Abstract
Purpose
The Lichtenstein technique (LT) has been recognized as the standard treatment for inguinal hernia in adults owing to the high recurrence rates of tissue-based repairs. However, Desarda technique (DT) appeared as promising tissue-based repair that provided low incidence of recurrence without the need for implanting prosthetic or foreign materials in the inguinal canal. This meta-analysis of randomized controlled trials (RCTs) comparing DT and LT for primary inguinal hernia in adults aimed to determine which technique had better clinical outcome regarding recurrence and complication rates.
Methods
A systematic literature search for RCTs comparing between DT and LT was conducted using electronic databases and Google scholar service. Patients’ characteristics, technical details, recurrence and complication rates, and time to resume daily activities were extracted from the original studies and analyzed.
Results
Six RCTs comprising 2159 patients (89% males) were included. No significant difference in the incidence of recurrence between both techniques was detected (OR = 0.946; P = 0.91). The overall complication rate of LT was significantly higher than DT (OR = 1.86; P < 0.001). LT had significantly higher rates of seroma formation and surgical site infection (OR = 2.17; P = 0.007) and (OR = 2.17; P = 0.029), respectively. Postoperative pain, operation time, and time to resume normal activities were comparable in both groups.
Conclusion
Both DT and LT provided satisfactory treatment for primary inguinal hernia with low recurrence rates and acceptable rates of complications that were significantly less after DT. More well-designed RCTs with longer follow-up are required for further validation of the DT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inguinal hernia is one of the most commonly encountered conditions in surgical practice with an estimated incidence of around 15% of the adult population [1], and estimated lifetime risk of 27% for men and 3% for women [2]. Surgical repair of inguinal hernia represents an important domain in the general surgical practice with around 800,000 mesh hernioplasties are performed annually in the United States [3].
A colossal number of surgical techniques was devised for treatment of inguinal hernia with no defined consensus on the optimal repair technique until 2009 when mesh-based Lichtenstein technique (LT) was strongly recommended (level IA) by the European Hernia Society (EHS) for treatment of primary inguinal hernia in adult men after thorough analysis of the results of several clinical trials [4].
The LT was first introduced more than three decades ago as a tension-free repair of inguinal hernia [5]. The LT is currently considered the most popular procedure for the treatment of inguinal hernia in adult men owing to its low recurrence and minimal complication rates [6]. However, LT is not exactly the ideal solution for inguinal hernia as it is associated with a number of issues related to the implantation of a prosthetic mesh such as increased incidence of chronic groin pain or foreign body sensation [7], stiffness of the abdominal wall that may interfere with daily activities [8] rejection or migration of the mesh to the intestine, preperitoneal space, and the scrotum [9, 10] and surgical site infection that may necessitate removal of the infected mesh.
The problems associated with placement of a synthetic mesh in the groin revived the idea of tissue-based repair for inguinal hernia. Shouldice herniorrhaphy is considered the best tissue-based repair for inguinal hernia in terms of recurrence, yet recurrence rates of Shouldice repair are still significantly higher than mesh hernioplasty as Amato et al. implied [11]. The sophisticated nature of Shouldice method that requires a long learning curve raised a question whether Shouldice method is the only tissue-based repair that confers satisfactory results that are comparable to the standard mesh-based repair of primary inguinal hernia. In 2001 Desarda provided an answer to these questions when he published a series of 400 patients who were treated with a novel tissue-based repair that carried his name [12]. The impressive results of Desarda technique (DT) with only one case of recurrence and a single reported complication after more than 10 years of follow-up drew growing attention for this technique which does not require complex dissection nor placement of prosthetic materials.
In order to determine the actual efficacy of the DT, it should be compared directly with the LT which can be considered the standard treatment for inguinal hernia in adults in the present time. There is a paucity of well-structured randomized controlled trials (RCTs) that compare between DT and LT. Nevertheless, in the current review, we collected and analyzed the available RCTs in the literature with an intent to reach one or more conclusions about the recurrence and complication rates, and technical details of each procedure to conclude which technique had conferred better outcomes.
Methods
Registration
The protocol of the current review can be accessed online at the PROSPERO website under the registration number of CRD42016039958.
Search strategy
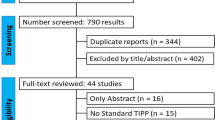
An organized literature search for RCTs comparing LT with DT was conducted by two different investigators (S.E & H.E) independently following the screening guidelines established by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (Fig. 1) [13]. Electronic databases including: PubMed/Medline, and Cochrane Central Register of Controlled Trials were searched for published and ahead-of-publication trails starting from January 2001 to April 2016. Further articles were searched via the “related articles” PubMed function. A parallel internet-based search was also conducted using the Google Scholar service and clinical trial registry at www.clinicaltrials.gov.
Keywords used in the search process included: “inguinal hernia,” “groin hernia,” “hernia,” “Desarda,” “Lichtenstein,” “Tissue-based,” “mesh,” “hernioplasty,” “tension-free,” “randomized,” “randomised,” “controlled trials,” and “clinical trials”. In addition, medical subject headings (MeSH) terms: (hernia, inguinal), (surgical mesh), (herniorrhaphy), and (randomized controlled trial) were used.
The reference section of each publication was manually searched for relevant articles. The search process was done in a systematic manner starting with title screen then abstract screen, and finally the full text versions of the selected articles were reviewed independently by two reviewers (S.E & H.E) to check eligibility. Duplicate reports were identified and excluded from this review.
Study selection
This meta-analysis included studies with the following inclusion criteria: (1) all original RCTs; (2) the treatment group underwent DT for primary inguinal hernia; (3) a parallel control group underwent LT for primary inguinal hernia; (4) only articles in English language were selected for this review.
We excluded non-randomized comparative trials, non-comparative observational studies, irrelevant articles, editorials, case reports, reviews, and meta-analyses. RCTs involving patients with recurrent inguinal hernia or comparing only one of the study arms with another comparator were excluded. After reviewing the full text of 19 articles, six RCTs [14,15,16,17,18,19] met the eligibility criteria of the review and were included.
Assessment of methodological quality within the included studies
The Cochrane Collaboration’s tool for assessing risk of bias in randomized trials devised by Higgins and colleagues [20] was used to assess the risk of bias in each study. Two reviewers (S.E & H.E) have independently assessed the risk of bias in each study, and any discrepancies in interpretation were resolved by discussion and mutual agreement (Fig. 2).
Assessment of publication bias across the included studies
A funnel plot of the standard error of the recurrence rates against the recurrence rates of the studies included was used to assess the publication bias across the studies of this review. Straight vertical line in the plot indicates the zone in which 95% of points (studies) should exist if there was no publication bias (Fig. 3).
The Begg and Mazumdar Rank Correlation Test was used to investigate publication bias and the Kendall’s tau b (corrected for ties, if any) was −0.50000, with a one-tailed P value of 0.154 and two-tailed P value of 0.308.
Egger’s regression test was also performed and the intercept (B0) was −1.3965, 95% confidence interval (−7.085, −4.292), with t = 1.056, df = 2. The one-tailed P value was 0.2, and the two-tailed P value was 0.4.
Data extraction and synthesis
We extracted information from each study about patients’ characteristics and demographic data including the sample size, mean age, gender distribution, type of hernia, follow-up time. Data of the randomization methods used, technical details, postoperative pain, recurrence and complication rates, and time to return to normal activities for each technique were also extracted from each study.
Endpoints of the review
The primary endpoint was the incidence of recurrence of inguinal hernia for each procedure after at least 6 months of follow-up. Recurrence was diagnosed clinically based on physical examination. Secondary endpoints included complication rate, postoperative groin pain, operation time, and time to return to normal activities. Postoperative complications were defined as any deviation from the normal postoperative course whether early (within 30 days of the operation) or late (beyond 30 days).
Statistical analysis
Data were extracted from the original articles into fields of Excel (Microsoft Windows). Variables were expressed using median, normal range, and percentage of patients reported in each variable.
A meta-analysis was conducted using open-source, cross-platform software for advanced meta-analysis “openMeta [Analyst] ™” version 12.11.14. Differences between the two groups with regard to recurrence and complication rates were expressed as Odds ratio (OR) with the 95% confidence interval (CI). A fixed-effect model was used to pool data when statistical heterogeneity was not present. In cases of significant (P < 0.1) statistical heterogeneity, the binary random-effect model was utilized for pooling of data.
Results
Characteristics of the studies and patients included
Six RCTs published between October 2011 and March 2016 was included in this review. Only one study [15] was a multicenter trial while the remaining five were single-center studies. Four studies [14,15,16,17] had an overall low risk of bias, and reported a study power of 80% whereas the remaining two trials had moderate risk of bias and did not report the study power clearly. None of the studies performed intention-to-treat analysis, except one [14].
The studies comprised 2159 patients who were 1923 (89%) male and 236 (11%) female of a median age of 52 (range, 32–58) years. The median age of patients in both groups was similar (49 years for LT and 48 years for DT). The studies followed the patients for a median duration of 15 (range, 0.5–78) months. Overall, 77.7% of the total number of patients reviewed was available at the end point of follow-up reported by each study. Summary of the studies included is shown in Table 1.
Overall, 2159 patients had 2254 inguinal hernias, of which 1099 were treated with DT and 1155 with LT. Ninety-five (4.4%) patients had bilateral primary inguinal hernia (64 underwent LT and 31 underwent DT), while 2064 (95.6%) patients had unilateral inguinal hernia (1132 right-sided and 932 left-sided hernias). The two techniques were not equally distributed in bilateral inguinal hernias because the number of patients with bilateral hernia treated with either technique varied among the studies, for example: Szopinski et al. [15] treated four patients with bilateral inguinal hernia with DT and treated eight patients with bilateral hernia with LT, such variation caused the disparity observed.
The size of hernia orifice was measured intraoperatively in two studies; in the first study [15], the average orifice size was equal (3 cm) in both groups; whereas, the second study [17] reported an average orifice size of 2.86 cm for LT versus 2.47 cm for DT.
Recurrence of hernia
Two studies [14, 18] did not report any recurrence in either group; however, both studies followed the patients for less than 6 months, therefore were excluded from the final analysis.
Four studies [15,16,17, 19] with more than 6 months of follow-up reported recurrence of inguinal hernia in 17 (0.94%) of 1795 patients who completed follow-up. There was no significant difference in the incidence of recurrence between DT and LT [8/882 (0.91%) Versus 9/913 (0.98%); OR = 0.946, 95% CI: 0.35–2.55; P = 0.912]. The incidence of recurrence across the studies ranged from 0.6 to 2.4% after DT and 0.4–6% after LT (Table 2, Fig. 4).
Complications
Postoperative complications occurred in 208 (9.6%) of 2159 patients. The overall incidence of complications of LT was significantly higher than DT [131/1091 (12%) versus 77/1068 (7.2%); OR = 1.86, 95% CI: 1.36–2.55; P < 0.001]. The incidence of complications across the studies ranged from 6.4 to 40% after LT and from 2.5 to 24.7% after DT. (Table 3; Fig. 5).
Overall, there were 186 early complications (DT = 71; LT = 115), and 22 late complications (DT = 6; LT = 16). The most common complication was seroma formation, occurring in 57 (2.6%) patients overall. The incidence of seroma formation after LT was significantly higher than DT [39/1091 (3.57%) versus 18/1068 (1.68%); OR = 2.17, 95% CI: 1.23–3.8; P = 0.007]. Two studies included a definition of seroma, Rodriguez et al. [16] defined seroma as aspiration of serous fluid from the wound swelling whereas Bhatti et al. [18] defined seroma as “presence of enclosed cavity containing serous fluid determined by ultrasonography at 30th post-operative day”.
Surgical site infection was diagnosed in 36 (1.67%) patients with a significantly higher incidence after LT than DT [25/1091 (2.3%) versus 11/1068 (1%); OR = 2.17, 95% CI: 1.08–4.36; P = 0.029]. Of the 25 cases who developed surgical site infection after LT, seven patients required extraction of the infected mesh as reported in two studies [16, 19].
There were no significant differences between the two techniques in the incidence of other complications as scrotal edema, hematoma, hydrocele, injury of ilioinguinal and iliohypogastric nerves, orchitis, and testicular atrophy. Nerve injury was detected intraoperatively in one study [14], and postoperatively in another trial [17] by clinical assessment of the extent of numbness or paranesthesia in the operative field, in the groin or toward the scrotum regarding the dermatomes of the iliohypogastric and ilioinguinal nerves.
Assessment of postoperative pain
Various methods were used for assessment of postoperative pain among the studies included. For the early postoperative pain, Ahmad et al. [19] reported that the number of patients who experienced mild to moderate pain after DT was significantly lower than LT up to the fifth postoperative day. In contrast, Rodríguez and coworkers [16] found no significant difference in the number of patients who experienced mild to moderate pain between the two groups.
Manyilirah and colleagues [14] and Youssef et al. [17] used a visual analogue scale from 0 to 10 to assess pain and did not observe any significant difference between the two techniques in the first 2 weeks postoperatively.
As for chronic groin pain (more than 3 months after surgery), Bhatti and colleagues [18] reported no significant difference between DT and LT with regard to chronic groin pain (4.8 versus 2.9%), which was in accord with the results of Szopinski et al. [15] On the other hand, another trial [16] reported that all patients in both groups were free of chronic groin pain after 6 months of follow-up.
Operation time
All trials reported the operation time except one [15]. Of the five trials, we excluded one study [14] that reported the operation time as the time from the beginning of a particular repair technique till the last stitch of the repair is knotted, before closing the other layers of the wound. The median operation times for LT and DT were comparable [39.5 (range, 28.8–72.3) min Vs 39 (range, 29.8–59.4) min, respectively].
Return to normal walk and daily activities
Two studies [16, 19] reported return of 84–89% of patients to work and daily activities within 15 days after DT versus 48–59% of patients who underwent LT. Szopinski and colleagues 15 found that patients returned to basic and home activities after both techniques within a similar period of time. Also Youssef et al. [17] stated that patients who underwent DT returned to work earlier than LT, however, the difference between the two groups was not statistically significant (17.4 versus 18.5 days, P = 0.14).
Only two studies reported the return to normal walk after surgery. Manyilirah et al. [14] found no significant difference between DT and LT regarding the mean time required to return to normal walk. Conversely, another study [17] observed that return to normal walk was achieved significantly earlier after DT than LT (3.9 versus 4.4 days, P = 0.02).
Discussion
Surgical treatment of inguinal hernia can be achieved via an open or a minimally invasive laparoscopic approach. The open hernia repair is classified into tissue-based and mesh-based repairs. Tissue-based repairs including the Bassini’s repair and its modifications were the standard method for treatment of inguinal hernia for a considerable period of time [17]. However, the excess tension exerted on the tissues predisposed to high failure and recurrence rates reaching up to 8.6% for Bassini’s repair and 11% for McVay repair [21]. Although the Shouldice method has been considered the best tissue-based repair with recurrence rates less than 1% [22], its technically demanding nature can potentially increase the incidence of recurrence up to 15% with the less experienced and less trained hands [23].
The idea of using prosthetic materials to accomplish tension-free repair of inguinal hernia was widely accepted and adopted by many surgeons. The prosthetic mesh induces an inflammatory reaction and eventually fibrosis that strengthens the posterior wall of the inguinal canal instead of using the already weakened muscles and fascia in repair. Although there are a number of techniques for mesh application, including single and double layer meshes and mesh plug, the LT was the only technique that had received sufficient evaluation to be recommended by the EHS [4], and the national Institute of Clinical Excellence [NICE] [24]. In addition, LT was deemed the gold standard for repair of inguinal hernia in adults by the American College of Surgeons [25].
The advantages of the LT including its technical feasibility being an easy to learn procedure, in addition to the minimal rates of recurrence and complications rendered it the standard technique for open inguinal hernia repair. Very low recurrence rates (less than 1%) were reported by The Lichtenstein Hernia Institute and the British Hernia Centre [6, 26]. Moreover, LT is usually performed as a day-case surgery, and sometimes as an outpatient procedure under local anesthesia which provides less extent of long-term pain and faster resumption of daily activities [27].
On the other hand, shortcomings of the LT include the cost of the mesh and the problems associated with implantation of a prosthetic material in the groin as the risk of seroma formation, surgical site infection, chronic groin pain or foreign body sensation, mesh migration, and impairment of testicular functions [28, 29]. Furthermore, the placement of synthetic mesh in the inguinal canal was thought to make it lose its dynamic nature, turning it into a static entity [17]. Most of these complications have been associated with the use of the classic polyprolene mesh; that is why the newer lightweight meshes, despite being more expensive than the standard polypropylene mesh, were introduced to overcome these problems [30].
Aside from the Shouldice method that requires a long training program, the concept of tissue-based repair of inguinal hernia had almost became obsolete until Desarda [12] introduced his novel technique which was thought to be a modification of Andrew’s original technique [31]. Desarda explained that his new technique entailed formation of a new posterior wall of the inguinal canal by separating a strip of the external oblique aponeurosis whilst keeping continuity of both ends then suturing this aponeurotic strip to the inguinal ligament and muscular arch behind the spermatic cord. The author presumed that when the muscles contract, this aponeurotic strip will act as a shield that strengthens the weakened muscles and prevents recurrence of hernia [12].
The physiology of the DT was thoroughly evaluated in a subsequent study [32] on 200 patients. The author stated the new posterior wall of the inguinal canal regained its physiological dynamic nature owing to the additional strength provided by the external oblique muscle. Additionally, the movement of the muscular arch improved after it was anchored to the inguinal ligament through a strip of the external oblique aponeurosis.
5 years after the original technique was published, Desarda reported a new series of 860 patients who underwent DT with zero recurrence after 7 years of follow-up. The main advantages of DT were absence of recurrence and postoperative neuralgia, being a simple procedure that does not require placement of any foreign body nor complicated dissection of the inguinal floor [33], and it can be used in contaminated surgical fields as in cases of strangulated hernia, all of these advantages concur with the criteria of the ideal repair for inguinal hernia [17].
The impressive initial results of the DT motivated investigators to conduct comparative studies between the DT and the standard LT. In a retrospective study, Desarda and Ghosh [34] reported zero recurrence after DT versus a recurrence rate of 1.97% after LT. Complication rates after DT and LT were 1.85 and 7%, respectively. Another study [35] reported shorter operation time and less severe postoperative pain after DT, nonetheless no recurrence was recorded after either technique.
Despite the excellent results of the DT, some researchers still have some objections against it. The main objection relays on the postulation that hernia is mainly caused by decrease in type I: III collagen ratio due to a defect in matrix metallopreitnase and their inhibitors, hence any tissue-based repair will not achieve satisfactory long-term results [36]. Nevertheless, the acceptable long-term results of another tissue-based repair, the Shouldice repair, stand against this theory. Furthermore, this theory is applicable in around 20% of hernia patients leaving about 80% of patients as valid candidates for DT [37].
Upon conducting the present review, we found only six RCTs [14,15,16,17,18,19] comparing the DT with the LT. It was interesting to notice that almost all of these trials were based in developing, resource-limited countries which may imply that the DT appeared as a cost-effective, economic alternative to the investigators in these countries which was clearly stated by Szopinski et al. [15] No significant differences in the baseline patients’ characteristics between the two compared groups were observed in the studies reviewed. Around 90% of patients were male concordant with the established male predominance in the literature [38].
During our analysis of data of recurrence, we excluded two short-term studies [14, 18] as the primary objective of both studies was the assessment of early postoperative outcome, particularly formation of seroma. On analysis of the remaining four trials, we did not detect any significant difference in the incidence of recurrence of hernia between the two techniques. The largest RCT in this review [16] also reported recurrence rates that were more or less equal in both groups. However, since the studies defined recurrence rates as the number of patients that developed recurrent inguinal hernia, and not the number of recurrent hernias per se, we were not able to perform statistical analysis of the recurrence rates based on the number of hernias which may cause some flaw in the estimation of recurrence rates in the cases of bilateral inguinal hernias that account for 4.4% of the population studied.
Although the incidence of recurrence may appear to be similar, yet the cause and site of recurrence quite differ. Recurrence after LT is usually near the pubic tubercle due to improper fixation of the mesh whereas recurrence after DT is either at the newly reconstructed internal ring due to insufficient narrowing [17], or at the entire posterior wall due to generalized weakness [15], or due to failure of proper lateralization of the cord [16].
The overall complication rate of LT was almost two-folds that of DT which is logical since synthetic materials implanted in the groin would predispose to higher morbidities. On further analysis, we observed no significant difference between DT and LT with regard to each individual complication with exception to seroma formation and surgical site infection which were significantly higher after LT, again owing to the presence of synthetic mesh. The incidence of surgical site infection after LT (2.3%) was less than what Taylor and associates [39] reported that 5.3% of 2665 patients developed wound infection within 30 days after groin hernia repair. Surgical site infection did not only have a different incidence amongst the two groups; but also had different consequences as seven of the 25 patients who developed infection after LT required a second procedure to remove the infected mesh inflicting further morbidity and cost. Although not statistically significant, DT had lower rates of testicular complications as edema, orchitis, atrophy, and hydrocele, yet higher rates of injury of ilioinguinal and iliohypogastric nerves which can be directly related to the surgical technique.
Regarding postoperative pain, we differentiated between the early postoperative pain and the chronic groin pain that lasts more than 3 months postoperatively as defined by the international association for the study of pain [40]. No remarkable differences in the degree of early postoperative pain were reported by the trials except one study [19] that reported lower degree of pain in favor to the DT. Chronic groin pain after hernia surgery is usually attributed to several risk factors as recurrence, age of patients and resection of the cremasteric muscle, and the experience of the surgeon [41]. The incidence of chronic groin pain after LT varies from 28.7 to 43.3%, this high incidence is probably caused by nerve entrapment syndrome secondary to excessive fibrosis around the mesh [42]. Chronic pain after mesh hernioplasty can be significantly reduced by fixating the mesh with glue instead of the conventional sutured technique [43]. Only half of the studies included in this review reported chronic groin pain and no significant differences between the two groups were noticed.
An important aspect that was not clearly discussed in the studies included was the cost-effectiveness of each technique. According to a systematic review [44], the average cost of open mesh repair of inguinal hernia in England is 987£ versus 942£ for open non-mesh repair, thus, we can assume that the difference (45£) reflects the cost of the prosthetic mesh used. Even though a recent RCT [45] demonstrated that recurrence rates after hernia repair with a low-cost mesh were similar to those of the commercial mesh, the cost of the mesh will still be an added element whilst calculating the final cost.
In summary, this is the first meta-analysis of RCTs comparing the DT with the standard LT. The results of this analysis imply that both techniques had comparable recurrence rates, operation times, postoperative pain, return to normal activities, yet high complication rates after LT. Although the estimated rates of recurrence and complications of DT in the current analysis were minimal, they were higher than the global results [46] of DT obtained by cumulating results from the main author (Desarda) and from all other surgeons worldwide; out of 11,170 patients who underwent DT, only 30 (0.26%) developed recurrence and 199 (1.78%) developed postoperative morbidities.
The limited number of RCTs comparing DT and LT and the average quality of most of them were obvious limitations to the present review. Also the heterogeneous nature of pain assessment methods and of reporting the time to return to normal walk and daily activities prevented the conduction of formal meta-analysis of these parameters. The majority of the studies suffered from lack of essential data about the duration and type of hernia, hospital stay, and cost of each procedure, therefore we did not include these variables in our analysis. The relatively short follow-up in some of the studies may prevent reaching a solid conclusion about the actual recurrence rates of both techniques since many recurrences occur several years after tissue-based repair and, to a lesser extent, prosthetic repair. Another important point is the different learning curves of both procedures which may have an impact on the incidence of recurrence and complications ultimately.
Conclusion
Both DT and LT provided satisfactory treatment for primary inguinal hernia in adults with low recurrence rates (less than 1%) as well as acceptable rates of complications that were significantly less after DT. Looking at the advantages and drawbacks of each procedure, DT can become a valid alternative to LT especially in resource-limited communities, and in cases of gross contamination. More well-designed RCTs with longer follow-up are required for further validation of the DT.
References
Awad SS, Fagan SP (2004) Current approaches to inguinal hernia repair. Am J Surg 188(6A Suppl):9S–16S
Primatesta P, Goldacre MJ (1996) Inguinal hernia repair: incidence of elective and emergency surgery, readmission and mortality. Int J Epidemiol 25:835–839
Scott NW, McCormack K, Graham P, Go PM, Ross SJ, Grant AM (2002) Open mesh versus non-mesh for repair of femoral and inguinal hernia. Cochrane Database Syst Rev (4):CD002197
Simons MP, Aufenacker T, Bay-Nielsen M et al (2009) European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 13:343–403
Lichtenstein IL, Shulman AG, Amid PK et al (1989) The tension free hernioplasty. Am J Surg 157:88–193
Amid PK, Shulman AG, Lichtenstein IL (1996) Open ‘‘tension free’’ repair of inguinal hernias: the Lichtenstein technique. Eur J Surg 162:447–453
Robert E (2001) Condon, groin pain after hernia repair. Ann Surg 233(1):8
D’Amore L, Gossetti F, Vermeil V et al (2008) Long-term discomfort after plug and patch hernioplasty. Hernia 12:445–446
Hamy A, Paineau J, Savigny JL et al (1997) Sigmoid perforation, an exceptional late complication of peritoneal prosthesis for treatment of inguinal hernia. Int Surg 82:307–308
Sakorafas GH, Halikias I, Nissotakis C et al (2001) Open tension free repair of inguinal hernias; the Lichtenstein technique. BMC Surg 1:3
Amato B, Moja L, Panico S, Persico G, Rispoli C, Rocco N, Moschetti I (2009) Shouldice technique versus other open techniques for inguinal hernia repair. Cochrane Database Syst Rev 7(4):CD001543. doi:10.1002/14651858.CD001543.pub3
Desarda MP (2001) New method of inguinal hernia: a new solution. ANZ J Surg 71:241–244
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and metaanalyses of studies that evaluate healthcareinterventions: explanation and elaboration. BMJ 21(339):b2700
Manyilirah W, Kijjambu S, Upoki A, Kiryabwire J (2012) Comparison of non-mesh (Desarda) and mesh (Lichtenstein) methods for inguinal hernia repair among black African patients: a short-term double-blind RCT. Hernia 16(2):133–144 Epub 2011 Oct 8
Szopinski J, Dabrowiecki S, Pierscinski S, Jackowski M, Jaworski M, Szuflet Z (2012) Desarda versus Lichtenstein technique for primary inguinal hernia treatment: 3-year results of a randomized clinical trial. World J Surg 36(5):984–992
Rodríguez P, Herrera P, Gonzalez O, Alonso J, Blanco H (2013) A randomized trial comparing lichtenstein repair and no mesh desarda repair for inguinal hernia: a study of 1382 patients. East Central Afr J Surg 18(2):18–25
Youssef T, El-Alfy K, Farid M (2015) Randomized clinical trial of Desarda versus Lichtenstein repair for treatment of primary inguinal hernia. Int J Surg 20:28–34
Bhatti I, Ishaqu H, Ahmad Z, Dar U (2015) Desarda’s versus lichtenstein technique of hernia repair. Pak J Med Health Sci 9(4):1331
Ahmad I, Dwivedi AC, Srivastava SK, Singh HP, Singh AK (2016) randomized trial comparing Lichenstein and Desarda technique for open inguinal hernia repair—a study of 100 patient. J Dent Med Sci 15(3):17–20. doi:10.9790/0853-1503081720
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA, Cochrane Bias Methods Group, Cochrane Statistical Methods Group (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 18(343):d5928
Hay JM, Boudet MJ, Fingerhut A et al (1995) Shouldice inguinal hernia repair in the male adult: the gold standard? A multicentral controlled trial in 1578 patients. Ann Surg 222:719–727
Shouldice EB (2003) The Shouldice repair for groin hernias. Surg Clin North Am 83:1163–1187
Junge K, Rosch R, Klinge U et al (2006) Risk factors related to recurrence in inguinal hernia repair: a retrospective analysis. Hernia 10:309–315
National Institute of Clinical Excellence(NICE) (2004) Final appraisal determination, laparoscopic surgery for inguinal hernia repair. London
Amid PK (2004) Lichtenstein tension-free hernioplasty: its inception, evolution, and principles. Hernia 8:1–7
Kurzer M, Belsham PA, Kark AE (2003) The Lichtenstein repair for groin hernias. Surg Clin North Am 83:1099–1117
Verstraete L, Becaus N, Swannet H, Ceelen W, Duchateau L, Speybroeck N (2015) Long term outcome after lichtenstein hernia repair using general, locoregional or local anaesthesia. Acta Chir Belg 115(2):136–141
Zieren J, Beyersdorff D, Beier KM et al (2001) Sexual function and testicular perfusion after inguinal hernia repair with mesh. Am J Surg 181(3):204–206
Kulacoglu H (2011) Current options in inguinal hernia repair in adult patients. Hippokratia 15(3):223–231
Earle DB, Mark LA (2008) Prosthetic material in inguinal hernia repair: how do I choose? Surg Clin North Am 88(1):179–201
Losanoff JE, Millis JM (2006) Aponeurosis instead of prosthetic mesh for inguinal hernia repair: neither physiological nor new. Hernia 10(2):1981–1999
Desarda MP (2003) Surgical physiology of inguinal hernia repair—a study of 200 cases. BMC Surgery. 3:2. doi:10.1186/1471-2482-3-2
Desarda MP (2006) Physiological repair of inguinal hernia: a new technique (study of 860 patients). Hernia 10(2):143–146 Epub 2005 Dec 9
Desarda MP, Ghosh DN (2006) Comparative study of open mesh repair and Desarda’s nomesh repair in a district hospital in India. East Central Afr J Surg 11(2):18–34
Mitura K, Romańczuk M (2008) Comparison between two methods of inguinal hernia surgery–Lichtenstein and Desarda. Pol Merkur Lekarski 24(143):392–395
Klinge U, Zheng H, Si ZY et al (1999) Synthesis of type I and III collagen, expression of fibronectin and matrix metalloproteinases1 and 13 in hernia sac of patients with inguinal hernia. Int J Surg Investig 1:219–227
Zheng H, Si Z, Kasperk R et al (2002) Recurrent inguinal hernia: disease of the collagen matrix? World J Surg 26:401–408
Rutkow IM, Robbins AW (1993) Demographic, classificatory, and socioeconomic aspects of hernia repair in the United States. Surg Clin North Am 73(3):413–426
Taylor EW, Duffy K, Lee K, Hill R, Noone A, Macintyre I, King PM, O’Dwyer PJ (2004) Surgical site infection after groin hernia repair. Br J Surg 91(1):105–111
(1986) Classification of chronic pain. Descriptions of chronic pain syndromes and definitions of pain terms. Prepared by the International Association for the Study of Pain, Subcommittee on Taxonomy. Pain Suppl 3:S1-226
Alfieri S, Amid PK, Campanelli G et al (2011) International guidelines for prevention and management of postoperative chronic pain following inguinal hernia surgery. Hernia 15:239–249
BayNielsen M, Perkins FM, Kehlet H (2001) Pain and functional impairment 1 year after inguinal herniorrhaphy: a nationwide questionnaire study. Ann Surg 233:1–7
de Goede B, Klitsie PJ, van Kempen BJ, Timmermans L, Jeekel J, Kazemier G, Lange JF (2013) Meta-analysis of glue versus sutured mesh fixation for Lichtenstein inguinal hernia repair. Br J Surg 100(6):735–742. doi:10.1002/bjs.9072
McCormack K, Wake B, Perez J, Fraser C, Cook J, McIntosh E, Vale L, Grant A (2005) Laparoscopic surgery for inguinal hernia repair: systematic review of effectiveness and economic evaluation. Health Technol Assess 9(14):1–203
Löfgren J, Nordin P, Ibingira C, Matovu A, Galiwango E, Wladis A (2016) A randomized trial of low-cost mesh in groin hernia repair. N Engl J Med 374(2):146–153
Jones P, Jones S, Guarnieri F, Moscatelli F, Smaldone W, Nwamba C, Desarda M (2015) Inguinal hernia—mesh vs non mesh. Hernia 19(Suppl 1):S265–S266
Author information
Authors and Affiliations
Contributions
Sameh Emile designed the study, shared in acquisition and analysis of data, and drafted the manuscript. Hossam Elfeki shared in acquisition and analysis of data, drafting and critical revision of the manuscript. Both authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interest to be declared by the authors.
Ethical approval
This article did not require ethical approval of any kind.
Human and animal rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
This article does not include patients, and therefore informed consent was not applicable.
Rights and permissions
About this article
Cite this article
Emile, S.H., Elfeki, H. Desarda’s technique versus Lichtenstein technique for the treatment of primary inguinal hernia: a systematic review and meta-analysis of randomized controlled trials. Hernia 22, 385–395 (2018). https://doi.org/10.1007/s10029-017-1666-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-017-1666-z