Abstract
Objectives
Irisin plays an important role in energy homeostasis, inflammation, glucose, and lipid metabolism, and it is shown to have relations with many inflammatory diseases. The aim of the study was to determine saliva and serum irisin and IL-6 levels in patients with stage III/grade B periodontitis compared with individuals with healthy periodontium.
Materials and methods
Twenty patients with stage III grade B periodontitis (P) and 20 periodontally healthy subjects (control; C) were included in this study. Clinical periodontal measurements were recorded. Saliva and serum levels of irisin and interleukin-6 (IL-6) were analyzed by enzyme-linked immunosorbent assay.
Results
Salivary irisin and IL-6 levels were significantly higher in the periodontitis group (p < 0.001, p = 0.002, respectively). Furthermore, serum IL-6 levels were found significantly higher in the periodontitis group compared with controls (p = 0.011). There was no significant difference between the periodontitis and control for serum irisin levels (p > 0.05). Significant positive correlations were found between all periodontal parameters and salivary irisin and IL-6 (p < 0.05) and also between BMI and saliva and serum IL-6 (respectively; r = 0.530, r = 0.329, p < 0.05). There was a positive correlation between salivary irisin and IL-6 (r = 0.369, p < 0.05).
Conclusions
Monitoring of salivary irisin and IL-6 might be potential biomarker for predicting the susceptibility to periodontitis.
Clinical relevance
Scientific rationale for the study: Irisin is a novel adipomyokine that has played an important role in energy homeostasis, glucose and lipid metabolism, angiogenesis, immunity, and inflammation. Irisin is involved in the pathogenesis of diseases affecting many body systems. IL-6, another adipomyokine, is a major inflammatory mediator and homeostatic regulator of glucose and lipid metabolism and is associated with periodontitis. No studies investigated the relationship between advanced periodontal disease, irisin, and IL-6 together.
Principal findings: The salivary irisin and IL-6 levels were significantly higher and positively correlated in patients with periodontitis relative to healthy controls. Furthermore, serum IL-6 levels were significantly increased in patients with periodontitis.
Practical implications: The study shows that irisin and IL-6 can be candidate salivary biomarkers for periodontitis and predict to periodontal status.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adipokines, which are factors secreted by adipose tissue, are bioactive peptides and hormone-like proteins such as adiponectin, resistin, leptin, and irisin as well as cytokines such as tumor necrosis factor-α (TNF-α) and interleukin-6 (IL-6). These factors have been reported to play a role in inflammation and immune response including glucose and lipid metabolism, neuroendocrine function, reproduction, and cardiovascular function [1].
Irisin is a novel adipomyokine known as a mediator of physical activity that is produced mainly by skeletal muscle and adipose tissues. It is cleaved from the fibronectin type III domain-containing protein 5 (FDNC5), which is, in turn, induced by peroxisome proliferator-activated receptor-ɣ co-activator 1-α (PGC-1α) [2]. Irisin has a critical role in energy homeostasis, glucose, and lipid metabolism and angiogenesis stimulation [3]. Irisin drives browning of mature white adipocytes in response to exercise, and the resultant increase in thermogenesis improved glucose tolerance and decreases insulin resistance and adipogenesis [4, 5]. Irisin regulates lipopolysaccharide (LPS)-induced rise in nuclear factor kappa B (NF-kB), TNF-α, and IL-6 levels in adipose tissue (6). It modulates metabolic processes and maintains the balance between bone formation and resorption [6]. Several studies reported that irisin is related with pathogenesis of many diseases which are known to be associated with periodontal disease such as obesity [7], diabetes mellitus [8], rheumatoid arthritis [9], cardiovascular disease [10], and metabolic bone diseases [11].
IL-6 is a multifunctional cytokine that is released by many cell types involving macrophages, adipocytes, skeletal muscle, endothelial cells, and fibroblasts in the early stages of inflammation [12]. IL-6 is a major inflammatory mediator and crucial regulator of acute phase proteins [13]. It is regulated by several factors including hypoxia, infection, cytokines, hormones, stress, and exercise [14]. IL-6 is a homeostatic regulator of energy and lipid metabolism [15]. IL-6, together with irisin, is involved in the regulation of liver autophagy [16]. Similarly, to irisin, several studies have shown its infusion leading to reduced energy intake and improved in insulin sensitivity [17]. IL-6 has also been associated with poorer metabolic health and many chronic inflammatory diseases such as periodontitis [18], obesity [14], diabetes [19], rheumatoid arthritis [20], and cardiovascular disease [21].
Periodontitis is a chronic inflammatory disease and is characterized by destruction of tooth-supporting tissues [22]. It develops with the interactions between the dysbiotic dental biofilm and the host immuno-inflammatory response [23]. With the result of inflammation and development of periodontitis, a change in microbial composition occurs and several putative pathogens emerge, resulting in increased host-induced tissue damage [24].
Periodontitis is closely related with diabetes and obesity in which irisin and IL-6 play roles in their pathogenesis. Recently, a bidirectional relationship has been identified between periodontitis, obesity, and diabetes related to the production of advanced glycation end products that trigger inflammatory cytokine production [25, 26]. It has been reported that there are associations between periodontitis, glucose, and lipid metabolisms [27]. There are several studies that have reported that increased IL-6 levels are associated with progression and severity of periodontitis [18, 28, 29]. Recently, it has been shown that irisin is expressed in human periodontal ligament cells (hPDLCs), dental pulp stem cells (hDPCs), and osteoblasts [30]. Also, a few studies revealed that irisin promotes growth, migration and matrix formation in hPDL cells [31], and cementoblast differentiation [32]. To the best of our knowledge, there is one study that has reported the higher levels of irisin in saliva in patient with chronic periodontitis [33]. Although this study tried to give a clue about the role of irisin in periodontitis, there is no study that has assessed irisin levels in the presence of advanced periodontal disease and also in serum. Therefore, we hypothesized that irisin may play a role in severe inflammation in periodontitis, and the aim of the present study was to determine saliva and serum irisin and IL-6 levels in patients with stage III/grade B periodontitis compared with individuals with healthy periodontium.
Materials and methods
Study population and diagnosis
Twenty systemically healthy subjects with healthy periodontium and 20 patients with stage III grade B generalized periodontitis were enrolled for this cross-sectional study.
For all study subjects, the exclusion criteria were (1) use of contraceptive drugs; (2) use of antibiotics, anti-inflammatory drugs, or immunosuppressants in the last 3 months before the study; (3) alcohol consumption; (4) pregnancy or breastfeeding; (5) taking drugs that could cause side effects such as gingival hypertrophy or hyperplasia; and (6) any periodontal treatments in the 3 months prior to enrollment. All participants were systemically healthy and non-smokers (never smokers) [34].
The clinical periodontal parameters (plaque index (PI), probing pocket depth (PD), gingival recession (GR), clinical attachment loss (CAL), and bleeding on probing (BOP)) were recorded on periodontal charts in each patient [30]. All periodontal indices were measured in six sites in each tooth present in the arch by one calibrated periodontist (EVU). Body mass index (BMI) was calculated as body weight in kilograms (kg) divided by the square of the height in meters (m).
All participants had at least 20 teeth (excluding third molars). Healthy patients enrolled presented no signs of inflammation, less than 10% of periodontal sites with BOP, no sites with PD ≥ 3 mm, and no radiographic signs of bone loss. Periodontitis patients consisted of generalized stage III–grade B and were selected from individuals who had interdental CAL ≥ 5 mm, PD ≥ 6 mm on at least two non-adjacent teeth, and radiographic bone loss extending to the middle or apical third of the root. These subjects had attachment and bone loss at ≥ 30% of the teeth and loss of ≤ 4 teeth due to periodontitis. Periodontitis grade has been determined by radiographic bone loss/age index. According to this, subjects between 0.25 and 1.00 were categorized as grade B [35].
Samples collection and laboratory analysis
The serum and unstimulated saliva samples were taken from all patients between 8:00 and 10:00 in the morning. The participants had refrained from performing oral hygiene applications, eating, and drinking for at least 2 h prior to specimen collection. The samples were taken before the periodontal examination. Saliva samples were centrifuged at 10,000 rpm (10 min), whereas venous blood samples were centrifuged at 4000 rpm for 10 min. All samples were transferred into Eppendorf tubes then preserved at − 80 °C until the day of the analysis [36].
For the analysis of irisin and IL-6, specific ELISA Kits (Elabscience, Houston, Texas, USA) were used to determine the molecules in both serum and saliva samples in accordance with the manufacturer’s instructions. The minimum levels of saliva irisin and IL-6 for our samples were 1.28 and 13.22 pg/ml, respectively. For serum, irisin level was 175.43, whereas IL-6 was 0.06 pg/ml. All samples were run in duplicate, and values have been averaged.
Statistical analyses
The power analysis was performed using a specific software (3.1.9.2 G*Power; https://www.psychologie.hhu.de/arbeitsgruppen/allgemeine-psychologie-und-arbeitspsychologie/gpower.html) before the initiation of the study. A total of 38 subjects per group are necessary to provide a statistical power (1–β) of 0.8 and a type I error rate of 0.05 according to the clinical differences.
All analyses were performed by commercial statistical software (SPSS 22.0 package for Windows, IBM Inc., Armonk, NY, USA). Data normality was determined using Shapiro–Wilk test and Kolmogorov–Smirnov test. For intergroup comparisons, the Mann–Whitney U test was used to compare the differences between non-normally distributed parameters while the Student t test was used for normally distributed parameters. Specifically, the numerical variables were analyzed using the Kruskal–Wallis test. Fisher–Freeman–Halton exact chi-square test and continuity (Yates) correction were used to compare qualitative data. Pearson correlation analysis was used to analyze the relationships between parameters conforming to the normal distribution, while Spearman’s rho correlation analysis was used to analyze the relationships between parameters not conforming to the normal distribution. All tests were performed at α = 0.05 significance level.
Results
Study population and clinical findings
This study involved twenty patients with stage III grade B generalized periodontitis (9 females, 11 males and mean age: 41.10 ± 6.42 years) and 20 periodontally healthy individuals (11 females, 9 males and mean age: 34.15 ± 7.37 years).
Demographic data and full mouth periodontal parameters are presented in Table 1. Periodontal measurements (PI, BOP, PD, CAL), age, and BMI were significantly higher in the periodontitis group compared with controls (p < 0.05). As shown in Table 1, there were no significant differences between groups regarding gender (p = 0.752).
Biochemical findings
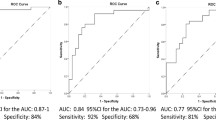
The biochemical parameters of groups are reported in Fig. 1 and Table 1. Salivary irisin and IL-6 levels were significantly higher in the periodontitis group (p < 0.001, p = 0.002, respectively; Fig. 1). Furthermore, serum IL-6 levels were found significantly higher in the periodontitis group compared with controls (p = 0.011, Table 1). There was found no statistically significant difference between the periodontitis and control groups in terms of serum irisin levels (p = 0.49; Table 1).
Comparisons of saliva and serum levels of ırisin and interleukin-6 (IL-6) for patients with periodontitis and periodontally healthy volunteers. Data shown as mean ± standard deviation. Asterisk symbol (*) indicates the following: significantly different (P < 0.05). Intergroup differences were determined using the Mann–Whitney U test
Correlations
The correlations between the biochemical parameters and the clinical periodontal measurements are presented in Table 2. Saliva irisin and saliva IL-6 were positively correlated with all periodontal clinical parameters, and most strongly correlated PD with saliva irisin (r = 0.546, p < 0.001). Serum irisin was not significantly correlated with any clinical parameters (p > 0.05), whereas serum IL-6 was positively correlated with only the BOP (r = 0.528, p < 0.05). There was a positive correlation between saliva irisin and saliva IL-6 (r = 0.369, p < 0.05), whereas there were no statistically significant correlations among other biochemical parameters (p > 0.05).
The correlation of BMI and age with biomarkers both in all participants (n = 40) and in periodontitis (n = 20) and healthy (n = 20) groups separately is shown in Table 3. However, a positive correlation between BMI and IL-6 (for both saliva and serum) (respectively; r = 0.530, r = 0.329, p < 0.05) was obtained; there has been no correlation between age and any molecules analyzed (p < 0.05) in all participants included (periodontitis and healthy groups both, n = 40). BMI was found to correlate only with serum IL-6 in periodontitis group (n = 20) (r = 0.464, p < 0.05). Similarly, when evaluated separately in the groups, there is no correlation between age and any molecule in neither the periodontitis nor the healthy group (p > 0.05).
Discussion
Periodontitis is characterized by low-grade inflammation that affects glucose and lipid metabolism [27]. Although the roles of IL-6 in inflammation have been demonstrated in the pathogenesis of periodontitis [18], IL-6 is an important regulator of glucose and lipid metabolism as well as inflammation [15]. Additionally, it has been reported that irisin has a major role in energy homeostasis, glucose, and lipid metabolism [3], and there is one study that has shown the increased levels of irisin in saliva in patient with chronic periodontitis [33]. However, there is no study that assessed the possible role of irisin in the pathogenesis of periodontitis together with IL-6 in advanced periodontal disease and also in serum. Therefore, we evaluated saliva and serum levels of irisin and IL-6 in patients with stage III/grade B periodontitis.
In this study, it was shown that irisin levels in saliva and IL-6 levels in saliva and serum were significantly higher in patients with stage III/grade B periodontitis than periodontally healthy individuals. We have demonstrated that increased irisin levels in saliva were related with generalized periodontitis for the first time. Irisin is known to plays a role in insulin secretion and sensitivity, glucose/lipid homeostasis, bone metabolism, inflammation, and metabolic diseases [6, 37]. Irisin improves glucose and lipid metabolism by regulating the AMPK (AMP-activated protein kinase) and p38 mitogen-activated protein kinase (p38 MAPK) signaling pathways [37, 38]. Irisin has been associated with markers of glucose and lipid homeostasis disturbance in a patient with obesity and metabolic syndrome. Stengel et al. (2013) reported that the circulating irisin levels were higher in obesity and positively correlated with altered BMI [7]. Park et al. (2022) demonstrated the high circulating irisin levels associated with metabolic syndrome and increased insulin resistance [39]. Also, increased serum irisin levels in a patient with type I diabetes mellitus have been shown [8]. Similarly, several studies reported that IL-6 improves glucose and lipid homeostasis and its increased level related with metabolic syndrome, diabetes, obesity, and BMI [14, 15, 19]. Periodontitis is closely associated with diseases such as obesity and diabetes, and glucose and lipid metabolism also play a role in the common pathogenesis of these diseases [27]. The findings of increased irisin and IL-6 levels in these studies are consistent with the findings of higher salivary irisin levels in periodontitis in our study. Also, one of the reasons for increased salivary irisin levels in periodontitis in our study can be explained by the fact that periodontitis group had a higher BMI. Recently, the increase in BMI has been associated with severity of periodontitis [40]. Various potential mechanisms could explain the relationship between obesity and periodontitis. The link between periodontitis and obesity is mediated through multiple inflammatory pathways involving cellular components and various mediators. Obesity is related with an altered pro‑ and anti-inflammatory cytokine network [25]. IL-6 may form a multidirectional link among periodontitis and obesity [27]. Recent studies have reported that a close involvement of irisin in inflammatory processes [41]. Obesity may also influence periodontal status by effecting glucose and lipid metabolism which can be regulated by IL-6 and irisin [27]. The positive correlation between BMI and IL-6 detected in periodontitis in our study, together with increased irisin levels, can be explained by these potential mechanisms. Additionally, in the present study, we found that individuals with periodontitis were older. It is known that the incidence of periodontitis increases with age [42]. Also, it was determined that irisin and IL-6 were not correlated with age. These results support potential mechanisms by which irisin and IL-6 are involved in glucose and lipid metabolism rather than aging in periodontitis.
It has been reported that irisin may have varying effects on NF-κB that depend on the pathway that it is acting on [43]. Irisin decreases the activity of NF-κB via inhibition of tool-like receptor 4/nuclear factor erythroid 2–related factor (TLR4/NRF2) and AMPK pathways resulting in reduced production of inflammatory markers such as IL-6 [43], whereas it also upregulates NF-κB activity which stimulated the release of CXCL1 in the adipocytes [44]. Irisin enhances osteoblast proliferation and differentiation via activating the p38/extracellular signal-regulated kinase (p38/ERK) MAPK pathways [38]. Besides, it has been shown that irisin increases sclerostin expression in osteocytes to induce bone resorption [45]. Buscemi et al. (2020) reported that serum irisin levels were increased in severely inflamed patients compared with the normal population, according to CRP levels [46]. On the contrary, there are several studies that associate lower irisin levels with rheumatoid arthritis [9], type 2 diabetes mellitus [47], cardiovascular diseases [10], and metabolic bone diseases [11]. These signal pathways such as MAPKs/AMPK/NF-κB/TLR4 influenced by the irisin have an important role in the pathogenesis of periodontitis [48, 49]. The findings of increased salivary irisin levels in periodontitis in our study may suggest that irisin is produced as a compensatory response to reduce or limit increased inflammatory signaling in response to periodontal disease.
Additionally, Yang et al. (2021) demonstrated that irisin is expressed and differently regulated in hPDLCs, hDPCs, and osteoblast. Pullisaar et al. (2020) reported that irisin induced cell growth, migration, and matrix formation in hPDLCs [31]. Also, a study by Zhu et al. (2020) shown that irisin promotes cementoblast differentiation by p38 MAPK pathway [32]. Consistent with our findings, a recent study by Khan et al. (2022) reported the increased salivary irisin levels in a patient with chronic periodontitis [33]. In addition to this study, we associated, for the first time, increased salivary irisin levels with stage III/grade B generalized periodontitis, a severe form of periodontal disease. In addition, increased IL-6 levels, which have been found to be associated with the progression and severity of periodontitis in many studies [18, 28, 29], were found to be higher in saliva and serum levels in periodontitis in our study. In this study, we also evaluated serum irisin levels; however, we did not find a significant difference in serum levels of irisin between a patient with periodontitis and healthy controls. It is known that irisin is produced in the serous and mucous acinar cells of salivary glands [50]. The salivary glands may contribute to the higher irisin levels in saliva in periodontitis. Thus, we think that saliva levels of irisin are more reliable in monitoring the potential role of irisin in periodontitis.
In the current study, positive correlations were found between all clinical parameters and saliva irisin and saliva IL-6 level. These findings for IL-6 are consistent with a previous study [29], and correlations for irisin have also been shown for the first time. Also, we have found positive correlations between the saliva and serum IL-6 levels and BMI, consistent with previous studies [28, 51]. This result may also be explained by the central role of IL-6 in the regulation of lipid metabolism [15]. We have shown that saliva irisin level is positively correlated with saliva IL-6 level for the first time. This study findings demonstrated that increased irisin and IL-6 levels in saliva are related with periodontitis and indicating that increased levels and correlations of these may help to predict the clinical sign of periodontal disease.
The main limitation of this study is the relatively small sample size. Another limitation is the controversy regarding commercially available irisin ELISA kits. The specificity of antibody detection of irisin, its cross-reactivity with precursor FNDC5, and the wide range of irisin values in different studies are among these controversies. It has been reported that the epitope of a protein may be masked in serum or plasma if present in complex with other proteins. Thus, a validated antibody that can quantify levels of irisin in serum is required [52]. Also, irisin can be induced by exercise; however, not evaluating irisin responses in relation to exercise or training in this study can be considered as another limitation.
In the present study, the results have emphasized the importance of irisin and IL-6 in periodontitis and their correlation with periodontal status. Increased saliva irisin and saliva and serum IL-6 levels in severe periodontitis may suggest irisin and IL-6 are regulating periodontal inflammation. However, further analysis and larger sample size are needed to fully elucidate the role of irisin in pathogenesis of periodontitis.
Conclusion
This is the first study evaluating saliva and serum levels of irisin in stage III grade B periodontitis. This study demonstrated that significantly higher levels of saliva irisin and saliva and serum IL-6 in a patient with periodontitis correlated with periodontal status, and, also, saliva irisin level is related with saliva IL-6 in periodontitis. Detection and monitoring of saliva irisin and IL-6 might be promising biomarkers and predict the susceptibility for periodontitis in the future with more precisely defined testing methods.
Data Availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Trayhurn P, Wood I (2004) Adipokines: inflammation and the pleiotropic role of white adipose tissue. Br J Nutr 92(3):347–355. https://doi.org/10.1079/BJN20041213
Roca-Rivada A, Castelao C, Senin LL et al (2013) FNDC5/irisin is not only a myokine but also an adipokine. FNDC5/irisin is not only a myokine but also an adipokine. PLoS One 8(4):e60563. https://doi.org/10.1371/journal.pone.0060563
Rodríguez A, Becerril S, Ezquerro S, Méndez-Giménez L, Frühbeck G (2017) Crosstalk between adipokines and myokines in fat browning. Acta Physiol (Oxf) 219(2):362–381. https://doi.org/10.1111/apha.12686
Bostrom P, Wu J, Jedrychowski MP, Korde A et al (2012) A PGC1- a-dependent myokine that drives brown-fat-like development of white fat and thermogenesis. Nature 481:463–468. https://doi.org/10.1038/nature10777
Stanford KI, Middelbeek RJ, Townsend KL et al (2013) Brown adipose tissue regulates glucose homeostasis and insulin sensitivity. J Clin Invest 123:215–223. https://doi.org/10.1172/JCI62308
Kornel A, Den Hartogh DJ, Klentrou P, Tsiani E (2021) Role of the myokine irisin on bone homeostasis: review of the current evidence. Int J Mol Sci 22(17):9136. https://doi.org/10.3390/ijms22179136
Stengel A, Hofmann T, Goebel-Stengel M, Elbelt U, Kobelt P, Klapp BF (2013) Circulating levels of irisin in patients with anorexia nervosa and different stages of obesity–correlation with body mass index. Peptides 39:125–130. https://doi.org/10.1016/j.peptides.2012.11.014
Ates I, Arikan MF, Erdogan K, Kaplan M, Yuksel M, Topcuoglu C, Yilmaz N, Guler S (2017) Factors associated with increased irisin levels in the type 1 diabetes mellitus. Endocr Regul 51(1):1–7. https://doi.org/10.1515/enr-2017-0001
Soliman SA, Gad R, Senosy T, Higazi AM, Elshereef E (2022) Serum irisin level in rheumatoid arthritis patients: relationship to disease activity, subclinical atherosclerosis, and cardiovascular risk factors. Egypt Rheumatologist 44(2):109–114. https://doi.org/10.1016/j.ejr.2021.10.008
Fu J, Li F, Tang Y, Cai L, Zeng C, Yang Y, Yang J (2021) The emerging role of irisin in cardiovascular diseases. J Am Heart Assoc 10(20):e022453. https://doi.org/10.1161/JAHA.121.022453
Polyzos SA, Anastasilakis AD, Efstathiadou ZA, Makras P, Perakakis N, Kountouras J, Mantzoros CS (2018) Irisin in metabolic diseases. Endocrine 59(2):260–274. https://doi.org/10.1007/s12020-017-1476-1
Febbraio MA, Pedersen BK (2002) Muscle-derived interleukin-6: mechanisms for activation and possible biological roles. FASEB J 16:1335–1347. https://doi.org/10.1096/fj.01-0876rev
Tanaka T, Narazaki M, Kishimoto T (2014) IL-6 in inflammation, immunity, and disease. Cold Spring Harb Perspect Biol 6(10):a016295. https://doi.org/10.1101/cshperspect.a016295
Eder K, Baffy N, Falus A, Fulop AK (2009) The major inflammatory mediator interleukin-6 and obesity. Inflamm Res 58(11):727–736. https://doi.org/10.1007/s00011-009-0060-4
Lehrskov LL, Christensen RH (2019) The role of interleukin-6 in glucose homeostasis and lipid metabolism. Semin Immunopathol 41(4):491–499. https://doi.org/10.1007/s00281-019-00747-2
Pinto AP, Ropelle ER, Quadrilatero J, da Silva ASR (2022) Physical exercise and liver autophagy: potential roles of IL-6 and irisin. Exerc Sport Sci Rev 50(2):89–96. https://doi.org/10.1249/JES.0000000000000278
Halpern B (2021) Irisin and its relationship with metabolic health: more questions than answers. Arch Endocrinol Metab 65(2):121–123. https://doi.org/10.20945/2359-3997000000355
Irwin CR, Myrillas TT (1998) The role of IL-6 in the pathogenesis of periodontal disease. Oral Dis 4(1):43–47. https://doi.org/10.1111/j.1601-0825.1998.tb00255.x
Akbari M, Hassan-Zadeh V (2018) IL-6 signalling pathways and the development of type 2 diabetes. Inflammopharmacol 26:685–698. https://doi.org/10.1007/s10787-018-0458-0
Kim GW, Lee NR, Pi RH et al (2015) IL-6 inhibitors for treatment of rheumatoid arthritis: past, present, and future. Arch Pharm Res 38:575–584. https://doi.org/10.1007/s12272-015-0569-8
Ridker PM, Rane M (2021) Interleukin-6 signaling and anti-interleukin-6 therapeutics in cardiovascular disease. Circ Res 128(11):1728–1746. https://doi.org/10.1161/CIRCRESAHA.121.319077
Gokmenoglu C, Turkmen E, Öngöz Dede F, Erbak Yilmaz H, Kara MC, Çanakçi V (2022) The resolvin D1 levels before and after periodontal therapy in periodontitis patients. Clin Oral Invest 26:6379–6385. https://doi.org/10.1007/s00784-022-04593-9
Hajishengallis G, Lamont RJ (2021) Polymicrobial communities in periodontal disease: their quasi-organismal nature and dialogue with the host. Periodontol 2000 86(1):210–230. https://doi.org/10.1111/prd.12371
Darveau RP, Curtis MA (2021) Oral biofilms revisited: a novel host tissue of bacteriological origin. Periodontol 2000 86(1):8–13. https://doi.org/10.1111/prd.12374
Pamuk F, Kantarci A (2022) Inflammation as a link between periodontal disease and obesity. Periodontol 2000 90(1):186–196. https://doi.org/10.1111/prd.12457
Teles F, Wang Y, Hajishengallis G, Hasturk H, Marchesan JT (2021) Impact of systemic factors in shaping the periodontal microbiome. Periodontol 2000 85(1):126–160. https://doi.org/10.1111/prd.12356
Washita M, Hayashi M, Nishimura Y et al (2021) The link between periodontal inflammation and obesity. Curr Oral Health Rep 8:76–83. https://doi.org/10.1007/s40496-021-00296-4
Teles FR, Teles RP, Martin L, Socransky SS, Haffajee AD (2012) Relationships among interleukin-6, tumor necrosis factor-α, adipokines, vitamin D, and chronic periodontitis. J Periodontol 83(9):1183–1191. https://doi.org/10.1902/jop.2011.110346
Isola G, Lo Giudice A, Polizzi A, Alibrandi A, Murabito P, Indelicato F (2021) Identification of the different salivary Interleukin-6 profiles in patients with periodontitis: a cross-sectional study. Arch Oral Biol 122:104997. https://doi.org/10.1016/j.archoralbio.2020.104997
Yang Y, Pullisaar H, Landin MA, Heyward CA, Schröder M, Geng T, Grano M, Reseland JE (2021) FNDC5/irisin is expressed and regulated differently in human periodontal ligament cells, dental pulp stem cells and osteoblasts. Arch Oral Biol 124:105061. https://doi.org/10.1016/j.archoralbio.2021.105061
Pullisaar H, Colaianni G, Lian AM, Vandevska-Radunovic V, Grano M, Reseland JE (2020) Irisin promotes growth, migration and matrix formation in human periodontal ligament cells. Arch Oral Biol 111:104635. https://doi.org/10.1016/j.archoralbio.2019.104635
Zhu J, Wang Y, Cao Z, Du M, Hao Y, Pan J, He H (2020) Irisin promotes cementoblast differentiation via p38 MAPK pathway. Oral Dis 26(5):974–982. https://doi.org/10.1111/odi.13307
Khan SU, Ghafoor S, Khaliq S, Syed AR (2022) Salivary irisin and periodontal clinical parameters in patients of chronic periodontitis and healthy individuals: a novel salivary myokine for periodontal disease. J Pak Med Assoc 72(1):27–33. https://doi.org/10.47391/JPMA.01367
Kurgan Ş, Önder C, Balcı N, Akdoğan N, Altıngöz SM, Serdar MA, Günhan M (2022) Influence of periodontal inflammation on tryptophan-kynurenine metabolism: a cross-sectional study. Clin Oral Invest 26:5721–5732. https://doi.org/10.1007/s00784-022-04528-4
Chapple ILC, Mealey BL, Van Dyke TE et al (2018) Periodontal health and gingival diseases and conditions on an intact and a reduced periodontium: consensus report of workgroup 1 of the 2017 World workshop on the classification of periodontal and peri-implant diseases and conditions. J Periodontol 89:S74–S84. https://doi.org/10.1111/jcpe.12940
Balci N, Kurgan Ş, Çekici A, Çakır T, Serdar MA (2021) Free amino acid composition of saliva in patients with healthy periodontium and periodontitis. Clin Oral Investig 25(6):4175–4183. https://doi.org/10.1007/s00784-021-03977-7
Mahgoub MO, D’Souza C, Al Darmaki RSMH, Baniyas MMYH, Adeghate E (2018) An update on the role of irisin in the regulation of endocrine and metabolic functions. Peptides 104:15–23. https://doi.org/10.1016/j.peptides.2018.03.018
Rabiee F, Lachinani L, Ghaedi S, Nasr-Esfahani MH, Megraw TL, Ghaedi K (2020) New insights into the cellular activities of Fndc5/Irisin and its signaling pathways. Cell Biosci 30(10):51. https://doi.org/10.1186/s13578-020-00413-3
Park KH, Zaichenko L, Brinkoetter M et al (2013) Circulating irisin in relation to insulin resistance and the metabolic syndrome. J Clin Endocrinol Metab 98(12):4899–4907. https://doi.org/10.1210/jc.2013-2373
Çetin MB, Sezgin Y, Önder C et al (2022) The relationship between body mass index and stage/grade of periodontitis: a retrospective study. Clin Oral Invest 26:1937–1945. https://doi.org/10.1007/s00784-021-04172-4
Arhire LI, Mihalache L, Covasa M (2019) Irisin: a hope in understanding and managing obesity and metabolic syndrome. Front Endocrinol 10:524
Reynolds MA (2014) Modifiable risk factors in periodontitis: at the intersection of aging and disease. Periodontol 2000 64(1):7–19
Slate-Romano JJ, Yano N, Zhao TC (2022) Irisin reduces inflammatory signaling pathways in inflammation-mediated metabolic syndrome. Mol Cell Endocrinol 552:111676. https://doi.org/10.1016/j.mce.2022.111676
Shaw A, Toth BB, Király R et al (2021) Irisin stimulates the release of CXCL1 from differentiating human subcutaneous and deep-neck derived adipocytes via upregulation of NFκB pathway. Front Cell Dev Biol 9:737872. https://doi.org/10.3389/fcell.2021.737872
Kim H, Wrann CD, Jedrychowski M et al (2018) Irisin mediates effects on bone and fat via αV integrin receptors. Cell 175(7):1756-1768.e17. https://doi.org/10.1016/j.cell.2018.10.025
Buscemi S, Corleo D, Vasto S et al (2020) Serum irisin concentrations in severely inflamed patients. Horm Metab Res 52(4):246–250
Liu JJ, Wong MD, Toy WC, Tan CS, Liu S, Ng XW, Tavintharan S, Sum CF, Lim SC (2013) Lower circulating irisin is associated with type 2 diabetes mellitus. J Diabetes Complications 27(4):365–369. https://doi.org/10.1016/j.jdiacomp.2013.03.002
Kirkwood KL, Rossa C Jr (2009) The potential of p38 MAPK inhibitors to modulate periodontal infections. Curr Drug Metab 10(1):55–67. https://doi.org/10.2174/138920009787048347
Li H, Zhang P, Lin H, Gao H, Yin J (2022) ETC-1002 Attenuates Porphyromonas gingivalis lipopolysaccharide-induced inflammation in RAW264.7 cells via the AMPK/NF-κB pathway and exerts ameliorative effects in experimental periodontitis in mice. Dis Markers 2022:8583674. https://doi.org/10.1155/2022/8583674
Aydin S, Aydin S, Kobat MA et al (2014) Decreased saliva/serum irisin concentrations in the acute myocardial infarction promising for being a new candidate biomarker for diagnosis of this pathology. Peptides 56:141–145. https://doi.org/10.1016/j.peptides.2014.04.002
Pîrsean C, Neguț C, Stefan-van Staden RI, Dinu-Pirvu CE, Armean P, Udeanu DI (2019) The salivary levels of leptin and interleukin-6 as potential inflammatory markers in children obesity. PLoS One 14(1):e0210288. https://doi.org/10.1371/journal.pone.0210288
Sanchis-Gomar F, Alis R, Lippi G (2015) Circulating irisin detection: does it really work? Trends Endocrinol Metab 26(7):335–336. https://doi.org/10.1016/j.tem.2015.05.004
Askari H, Rajani SF, Poorebrahim M, Haghi-Aminjan H, Raeis-Abdollahi E, Abdollahi M (2018) A glance at the therapeutic potential of irisin against diseases involving inflammation, oxidative stress, and apoptosis: an introductory review. Pharmacol Res 129:44–55. https://doi.org/10.1016/j.phrs.2018.01.012
Author information
Authors and Affiliations
Contributions
ET contributed to the design of the study, recorded the clinic data, and wrote the manuscript with input from other authors. EVU contributed to the design of the study, collected the samples, and helped interpret the results. FB contributed to the design of the study, wrote the manuscript with input from other authors, and helped interpret the results. NB contributed to the design of the study, performed the statistical analysis, and helped interpret the results. HT recorded the clinic data and wrote the manuscript with input from other authors. All authors reviewed and approved the submitted manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This research was approved by the Ethics Committee on Clinical Research of Istanbul Medipol University according to the Declaration of Helsinki (date: 13 April 2022; Number: 361). This study is registered at ClinicalTrials.gov as NCT05474820. All participants were informed about the content and procedures of the research, and signed informed consent was obtained.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Turkmen, E., Uzun, E.V., Bozaba, F. et al. Salivary irisin level is higher and related with interleukin-6 in generalized periodontitis. Clin Oral Invest 27, 3001–3008 (2023). https://doi.org/10.1007/s00784-023-04903-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-023-04903-9