Abstract
Purpose
To determine the effectiveness of vacuum-assisted wound closure and mesh-mediated fascial traction (VAWCM) in patients undergoing open abdomen management (OAM).
Methods
Data from cases with OAM for at least five days who were admitted to our institution between January 2011 and December 2020 were included. We compared the patient’s age, sex, medical history, indication for initial surgery, APACHE II scores, indication for OAM, operative time, intraoperative blood loss, intraoperative transfusion, success of primary fascial closure (rectus fascial closure and bilateral anterior rectus abdominis sheath turnover flap method), success of planned ventral hernia, duration of OAM, and in-hospital mortality between patients undergoing VAWCM (VAWCM cases, n = 27) and vacuum-assisted wound closure (VAWC) alone (VAWC cases, n = 25).
Results
VAWCM cases had a significantly higher success rate of primary fascial closure (70% vs. 36%, p = 0.030) and lower in-hospital mortality (26% vs. 72%, p = 0.002) than VAWC cases. A multivariate logistic regression analysis showed that VAWCM was an independent factor influencing in-hospital mortality (odds ratio, 0.14; 95% confidence interval: 0.04–0.53; p = 0.004).
Conclusion
VAWCM is associated with an increased rate of successful primary fascial closure and may reduce in-hospital mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Open abdomen management (OAM) is indicated for temporary abdominal closure in damage control surgery and decompression laparotomy for abdominal compartment syndrome. In recent years, OAM has been applied to severe peritonitis and major vascular surgery, and its indications have expanded significantly. The development of open abdominal wound-dressing devices has allowed for the rapid implementation of OAM. The World Society for Emergency Surgery (WSES) published guidelines for OAM in trauma and non-trauma patients in 2018 [1].
Although OAM has become a very important procedure in acute care surgery, it requires specialized knowledge and skills. Prolonged OAM causes lateral deviation and retraction of the muscles and fascia of the abdominal wall, making primary fascial closure difficult. Generally, primary fascial closure means any fascial closure and includes rectus fascial closure, the bilateral anterior rectus abdominis sheath turnover flap method, and the component separation method [2,3,4]. If primary fascial closure is difficult, a planned ventral hernia should be considered [5]. As prolonged OAM also increases complication and mortality rates, early primary fascial closure is important to improve the prognosis [6].
Vacuum-assisted wound closure and mesh-mediated fascial traction (VAWCM) is a temporary abdominal closure technique that has been reported to be useful for OAM because of the increased success rate of primary fascial closure [7,8,9]. However, the effectiveness of VAWCM has not been reported in Japan.
In this study, to better understand the effectiveness of VAWCM, we compared cases with OAM for at least five days treated with VAWCM and vacuum-assisted wound closure (VAWC) alone at our institution.
Methods
Study design and setting
We conducted a single-institutional retrospective observational study by examining the medical records of patients admitted to our institution between January 2011 and December 2020 with OAM commencing after the initial surgery and continuing for at least five days. All procedures performed in this study involving human participants were in accordance with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The study was approved by the Institutional Review Board of Nippon Medical School Hospital (B-2021-494).
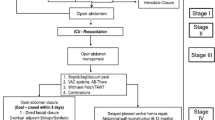
The indications for OAM in our institution were identical to the WSES guidelines [1] and included abdominal compartment syndrome (including cases with difficult abdominal closure at the time of initial surgery), damage control surgery for trauma, and damage control surgery for non-traumatic diagnoses, such as peritonitis and intestinal ischemia requiring a second-look procedure. Damage control surgery for non-traumatic cases was defined as the completion of the initial surgery with only hemostasis and control of contamination achieved because of acidosis, coagulopathy, hypothermia, and/or the need for high-dose vasopressors. Patients who underwent OAM for intestinal ischemia requiring a second look, reoperation, and/or surgical wound dehiscence were excluded from the study. Patients who experienced cardiopulmonary arrest upon arrival were excluded. Patients meeting the inclusion criteria were divided into two groups: those undergoing VAWCM (VAWCM cases) and those undergoing VAWC alone (VAWC cases).
VAWCM indications
Indications for VAWCM were difficulty closing the abdomen following long-term OAM and expected difficulty in closing the abdomen during OAM. There was no clear prior protocol for VAWCM, and the surgeon in charge determined the indications and management of VAWCM in each case.
VAWCM cases
VAWCM is a temporary abdominal closure technique first reported by Petersson et al. in 2007 [10]. In the original procedure, to prevent lateral deviation and retraction of the muscles and fascia of the abdominal wall that can occur in OAM, a sheet of polypropylene mesh was sutured to the edge of each rectus abdominis muscle. The sheets were then pulled together under tension and sutured at the midline. Every 48–72 h, the abdominal dressing was changed, and the meshes were resutured closer together to reduce the abdominal wall separation distance. At our institution, we modified the original method and used the following procedure for VAWCM:
-
1.
The mesh was a polypropylene mesh used in abdominal incisional hernia surgery. The mesh was divided into two halves and cut to a length equivalent to the wound, and each half was sutured to one rectus abdominis muscle (Fig. 1a). The suture is 0 absorbable thread, and the meshes are fixed to the rectus abdominis muscles (a 2-cm bite is taken from the edge of the rectus abdominis muscle, and the mesh is sewn in a 5-cm pitch, because the narrow bite and narrow pitch sutures that are usually used can damage the rectus abdominis wound margin, making it impossible to perform rectus sheath anterior leaflet inversion in subsequent abdominal closure).
-
2.
Direct contact of the meshes with the intestinal tract is thought to increase complications such as bleeding, enteroatmospheric fistula, gastro-atmospheric fistula, and adhesion of the omentum or liver to the mesh, which can result in inadvertent bleeding when the abdomen is reopened, it is crucial that the intra-abdominal viscera be covered with a sheet of polyethylene (Fig. 1b) under the mesh. The polyethylene sheet used in this study was the same as that used in intestinal isolation bags in surgical procedures.
-
3.
For further protection, towel gauze was laid on the upper surface of the protective polyethylene layer, and the meshes above the gauze were pulled together under tension and sutured at the midline (Fig. 1c, d).
-
4.
The meshes were always sutured while monitoring hemodynamics, respiratory status, and intra-abdominal pressure (IAP) to avoid abdominal compartment syndrome.
-
5.
Vacuum-assisted wound closure was performed above the mesh layer between the separated rectus muscles using one of two methods: (a) A towel gauze was laid down, and a suction drain was placed on top of the sutured meshes and sealed with a drape along with the surrounding skin (Fig. 1e). (b) In cases employing a commercial negative pressure wound therapy device (NPWT; V.A.C.®, 3 M Company, San Antonio, TX, USA), instead of towel gauze and a suction drain, a perforated foam layer and a suction drain enclosed within the commercial NPWT device were used for VAWC (Fig. 1f).
Procedure of vacuum-assisted wound closure and mesh-mediated fascial traction. a A sheet of polypropylene mesh is sutured to the edge of each rectus abdominis muscle. b All exposed intraabdominal viscera are covered with a protective sheet of polyethylene to completely separate the intraabdominal viscera from contact with the abdominal wall and polypropylene mesh. c A towel gauze is placed on the upper surface of the protective polyethylene sheet, and the meshes are pulled together under tension and then sutured at the midline. d Respiratory status, circulatory status, and intra-abdominal pressure are closely monitored to avoid abdominal compartment syndrome. e A case of vacuum-assisted wound closure using a second towel gauze placed on the upper surface of the meshes. f A case of vacuum-assisted wound closure using perforated foam with the commercial negative pressure wound therapy device on the upper surface of the meshes. g Overview of VAWCM. Negative pressure is −50 to −150 mmHg, depending on the patient’s condition
An overview of VAWCM in a case using the commercial NPWT device is shown in Fig. 1g.
VAWC cases
For VAWC, we used a homemade vacuum pack technique or a commercial open abdominal wound-dressing device (AbThera™; 3 M Company). The homemade vacuum pack technique is a modified Barker’s method [11] with abdominal dressing changes every 24–72 h.
In the VAWCM and VAWC cases, we attempted to close the abdomen at each dressing change if the abdominal cavity was under control. This is because unnecessary prolongation of OAM is associated with a poor prognosis. In patients with abdominal compartment syndrome, abdominal closure is performed while monitoring the vital signs, IAP, and respiratory status.
Ten to 14 days after the initial laparotomy, the use of a turnover flap constructed from the anterior rectus abdominis sheath was considered if the distance to be closed with fascia was < 15 cm in patients unsuitable for rectus fascial closure because of prolonged visceral edema [2]. In the VAWCM cases, the meshes were removed, and the abdominal wall underwent primary fascial closure (rectus fascial closure or bilateral anterior rectus abdominis sheath turnover flap method).
Data collection and processing
We collected data on the patient’s age, sex, medical history, preoperative and postoperative acute physiology and chronic health evaluation (APACHE) II scores, operative time, intraoperative blood loss, and intraoperative transfusions. We recorded the indications for OAM, indications for initial surgery, success of primary fascial closure (rectus fascial closure or bilateral anterior rectus abdominis sheath turnover flap method), operative procedures, success of planned ventral hernia, duration of OAM (termination of OAM was defined as either primary fascial closure, planned ventral hernia, or death during OAM), complications associated with OAM, and in-hospital mortality.
Study outcomes
The primary outcome was in-hospital mortality, and the secondary outcomes were the success of primary fascial closure, success of planned ventral hernia, duration of OAM, and complications associated with OAM. These outcomes were compared between the VAWCM and VAWC cases.
Statistical analyses
Data are presented as numbers (%) or medians (interquartile range [IQR]). A multiple imputation method was used for missing data [12, 13]. Continuous variables were compared between the groups using the Mann–Whitney U test, and categorical variables were compared using Fisher’s exact test. In addition, a multivariate logistic regression analysis was used to determine the factors influencing in-hospital mortality. The explanatory variables were based on previous reports: preoperative APACHE II score [14,15,16], duration of OAM [6], and VAWCM for in-hospital mortality [17]. A value of p < 0.05 was considered statistically significant at p < 0.05. All statistical analyses were performed using a commercial software program (SPSS Version 27.0®; IBM Corp., Armonk NY, USA).
Results
Patients’ characteristics
This retrospective study included 207 patients who underwent OAM between January 2011 and December 2020. Of these, 152 patients were excluded (122 for an OAM duration of less than 5 days, 22 for intestinal ischemia requiring a second-look operation, 6 for reoperation and surgical wound dehiscence, and 2 for cardiopulmonary arrest on arrival), and the remaining 52 cases were included in the present study (Fig. 2). There were 37 missing values (2.8%) in this study dataset that were handled using the multiple imputation method. VAWCM was performed in 27 patients (52%) and VAWCM in 25 patients (48%).
The clinical characteristics of the patients (n = 52) are shown in Table 1. Among all eligible cases, the median age was 73 (IQR, 61–82) years old, and 26 patients (50%) were male. The median preoperative and postoperative APACHE II scores were 20 (IQR 15–24) and 26 (IQR 22–29). There were no significant differences in patient characteristics between the VAWCM and VAWC cases.
Indications and operative procedures in initial surgery
The indications for OAM and the initial surgery are shown in Table 2. The leading indication for OAM was non-trauma damage control surgery (n = 31 [60%]), and the leading indication for initial surgery was bowel perforation (n = 27 [52%]). The differences in indications between the two groups were not significant. Table 2 also shows the operative procedures in the initial surgery and reveals no significant differences between the two groups. The most common operative procedure at the initial surgery was bowel resection, and owing to the wide variety of surgical procedures used, the details of bowel resection are shown as supplementary data (Supplemental Table 1). The VAWCM cases had significantly more colostomies at initial surgery than the VAWC cases (including Hartmann’s operation), but there were no significant differences in the other procedures. Intestinal reconstruction after bowel resection was also observed; however, there was no significant difference in rates between the two groups. Anastomosis with covering stoma construction and ileostomy were not performed at the initial surgery.
Patient outcomes
For the primary outcome, the overall in-hospital mortality rate was 48%, and the VAWCM cases had a significantly lower in-hospital mortality (26% vs. 72%, p = 0.002). Among the secondary outcomes, the success rate of primary fascial closure was 54%, of which the VAWCM cases had a higher success rate than the VAWC cases (70% vs. 36%, p = 0.030). In contrast, there was no significant difference in the success rate of rectus fascial closure between the two groups. The median duration of OAM was 11 (IQR, 8–37) days, showing no significant difference between the two groups (Table 3).
Complications
The overall rate of complications associated with OAM was 75%, with no significant difference between the two groups. The most common complication was intra-abdominal infection (n = 26 [50%]). Of these, 62% were secondary to bowel perforation followed by trauma (12%). For intra-abdominal infections, the priority was to control the infected lesions, and for those that remained, intra-abdominal lavage was performed during dressing changes. Enterocutaneous fistulas were found in 4% of all cases (Table 3).
Prognostic factors
A multivariate logistic regression analysis showed that VAWCM and preoperative APACHE II scores were independent factors influencing in-hospital mortality (VAWCM, odds ratio [OR]: 0.14, 95% confidence interval [CI]: 0.04–0.53, p = 0.004; preoperative APACHE II score, OR: 1.12, 95% CI: 1.01–1.24, p = 0.026) (Table 4).
Discussion
In recent years, indications for OAM have expanded significantly. Nevertheless, abdominal closure remains difficult in some cases, even with intra-abdominal disease control. Prolonged OAM in both trauma and non-trauma patients has been reported to increase complication and mortality rates [7, 8]. In 2007, Petersson et al. [10] reported seven cases of VAWCM as a new temporary abdominal closure technique that allowed for primary fascial closure in patients requiring long-term OAM.
Following the introduction of VAWCM for cases of difficult abdominal closure during OAM at our institution in 2011, the success rate of primary fascial closure was significantly higher in VAWCM than in VAWC alone (70% vs. 36%, p = 0.030). Similarly, in their multicenter prospective study of 151 patients who were expected to have OAM for at least 5 days at the time of initial surgery, Acosta et al. [18] reported a primary fascial closure rate in VAWCM cases (n = 111) of 76.6% and an in-hospital mortality rate of 29.7%. In addition to this report, clinical experience at our institution suggests that early initiation of VAWCM may lead to more successful primary fascial closure. In recent years, we have aggressively performed VAWCM in patients with OAM who are expected to have difficulty with abdominal closure.
Our present 70% success rate for primary fascial closure with VAWCM was slightly lower than that reported by Acosta et al. [18]. In our study, the median time from OAM initiation to VAWCM initiation was 5 (range, 2–37) days, whereas Acosta et al. used a 2- to 3-day period from OAM initiation to VAWCM initiation. Furthermore, our primary fascial closure rate was 86% in cases in which VAWCM was initiated within 5 days of the start of OAM and 54% in those in which it was initiated more than 5 days after OAM (p = 0.103); the rates for rectus fascial closure were 79% and 31%, respectively (p = 0.021). Given these findings, we suggest that the time between the initiation of OAM and VAWCM may affect the rate of primary fascial closure. Although no recommendations for the timing of VAWCM initiation have been reported, Berrevoet et al. [8] found that patients who initiated VAWCM from the initial surgery had a significantly higher fascial closure rate than those in whom it was initiated 3 or more days later. However, it is difficult to initiate VAWCM at the time of initial surgery in all patients who undergo OAM because the initial surgery is often used for damage control in both trauma and non-trauma cases. We also assume that the report by Berrevoet et al. included a small number of cases in which primary fascial closure could have been achieved without VAWCM. Based on the above, we believe that VAWCM should be initiated within five days after the start of OAM, depending on the condition of the abdomen.
In our study, a commercial open abdominal wound dressing device, which was recently suggested to be useful [19], was used in only four of the VAWC cases and in none of the VAWCM cases. There was no statistically significant difference in the frequency of use between the two groups.
The VAWCM cases had a significantly lower in-hospital mortality rate than the VAWC cases (26% vs. 72%, p = 0.002). In the multivariate logistic regression analysis, VAWCM was an independent factor influencing the decrease in in-hospital mortality (OR, 0.14; 95% CI: 0.04–0.53; p = 0.004). Salamone et al. [7] also reported that VAWCM influenced in-hospital mortality (OR, 0.15; 95% CI: 0.05–0.46; p < 0.01). This may be attributed to the significantly higher rates of primary fascial closure in VAWCM cases than in VAWC cases, given our finding that successful primary fascial closure was associated with a lower rate of in-hospital death (18% vs. 83%, p < 0.001).
A complication specific to VAWCM is abdominal incisional hernia after primary fascial closure. This is due to tissue injuries caused by sewing the polypropylene mesh to the edges of the rectus abdominis muscles and pulling them together under tension. The incidence is reported to be 35%–41%, and the possibility that it may reduce the quality of life should be noted [8, 20]. Another complication of OAM that is not specific to VAWCM is entero-atmospheric fistula, defined as communication between the gastrointestinal tract and the atmosphere [21]. This complication makes OAM difficult and leads to high mortality rates of 20%–44% [22]. A systematic review by Petersson et al. [23] reported a 5.6% incidence of enteroatmospheric fistulas in VAWCM. Another systematic review of the relationship between complications and mortality in temporary abdominal closure techniques [24] showed that VAWCM was associated with lower mortality and a lower incidence of entero-atmospheric fistula than VAWC alone. Although there were no significant differences in the complications associated with OAM in this study, incisional hernia could not be evaluated because of the lack of long-term follow-up. From the above, we conclude that a similar or lower complication rate can be achieved with VAWCM than with VAWC alone.
Limitations
Several limitations associated with the present study warrant mention. First, it was conducted retrospectively, and the degree of selection bias was inevitable. In our institution, during the early days of VAWCM introduction, the procedure was performed in patients who required long-term OAM. It is plausible that the VAWCM cases included more patients who could tolerate long-term OAM than the VAWC cases, which might have influenced their prognosis. Given the possible involvement of these biases, we have provided the causes of death for all patients as supplementary data (Supplemental Table 2). Second, we had a relatively small sample size, which could not provide sufficient power for a comprehensive statistical analysis. Third, there were no clear definite indications for VAWCM; rather, the implementation was at the discretion of the surgeon. Fourth, although there are likely to be overlapping pathologies regarding the indication for OAM, we consulted the medical records and selected the one that seemed to be more elemental. Finally, we did not examine the long-term prognosis.
Conclusion
VAWCM is associated with a higher rate of successful primary fascial closure than VAWC and may reduce in-hospital mortality.
References
Coccolini F, Roberts D, Ansaloni L, Ivatury R, Gamberini E, Kluger Y, et al. The open abdomen in trauma and non-trauma patients: WSES guidelines. World J Surg. 2018;13:7.
Kushimoto S, Yamamoto Y, Aiboshi J, Ogawa F, Koido Y, Yoshida R, et al. Usefulness of the bilateral anterior rectus abdominis sheath turnover flap method for early fascial closure in patients requiring open abdominal management. World J Surg. 2007;31:2–8.
Arai M, Kim S, Ishii H, Hagiwara J, Kushimoto S, Yokota H. The long-term outcomes of early abdominal wall reconstruction by bilateral anterior rectus abdominis sheath turnover flap method in critically ill patients requiring open abdomen. World J Emerg Surg. 2018;13:39.
Ramirez OM, Ruas E, Dellon AL. “Components separation” method for closure of abdominal-wall defects: an anatomic and clinical study. Plast Reconstr Surg. 1990;86:519–26.
Jernigan TW, Fabian TC, Croce MA, Moore N, Pritchard FE, Minard G, et al. Staged management of giant abdominal wall defects: acute and long-term results. Ann Surg. 2003;238:349–55.
Miller RS, Morris JA Jr, Diaz JJ Jr, Herring MB, May AK. Complications after 344 damage-control open celiotomies. J Trauma. 2005;59:1365–71.
Salamone G, Licari L, Guercio G, Comelli A, Mangiapane M, Falco N, et al. Vacuum-assisted wound closure with mesh-mediated fascial traction achieves better outcomes than vacuum-assisted wound closure alone: a comparative study. World J Surg. 2018;42:1679–86.
Berrevoet F, Lampaert S, Singh K, Jakipbayeva K, van Cleven S, Vanlander A. Early initiation of a standardized open abdomen treatment with vacuum assisted mesh-mediated fascial traction achieves best results. Front Surg. 2021;7: 606539.
Acosta S, Björck M, Petersson U. Vacuum-assisted wound closure and mesh-mediated fascial traction for open abdomen therapy–a systematic review. Anaesthesiol Intensive Ther. 2017;49:139–45.
Petersson U, Acosta S, Björck M. Vacuum-assisted wound closure and mesh-mediated fascial traction a novel technique for late closure of the open abdomen. World J Surg. 2007;31:2133–7.
Barker DE, Kaufman HJ, Smith LA, Ciraulo DL, Richart CL, Burns RP. Vacuum pack technique of temporary abdominal closure: a 7-year experience with 112 patients. J Trauma. 2000;48:201–6.
Janssen KJ, Donders AR, Harrell FE Jr, Vergouwe Y, Chen Q, Grobbee DE, et al. Missing covariate data in medical research: to impute is better than to ignore. J Clin Epidemiol. 2010;63:721–7.
Little RJ, D’Agostino R, Cohen ML, Dickersin K, Emerson SS, Farrar JT, et al. The prevention and treatment of missing data in clinical trials. N Engl J Med. 2012;367:1355–60.
Cristaudo AT, Jennings SB, Hitos K, Gunnarsson R, DeCosta A. Treatments and other prognostic factors in the management of the open abdomen: a systematic review. J Trauma Acute Care Surg. 2017;82:407–18.
Morais M, Gonçalves D, Bessa-Melo R, Devesa V, Costa-Maia J. The open abdomen: analysis of risk factors for mortality and delayed fascial closure in 101 patients. Porto Biomed J. 2018;3: e14.
Tartaglia D, Marin JN, Nicoli AM, De Palma A, Picchi M, Musetti S, et al. Predictive factors of mortality in open abdomen for abdominal sepsis: a retrospective cohort study on 113 patients. Updates Surg. 2021;73:1975–82.
Rasilainen S, Mentula P, Salminen P, Koivukangas V, Hyöty M, Mäntymäki LM, et al. Superior primary fascial closure rate and lower mortality after open abdomen using negative pressure wound therapy with continuous fascial traction. J Trauma Acute Care Surg. 2020;89:1136–42.
Acosta S, Bjarnason T, Petersson U, Pålsson B, Wanhainen A, Svensson M, et al. Multicentre prospective study of fascial closure rate after open abdomen with vacuum and mesh-mediated fascial traction. Br J Surg. 2011;98:735–43.
Cheatham ML, Demetriades D, Fabian TC, Kaplan MJ, Miles WS, Schreiber MA, et al. Prospective study examining clinical outcomes associated with a negative pressure wound therapy system and Barker’s vacuum packing technique. World J Surg. 2013;37:2018–30.
Schaaf S, Schwab R, Willms A. Quality of life after open abdominal treatment with vacuum-assisted wound closure and mesh-mediated fascial traction. Mil Med. 2021;186:452–7.
Terzi C, Egeli T, Canda AE, Arslan NC. Management of enteroatmospheric fistulae. Int Wound J. 2014;11:17–21.
Bobkiewicz A, Walczak D, Smoliński S, Kasprzyk T, Studniarek A, Borejsza-Wysocki M, et al. Management of enteroatmospheric fistula with negative pressure wound therapy in open abdomen treatment: a multicentre observational study. Int Wound J. 2017;14:255–64.
Petersson P, Petersson U. Dynamic fascial closure with vacuum-assisted wound closure and mesh-mediated fascial traction (VAWCM) treatment of the open abdomen-an updated systematic review. Front Surg. 2020;7: 577104.
Cristaudo A, Jennings S, Gunnarsson R, DeCosta A, Cristaudo A, Jennings S, Gunnarsson R, et al. Complications and mortality associated with temporary abdominal closure techniques: a systematic review and meta-analysis. Am Surg. 2017;83:191–216.
Acknowledgements
We thank Libby Cone, MD, and MA from Dmed (dmed.co.jp <https://dmed.co.jp/ >) for editing the drafts of this manuscript.
Funding
Funding for this study was provided by ZENKYOREN (National Mutual Insurance Federation of Agricultural Cooperatives). This funding source had no role in the design, practice, or analysis of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest associated with this manuscript.
Ethical approval
This study was approved by the Institutional Review Board of Nippon Medical School Hospital and conformed to the provisions of the Declaration of Helsinki. Approval No. B-2021–494.
Informed consent
As this study used only medical and other information without invasion or intervention, opt-out by posting on the Nippon Medical School Hospital Clinical Research Center’s website (http://ctr-nms.com/) was used.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shigeta, K., Kim, S., Nakae, R. et al. Effectiveness of vacuum-assisted wound closure and mesh-mediated fascial traction in open abdomen management. Surg Today (2024). https://doi.org/10.1007/s00595-024-02899-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00595-024-02899-7