Abstract
Contrast-enhanced magnetic resonance imaging with maximum intensity projection (MRI-MIP) is an easy, useful imaging method to evaluate synovitis in rheumatoid hands. However, the prognosis of synovitis-positive joints on MRI-MIP has not been clarified. The aim of this study was to evaluate the relationship between synovitis visualized by MRI-MIP and joint destruction on X-rays in rheumatoid hands. The wrists, metacarpophalangeal (MP) joints, and proximal interphalangeal (PIP) joints of both hands (500 joints in total) were evaluated in 25 rheumatoid arthritis (RA) patients. Synovitis was scored from grade 0 to 2 on the MRI-MIP images. The Sharp/van der Heijde score and Larsen grade were used for radiographic evaluation. The relationships between the MIP score and the progression of radiographic scores and between the MIP score and bone marrow edema on MRI were analyzed using the trend test. As the MIP score increased, the Sharp/van der Heijde score and Larsen grade progressed severely. The rate of bone marrow edema-positive joints also increased with higher MIP scores. MRI-MIP imaging of RA hands is a clinically useful method that allows semi-quantitative evaluation of synovitis with ease and can be used to predict joint destruction.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Evaluation of synovitis in the hands is of great importance in diagnosing rheumatoid arthritis (RA) and evaluating disease activity. Synovitis has traditionally been evaluated from physical findings, particularly palpation and observation. With recent advances in RA treatment, early diagnosis and treatment have become more important and this requires earlier and more accurate evaluation of synovitis in the hands [1, 2]. For this reason, magnetic resonance imaging (MRI) and ultrasonography (US) are now used for synovitis evaluation in RA [2, 3]. These diagnostic imaging techniques are useful for early diagnosis and prediction of joint destruction, because they are able to identify synovitis with greater sensitivity and accuracy than physical findings [4–6].
Contrast-enhanced MRI can visualize synovitis in great detail, and evaluation of synovitis by contrast-enhanced MRI is useful for early diagnosis, evaluation of disease activity, and prediction of joint destruction, because bone erosion and joint space narrowing are invariably preceded by synovitis. Quantitative evaluation of synovitis is important because the severity of synovitis has been found to correlate with the volume of hypertrophic synovial membrane [7]. A method for quantifying synovitis has been reported by OMERACT [8], but despite being very important because it allows detailed and accurate evaluation, this method is not convenient clinically because the interpretation of the images is time-consuming.
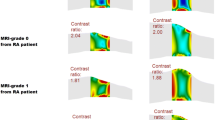
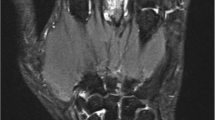
We use maximum intensity projection (MIP) as a method for reconstructing contrast-enhanced MRI of RA hands. MIP is a method of image processing in which the brightest regions of different slices are superimposed on each other to create a single, three-dimensional (3D) image [9]. Contrast-enhanced MRI with MIP (MRI-MIP) of the hand in RA provides clear visualization of synovitis and also enables differentiation of articular synovitis and tenosynovitis anatomically [10, 11]. A single MIP image of the hands allows observation of the whole of both hands, like plain radiographs (Fig. 1); we have previously reported the usefulness of MRI-MIP of the hand for the early diagnosis of RA [11] and evaluating synovitis; the agreement on the synovitis score between MIP and conventional MRI was excellent [12]. However, these previous studies did not clarify whether MRI-MIP images could be directly used for prediction of joint destruction. The objective of the present study was to elucidate the relationship between synovitis in RA hands visualized by MRI-MIP and the radiographic prediction of joint destruction.
Materials and methods
Patients
The subjects in this study were RA patients who had undergone plain hand radiographs and contrast-enhanced MRI scans as outpatients at our hospital between 2010 and 2012 and who then underwent plain radiographs of both hands after a minimum of 1 year. All patients fulfilled the ACR1987 rheumatoid arthritis classification criteria. This study was approved by the ethics committee of Kyoto Prefectural University of Medicine, and informed consent was obtained from all patients.
Radiographs
Radiographs were taken of both hands of all patients when the MRI scans were done and at least 1 year after MRI was performed. Imaging was done by standard methods in the posteroanterior view with both hands pronated. The joint space narrowing (JSN) score (score 0–4) was scored at 15 sites, and bone erosion was scored (score 0–5) at 16 sites using a Sharp/van der Heijde scoring system [13, 14]. For metacarpophalangeal (MP) joints and proximal interphalangeal (PIP) joints, each joint was evaluated separately, but the sum of the JSN scores for six sites in the wrist was taken as the wrist JSN score and the sum of the erosion scores for six sites in the wrist was taken as the wrist erosion score. A Larsen grade (grade 0–5) was also given with reference to standard X-ray films [15] for MP joints, PIP joints, and wrists. Evaluations were made using plain radiographs taken when the MRI scans were done and at follow-up. The images were read and scored separately by two orthopedic surgery specialists trained in the scoring method without reference to any other clinical information.
MRI scans
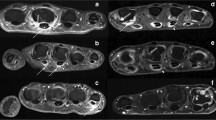
Contrast-enhanced MRI was performed of both hands of all patients using a 1.5-T clinical scanner (EXCELART Vantage powered by Atlas; Toshiba, Tokyo, Japan) with an Atlas SPEEDER 16-channel phased array coil. Patients were scanned in the supine position with both hands resting on their thighs. First, a non-contrast STIR, a T1-weighted image (T1WI), and a T2WI coronal scan were taken. Then, 0.1 mmol gadoteridol/kg body weight (Prohance, Eisai, Tokyo, Japan) was administered intravenously, and within 3 min, a fat-suppressed contrast-enhanced 3D gradient echo TIWI was performed under the following conditions: repetition time/echo time (TR/TE) = 5.5/2.5 ms, number of acquisitions = 1, slice thickness = 2 mm, field-of-view = 350 mm × 350 mm, acquisition matrix = 256 × 256, and acquisition time = approximately 3 min 40 s. The MIP image was reconstructed from the fat-suppressed contrast-enhanced 3D gradient echo. Synovitis scores from the MIP images were classified for each joint (wrist, MP, PIP) from grade 0 to grade 2 (grade 0: no enhancement, grade 1: partial enhancement of the joint, grade 2: full enhancement of the joint) as reported previously (Fig. 1) [12]. Bone marrow edema was also seen as enhancement on contrast-enhanced MRI, but the contrast effect was weaker than that of synovitis, with almost equal enhancement to surrounding soft tissue. MIP is a method of image processing in which the brightest regions of different slices are superimposed; thus, the MIP image visualized almost only synovitis. Therefore, the presence or absence of bone marrow edema was also evaluated from STIR images. The two orthopedic surgery specialists were blinded to patient information and separately judged the MIP scores and the presence or absence of bone marrow edema.
Statistical analysis
The baseline characteristics of the study group are reported as mean values for continuous variables including standard deviations. Levels of agreement for the radiographic score, MIP score, and bone marrow edema were estimated using the weighted kappa statistic. A κ value of 0–0.40 denotes poor agreement, 0.41–0.60 moderate, 0.61–0.80 substantial, and 0.81 or higher excellent agreement. If the score for an image differed between the two readers, the final score decision was made after discussion between the two examiners. The relationship between MIP scores and progression of radiographic scores (JSN score, bone erosion score, Larsen grade) was tested to investigate whether joint destruction progression was correlated with higher MIP scores. The Cochran-Armitage test was used to investigate the proportion of progressed joints at each MIP score, and the Jonckheere test was used to investigate the mean progressed score (sum of radiographically progressed scores/total number of joints) at each MIP score. The Cochran-Armitage test was also used to investigate the proportion of bone marrow edema-positive joints at each MIP score, in order to investigate whether the presence of bone marrow edema increased with higher MIP scores. The Jonckheere test was used to investigate whether joint destruction had progressed more in bone marrow edema-positive than in -negative joints. The significance level was set at P < 0.05 for all tests. All statistical analyses were performed using R, version 3.0.2 (R Foundation for Statistical Computing, Vienna, Austria).
Results
A total of 500 joints (wrist, MP, and PIP joints) were studied in 25 RA patients. There were 4 male and 21 female subjects, with a mean age of 61.2 ± 9.8 years (range 37–80 years). The mean disease duration was 10.1 ± 11.3 years (range 1 month to 45 years). Steinbrocker classifications were stage 1 for 8 patients, stage 2 for 4, stage 3 for 5, and stage 4 for 8, and class 1 for 12, class 2 for 11, class 3 for 1, and class 4 for 1. When contrast-enhanced MRI scans were performed, the mean disease activity score (DAS) 28-CRP score for the study group was 2.68 ± 1.16 (range 0.96–5.37). There were 9 patients in remission with DAS28-CRP scores less than 2.3, 3 with low disease activity with scores of 2.3–2.7, 11 with moderate disease activity with scores of 2.7–4.1, and 2 with high disease activity with scores of more than 4.1. When MRI scans were performed, 17 patients were receiving methotrexate (MTX) monotherapy, 2 patients were receiving MTX + tacrolimus (TAC), 2 patients were receiving MTX + salazosulfapyridine (SASP), 1 patient was receiving prednisolone (PSL) + SASP, 1 patient was receiving PSL + TAC, and 2 patients were receiving MTX + etanercept (ETN). The period from MRI scans to follow-up radiographs was 20 ± 6 months (range 12–34 months).
Interobserver agreement was excellent for the JSN score (κ value 0.85), erosion score (0.83), Larsen grade (0.84), MIP score (0.92), and bone marrow edema (0.91), with κ values of more than 0.81. In a total of 500 joints, 348 joints had MIP score 0, 71 joints had MIP score 1, and 81 joints had MIP score 2. The numbers of joints whose JSN score had progressed were 20 (5.7 %) with MIP score 0, 14 (19.7 %) with MIP score 1, and 25 (30.9 %) with MIP score 2 (Table 1). The proportion of joints with a progressed JSN score increased significantly with higher MIP scores. The mean progressed JSN scores were 0.0632 for MIP score 0, 0.2535 for MIP score 1, and 0.6172 for MIP score 2, showing that the mean progressed JSN score was significantly greater as the basic MIP score increased (Fig. 2a).
The numbers of joints whose bone erosion score had progressed were 36 (10.3 %) with MIP score 0, 13 (18.3 %) with MIP score 1, and 30 (37 %) with MIP score 2 (Table 1). The mean progressed bone erosion scores were 0.1063, 0.2676, and 0.9753, respectively (Fig. 2b). Similarly, the proportion of joints with progressed bone erosion scores increased significantly as the MIP score increased, and the mean progress score also increased.
The numbers of joints whose Larsen grade had progressed were 20 (5.7 %) with MIP score 0, 10 (14.1 %) with MIP score 1, and 16 (19.8 %) with MIP score 2 (Table 1). The mean progressed grades were 0.0689, 0.1690, and 0.2592, respectively (Fig. 2c). The proportion of joints with progressed Larsen grades was significantly higher as the MIP score increased, and the mean progressed grade was also greater as the MIP score increased.
Bone marrow edema was seen in 69 joints, of which there were 3 joints (0.9 %) with MIP score 0, 12 joints (16.9 %) with MIP score 1, and 54 joints (66.7 %) with MIP score 2. The proportion of bone marrow edema-positive joints was significantly greater as the MIP score increased (Table 1). Sixty-six of the 69 bone marrow edema-positive joints (96 %) were included among the MIP-positive joints. Among the 69 bone marrow edema-positive joints, progression of destruction was seen in 27 joints (39.1 %) based on the JSN score, 26 joints (37.7 %) based on the erosion score, and 13 joints (18.8 %) based on the Larsen grade. Progression of joint destruction was significantly greater in bone marrow edema-positive than in -negative joints (Table 2).
Discussion
Evaluation of synovitis is the most important step in RA diagnosis or assessing disease activity. Advances in RA treatments have been accompanied by widespread use of diagnostic imaging techniques such as US and contrast-enhanced MRI for evaluating synovitis, because these techniques can evaluate synovitis with greater sensitivity than conventional physical findings [3, 5, 16]. US and MRI findings are also used as predictors of joint destruction, and there is evidence that power Doppler (PD)-positive findings in ultrasonography correlate with radiograph-based prognosis [17, 18], and that the MRI-measured volume of hypertrophic synovial membrane correlates with joint destruction [7]. We have been using MRI-MIP images for early diagnosis and evaluation of RA disease activity, because it is a convenient method that allows evaluation of synovitis over the whole of both hands on a single image [11, 12]. Like US and contrast-enhanced MRI, MRI-MIP images of RA hands can detect synovitis with greater sensitivity than physical findings and we have previously reported that scoring of MIP images correlates with synovitis evaluation in normal contrast-enhanced MRI and with PD scores on US [12]. The inter-reader MIP score agreement rate was excellent, indicating that synovitis scoring on MIP images may be easier than by conventional methods. We therefore decided that the correlation between MIP scores and joint prognosis from radiographs needed to be investigated.
The present results clearly showed that the proportion of joints with progression of destruction based on the JSN score, bone erosion score, and Larsen grade increased as the MIP score increased. The mean progressed score and grade also increased with higher MIP scores, demonstrating that the extent of joint destruction was also higher as the MIP score increased. These findings suggest that higher MIP scores are associated with more severe synovitis and a greater risk of joint destruction. These results are similar to those of previous studies using PD and contrast-enhanced MRI [7, 17]. MRI-MIP images of RA hands thus allow synovitis to be easily diagnosed over the whole of both hands on a single image, provide a convenient way of semi-quantitatively evaluating synovitis, and they are useful for predicting joint destruction.
In addition to synovitis, bone marrow edema has also been reported as an imaging finding that predicts joint destruction [3, 19, 20] and bone marrow edema findings on MRI have been shown to correlate with severity of synovitis on US [21]. It was also confirmed that the progress of joint destruction was significantly greater in bone marrow edema-positive joints than in bone marrow edema-negative joints, and that the proportion of bone marrow edema-positive joints was significantly greater as the MIP score increased in this study. Most of the bone marrow edema-positive joints were included among the MIP-positive joints, and bone marrow edema was seen in 67 % of joints with MIP score 2, suggesting that, in addition to severe synovitis, MIP score 2 joints were likely to have bone marrow edema.
Although the first goal of RA treatment is to achieve clinical remission, progression of joint destruction has been reported even during remission [22]. In a 5-year follow up of RA hands, we similarly found progression of joint destruction regardless of disease activity [23]. Our results indicated that joint destruction might be progressing in patients in remission who show synovitis on MRI-MIP images. This suggests that it may be necessary to intensify treatment for patients with MIP-positive joints. However, joints with MIP score 2 included both joints that showed progression of joint destruction and joints that did not. A limitation of this study was that it was not possible to elucidate the cause of this variation. One of the causes may have been differences in the effects of treatment. Biologic agents have been found to be more effective for controlling the progression of joint destruction than MTX monotherapy [24, 25]. However, the number of subjects taking biologic agents was too small, and it was therefore not possible to investigate the differences resulting from their use, but it is possible that joint destruction was affected by treatment-induced changes in synovitis, regardless of the use of biologic agents. To clarify this, we would need to perform MRI-MIP images again and evaluate the results. Differences in the extent of baseline joint destruction in each joint may also have had an effect. It has been reported that joints that have undergone a certain degree of destruction are at a higher risk of further destruction regardless of treatment [18, 26]. To clarify this, it will be necessary to study cases with the same level of joint destruction at baseline.
In conclusion, higher MIP scores on MRI-MIP images of RA hands were associated with a higher risk of joint destruction, greater extent of joint destruction, and a higher number of joints with bone marrow edema. Evaluation of MRI-MIP images of RA hands is a clinically useful method that allows semi-quantitative evaluation of synovitis and can be used to predict joint destruction.
References
Smolen JS, Landewé R, Breedveld FC et al (2014) EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2013 update. Ann Rheum Dis 73:492–509. doi:10.1136/annrheumdis-2013-204573
Kawashiri S, Suzuki T, Okada A et al (2013) Musculoskeletal ultrasonography assists the diagnostic performance of the 2010 classification criteria for rheumatoid arthritis. Mod Rheumatol 23:36–43. doi:10.1007/s10165-012-0628-7
Colebatch AN, Edwards CJ, Østergaard M et al (2013) EULAR recommendations for the use of imaging of the joints in the clinical management of rheumatoid arthritis. Ann Rheum Dis 72:804–814. doi:10.1136/annrheumdis-2012-203158
Nakagomi D, Ikeda K, Okubo A et al (2013) Ultrasound can improve the accuracy of the 2010 American College of Rheumatology/European League against rheumatism classification criteria for rheumatoid arthritis to predict the requirement for methotrexate treatment. Arthritis Rheum 65:890–898. doi:10.1002/art.37848
Østergaard M, Ejbjerg B, Szkudlarek M (2005) Imaging in early rheumatoid arthritis: roles of magnetic resonance imaging, ultrasonography, conventional radiography and computed tomography. Best Pract Res Clin Rheumatol 19:91–116. doi:10.1016/j.berh.2004.08.006
Ostergaard M, Ejbjerg B (2004) Magnetic resonance imaging of the synovium in rheumatoid arthritis. Semin Musculoskelet Radiol 8:287–299. doi:10.1055/s-2004-861576
Ostergaard M, Hansen M, Stoltenberg M et al (1999) Magnetic resonance imaging-determined synovial membrane volume as a marker of disease activity and a predictor of progressive joint destruction in the wrists of patients with rheumatoid arthritis. Arthritis Rheum 42:918–929. doi:10.1002/1529-0131(199905)42:5<918::AID-ANR10>3.0.CO;2-2
McQueen F, Lassere M, Edmonds J et al (2003) OMERACT Rheumatoid Arthritis Magnetic Resonance Imaging Studies. Summary of OMERACT 6 MR Imaging Module. J Rheumatol 30:1387–1392
Fishman EK, Ney DR, Heath DG et al (2006) Volume rendering versus maximum intensity projection in CT angiography: what works best, when, and why. Radiographics 26:905–922. doi:10.1148/rg.263055186
Li X, Liu X, Du X, Ye Z (2014) Diagnostic performance of three-dimensional MR maximum intensity projection for the assessment of synovitis of the hand and wrist in rheumatoid arthritis: a pilot study. Eur J Radiol 83:797–800. doi:10.1016/j.ejrad.2014.02.004
Mori G, Tokunaga D, Takahashi KA et al (2008) Maximum intensity projection as a tool to diagnose early rheumatoid arthritis. Mod Rheumatol 18:247–251. doi:10.1007/s10165-008-0043-2
Taniguchi D, Tokunaga D, Oda R et al (2014) Maximum intensity projection with magnetic resonance imaging for evaluating synovitis of the hand in rheumatoid arthritis: comparison with clinical and ultrasound findings. Clin Rheumatol 33:911–917. doi:10.1007/s10067-014-2526-1
Van der Heijde DM (1996) Plain X-rays in rheumatoid arthritis: overview of scoring methods, their reliability and applicability. Baillieres Clin Rheumatol 10:435–453
Van der Heijde D (1999) How to read radiographs according to the Sharp/van der Heijde method. J Rheumatol 26:743–745
Larsen A, Dale K, Eek M (1977) Radiographic evaluation of rheumatoid arthritis and related conditions by standard reference films. Acta Radiol Diagn (Stockh) 18:481–491
Suter LG, Fraenkel L, Braithwaite RS (2011) Role of magnetic resonance imaging in the diagnosis and prognosis of rheumatoid arthritis. Arthritis Care Res 63:675–688. doi:10.1002/acr.20409
Naredo E, Collado P, Cruz A et al (2007) Longitudinal power Doppler ultrasonographic assessment of joint inflammatory activity in early rheumatoid arthritis: predictive value in disease activity and radiologic progression. Arthritis Rheum 57:116–124. doi:10.1002/art.22461
Kirino Y, Hama M, Takase-Minegishi K et al. (2015) Predicting joint destruction in rheumatoid arthritis with power Doppler, anti-citrullinated peptide antibody, and joint swelling. Mod Rheumatol 1–7. doi: 10.3109/14397595.2015.1026025
Bøyesen P, Haavardsholm EA, Ostergaard M et al (2011) MRI in early rheumatoid arthritis: synovitis and bone marrow oedema are independent predictors of subsequent radiographic progression. Ann Rheum Dis 70:428–433. doi:10.1136/ard.2009.123950
Kita J, Tamai M, Arima K et al (2013) Significant improvement in MRI-proven bone edema is associated with protection from structural damage in very early RA patients managed using the tight control approach. Mod Rheumatol 23:254–259. doi:10.1007/s10165-012-0646-5
Kawashiri S, Suzuki T, Nakashima Y et al (2014) Synovial inflammation assessed by ultrasonography correlates with MRI-proven osteitis in patients with rheumatoid arthritis. Rheumatology (Oxford) 53:1452–1456. doi:10.1093/rheumatology/keu034
Brown AK, Conaghan PG, Karim Z et al (2008) An explanation for the apparent dissociation between clinical remission and continued structural deterioration in rheumatoid arthritis. Arthritis Rheum 58:2958–2967. doi:10.1002/art.23945
Toyama S, Tokunaga D, Fujiwara H et al (2014) Rheumatoid arthritis of the hand: a five-year longitudinal analysis of clinical and radiographic findings. Mod Rheumatol 24:69–77. doi:10.3109/14397595.2013.854054
Takeuchi T, Yamanaka H, Inoue E et al (2008) Retrospective clinical study on the notable efficacy and related factors of infliximab therapy in a rheumatoid arthritis management group in Japan: one-year outcome of joint destruction (RECONFIRM-2J). Mod Rheumatol 18:447–454. doi:10.1007/s10165-008-0077-5
Ikeda K, Nakagomi D, Sanayama Y et al (2013) Correlation of radiographic progression with the cumulative activity of synovitis estimated by power Doppler ultrasound in rheumatoid arthritis: difference between patients treated with methotrexate and those treated with biological agents. J Rheumatol 40:1967–1976. doi:10.3899/jrheum.130556
Kaneko A, Matsushita I, Kanbe K et al (2013) Development and validation of a new radiographic scoring system to evaluate bone and cartilage destruction and healing of large joints with rheumatoid arthritis: ARASHI (Assessment of rheumatoid arthritis by scoring of large joint destruction and healing in radiographic imaging) study. Mod Rheumatol 23:1053–1062. doi:10.1007/s10165-012-0823-6
Acknowledgments
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was conducted according to the principles of the Declaration of Helsinki and approved by the ethics committee of Kyoto Prefectural University of Medicine, and informed consent was obtained from all patients.
Disclosures
None.
Rights and permissions
About this article
Cite this article
Akai, T., Taniguchi, D., Oda, R. et al. Prediction of radiographic progression in synovitis-positive joints on maximum intensity projection of magnetic resonance imaging in rheumatoid arthritis. Clin Rheumatol 35, 873–878 (2016). https://doi.org/10.1007/s10067-016-3208-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-016-3208-y