Abstract
Background
Methylenetetrahydrofolate reductase (MTHFR) gene C677T polymorphism was reported as risk factor for multiple diseases due to its role in conversion of homocysteine to methionine. The aim of the present meta-analysis was to find out the validity of association of C677T polymorphism with epilepsy susceptibility.
Methods
Pubmed, Science Direct, Springer Link and Google Scholar, databases were searched for relevant studies up to January, 31, 2018. The pooled odds ratios (ORs) with 95% confidence intervals (CIs) were performed using five genetic models. All statistical analysis was done by MetaAnalyst and Mix programs.
Results
Except recessive model, significant association was found between MTHFR C677T polymorphism and epilepsy risk in other four genetic models (T vs C: OR = 1.29, 95% CI = 1.08–1.52, p = 0.004; TT vs CC: OR = 1.48, 95% CI = 1.19–1.82, p = 0.0003; TT + CT vs CC: OR = 1.20, 95% CI = 1.05–1.38, p = 0.008; TT vs CT + CC: OR = 1.35, 95% CI = 1.11–1.62, p = 0.002). Similarly, in the subgroup analysis based on ethnicity, significant association was found in Asian (T vs C: OR = 1.85; 95% CI = 1.15–2.99; p = 0.03) and Caucasian populations (TT vs CC: OR = 1.38; 95% CI = 1.10–1.1.73; p = 0.005). No evidence of heterogeneity and publication bias was detected in present meta-analysis.
Conclusion
In conclusion, results of present meta-analysis suggested that 677T allele of MTHFR is significantly increases the epilepsy susceptibility.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Epilepsy is a common neurological disorder, triggered by abnormal electrochemical activities in the brain, resulting in seizure [2, 67]. Worldwide, about more than 65 million individuals suffer with epilepsy with more than 80% of epileptics residing in low- and middle-income countries [6, 17, 34, 60, 63, 66]. In all epileptics, about 40% cases are of idiopathic epilepsies (IEs). In idiopathic epilepsy, genetics play important role. Epilepsy is genetically heterogenous and showed autosomal dominant and recessive mode of inheritance, which suggests complex inheritance, i.e., involvement of many genes and nongenetic factors also [13, 19, 28, 56, 67].
Numerous studies have reported that hyperhomocysteinemia is a risk factor for stroke, psychiatric, and neurodegenerative diseases [14, 25]. About 10–40% epileptic patients exhibit hyperhomocysteinemia [1, 8, 10, 25, 27]. Folate is essential for DNA synthesis, methylation, and repair. It provides primary methyl donor for conversion of homocysteine in to methionine. Folate deficiency or folate pathway enzyme variants are the main cause of hyper homocysteinemia. Most of the folate/methionine genes are polymorphic, especially C677T polymorphism of methylenetetrahydrofolate reductase (MTHFR) and A66G polymorphism of methionine synthase reductase (MTRR). The frequency of these polymorphisms (C677T, A1298C and A66G) varies greatly in different populations [53, 54].
MTHFR gene is located on chromosome 1p. Several polymorphisms are reported in MTHFR gene, but C677T polymorphism is the most studied and clinically important polymorphism, in which cytosine is substituted with thymine at position 677, leading to substitution of alanine to valine (A333V). MTHFR mutant homozygous (VV) enzyme has approximately 70% decreased enzyme activity in compare to normal MTHFR enzyme [22]. MTHFR C677T polymorphism is reported as risk factor for multiple diseases- ischemic vascular disease, psychiatric and neurological diseases including Alzheimer, Parkinson’s disease, and migraine [11, 16, 38, 55, 58]. The frequency of T allele varies greatly worldwide [24, 41, 52, 70]. There are conflicting results about the role of MTHFR C677T polymorphism in epilepsy susceptibility. To derive a precise estimation of relationship between MTHFR C677T polymorphism and epilepsy risk, we conducted the present meta-analysis.
Methods
Present meta-analysis was carried out according to meta-analysis of observational studies in epidemiology (MOOSE) guidelines [61].
Literature search
The electronic databases PubMed (http://www.ncbi.nlm.nih.gov/pubmed), Science Direct (http://www.sciencedirect.com), Springer Link (http://springerlink.bibliotecabuap.elogim.com), and Google Scholar (http://scholar.google.com) were searched for eligible studies. The search terms used are “Epilepsy” and “Methylenetetrahydrofolate reductase” or “MTHFR” or “C677T.”
Inclusion and exclusion criteria
The included studies must meet the following criteria: (i) study should be published, (ii) study should be case–control study, (iii) study should evaluated MTHFR C677T polymorphism in epilepsy patients, (iv) study should report numbers of MTHFR genotypes (CC, CT, and TT) or alleles in cases and controls, and (v) epilepsy patients were diagnosed according to the clinical and electroencephalography criteria of the International League Against Epilepsy (ILAE).
Studies were excluded if (i) MTHFR genotypes/allele numbers in cases and controls were not mentioned in the study, (ii) only cases were reported, and (iii) article was review or editorials or book chapter or linkage studies.
Data extraction
Following information were extracted from each included studies like (i) first author’s family name, (ii) country name of participants, (iii) ethnicity of participants, (iv) journal’s name, (v) year of publication, (vi) number of cases and controls, (vii) MTHFR genotypes in cases and controls, and (viii) genotyping methods.
Meta-analysis
Pooled odds ratio with 95% CI were used as association measure to assess association between MTHFR C677T genotypes and risk of epilepsy using five genetic models like- additive/ allele contrast (T vs C), homozygote (TT vs CC), co-dominant/heterozygote (CT vs CC), dominant (TT + CT vs CC) and recessive (TT vs CT + CC) models. The statistical significance of the pooled OR was determined using a Z test, and p < 0.05 was considered statistically significant. The heterogeneity was tested by the Q statistic and was considered statistically significant when p < 0.05 [26]. The pooled OR was estimated using the fixed effects model when there was less heterogeneity [36] or random effects model when there was higher heterogeneity [15]. All included studies were tested for genotypic distribution of the MTHFR C677T polymorphism in the control group with the HWE principle using the χ2 test. Subgroup analysis based on ethnicity was also performed.
Publication bias was evaluated by the funnel plot of precision and standard error. Funnel plot asymmetry was further assessed by the method of Egger’s linear regression test [18]; if p < 0.05, the publication bias was statistically significant. Meta-analysis was performed using Mix [7] and MetaAnalyst [65] programs.
Results
Characteristics of included studies
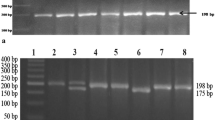
PubMed, Science direct, Springer Link, and Google Scholar databases search returned 195 articles. Initial examination involving abstracts and titles leads to the exclusion of 130 nonrelevant articles. Of the remaining 65 relevant articles, 48 articles again excluded (articles lack complete genotyping data, comments, letter to editors, not analyzed MTHFR gene, etc.). Seventeen articles were remaining, out of which five articles excluded again, because they were meta-analysis and duplicate articles. Finally, 12 studies which met the inclusion criteria were included in the present meta-analysis [4, 9, 10, 13, 23, 30, 39, 40, 57, 59, 64, 71] (Table 1; Fig. 1).
In total 12 included studies, the numbers of cases and controls were 1931 and 1985 respectively. Largest sample size was 689 [57], and lowest sample size was 18 [4]. In cases, the frequency of CC-homozygous individuals was 39.28%. However, 43.85% of CT-heterozygous individuals and 16.87% of TT-homozygous individuals displayed the C677T polymorphism. In control groups, the frequencies of CC, CT, and TT individuals were 43.4%, 43.39%, and 12.9%, respectively. The T allele frequencies in the case and control groups were 37.83% and 33.35%, respectively. All 12 studies were carried out in different countries—India [4], Italy [9, 10, 23], Japan [40], Korea [71], Poland [59], Saudi Arab [39], Spain [64], the UK [13, 30], and the USA [57] (Table 1).
Meta-analysis
In the overall analysis, significant associations were observed for the dominant model using both fixed effect (TT + CT vs CC: OR = 1.20, 95% CI = 1.05–1.38, p = 0.008) and random effect models (TT + CT vs CC, OR = 1.20, 95% CI = 1.05–1.38, p = 0.008). Meta-analysis of mutant homozygote showed strong significant association between C677T polymorphism and epilepsy risk using both fixed and random effect models (TT vs CC: OR = 1.48, 95% CI = 1.19–1.82, p = 0.0003). Results of allele contrast meta-analysis showed significant association of epilepsy risk with MTHFR T allele with both fixed effect (T vs C: OR = 1.26, 95% CI = 1.14–1.38, p < 0.0001) and random effect models (T vs C: OR = 1.29, 95% CI = 1.08–1.52, p = 0.004) (Table 2; Fig. 2). Meta-analysis using recessive model results also showed positive association between MTHFR polymorphism and epilepsy risk using both fixed and random effects models (TT vs CT + CC: OR = 1.35, 95% CI = 1.11–1.62, p = 0.002), but co-dominant model meta-analysis did not show any association (CT vs CC: OR = 1.13, 95% CI = 0.98–1.30, p = 0.10) (Table 2). In cumulative analysis using fixed and random effect models, the association of mutant “T” allele with epilepsy remained statistically significant with the addition of new study (Fig. 3).
Heterogeneity analysis
The between studies heterogeneity of different genetic models was analyzed for 12 case–control studies. The results in allele contrast model (p = 0.03; I2 = 60.06), homozygote model (p = 0.69; I2 = 0), dominant model (p = 0.47; I2 = 0), recessive model (p = 0.50; I2 = 0), and heterozygote model (p = 0.77; I2 = 0) had no heterogeneity.
Subgroup analysis
Out of 12 included studies, four studies were from Asian population (393 cases/318 controls) and eight studies were from Caucasian population (1538 cases/1667 controls). Meta-analysis of Caucasian studies showed that the T allele was significantly associated with epilepsy risk using homozygote model (TT vs CC: OR = 1.38; 95% CI = 1.10–1.73; p = 0.005) and allele contrast model (T vs C: OR = 1.14; 95% CI = 1.04–1.28; p = 0.02) (T vs C) (Table 2; Fig. 4). In addition, meta-analysis of Asian population also indicated that the T allele was strongly associated with epilepsy risk using allele contrast (T vs C: OR = 1.85; 95% CI = 1.15–2.99; p = 0.03) and homozygote model (TT vs CC: OR = 2.19; 95% CI = 1.2–2.30; p = 0.005) (Table 2; Fig. 5).
Publication bias
The shapes of Funnel plots did not reveal any asymmetry (Figs. 6 and 7). p value of Eggers test was > 0.05 and also did not suggest any publication bias (T vs C: p = 0.52; TT vs CC: p = 0.70; CT vs CC: p = 0.92; CT + TT vs CC: p = 0.94; and TT vs CT + CC: p = 0.58).
Discussion
Twelve case–control studies with 1731 epilepsy cases and 1885 controls were included in the present meta-analysis. The results of current meta-analysis indicated that the T allele of MTHFR gene was significantly associated with risk of epilepsy. The mechanism of epileptogenesis has not been clearly known [12], but several reports supported the homocysteine hypothesis of epilepsy [5]. Folate deficiency or reduced activity of MTHFR enzyme may lead to increased serum Hcy levels [29, 62]. MTHFR C677T polymorphism and its association with increased epilepsy risk are due to higher concentration of homocysteine. Higher homocysteine concentration stimulates N-methyl-d-aspartate (NMDA) receptors and by mediating excitotoxicity produces free radicals, which causes neuronal death [21, 31]. In addition, metabolite of homocysteine like homocysteic acid and l-Hcy sulfinic acid interacts with glutamate receptor and exhibits excitotoxicity [20, 35]. Experiments with animal models also supported the homocysteine hypothesis of epilepsy like (i) administration of high doses of Hcy produces convulsive seizures, a fact that has been exploited in models of experimental epilepsy [32]; (ii) Hcy sequesters adenosine, an endogenous anticonvulsant [37]; and (iii) Hcy potentiates pilocarpine in inducing status epilepticus [5].
Meta-analysis is an acceptable useful methodology suitable for elucidating genetic factors in different diseases/disorders. The individual studies are usually small and underpowered and, thus, unable to provide a definite answer even in the case where a true association exists [3]. Several meta-analyses were published which evaluated risk of folate pathway genes polymorphism for different disease and disorders like Down syndrome [41], orofacial clefts [49], male infertility [50], recurrent pregnancy loss [45], autism [48], schizophrenia [68], bipolar [42], depression [44], Alzheimer’s disease [47], breast cancer [33, 43], prostate cancer [67], and colorectal cancer [46].
Certain potential limitations exist in our meta-analysis, which should be acknowledged—(i) present meta-analysis based on unadjusted data, (ii) only 12 studies were included, (iii) single gene polymorphism was considered, (iv) interactions between gene–gene and gene–environment could not be included in present meta-analysis due to a lack of relative data, and (v) only four databases were searched, so it might be possible that few relevant studies were left. Besides limitations, present meta-analysis has several strengths also like absence of publication bias and heterogeneity etc.
In conclusion, results of the present meta-analysis suggested that there are strong significant associations between the MTHFR C677T polymorphism and epilepsy susceptibility. Folate deficiency and folate pathway hypofunctional enzymes especially MTHFR are the main risk factor for hyperhomocysteinemia, and C677T polymorphism reduces ~ 70% enzyme activity; hence, individuals with TT genotype are higher risk of epilepsy due to higher homocysteine concentration. Further studies with large sample sizes and a well designed case–control stratified by ethnicity are warranted to confirm present findings.
References
Apeland T, Mansoor MA, Pentieva K, McNulty H, Strandjord RE (2003) Fasting and post-methionine loading concentrations of homocysteine, vitamin B2, and vitamin B6 in patients on antiepileptic drugs. Clin Chem 49:1005–1008
Avoli M, D’Antuono M, Louvel J, Köhling R, Biagini G, Pumain R, D’Arcangelo G, Tancredi V (2002) Network and pharmacological mechanisms leading to epileptiform synchronization in the limbic system in vitro. Prog Neurobiol 68(3):167–207
Bagos PG (2009) Plasminogen activator inhibitor-1 4G/5G and 5,10-methylenetetrahydrofolate reductase C677T polymorphisms in polycystic ovary syndrome. Mol Hum Reprod 15:19–26
Balamuralikrishnan B, Balachandar V, Mohana Devi S, Karthic Kumar A, Mustaq Ahammed SAK, Sasikala K (2013) Cytogenetic evaluation in epilepsy patients correlated with MTHFR C677T gene mutation and frequency of homocysteine levels. WCN 333:e44–e45. https://doi.org/10.1016/j.jns.2013.07.161
Baldelli E, Leo G, Andreoli N, Fuxe K, Biagini G, Agnati LF (2010) Homocysteine potentiates seizures and cell loss induced by pilocarpine treatment. NeuroMolecular Med 12(3):248–259
Banerjee PN, Filippi D, Allen Hauser W (2009) The descriptive epidemiology of epilepsy-a review. Epilepsy Res 85(1):31–45
Bax L, Yu LM, Ikeda N, Tsuruta H, Moons KG (2006) Development and validation of MIX: comprehensive free software for meta-analysis of causal research data. BMC Med Res Methodol 6:50
Belcastro V, Gorgone G, Italiano D, Oteri G, Caccamo D, Pisani LR et al (2007) Antiepileptic drugs and MTHFR polymorphisms influence hyper-homocysteinemia recurrence in epileptic patients. Epilepsia 48:1990–1994
Belcastro V, Striano P, Gorgone G, Costa C, Ciampa C, Caccamo D, Pisani LR, Oteri G, Marciani MG, Aguglia U, Striano S, Ientile R, Calabresi P, Pisani F (2010) Hyperhomocysteinemia in epileptic patients on new antiepileptic drugs. Epilepsia 51:274–279
Caccamo D, Condello S, Gorgone G, Crisafulli G, Belcastro V, Gennaro S, Striano P, Pisani F, Ientile R (2004) Screening for C677T and A1298C MTHFR polymorphisms in patients with epilepsy and risk of hyperhomocysteinemia. NeuroMolecular Med 6:117–126
Cronin S, Furie KL, Kelly PJ (2005) Dose-related association of MTHFR 677T allele with risk of ischemic stroke: evidence from a cumulative meta-analysis. Stroke 36:1581–1587
Curia G, Lucchi C, Vinet J, Gualtieri F, Marinelli C, Torsello A, Costantino L, Biagini G (2014) Pathophysiogenesis of mesial temporal lobe epilepsy: is prevention of damage antiepileptogenic? Curr Med Chem 21(6):663–688
Dean JC, Robertson Z, Reid V, Wang Q, Hailey H, Moore S et al (2008) A high frequency of the MTHFR 677C > T polymorphism in Scottish women with epilepsy: possible role in pathogenesis. Seizure 17:269–275
den Heijer T, Vermeer SE, Clarke R, Oudkerk M, Koudstaal PJ, Hofman A, Breteler MMB (2003) Homocysteine and brain atrophy on MRI of non-demented elderly. Brain 126:170–175
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
Diaz-Arrastia R (2000) Homocysteine and neurologic disease. Arch Neurol 57:1422–1427
Duncan JS, Sander JW, Sisodiya SM, Walker MC (2006) Adult epilepsy. Lancet 367:1087–1100
Egger M, Smith DJ, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634
Engel J (2001) A proposed diagnostic scheme for people with epileptic seizures and epilepsy: report of the ILEA task force on classification and terminology. Epilepsia 42:796–803
Flott-Rahmel B, Schurmann M, Schluff P, Fingerhut R, Musshoff U, Fowler B et al (1998) Homocysteic and homocysteine sulphinic acid exhibit excitotoxicity in organotypic cultures from rat brain. Eur J Pediatr 157(2):112–117
Folbergrova J (1997) Anticonvulsant action of both NMDA and non-NMDA receptor antagonists against seizures induced by homocysteine in immature rats. Exp Neurol 145:442–450
Frosst P, Blom HJ, Milos R, Goyette P, Sheppard CA, Matthews RG, Boers GJH, den Heijer M, Kluijtmans LAJ, van den Heuve LP, Rozen R (1995) A candidate genetic risk factor for vascular disease: a common mutation in methylenetetrahydrofolate reductase. Nat Genet 10:111–113
Gorgone G, Caccamo D, Pisani LR, Curro M, Parisi G, Oteri G et al (2009) Hyperho-mocysteinemia in patients with epilepsy: does it play a role in the pathogenesis of brain atrophy? A preliminary report. Epilepsia 50:33–36
Hegele RA, Tully C, Young TK, Connelly PW (1997) V677 mutation of methylenetetrahydrofolate reductases and cardiovascular disease in Canadian Inuit. Lancet 34:1221–1222
Herrmann W, Herrmann M, Obeid R (2007) Hyperhomocysteinaemia: a critical review of old and new aspects. Curr Drug Metab 8:17–31
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558
Huemer M, Ausserer B, Graninger G, Hubmann M, Huemer C, Schlachter K (2005) Hyperhomocysteinemia in children treated with antiepileptic drugs is normalized by folic acid supplementation. Epilepsia 46:1677–1683
Johnson MR, Sander JWAS (2001) The clinical impact of epilepsy genetics. J Neurol Neurosurg Psychiatry 70:428–430
Karabiber H, Sonmezgoz E, Ozerol E, Yakinci C, Otlu B, Yologlu S (2003) Effects of valproate and carbamazepine on serum levels of homocysteine, vitamin B12,and folic acid. Brain and Development 25:113–115
Kini U, Lee R, Jones A, Smith S, Ramsden S, Fryer A, Clayton-Smith J (2007) Influence of the MTHFR genotype on the rate of malformations following exposure to antiepileptic drugs in utero. Eur J Med Genet 50:411–420
Kruman II, Culmsee C, Chan SL, Kruman Y, Guo Z, Penix L, Mattson MP (2000) Homocysteine elicits a DNA damage response in neurons that promotes apoptosis and hypersensitivity to excitotoxicity. J Neurosci 20:6920–6926
Kubova H, Folbergrova J, Mares P (1995) Seizures induced by homocysteine in rats during ontogenesis. Epilepsia 36:750–756
Kumar P, Yadav U, Rai V (2016) Methylenetetrahydrofolate reductase gene C677T polymorphism and breast cancer risk: evidence for genetic susceptibility. Meta Gene 6:2–84
Kwan P, Brodie MJ (2001) Neuropsychological effects of epilepsy and antiepileptic drugs. Lancet 357:216–222
Lipton SA, Kim WK, Choi YB, Kumar S, D’Emilia DM, Rayudu PV et al (1997) Neurotoxicity associated with dual actions of homocysteine at the N-methyl-D-aspartate receptor. Proc Natl Acad Sci U S A 94(11):5923–5928
Mantel N, Haenszel W (1959) Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst 22(4):719–748
Marangos PJ, Loftus T, Wiesner J, Lowe T, Rossi E, Browne CE, Gruber HE (1990) Adenosinergic modulation of homocysteine-induced seizures in mice. Epilepsia 31(3):239–246
Mattson MP, Shea TB (2003) Folate and homocysteine metabolism in neural plasticity and neurodegenerative disorders. Trends Neurosci 26:137–146
Munisamy M, Al-Gahtany M, Tripathi M, Subbiah (2015) Impact of MTHFR (C677T) gene polymorphism on antiepileptic drug monotherapy in North Indian epileptic population. Ann Saudi Med 35(1):51–57
Ono H, Sakamoto A, Mizoguchi N, Sakura N (2000) Methylenetetrahydrofolate reductase 677C>T and epilepsy. J Inherit Metab Dis 23:525–526
Pepe G, Camacho Vanegas O, Giusti B, Brunelli T, Marcucci R, Attanasio M, Rickards O, de Stefano GF, Prisco D, Gensini GF, Abbate R (1998) Heterogeneity in world distribution of the thermolabile C677T mutation in 5,10-methylenetetrahydrofolate reductase. Am J Hum Genet 63:917–920
Rai V (2011a) Polymorphism in folate metabolic pathway gene as maternal risk factor for down syndrome. Int J Biol Med Res 2(4):1055–1060
Rai V (2011b) Evaluation of methylenetetrahydrofolate reductase gene variant (C677T) as risk factor for bipolar disorder. Cell Mol Biol 57:1558–1566
Rai V (2014a) Methylenetetrahydrofolate reductase A1298C polymorphism and breast cancer risk: a meta-analysis of 33 studies. Ann Med Health Sci Res 4(6):841–851
Rai V (2014b) Genetic polymorphisms of methylenetetrahydrofolate reductase (MTHFR) gene and susceptibility to depression in Asian population: a systematic meta-analysis. Cell Mol Biol 60(3):29–36
Rai V (2016a) Methylenetetrahydrofolate reductase C677T polymorphism and recurrent pregnancy loss risk in Asian population: a meta-analysis. Ind J Clin Biochem 31:402–413
Rai V (2016b) Evaluation of the MTHFR C677T polymorphism as a risk factor for colorectal cancer in Asian populations. Asian Pac J Cancer Prev 16(18):8093–8100
Rai V (2016c) Methylenetetrahydrofolate reductase (MTHFR) C677T polymorphism and Alzheimer disease risk: a meta-analysis. Mol Neurobiol 54(2):1173–1186
Rai V (2016d) Association of methylenetetrahydrofolate reductase (MTHFR) gene C677T polymorphism with autism: evidence of genetic susceptibility. Metab Brain Dis 31:727–735
Rai V (2017) Strong association of C677T polymorphism of methylenetetrahydrofolate reductase gene with nosyndromic cleft lip/palate (nsCL/P). Ind J Clin Biochem 33(1):5–15
Rai V, Kumar P (2017) Methylenetetrahydrofolate reductase C677T polymorphism and risk of male infertility in Asian population. Ind J Clin Biochem 32(3):253–226
Rai V, Yadav U, Kumar P, Yadav SK (2010) Methylenetetrahydrofolate reductase polymorphism (C677T) in Muslim population of Eastern Uttar Pradesh, India. Ind J Med Sci 64(5):219–223
Rai V, Yadav U, Kumar P (2012) Genotype prevalence and allele frequencies of 5,10-methylenetetrahydrofolate reductase (MTHFR) C677T mutation in two caste groups of India. Cell Mol Biol 58:OL1695–OL1701
Rai V, Yadav U, Kumar P, Yadav SK (2013) Analysis of methionine synthase reductase polymorphism (A66G) in Indian Muslim population. Ind J Hum Genet 19(2):183–187
Rubino E, Ferrero M, Rainero I, Binello E, Vaula G, Pinessi L (2007) Association of the C677T polymorphism in the MTHFR gene with migraine: a meta-analysis. Cephalalgia 29:807–808
Scheffer IE, Berkowic SF (2003) The genetics of human epilepsy. Trends Pharmacol Sci 24:428–433
Scher AI, Wu H, Tsao JW, Blom HJ, Feit P, Nevin RL, Schwab KA (2011) MTHFR C677T genotype as a risk factor for epilepsy including post-traumatic epilepsy in a representative military cohort. J Neurotrauma 28:1739–1745
Schurks M, Rist PM, Kurth T (2010) MTHFR 677C > T and ACE D/I polymorphisms in migraine: a systematic review and meta-analysis. Headache 50:588–599
Sniezawska A, Dorszewska J, Rozycka A, Przedpelska-Ober E, Lianeri M, Jagodzinski PP, Kozubski W (2011) MTHFR, MTR, and MTHFD1 gene polymorphisms compared to homocysteine and asymmetric dimethylarginine concentrations and their metabolites in epileptic patients treated with antiepileptic drugs. Seizure 20:533–540
Song P, Liu Y, Yu X, Wu J, Poon AN, Demaio A, Wang W, Rudan I, Chan KY (2017) Prevalence of epilepsy in China between 1990 and 2015: a systematic review and meta-analysis. J Glob Health 7(2):020706. https://doi.org/10.7189/jogh.07.020706
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 283(15):2008–2012
Tamura T, Aiso K, Johnston KE, Black L, Faught E (2000) Homocysteine, folate, vitamin B12 and vitamin B6 in patients receiving antiepileptic drug monotherapy. Epilepsy Res 40:7–15
Thurman DJ, Beghi E, Begley CE, Berg AT, Buchhalter JR, Ding D, Hesdorffer DC, Hauser WA, Kazis L, Kobau R, Kroner B, Labiner D, Liow K, Logroscino G, Medina MT, Newton CR, Parko K, Paschal A, Preux PM, Sander JW, Selassie A, Theodore W, Tomson T, Wiebe S, for the ILAE Commission on Epidemiology (2011) Standards for epidemiologic studies and surveillance of epilepsy. Epilepsia 52:2–26
Vilaseca MA, Monros E, Artuch R, Colome C, Farre C, Valls C et al (2000) Anti-epileptic drug treatment in children: hyperhomocysteinaemia, B-vitamins and the 677C!T mutation of the methylenetetrahydrofolate reductase gene. Eur J Paediatr Neurol 4:269–277
Wallace BC, Dahabreh IJ, Trikalinos TA, Lau J, Trow P, Schmid CH (2013) Closing the gap between methodologists and end-users: R as a computational back-end. J Stat Software 49:1–15
World Health Organization (2001) International classification of functioning, disability and health. World Health Organization, Geneva
Xu YL, Li XX, Zhuang SJ, Guo SF, Xiang JP, Wang L et al (2018) Significant association of BDNF rs6265 G-->A polymorphism with susceptibility to epilepsy: a meta-analysis. Neuropsychiatr Dis Treat 14:1035–1046
Yadav U, Kumar P, Rai V (2016a) Role of MTHFR A1298C gene polymorphism in the etiology of prostate cancer: a systematic review and updated meta-analysis. Egyptian J Med Hum Genet 17(2):141–148
Yadav U, Kumar P, Gupta S, Rai V (2016b) Role of MTHFR C677T gene polymorphism in the susceptibility of schizophrenia: an updated meta-analysis. Asian J Psychiatry 20:41–51
Yadav U, Kumar P, Gupta S, Rai V (2017) Distribution of MTHFR C677T gene polymorphism in healthy North Indian population and an updated meta-analysis. Ind J Clin Biochem 32(4):399–410
Yoo JH, Hong SB (1999) A common mutation in the methylenetetrahydrofolate reductase gene is a determinant of hyperhomocysteinemia in epileptic patients receiving anticonvulsants. Metabolism 48:1047–1051
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Rai, V., Kumar, P. Methylenetetrahydrofolate reductase C677T polymorphism and susceptibility to epilepsy. Neurol Sci 39, 2033–2041 (2018). https://doi.org/10.1007/s10072-018-3583-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-018-3583-z