MIC values within the susceptibility range may not impact on the risk of complicated SAB.
The current study has a number of limitations deserving mention: (i) clinical data were retrospectively collected and thus possibly subject to information bias; (ii) our single-center design precludes generalizing the study’s conclusions to other communities; (iii) the relatively scarce number and heterogeneity of SAB complications in our series may have resulted in a high probability of type II errors and prevented us from performing robust multivariate analyses; (iv) different sources of SAB; (v) occurrence of recurrent SAB was only assessed through inpatient hospitalization at our center; (vi) conclusions regarding the impact of antibiotic therapy should be taken cautiously due to lack of control over choice of antibiotics and lack of data on vancomycin serum levels; (vii) cryopreserved isolates were used for S. aureus VAN MICs testing; in this sense, we are not certain how long-term storage may impact on MIC values measured by our BMD method. In summary, the data presented herein argue against a potential impact of VAN MIC values on risk of complicated bacteremia due to glycopeptide-susceptible S. aureus, regardless of isolate susceptibility to methicillin. In addition, although firm conclusions on the relevance of sec and sel genes as pathogenetic factors predisposing to complicated SAB cannot be drawn here, our data warrant further studies to explore the possibility.
References
Soriano A, Marco F, Martínez JA, Pisos E, Almela M, Dimova VP et al (2008) Influence of vancomycin minimum inhibitory concentration on the treatment of methicillin-resistant Staphylococcus aureus bacteremia. Clin Infect Dis 46:193–200
Pea F, Viale P (2009) Is the minimum inhibitory concentration of vancomycin an infallible predictor of the clinical outcome of Staphylococcus aureus bacteremia treated with vancomycin? Clin Infect Dis 49:642–643
Holmes NE, Turnidge JD, Munckhof WJ, Robinson JO, Korman TM, O'Sullivan MV et al (2011) Antibiotic choice may not explain poorer outcomes in patients with Staphylococcus aureus bacteremia and high vancomycin minimum inhibitory concentrations. J Infect Dis 204:340–347
Aguado JM, San-Juan R, Lalueza A, Sanz F, Rodríguez-Otero J, Gómez-Gonzalez C et al (2011) High vancomycin MIC and complicated methicillin-susceptible Staphylococcus aureus bacteremia. Emerg Infect Dis 17:1099–1102
Holland TL, Fowler VG Jr (2011) Vancomycin minimum inhibitory concentration and outcome in patients with Staphylococcus aureus bacteremia: pearl or pellet? J Infect Dis 204:329–331
Aguado JM, San-Juan R, Fernández-Ruiz M, Chaves F (2012) Role of high vancomycin minimum inhibitory concentration in the outcome of methicillin-susceptible Staphylococcus aureus bacteremia. J Infect Dis 205:1024–1025
Gould IM (2012) Vancomycin minimum inhibitory concentrations and outcome in patients with severe Staphylococcus aureus infection. J Infect Dis 205:864–865
Cervera C, Castañeda X, García de la María C, del Rio A, Moreno A, Soy D et al (2014) Effect of vancomycin minimal inhibitory concentration on the outcome of methicillin-susceptible Staphylococcus aureus endocarditis. Clin Infect Dis 58:1668–1675
Jacob JT, Diaz Granados CA (2013) High vancomycin minimum inhibitory concentration and clinical outcomes in adults with methicillin-resistant Staphylococcus aureus infections: a meta-analysis. Int J Infect Dis 17:e93–e100
Kalil AC, Van Schooneveld TC, Fey PD, Rupp ME (2014) Association between vancomycin minimum inhibitory concentration and mortality among patients with Staphylococcus aureus bloodstream infections: a systematic review and meta-analysis. JAMA 312:1552–1564
Rojas L, Bunsow E, Muñoz P, Cercenado E, Rodríguez-Créixems M, Bouza E (2012) Vancomycin MICs do not predict the outcome of methicillin-resistant Staphylococcus aureus bloodstream infections in correctly treated patients. J Antimicrob Chemother 67:1760–1768
López-Cortés LE, Velasco C, Retamar P, del Toro MD, Gálvez-Acebal J, de Cueto M et al (2015) Is reduced vancomycin susceptibility a factor associated with poor prognosis in MSSA bacteraemia? J Antimicrob Chemother 70:2652–2660
Chen SY, Liao CH, Wang JL, Chiang WC, Lai MS, Chie WC et al (2014) Method-specific performance of vancomycin MIC susceptibility tests in predicting mortality of patients with methicillin-resistant Staphylococcus aureus bacteraemia. J Antimicrob Chemother 69:211–218
Shoji H, Maeda M, Shirakura T, Takuma T, Ugajin K, Fukuchi K et al (2015) More accurate measurement of vancomycin minimum inhibitory concentration indicates poor outcomes in meticillin-resistant Staphylococcus aureus bacteraemia. Int J Antimicrob Agents 46:532–537
Adani S, Bhowmick T, Weinstein MP, Narayanan N (2018) Impact of vancomycin MIC on clinical outcomes of patients with methicillin-resistant Staphylococcus aureus bacteremia treated with vancomycin at an institution with suppressed MIC reporting. Antimicrob Agents Chemother 62:e02512–e02517
Bouiller K, Laborde C, Aho SL, Hocquet D, Pechinot A, Le Moing V et al (2018) No effect of vancomycin MIC ≥ 1.5 mg/L on treatment outcome in methicillin-susceptible Staphylococcus aureus bacteraemia. Int J Antimicrob Agents 51:721–726
Fernández-Hidalgo N, Ribera A, Larrosa MN, Viedma E, Origüen J, de Alarcón A et al (2018) Impact of Staphylococcus aureus phenotype and genotype on the clinical characteristics and outcome of infective endocarditis. A multicentre, longitudinal, prospective, observational study. Clin Microbiol Infect 24:985–991
San-Juan R, Fernández-Ruiz M, Gasch O, Camoez M, López-Medrano F, Domínguez MÁ et al (2017) High vancomycin MICs predict the development of infective endocarditis in patients with catheter-related bacteraemia due to methicillin-resistant Staphylococcus aureus. J Antimicrob Chemother 72:2102–2109
Gasch O, Camoez M, Dominguez MA, Padilla B, Pintado V, Almirante B et al (2013) Predictive factors for mortality in patients with methicillin-resistant Staphylococcus aureus bloodstream infection: impact on outcome of host, microorganism and therapy. Clin Microbiol Infect 19:1049–1057
Sullivan SB, Austin ED, Stump S, Mathema B, Whittier S, Lowy FD et al (2017) Reduced vancomycin susceptibility of methicillin-susceptible Staphylococcus aureus has no significant impact on mortality but results in an increase in complicated infection. Antimicrob Agents Chemother 61:e00316–e00317
Falcón R, Madrid S, Tormo N, Casañ C, Albert E, Gimeno C et al (2015) Intra- and interinstitutional evaluation of an Etest for vancomycin minimum inhibitory concentration measurement in Staphylococcus aureus blood isolates. Clin Infect Dis 61:1490–1492
Falcón R, Mateo EM, Talaya A, Giménez E, Vinuesa V, Clari MÁ et al (2017) Reproducible measurement of vancomycin MICs within the susceptible range in Staphylococcus aureus by a broth microdilution method with a “quasi-continuum” gradient of antibiotic concentrations. Eur J Clin Microbiol Infect Dis 36:2355–2360
Cui L, Murakami H, Kuwahara-Arai K, Hanaki H, Hiramatsu K (2000) Contribution of a thickened cell wall and its glutamine nonamidated component to the vancomycin resistance expressed by Staphylococcus aureus Mu50. Antimicrob Agents Chemother 44:2276–2285
Cui L, Ma X, Sato K, Tenover FC, Mamizuka EM, Gemmell CG et al (2003) Cell wall thickening is a common feature of vancomycin resistance in Staphylococcus aureus. J Clin Microbiol 41:5–14
Falcón R, Martínez A, Albert E, Madrid S, Oltra R, Giménez E et al (2016) High vancomycin MICs within the susceptible range in Staphylococcus aureus bacteraemia isolates are associated with increased cell wall thickness and reduced intracellular killing by human phagocytes. Int J Antimicrob Agents 47:343–350
Lalani T, Federspiel JJ, Boucher HW, Rude TH, Bae IG, Rybak MJ et al (2008) Associations between the genotypes of Staphylococcus aureus bloodstream isolates and clinical characteristics and outcomes of bacteremic patients. J Clin Microbiol 46:2890–2896
Viedma E, Sanz F, Orellana MA, San Juan R, Aguado JM, Otero JR et al (2014) Relationship between agr dysfunction and reduced vancomycin susceptibility in methicillin-susceptible Staphylococcus aureus causing bacteraemia. J Antimicrob Chemother 69:51–58
Holmes NE, Turnidge JD, Munckhof WJ, Robinson JO, Korman TM, O'Sullivan MV et al (2014) Genetic and molecular predictors of high vancomycin MIC in Staphylococcus aureus bacteremia isolates. J Clin Microbiol 52:3384–3393
San-Juan R, Pérez-Montarelo D, Viedma E, Lalueza A, Fortún J, Loza E et al (2017) Pathogen-related factors affecting outcome of catheter-related bacteremia due to methicillin-susceptible Staphylococcus aureus in a Spanish multicenter study. Eur J Clin Microbiol Infect Dis 36:1757–1765
Kruzel MC, Lewis CT, Welsh KJ, Lewis EM, Dundas NE, Mohr JF et al (2011) Determination of vancomycin and daptomycin MICs by different testing methods for methicillin-resistant Staphylococcus aureus. J Clin Microbiol 49:2272–2273
Muñoz-Cobo B, Sancho-Tello S, Costa E, Bravo D, Torregrosa I, de Lomas JG et al (2011) Differences in vancomycin minimum inhibitory concentrations for Staphylococcus aureus obtained with the automated Phoenix™ system, the clinical and laboratory standards institute broth microdilution method and the standard Etest. Int J Antimicrob Agents 37:278–279
Charlton CL, Hindler JA, Turnidge J, Humphries RM (2014) Precision of vancomycin and daptomycin MICs for methicillin-resistant Staphylococcus aureus and effect of subculture and storage. J Clin Microbiol 52:3898–3905
Baxi SM, Clemenzi-Allen A, Gahbauer A, Deck D, Imp B, Vittinghoff E et al (2016) Vancomycin MIC does not predict 90-day mortality, readmission, or recurrence in a prospective cohort of adults with Staphylococcus aureus bacteremia. Antimicrob Agents Chemother 60:5276–5284
Fowler VG Jr, Nelson CL, McIntyre LM, Kreiswirth BN, Monk A, Archer GL et al (2007) Potential associations between hematogenous complications and bacterial genotype in Staphylococcus aureus infection. J Infect Dis 196:738–747
Xiong YQ, Fowler VG, Yeaman MR, Perdreau-Remington F, Kreiswirth BN, Bayer AS (2009) Phenotypic and genotypic characteristics of persistent methicillin-resistant Staphylococcus aureus bacteremia in vitro and in an experimental endocarditis model. J Infect Dis 199:201–208
Nienaber JJ, Sharma Kuinkel BK, Clarke-Pearson M, Lamlertthon S, Park L, Rude TH et al (2011) Methicillin-susceptible Staphylococcus aureus endocarditis isolates are associated with clonal complex 30 genotype and a distinct repertoire of enterotoxins and adhesins. J Infect Dis 204:704–713
Nethercott C, Mabbett AN, Totsika M, Peters P, Ortiz JC, Nimmo GR et al (2013) Molecular characterization of endocarditis-associated Staphylococcus aureus. J Clin Microbiol 51:2131–2138
Bouchiat C, Moreau K, Devillard S, Rasigade JP, Mosnier A, Geissmann T et al (2015) Staphylococcus aureus infective endocarditis versus bacteremia strains: subtle genetic differences at stake. Infect Genet Evol 36:524–530
Wong H, Watt C, Elsayed S, John M, Johnson G, Katz K et al (2014) Characterization of methicillin-resistant Staphylococcus aureus isolates from patients with persistent or recurrent bacteremia. Can J Infect Dis Med Microbiol 25:83–86
Lilje B, Rasmussen RV, Dahl A, Stegger M, Skov RL, Fowler VG, et al. (2017) Whole-genome sequencing of bloodstream Staphylococcus aureus isolates does not distinguish bacteraemia from endocarditis. Microb Genom. https://doi.org/10.1099/mgen.0.000138
Spaulding AR, Salgado-Pabon W, Kohler PL, Horswill AR, Leung DY, Schlievert PM (2013) Staphylococcal and streptococcal superantigen exotoxins. Clin Microbiol Rev 26:422–447
Li H, Llera A, Malchiodi EL, Mariuzza RA (1999) The structural basis of T cell activation by superantigens. Annu Rev Immunol 17:435–466
Salgado-Pabón W, Breshears L, Spaulding AR, Merriman JA, Stach CS, Horswill AR et al. (2013) Superantigens are critical for Staphylococcus aureus infective endocarditis, sepsis, and acute kidney injury. MBio. https://doi.org/10.1128/mBio.00494-13
Acknowledgements
Estela Giménez holds a Río Hortega research contract from the Carlos III Health Institute (Ref. CM16/00200). Eva María Mateo is grateful to the Ministry of Economy and Competitiveness (MINECO, Spanish Government) for the “Juan de la Cierva” postdoctoral contract (Ref. FJCI-2015-25992).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Transparency declarations
None to declare
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Falcón, R., Mateo, E., Oltra, R. et al. Vancomycin MICs and risk of complicated bacteremia by glycopeptide-susceptible Staphylococcus aureus. Eur J Clin Microbiol Infect Dis 38, 903–912 (2019). https://doi.org/10.1007/s10096-019-03500-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-019-03500-7