Abstract
Angiomatoid fibrous histiocytoma (AFH) is a soft tissue tumor of uncertain differentiation. Although its prognosis is good, its diagnosis and differential diagnosis remain a challenge, particularly for tumors with an atypical morphology. We evaluated the clinicopathological characteristics of 14 AFH cases and examined the key factors in its diagnosis or differential diagnosis. The cohort comprised 6 men and 8 women aged 9–65 years (average age: 31.2 years). Most of the tumors (11/14, 79%) were located in soft tissues, whereas 3/14 (21%) were located in the lung (1 case) and brain (2 cases). Tumor cells were spindle-shaped to epithelioid, with a visible fibrous capsule (9/14, 64%), hemorrhagic gap (9/14, 64%), lymphocyte sleeve (7/14, 50%), necrosis (3/14, 21%), and infiltrative boundary (4/14, 29%). The tumors expressed desmin (10/14, 71%) and exhibited low levels of Ki-67. 13 cases (93%) displayed ESWSR1 gene rearrangement. At follow-up, 1 case (7%) experienced local tumor recurrence. AFH is a rare intermediate tumor. Its pathological diagnosis requires a comprehensive analysis of histological, immunophenotypic, and molecular genetic features to avoid misdiagnosis. Our study has further enriched the histological features of AFH, emphasizing the importance of differential diagnosis and providing a reference for clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Angiomatoid fibrous histiocytoma (AFH) is a rare intermediate tumor that often occurs in the subcutaneous soft tissue of young people. AFH was first described by Enzinger in 1979 [1] and was considered a variant of malignant fibrous histiocytoma. However, subsequent large-scale studies have revealed that it differs significantly in biological behavior from other tumors in this category and has a good prognosis after extensive resection [2]. Therefore, AFH is now considered an independent solid tumor. Histologically, it is primarily composed of epithelioid or spindle-shaped cells arranged in nodular or patchy shapes and accompanied by hemorrhagic stroma. Characteristic lymphoplasma cell sleeves are present around the tumor and most tumors exhibit EWSR1 gene mutations [3]. However, AFH often exhibits morphological variations rather than a typical microscopic morphology and lacks specific immunohistochemical markers. Additionally, EWSR1 gene alterations can also occur in other tumor types. Therefore, AFH is easily misdiagnosed as other tumors, making the accurate diagnosis of AFH a significant challenge. Herein, we retrospectively analyzed the clinical and pathological data of 14 AFH cases through a literature review to identify their clinicopathological characteristics. The results enhance our understanding of this disease and will aid pathologists and clinical physicians in improving the accuracy of diagnosing and differentially diagnosing AFH.
Materials and methods
Clinical data
We collected clinical data, tissue sections, immunohistochemical results, and fluorescence in situ hybridization (FISH) results for the EWSR1 isolation probe from 14 patients with AFH at the First Affiliated Hospital of Fujian Medical University and Fujian Provincial Hospital from 2012 to 2022. The clinical data were obtained from the hospital’s medical record system and the deadline for postoperative follow-up was April 3, 2023. The trial was approved by the ethics committee of the hospital and all patients voluntarily participated and signed informed consent forms.
Methods
Tumor tissue samples were fixed with 10% neutral formalin, dehydrated, and paraffin-embedded. The blocks were sliced to a thickness of 4 μm and the sections were stained with hematoxylin–eosin. Immunohistochemistry (EliVision method) was used to detect the expression of epithelial membrane antigen (EMA) (GP14, Fuzhou Maixin Biotech Co., Ltd., China), Vimentin (MX034, Fuzhou Maixin Biotech Co., Ltd., China), S100 (4C4.9, Fuzhou Maixin Biotech Co., Ltd., China), SOX10 (EP268, Fuzhou Maixin Biotech Co., Ltd., China), SMA (MX097, Fuzhou Maixin Biotech Co., Ltd., China), CD68 (KP1, Fuzhou Maixin Biotech Co., Ltd., China), CD34 (MX123, Fuzhou Maixin Biotech Co., Ltd., China), desmin (MX046, Fuzhou Maixin Biotech Co., Ltd., China), CD99 (MX111, Fuzhou Maixin Biotech Co., Ltd., China), CKpan (MX005, Fuzhou Maixin Biotech Co., Ltd., China), MyoD1 (EP212, Beijing ZSGB Biotech Co., Ltd., China), myogenin (EP162, Beijing ZSGB Biotech Co., Ltd., China), and Ki-67 (MIB-1, Beijing ZSGB Biotech Co., Ltd., China). Fourteen patients with AFH were all subjected to FISH detection. The EWSR1 isolation probe was obtained from ABBOTT Biotechnology Co., Ltd. The detection steps were performed based on the manufacturer’s instructions, with a signal separation rate of > 15% as the positive standard. The pathological characteristics of all cases were independently evaluated by two senior pathologists.
Results
Clinical characteristics
The average age of AFH onset for the 14 patients was 31.2 years, with a median of 35 years. Women were slightly more likely to have hair than men (male-to-female ratio: 6:8). Three cases of tumors occurred within internal organs (meninges and lungs), whereas the remainder occurred in soft tissues, including nine in superficial soft tissues (subcutaneous and limb) and two in deep soft tissues (retroperitoneum and skeletal muscles). One patient with a tumor in the knee experienced limited joint movement, whereas the others did not experience discomfort. Patients with AFH in the meninges and lungs exhibited meningeal irritation and cough, respectively. All patients underwent complete tumor resection without postoperative radiotherapy or chemotherapy. Postoperative pathological examination indicated negative surgical margins. All 14 patients underwent annual postoperative follow-up visits and radiological examinations. The patients remain alive, with only one experiencing tumor recurrence at the original site. Imaging examinations of the remaining patients did not reveal any tumor recurrence or metastasis to other anatomical sites (Table 1).
Organizational characteristics
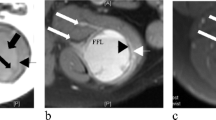
The pathological characteristics of the tumors in the 14 AFH patients are shown in Table 2. Most tumors had a diameter exceeding 2 cm (9 cases), with a maximum diameter of approximately 10 cm. The fibrous capsule and hemorrhagic gaps of the tumors were common (all 9 cases) (Fig. 1A), whereas 7 cases did not show the characteristic lymphocyte sleeve (Fig. 1B). However, these classic morphological features were not found in the patient samples with tumor recurrence. Necrosis (3 cases) and infiltrative boundaries (4 cases) were rare. The tumor cells exhibited a mild morphology, ranging from epithelioid to spindle-shaped, and were arranged in a nodular or sheet-like manner, with a rich and eosinophilic cytoplasm. The nucleus was round or oval, with a vacuolar shape and visible small nucleoli (Fig. 1C). Additionally, some tumors exhibited obvious pleomorphic cells, multinucleated tumor giant cells, or a focal mucoid matrix upon microscopic examination (Fig. 1D). Pathological mitotic figures were rare and generally less than 5/10 high-power field (HPF). However, in one patient with subcutaneous leg involvement, the mitotic figures in the tumor hotspot area reached 8/10 HPF. None of the tumors exhibited sclerotic stroma, extensive mucinous stroma, or small cell morphology (Table 2). Notably, in five cases (5/14), multiple biopsies revealed classic histological features (hemorrhagic gap, lymphocyte sleeve, fibrous capsule), leading to the diagnosis of AFH.
Pathological manifestations of AFH. A Hemorrhagic gap surrounded by tumor cells (arrow). B Lymphocyte sleeve with locally visible germinal center formation (arrow). C Tumor cells with epidermic to short spindle-shaped morphology, eosinophilic cytoplasm, round or oval nuclei with nucleoli present, without pathological nuclear division. D Special histological features including scattered multinucleated giant cells (as indicated by the arrow in the left figure) and mucoid matrix (right figure). E Strong desmin expression in tumor cells (EliVision method). F FISH detection. An EWSR1 separation probe exhibiting red and green signal separation (arrow), indicating EWSR1 gene translocation rearrangement
Immunophenotype
All tumors strongly expressed vimentin and most expressed CD68 and CD99, whereas a few tumors expressed SMA. CK, EMA, CD34, S100, and SOX10 were not expressed. Additionally, most tumors expressed desmin (10 cases) (Fig. 1E), but the striated muscle markers MyoD1 and myogenin were negative. Ki-67 expression in all tumors was less than 10% (Table 3).
FISH results
Thirteen patients exhibited EWSR1 gene segregation (Fig. 1F), whereas one patient with back tumors did not show changes in EWSR1.
Discussion
AFH is a rare intermediate tumor characterized by heterogeneous morphology and nonspecific immunophenotype. Our study, originating from two provincial tertiary grade A hospitals in China, encompasses 14 cases of AFH, representing a relatively large-scale study. Our cases further enrich the morphological characteristics of AFH. Our results indicate that encountering spindle cell tumors during pathological diagnosis, with features such as hemorrhagic gaps, lymphocytic sleeves, or fibrous capsules observed microscopically, alongside positive immunostaining for desmin, CD68, or CD99, and positive EWSR1 rearrangement, should raise suspicion for AFH.
AFH accounts for 0.3% of soft tissue tumors and predominantly affects young individuals without sex difference. It commonly occurs in the limbs, presenting as painless soft tissue masses and occasionally involving internal organs [3]. In our study, we report one case of pulmonary AFH and two cases of cerebral AFH, which provides additional insights into the locations where this tumor can occur. The etiology and source of AFH remain unclear, although AFH was initially believed to originate from fibrous tissue cells, similar to malignant fibrous histiocytoma. However, no conclusive ultrastructural or immunohistochemical evidence has been found to support this claim [4]. Recent findings based on desmin-positive tumor cells suggest that AFH likely originates from myoid or myofibroblast lineages. [5]
Microscopically, the tumor exhibits a clear boundary and is arranged in a lobulated or multinodular shape. It consists of the following four morphologies in different proportions [3]: (1) epithelial or spindle-shaped cells with eosinophilic cytoplasm and mild atypical vesicular nuclei, arranged in a syncytial structure, sometimes with pseudoinclusion bodies visible in the nucleus; (2) pseudoangiomatous spaces containing blood surrounded by tumor cells; (3) a thick fibrous pseudocapsule with deposition of hemosiderin; and (4) lymphocyte sheaths of varying number and thickness around the tumor as well as visible germinal centers. Our results showed that nine cases (64%) exhibited fibrous capsules and hemorrhagic gaps, while lymphocytic sleeve was observed in half of the cases. A few cases exhibited necrosis (3/14), invasive growth (4/14), and high mitotic counts (1/14). It is evident that not all AFH cases exhibit these typical features, and they may even be completely absent. Therefore, a comprehensive analysis combining clinical features, immunophenotypes, and molecular genetics is necessary for an accurate diagnosis of AFH. Additionally, in 5 out of 14 cases in this group, after multiple rounds of sampling, the classic histological morphology was finally identified, leading to a definitive diagnosis of AFH. Therefore, extensive sampling can improve the detection rate of AFH, particularly in cases with atypical morphology. In addition to these classic histological characteristics, AFH exhibits various tissue variant forms, including the presence of prominent nuclear heterotypic hyperchromatic giant cells and distinct mucoid stroma in the tumors. However, these changes are not related to tumor biological behavior [6,7,8]. In the present study, two tumors exhibited scattered nuclear heterotypic giant cells and one lung tumor showed obvious mucoid stroma. Nonetheless, these patients had a good prognosis and did not experience tumor progression following surgery.
AFH lacks specific immune characteristics; therefore, immunohistochemistry is only used as a reference. Approximately, 50% of AFH tumors express desmin, whereas 40–50% of tumors exhibit variable positive expression for EMA, CD99, and CD68 but are negative for skeletal muscle markers (myogenin or MyoD1) or vascular endothelial markers (CD31, CD34, and factor VIII-related antigens) [3, 4]. Ki-67 expression generally occurs in 2–4% of the tumors [9]. Our results indicate that AFH tumor cells express desmin (71.4%), CD68 (85.7%), and CD99 (85.7%), while none expressed myogenin, MyoD1, or CD34. These findings align with previous reports, [3, 4] underscoring the heterogeneity in AFH morphology and the nonspecific nature of its immunohistochemistry. However, the presence of classic morphological features and positive immunostaining for desmin, CD68, or CD99 should prompt consideration of AFH, warranting further molecular testing.
AFH is associated with three characteristic translocations: t (2:22) (q33: q12) (producing an EWSR1-CREB1 fusion gene), t (12:22) (q13: q12) (producing an EWSR1-ATF1 fusion gene), and t (12:16) (q13: p11) (producing a FUS-ATF1 fusion gene). EWSR1 and FUS belong to the FET RNA-binding protein family, which is involved in various processes, such as gene expression regulation, genome integrity maintenance, and messenger RNA processing [4, 10]. Although FUS-ATF1 gene fusion is a unique genetic change in AFH, its incidence is very low [11], and > 90% of the genetic changes in AFH are EWSR1-CREB1 gene fusions [4]. Currently, FISH and reverse-transcription polymerase chain reaction are the main diagnostic tools to detect EWSR1 rearrangement, particularly in variant AFH or biopsy specimens [4]. Tanas found EWSR1 rearrangement in 13 of 17 AFH cases (76.5%), but no FUS rearrangement, which suggests that EWSR1 is a common genetic event in AFH [12]. Consistent with previous reports, our results indicate that EWSR1 gene rearrangement was detected in 13 out of 14 cases (93%). However, EWSR1 involves the recombination of multiple companion genes, and the same EWSR1 gene recombination can also result in different tumor entities that have different clinical and pathological characteristics. Currently, it is not clear how the same gene fusion produces different tumor types. One possible explanation is that these tumors originate from progenitor cells at different anatomical sites, which have different histological forms corresponding to specific cells of origin [13].
The classic morphological characteristics of AFH are not usually prominent and result from clinical manifestations, imaging, and genetic similarities, which is why AFH is often misdiagnosed [14]. The differential diagnosis of AFH includes various benign and malignant tumors as follows. (1) Primary pulmonary myxoid sarcoma (PPMS): PPMS is more common in young people and also exhibits EWSR1-CREB1 gene fusion. PPMS is lobulated and may have a fibrous capsule. The tumor consists of spindle- or oval-shaped cells arranged in clusters and cords, with a mild cell morphology. The tumor stroma typically has a prominent mucinous-like matrix and abundant infiltration of lymphoid plasma cells. Compared with AFH, PPMS typically has a larger average volume (4 cm vs. 2 cm), a more extensive mucoid matrix, and necrosis, and PPMS does not contain a lymphocyte sheath [15,16,17]. The expression of desmin is more indicative of an AFH diagnosis. In one case of pulmonary AFH, we observed EWSR1 gene segregation, which exhibited diverse cytological morphology and a mucoid matrix, which was very similar to PPMS. However, a lymphocyte sheath was observed in this tumor along with immunohistochemical expression of desmin. Therefore, we ultimately diagnosed this tumor as AFH; however, the relationship between PPMS and AFH is still being studied. Owing to the similarity in morphology, immunophenotype, and molecular genetics, it has been suggested that PPMS and AFH represent the same disease lineage. They may originate from primitive mesenchymal cells driven by similar EWSR1 fusion gene products and may be closely related in lineage and pathogenesis [18]. However, similar fusion gene products can drive tumor growth in different anatomical and cellular environments, resulting in various tumors having overlapping or different forms and phenotypes. Therefore, different tumors with the same gene translocation cannot be simply classified as the same disease lineage. (2) Intracranial mucinous mesenchymal tumors (IMMT): this is a novel central nervous system tumor described in recent studies [19] and characterized by a molecular change in the fusion of FET family genes with CREB family transcription factors. There are many overlaps with AFH in terms of organizational structure (including characteristic mucinous matrix), cell morphology, and immunohistochemistry. We analyzed two brain tumor cases (one of the meninges and one of brain parenchyma), both of which had epithelioid to spindle-shaped tumor cells and a local mucinous matrix in the tumor stroma. Both expressed desmin and exhibited EWSR1 gene isolation. Based on the extensive similarity with pathological characteristics of AFH, it is believed that IMMT may be an AFH that occurs in the brain [20]; however, further studies are needed to determine whether IMMT and AFH represent single entities, including epigenetic analyses to determine the true attributes of these unique intracranial tumors. (3) Inflammatory myofibroblastoma (IMT): this tumor type is more common in children and adolescents. The tumors are composed of spindle-shaped fibroblasts and myofibroblasts and are often accompanied by varying degrees of collagenization and mixed inflammatory cells between tumor cells. However, IMT lacks a fibrous pseudocapsule and lymphocyte sheath and is often associated with an ALK gene rearrangement without EWSR1 gene changes. (4) Myoepithelioma: microscopically, it can exhibit various cell morphology, arrangement, and interstitial manifestations. The histological morphology of epithelioid to spindle-like cells in AFH can be similar to that of myoepithelioma; however, myoepithelioma does not show characteristics such as lymphocyte sheaths and tissue/dendritic cell complex arrangements. Myoepithelial tumors express CKpan, S100, and caponin, although desmin positivity is rare. It should be noted that myoepithelioma may contain fusion genes, such as EWSR1-POU5F or EWSR1-PBX1 [21, 22]. Therefore, the EWSR1 fusion probe should be used to differentiate tumors from AFH. (5) Aneurysmal fibrous histiocytoma: this is a rare variant of skin fibroma. The tumor is located in superficial soft tissue and has a hemorrhagic cavity, which may lead to its misdiagnosis as AFH. However, aneurysmal fibrous histiocytoma primarily occurs in the dermis and retains the typical structural characteristics of skin fibromas, such as epidermal hyperplasia and peripheral collagen bundles. Aneurysmal fibrous histiocytoma also has a more heterogeneous cell population compared with AFH (such as giant cells and iron phagocytes), lacks infiltration of surrounding lymphatic plasma cells, and does not express desmin [4].
Although the overall prognosis of AFH is good, studies have shown a local recurrence rate of up to 15%. Recurrence is more common in cases with invasive growth, larger tumor volume, and higher average age [3, 4, 23, 24]. In the present study, one patient (1/14, 7%) experienced local tumor recurrence, who was the oldest and exhibited the largest tumor volume among the 14 patients. In addition, unlike the other 13 cases, this case did not exhibit any classic histological features of AFH under microscopic examination. The absence of these histological manifestations may also impact its prognosis, which has not been mentioned in current literature. However, further analysis and confirmation with more cases are required.
In summary, AFH is a rare intermediate tumor that often presents with diverse histological patterns, particularly when located in uncommon sites, which complicates accurate diagnosis. Our results indicate that in cases wherein patients present with spindle cell tumors exhibiting benign clinical manifestations, microscopic examination revealing features such as hemorrhagic gaps, lymphocytic sleeves, or fibrous capsules, along with positive immunohistochemical staining for desmin, CD68, or CD99, and evidence for EWSR1 gene rearrangement, AFH should be considered. Moreover, extensive sampling to identify classic histological patterns is crucial for improving the detection rate of AFH.
Availability of data and materials
The datasets generated and/or analyzed in the present study are available from the corresponding author upon reasonable request.
References
Enzinger FM (1979) Angiomatoid malignant fibrous histiocytoma: a distinct fibrohistiocytic tumor of children and young adults simulating a vascular neoplasm. Cancer 44:2147–2157
Costa MJ, Weiss SW (1990) Angiomatoid malignant fibrous histiocytoma. A follow-up study of 108 cases with evaluation of possible histologic predictors of outcome. Am J Surg Pathol 14:1126–1132
Bharat R, Gang C (2020) WHO classification of tumours: soft tissue and bone tumours. IARC Press, Lyon, pp 271–273
Thway K, Fisher C (2015) Angiomatoid fibrous histiocytoma: the current status of pathology and genetics. Arch Pathol Lab Med 139:674–682
Fletcher CD (1991) Angiomatoid “malignant fibrous histiocytoma”: an immunohistochemical study indicative of myoid differentiation. Hum Pathol 22:563–568
Kao YC, Lan J, Tai HC et al (2014) Angiomatoid fibrous histiocytoma: clinicopathological and molecular characterisation with emphasis on variant histomorphology. J Clin Pathol 67:210–215
Gong QX, Zhang ZH, Fan QH (2018) Myxoid variant of angiomatoid fibrous histiocytoma: a clinicopathologic analysis of 3 cases. Zhonghua Bing Li Xue Za Zhi 47:700–705
Maqbool H, Bashir S, Hassan U et al (2022) Angiomatoid fibrous histiocytoma: a tumor with uncertain behavior and various clinicopathological presentations. Cureus 14:e28985
Chen G, Folpe AL, Colby TV et al (2011) Angiomatoid fibrous histiocytoma: unusual sites and unusual morphology. Mod Pathol 24:1560–1570
Andersson MK, Ståhlberg A, Arvidsson Y et al (2008) The multifunctional FUS, EWS and TAF15 proto-oncoproteins show cell type-specific expression patterns and involvement in cell spreading and stress response. BMC Cell Biol 9:37
Moura RD, Wang X, Lonzo ML et al (2011) Reticular angiomatoid “malignant” fibrous histiocytoma—a case report with cytogenetics and molecular genetic analyses. Hum Pathol 42:1359–1363
Tanas MR, Rubin BP, Montgomery EA et al (2010) Utility of FISH in the diagnosis of angiomatoid fibrous histiocytoma: a series of 18 cases. Mod Pathol 23:93–97
Taylor BS, Barretina J, Maki RG et al (2011) Advances in sarcoma genomics and new therapeutic targets. Nat Rev Cancer 11:541–557
Rekhi B, Adamane S, Ghodke K et al (2016) Angiomatoid fibrous histiocytoma: clinicopathological spectrum of five cases, including EWSR1-CREB1 positive result in a single case. Indian J Pathol Microbiol 59:148–152
Wang Z, Zhang L, Ren L et al (2021) Distinct clinicopathological features of pulmonary primary angiomatoid fibrous histiocytoma: a report of four new cases and review of the literature. Thorac Cancer 12:314–323
Chen Z, Yang Y, Chen R et al (2020) Primary pulmonary myxoid sarcoma with EWSR1-CREB1 fusion: a case report and review of the literature. Diagn Pathol 15:15
Chen Q, Li F, He L et al (2020) A case of pulmonary solid angiomatoid fibrous histiocytoma. J Clin Exp Pathol 06:750–751
Gui H, Sussman RT, Jian B et al (2020) Primary pulmonary myxoid sarcoma and myxoid angiomatoid fibrous histiocytoma: a unifying continuum with shared and distinct features. Am J Surg Pathol 44:1535–1540
Sloan EA, Chiang J, Villanueva-Meyer JE et al (2021) Intracranial mesenchymal tumor with FET-CREB fusion-A unifying diagnosis for the spectrum of intracranial myxoid mesenchymal tumors and angiomatoid fibrous histiocytoma-like neoplasms. Brain Pathol 31:e12918
Tauziède-Espariat A, Sievers P, Larousserie F et al (2022) An integrative histopathological and epigenetic characterization of primary intracranial mesenchymal tumors, FET: CREB-fused broadening the spectrum of tumor entities in comparison with their soft tissue counterparts. Brain Pathol 32:e13010
Suurmeijer AJH, Dickson BC, Swanson D et al (2020) A morphologic and molecular reappraisal of myoepithelial tumors of soft tissue, bone, and viscera with EWSR1 and FUS gene rearrangements. Genes Chromosom Cancer 59:348–356
Jo VY, Fletcher CD (2015) Myoepithelial neoplasms of soft tissue: an updated review of the clinicopathologic, immunophenotypic, and genetic features. Head Neck Pathol 9:32–38
Hashimoto K, Nishimura S, Kakinoki R et al (2018) Treatment of angiomatoid fibrous histiocytoma after unplanned excision: a case report. BMC Res Notes 11:628
Maharjan S, Satyal B, Baidya R et al (2022) Angiomatoid fibrous histiocytoma mimicking a lymph nodal lesion: a case report. JNMA J Nepal Med Assoc 60:200–203
Acknowledgements
Not applicable.
Funding
This study was financially supported by the National Key Clinical Specialty Discipline Construction Program of China (2022YBL-ZD-02).
Author information
Authors and Affiliations
Contributions
All authors participated sufficiently in the study to take public responsibility for the content. Specifically, QZ was involved in data collection and drafting, JL contributed to the analysis and revision of the manuscript, GL, YC, and FS participated in the equipment, reagents, and experimental procedures of the study, while FG contributed to the conception of the manuscript and provided financial support. In addition, each author confirms that this material or similar material has not been and will not be submitted or published in any other publication.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interest.
Consent for publication
Not applicable.
Ethical approval
The study complied with the Helsinki Declaration, and the study protocol and exemption of informed consent were approved by the Institutional Ethics Committee of the First Affiliated Hospital of Fujian Medical University, Fuzhou, China (IEC-FOM-013-2.0).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zeng, Q., Li, Jz., Li, Gp. et al. Clinical and pathological analyses of 14 cases of angiomatoid fibrous histiocytoma. Med Mol Morphol (2024). https://doi.org/10.1007/s00795-024-00400-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00795-024-00400-4