Abstract
Introduction
Irisin is a myokine/adipokine induced by the exercise in mice and humans, which is proposed to induce “browning” of white adipose tissue, its primary target, thus increasing thermogenesis and energy expenditure. Since its identification, irisin has been linked to favorable effects on metabolic diseases, including obesity, type 2 diabetes mellitus (T2DM), lipid metabolism and cardiovascular disease (CVD), nonalcoholic fatty liver disease (NAFLD), polycystic ovary syndrome (PCOS), and metabolic bone diseases. Generally, despite the promising profile of irisin in rodents, its effects on human are less recognized.
Review
Most, but not all studies show a positive association between irisin and indices of adiposity. In T2DM, NAFLD, and CVD, most observational studies reported lower irisin levels in patients than controls. Regarding metabolic bone diseases, irisin is positively associated with bone mineral density and strength in athletes, and inversely associated with osteoporotic fractures in postmenopausal osteoporosis. In PCOS, data remain largely conflicting. Irisin does not seem to be further reduced when two metabolic diseases, e.g., T2DM and NAFLD, or obesity and NAFLD exist though more data are needed. Furthermore, it seems that diverse confounders may have affected the results of different clinical studies.
Conclusion
Irisin remains an appealing molecule from a pathophysiological point of view and an appealing therapeutic target for metabolic diseases, albeit much research is still needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The skeletal muscle communicates with other tissues, including the adipose tissue, the liver and the bone, through the secretion of hormones, collectively known as myokines, whose pattern of secretion may be altered by the type and the intensity of physical activity [1]. The identification of myokines has led to the hypothesis that some of the beneficial effects of exercise on the metabolic diseases may be related to myokines and their interactions with other systems [1].
Irisin is a novel myokine, first described by Boström et al. [2] and named after the ancient Goddess Iris, who served as a messenger among the Gods in Greek mythology [1]. Initially identified as a myokine, small amounts of irisin are also synthesized and secreted from the liver or adipose tissue [3]. Irisin is induced by the exercise in mice and humans. Irisin is proposed to induce the “browning” of white adipose tissue (WAT), which is defined as the occurrence of thermogenic brown adipocytes within the WAT, a process increasing energy expenditure [4]. Irisin induces the expression of a number of pro-myogenic and exercise response genes in myotube; its injection in mice induces significant hypertrophy due to activation of satellite cells and increased protein synthesis, thereby suggesting that irisin functions as a pro-myogenic agent [5].
The molecular sequence leading to irisin secretion is briefly the following: exercise increases the expression of peroxisome proliferator-activated receptor (PPAR)-γ co-activator (PGC)-1α, resulting in the expression of fibronectin type III domain containing (FNDC)5 [2]. FNDC5 is a membrane protein expressed in the brain and skeletal muscle; it is a type of transmembrane protein encoded by the Fndc5 gene and is the precursor of irisin, i.e., irisin is produced by proteolytic cleavage of FNCD5 at the level of cell membrane [2] by yet unknown proteolytic enzyme(s). Irisin binds to yet unknown receptor(s) of white adipocytes and other cells, including myocytes and hepatocytes [6]. Partly through increasing PPAR-α expression, irisin induces the expression of mitochondrial uncoupling protein (UCP)1 [7], which increases thermogenesis and thus energy expenditure in the skeletal muscle and brown adipose tissue (BAT) [8]. Since this effect seems to improve the metabolic profile, irisin is emerging as a promising therapeutic target for the treatment of metabolic diseases, at least those known to ameliorate with exercise [7].
Important to note, however, that despite the expectations initially generated for irisin, there is justifiable skepticism on the quality (lack of specificity) of commercially available ELISA kits currently used for the measurement of circulating FNDC5 and irisin, and on possible misinterpretation of findings of the relative existing studies [9, 10]. We have previously published on the reliability of assays and have used in our studies the most reliable assay, which is not widely available to all [11, 12].
The aim of this review is to summarize existing evidence linking irisin with metabolic disorders, including obesity, type 2 diabetes mellitus (T2DM), lipid metabolism and cardiovascular disease (CVD), nonalcoholic fatty liver disease (NAFLD), polycystic ovary syndrome (PCOS), and metabolic bone diseases.
Irisin in obesity
The WAT is considered the second most important source of irisin after the skeletal muscle [6]. In rodents, FNDC5/irisin is secreted primarily from adipocytes of the subcutaneous adipose tissue (SAT) and in lower amount from adipocytes of the visceral adipose tissue (VAT) [3]. The WAT-derived FNDC5/irisin may represent up to ~30% of its circulating levels [2, 3] and, similarly to skeletal muscle, its secretion is increased after endurance exercise training [3]. In humans though, FNDC5 expression is 100–200 times lower in WAT than in muscle, indicating a minor contribution of WAT in the circulating irisin levels [13,14,15]. Once released to circulation upon exercise or cold exposure, irisin stimulates UCP1 expression and browning of WAT, resulting in an increase in total body energy expenditure by increased UCP1-mediated thermogenesis [16].
The primary target of irisin is the adipose tissue. Irisin demonstrates differential effects depending on the species (rodents, humans), type of adipocytes (premature or mature adipocytes), and location/type of the adipose tissue (SAT, VAT, BAT). In obese mice, increase of circulating irisin levels with intravenous injection of FNDC5-expressing adenoviral particles or intraperitoneal administration of recombinant human irisin improves glucose metabolism, but has minor effects on body weight [2, 17]. Treatment of stromal vascular fractions from inguinal depots with FNDC5 stimulates browning, indicated by a 7-fold increase in UCP1 [2]. The FNDC5/irisin-treated adipocytes have multilocular lipid droplets, higher density of mitochondria, and increased energy expenditure, which are all signs of a beige/brown phenotype [2]. Additionally, in vitro or in vivo treatment with irisin stimulates basal and isoproterenol-induced lipolysis, increases lipid metabolism, and downregulates lipid synthesis in mice [18, 19]. Interestingly, recent evidence suggests that irisin is an anorexigenic factor in fish and its actions might be partly mediated by appetite-regulating factors, including cocaine and amphetamine-regulated transcript, orexins, UCP2 and brain agents such as brain-derived neurotropic factor [20]. The role of endogenous irisin on food intake is likely mediated by its actions on other metabolic peptides; unaltered endogenous irisin is required to maintain food intake in zebrafish [21]. In humans, the reduction in irisin concentrations with increased energy intake is consistent with the detrimental metabolic effects of overeating [22].
The browning effects of irisin in humans are less established compared with rodents. In human preadipocytes from SAT, irisin inhibits differentiation to mature adipocytes [23,24,25]. Interestingly, it does not stimulate browning and rather decreases browning-related genes. In contrast, in mature human adipocytes, irisin stimulates browning, indicated by an increase in UCP1 and PR/SET Domain 16 (PRDM16), probably by activation of the p38 mitogen-activated protein kinase (MAPK) and extracellular signal-regulated kinase (ERK) signaling pathway [2, 17, 23,24,25]. Additionally, irisin stimulates glycolysis demonstrated by an increase in lactate secretion [23]. The irisin-induced browning is observed primarily in human neck adipose depots and secondarily in SAT [26]. Omental or renal adipose tissue (considered BAT due to high UCP1 expression) are not affected by irisin treatment [25, 26]. This implies that irisin does not further affect BAT.
Based on the in vitro and ex vivo results, several human research studies focused on the potential correlations between circulating irisin levels and obesity. Most, but not all, studies have reported that circulating irisin is positively associated with body mass index (BMI) and weight [6, 13, 27,28,29,30,31,32]. This association remains positive also in extreme BMI phenotypes. Patients with anorexia nervosa have 15% lower circulating irisin levels compared to normal weight and 30% lower compared to morbidly obese individuals [31, 32]. Moreover, irisin is positively associated with fat mass, waist circumference, waist-to-hip ratio [27, 30, 32, 33] and muscle mass [13, 30]. Notably, obese subjects following an 8-week program of endurance exercise and strength training combined with dietary restriction demonstrated significantly higher irisin levels, which correlated positively with the circulating endothelial progenitor cells [34]. Furthermore, irisin levels are reported to correlate positively with leptin [35] and negatively with adiponectin [36]. A direct interaction between leptin and irisin is thought to be improbable, since leptin administration in humans does not alter circulating irisin [37]. Finally, weight loss reduces irisin levels, which are restored after regaining the lost weight [27, 33].
Altogether, irisin levels increase in obesity. This increase may only partially be explained by the higher fat mass and presumably the higher concentration of adipose tissue-derived irisin. It may represent a counterbalancing mechanism to increase energy expenditure and improve insulin sensitivity, though it remains to be elucidated. It may also indicate resistance to the action of irisin, similar to insulin and leptin resistance observed in obesity and T2DM [1]. Whether irisin treatment can induce browning, increase energy expenditure, reduce weight or have other positive metabolic effects in humans could be answered at the setting of prospective interventional studies.
Irisin in diabetes and gestational diabetes
Insulin resistance (IR) and diabetes mellitus
Irisin has potential multiple favorable effects on glucose homeostasis and insulin sensitivity by promoting energy expenditure, glucose uptake, and glycogenolysis and reducing gluconeogenesis, adipogenesis, and lipid accumulation [6, 38, 39]. Interventional animal studies have shown that irisin improves [2, 17] blood glucose levels by reducing IR. Additionally, it may promote pancreatic beta-cell survival and improve glucose-induced insulin secretion in lipotoxic conditions [40].
Several studies have examined the association between irisin and blood glucose levels, beta-cell function and IR in non-diabetic subjects. Fasting blood glucose has been generally positively associated with irisin levels [13, 29, 41]. In a cross-sectional study including 254 subjects with normal glucose regulation, irisin was positively correlated with beta-cell function according to the homeostasis model assessment (HOMA)-β, even after adjusting for anthropometric and metabolic confounders [42]. However, acute changes in glucose or insulin levels, as during an OGTT, do not affect irisin levels [29]. A weak but significant positive association of circulating irisin with IR in non-diabetic subjects was shown in a recent meta-analysis of 17 studies comprising of 1912 individuals [43]. Ethnic variability might affect the association, since it was found significant in people of Asiatic and American origin, but not in Europeans. This provides a plausible explanation to the contradictory findings of negative irisin association with both blood glucose and IR in a Saudi Arabian children population, in which very young age might also be a confounder [44]. Accordingly, insulin sensitivity indices show an inverse association with irisin [43, 45], with the exemption of a European study, in which a positive association was reported [15]. Interestingly, in apparently healthy individuals, higher irisin levels independently predicted the onset of diabetes in a longitudinal 2.6-year study in a Korean population [46].
In the diabetic state, irisin levels seem to dissociate between the two diabetes types. In type 1 diabetes mellitus (T1DM), irisin has been consistently reported to be higher than in controls [47, 48]. On the contrary, the majority of studies [41, 49,50,51,52,53], including two meta-analyses [25, 54], have shown lower irisin levels in T2DM patients than controls. The more recent meta-analysis, which included 15 studies with 1289 T2DM patients and 834 controls, showed lower irisin in T2DM [54]. Ethnicity, again, emerged as a determinant, since the association between T2DM and irisin was more pronounced in Asian than European populations. This might explain the contradictory findings of slightly higher irisin levels in Caucasian [55] and Saudi Arabian [56] T2DM patients, in two studies not included in the previous meta-analysis. Similarly, lower irisin levels have been reported in populations with prediabetes [57, 58] and in drug naïve T2DM patients [57, 59].
Irisin levels have also been independently associated to diabetic microvascular complications [51, 60,61,62] and macrovascular risk factors [63, 64]. In 100 newly diagnosed, non-obese, drug-naïve T2DM patients, serum irisin levels were negatively correlated with urinary albumin excretion [62]. Furthermore, T2DM patients and macroalbuminuria have significantly lower irisin levels than T2DM patients with normoalbuminuria/microalbuminuria and healthy controls [51, 52]. A more pronounced reduction in irisin levels is seen in stage 5 chronic kidney disease [60], although the reduction in muscle mass and/or the significant reduction in renal function may affect irisin levels. Thus, it seems that there is a decrease in serum irisin level in T2DM and even more substantial reduction in diabetic nephropathy patients [65]. Besides, T2DM patients with proliferative diabetic retinopathy had significantly lower serum and vitreous irisin levels than controls and patients without retinopathy [51]. In nonproliferative diabetic retinopathy, an interaction between interleukin (IL)-17A, a proinflammatory cytokine implicated in the pathogenesis of diabetic retinopathy, and irisin levels were suggested [61]. Irisin levels are also associated with indices of endothelial function, as a positive association of irisin concentration with arterial flow-mediated dilatation has been reported [62, 63]. Moreover, in Chinese patients with T2DM, irisin levels negatively correlated with advanced glycation end-products, which are established contributors to the pathogenesis of diabetic complications [53].
Irisin might be considered for the future management of T2DM. Currently, there are some experimental studies toward this direction. First, metformin was shown to increase FDNC5 mRNA/protein expression and irisin levels in diabetic mice, in an adenosine monophosphate (AMP)-activated protein kinase (AMPK) independent manner [66]. This finding implies a novel molecular mechanism by which metformin exerts its positive metabolic effects. Next, it was demonstrated that irisin administration in diabetic [39, 67] and insulin-resistant [68, 69] mice models were followed by reduced gluconeogenesis, increased glycogenesis and improvement in muscle IR, which is mediated thought the AMPK pathway [68]. Furthermore, irisin was shown to improve endothelial function in diabetic mice models [70]. Likewise, irisin can promote beta-cell survival by restraining apoptosis induced by either high glucose [71] or high saturated fatty acids [40]. Recent data indicate that β-arrestin-2 plays a crucial role in irisin-induced glucose metabolism in T2DM by regulating the p38 MAPK signaling, thereby possibly representing a novel therapeutic target of diabetes treatment; β-arrestin-2 improves glucose utilization in diabetes by increasing the glucose uptake and insulin sensitivity, as shown in mice overexpressing β-arrestin-2 [72].
Gestational diabetes mellitus (GDM)
Gestation is a physiologic condition of IR. In normal pregnancies, irisin levels have been positively correlated with fasting insulin and HOMA-IR [73, 74]. A number of studies have examined second trimester maternal circulating irisin levels in GDM in comparison to control pregnancies. The results were conflicting, showing higher [75], lower [54, 76,77,78,79,80,81], or comparable [73, 74, 82] irisin levels in GDM vs. healthy pregnancies, respectively. However, the majority of studies and a meta-analysis [80] support that irisin levels are lower in pregnancies complicated with diabetes. Furthermore, in the only study that reported higher irisin levels in GDM, this result was only apparent after model adjustment for BMI, lipids, and glucose [75].
Interestingly, one prospective study, in which irisin levels were measured both early (6–11 weeks of gestation) and later in the second trimester, showed lower early irisin levels in women who subsequently developed GDM; nevertheless, this difference was attenuated in the second trimester [73]. This finding suggests that maternal serum irisin might serve as a prognostic factor for GDM. Finally, the presence of GDM did not seem to affect cord blood irisin levels [75, 79, 83].
Irisin in NAFLD
FNDC5 is expressed in the liver, albeit in lower amounts than the skeletal muscle or adipose tissue [13]. Irisin expression is detected immunohistochemically in hepatocytes, Kupffer cells, and sinusoidal endothelial cells [84, 85]. A study with 125I-labeled irisin and single-photon emission computed tomography (SPECT/CT) showed high radioactivity in the mouse liver, implying the liver as a target for irisin [86]. Moreover, irisin was high in the gallbladder too, indicating that the hepatobiliary system possibly plays a role in irisin clearance [86]. Irisin was located inside mouse hepatic cells (AML12) and primary hepatocytes after irisin treatment [87], a finding implying hepatocyte as a target of irisin, but also a potential intra-hepatic irisin receptor, warranting further research. More interestingly, irisin expression increased in parallel with the activation of hepatic stellate cells and irisin treatment increased fibrogenic markers in activated hepatic stellate cells [88]. Hepatic irisin production can be induced, at least partly, by the constitutive androstane receptor, a nuclear receptor capable to directly induce FNDC5 expression in the liver, thus increasing circulating irisin levels in mice [38]. Irisin was shown to be involved in hepatic glucose and lipid metabolism in cell lines and animal models. In human hepatocellular carcinoma cells (HepG2), mouse and human primary hepatocytes and in diabetic mice, irisin reduced hepatic gluconeogenesis and increased glycogenesis, thereby improving glucose homeostasis [38, 39, 68, 89]. These effects were achieved via phosphoinositide 3-kinase (PI3K)/protein kinase B (Akt) [39] and AMPK [38, 68, 89] pathways. As to lipid metabolism, it was initially shown that irisin treatment prevented the palmitic acid-induced lipid accumulation in hepatocytes by inhibiting two main regulators of lipogenesis (liver X receptor-α and sterol regulatory element-binding protein [SREBP]1c) in mouse hepatic cells (AML12) and primary hepatocytes [87]. Subsequently, irisin treatment was shown to reduce cholesterol content in mouse primary hepatocytes and in high fat diet obese mice [90], or triglyceride content in human HepG2 cells [89], human primary hepatocytes and ob/ob mice [38], via activating AMPK and subsequent inhibition of SREBP2 and other lipogenic enzymes [38, 89, 90]. Of importance, injection of adenovirus carrying human FNDC5 cDNA increased serum irisin, suppressed hepatic gluconeogenic and lipogenic enzymes, thus improving IR and decreasing hepatic triglyceride (but not cholesterol) levels in ob/ob mice [38], a leptin-deficient model exerting severe steatosis [91]. These results were confirmed in irisin transgenic mice, showing 35-fold higher irisin levels than wild-type mice [91].
Irisin may also play a role in the oxidative stress and hepatic cell survival, which are closely related to the pathogenesis of NAFLD [92]. Reactive oxygen species induced by hydrogen peroxide in mouse hepatic cells were slightly reduced after treatment with irisin [93]. Formaldehyde inhalation damaged the liver (as well as the lung) together with decreasing irisin levels, which were restored after carnosine supplementation in Sprague-Dawley rats [94]. Furthermore, irisin treatment attenuated palmitic acid-induced oxidative stress in mouse hepatic cells and primary hepatocytes [87]. Some studies showed that irisin promotes cell survival in HepG2 cells in an AMPK-dependent manner [89]. More recent data indicate that augmented irisin levels might have protective roles in liver malignant cells via partial activation of the PI3K/Akt pathway, which may facilitate hepatocellular carcinoma (HCC) and decrease the sensitivity to chemotherapy [95]. Of note, NAFLD is an important risk factor for HCC development [92]. Therefore, further research is needed on the association between irisin, oxidative stress, and cell survival.
Data on irisin in human NAFLD remain controversial. In the first histologically confirmed study in NAFLD adults, we observed similar circulating irisin levels among patients with simple steatosis, nonalcoholic steatohepatitis (NASH) and obese controls, whereas higher irisin in lean controls [96]. Notably, irisin was independently associated with portal inflammation in NAFLD patients; irisin also tended to be higher, albeit statistically nonsignificantly, by increasing the severity of steatosis, lobular inflammation, and fibrosis [96]. In a post hoc analysis of the same study, we also observed that circulating irisin and homocysteine were independently and inversely associated in NAFLD patients [97]. In a more recent study with histological confirmation, both circulating irisin levels and hepatic irisin expression were higher in patients with higher steatosis grade and fibrosis stage, and in NASH patients [98]. Interestingly, the rs3480 (A>G) variant of FNDC5, but not the rs726344 variant, was protective against hepatic fibrosis (F2–F4), albeit not the severity of steatosis [98]. However, irisin levels were not associated with either FNDC5 polymorphisms. Lower irisin levels in NAFLD (assessed by transient elastography) patients than lean controls were confirmed in a more recent study [99]. Irisin levels were similar between NAFLD patients with and without T2DM [99]. On the contrary, higher irisin levels in NAFLD (assessed by ultrasonography) adults than controls of lower BMI were observed in another study [100]. Of interest, within the NAFLD group, higher irisin levels were observed in patients with mild steatosis than those with moderate-to-severe steatosis [100]. In another study, irisin levels were independently inversely associated with hepatic triglyceride content (assessed by 1H magnetic resonance spectroscopy) in obese Chinese adults [101]. In a children cohort, I148M polymorphism of patatin-like phospholipase domain-containing protein (PNPLA)3 gene was independently positively associated with plasma irisin [102]. Specifically, irisin gradually increased from individuals with the I148I variant (CC homozygous) to I148M variant (GC heterozygous) and then to M148M (GG homozygous) variant [102]. This study provided the first evidence for an association between circulating irisin and PNPLA3 gene I148M polymorphism. It is highlighted that PNPLA3 is a strong genetic factor for NAFLD and its severity; it is the most validated gene polymorphism strongly associated with the full spectrum of NAFLD, being simple steatosis, NASH, NASH-related cirrhosis, and HCC [12]. Although this study refers to children without established NAFLD [102] and the fact that PNPLA3 gene is also expressed in extra-hepatic tissues (e.g., the kidneys, brain), the results of this study warrant further research in NAFLD populations. There is no secure explanation for any discrepancies among existing clinical data on circulating irisin in human NAFLD; however, differences might be partly attributed to population (ethnicity, age, gender, BMI, sample size) and methodological differences (mainly the method used for the diagnosis of NAFLD), as well as potential differences between ELISA kits, as we have previously summarized [12].
In summary, in experimental models, irisin, acting mainly via the AMPK pathway, improves hepatic glucose homeostasis and steatosis, whereas more data are required on its effect on hepatic oxidative stress and apoptosis. On the other hand, data from clinical studies are conflicting, largely implicated by the fact that all studies are to date cross-sectional. Cohort studies in histologically confirmed NAFLD are needed to clarify the prognostic role of irisin in NAFLD and its related HCC. As a next step, a phase I randomized controlled trial is needed to evaluate the effect of recombinant irisin in NASH and fibrosis. Nonetheless, results of recombinant irisin on hepatic fibrosis, the main prognostic endpoint for advanced NASH, may be limited similar to the limited effects of metformin, which acts mainly via the same pathway (AMPK) [103].
Irisin in lipid metabolism and CVD
Lipid metabolism
As mentioned above, besides myocytes, FNDC5 is also expressed and irisin is also secreted by the adipocytes [15]. Experimental data suggest that FNDC5 expression and/or irisin administration inhibit lipid synthesis and stimulate lipolysis and intracellular lipid metabolism by regulating the expression of genes, such as Pnpla2 (which encodes adipose triglyceride lipase), hormone-sensitive lipase, and of proteins such as fatty acid-binding protein 4 [18, 19, 23]. Adipocytes treated with irisin are smaller and accumulate fewer lipids than control adipocytes [19], while ex vivo irisin and FNDC5 treatment reduce the differentiation of human preadipocytes leading to decreased fat mass [18]. In obese mice, FNDC5 overexpression and irisin perfusion reduced hyperlipidemia and hyperinsulinemia [19], while subcutaneous irisin infusion induced a reduction in plasma cholesterol through inhibition of hepatic cholesterol synthesis via AMPK-SREBP2 pathway [90].
However, in human studies data are conflicting. A positive correlation between irisin levels and an unfavorable lipid profile has been reported in most studies, e.g., circulating irisin was positively associated with fasting triglycerides in sedentary subjects [104] and patients with metabolic syndrome [105], with total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C) and fasting fatty acids in Chinese patients [106] and with TC, LDL-C and triglycerides in Korean adolescents [107], while negatively associated with high-density lipoprotein cholesterol in patients at high cardiometabolic risk [105, 108]. On the other hand, circulating irisin has been associated with a favorable lipid profile in a Central European general population [109], while in other studies no correlation of irisin with lipid parameters has been observed in healthy young individuals [110] in normal weight individuals with increased body fat (>30%) [111] and in men with mild hypercholesterolemia [112]. The reason for these discrepancies in different studies is unclear. Differences in studied populations or different ELISA kits used for irisin measurements could be responsible. Another explanation could be that, although FNDC5 expression in adipose tissue and circulating irisin is proportionally lower in obese or diabetic subjects compared to lean controls [14, 15], the increased fat mass in these individuals, who traditionally have an unfavorable lipid profile, could result in an overall irisin release that is equal or even higher than in lean controls. Statin (simvastatin) treatment has been reported to increase FNDC5 mRNA expression and irisin secretion both in vitro and in vivo [112].
Cardiovascular disease
Myocardium, being one of the largest muscles in the human body, secretes irisin and its contribution to circulating irisin levels is substantial, at least in animals [84]. Ischemic conditions of the heart, i.e., coronary artery disease (CAD) and its severe outcome, myocardial infarction (MI), modify irisin secretion [113]. This effect could be direct, through stress or damage of the cardiomyocytes, or indirect, through the unfavorable lipid profile that accompanies such conditions, as described above [104, 108]. In respect to the direct effect of CAD/MI on irisin secretion, it was initially thought that increased release from the damaged cardiomyocytes would result in higher irisin levels following MI. However, in rats, irisin tissue expression and circulating levels were lower in isoproterenol-induced MI and negatively correlated with established markers of cardiac damage, such as troponin and creatine phosphokinase-myocardial band isoenzyme (CK-MB) [114]. Similar findings have been reported in humans: not only MI [113, 115], but also CAD patients [113, 116] had lower irisin levels than controls. In addition, T2DM patients with macrovascular disease had lower irisin levels than patients without macrovascular disease and healthy controls [64], while lower irisin levels have been associated with endothelial dysfunction [117]. These findings imply that irisin is not passively released as a result of cardiomyocyte injury, as does CK-MB, but is rather energetically secreted reflecting the sufficiency of blood supply, and thus the functional potential of the cardiac muscle [113]. In the latter study [113], it has been hypothesized that, in state of reduced blood and oxygen supply, myocardium may release less irisin to restrain the metabolic demands of the heart in an attempt to compensate for the lower energy availability. This hypothesis is supported by studies suggesting regulation of FNDC5 expression by the oxidative stress [2, 112] and a significant role of irisin in energy homeostasis and cardiomyoblast growth and function [118].
Recombinant irisin treatment has shown positive cardiovascular effects in several animal studies. Specifically, irisin exerted anti-apoptotic effects on ischemic cardiomyocytes, through protection of mitochondrial function [119], and protected apolipoprotein E-deficient mice from atherosclerosis through endothelial cell proliferation [120] and/or suppression of oxidized LDL-induced cell inflammation and apoptosis [121], while inhibited vascular smooth muscle cells proliferation [122]. Similar results were reported in obese [123] and streptozotocin-induced diabetic apolipoprotein E-Null mice, through activation of the AMPK-endothelial nitric oxide synthase pathway [124]. Furthermore, irisin induced dose-dependent relaxation in mice mesenteric arteries with or without endothelium [125] and increased diastolic volume, heart rate and cardiac output in zebrafish, while knockdown of irisin showed opposing effects on cardiovascular function [21]. Regarding diabetic cardiomyopathy, recent data indicate that recombinant irisin low-dose treatment attenuates cardiac fibrosis and left ventricular function in diabetic mice, while high-dose irisin fails to diminish ventricular function impairment and augmented collagen deposition. The possible mechanism underlying the effect of low dosage involves irisin-mediated inhibition of high glucose-induced endothelial-to-mesenchymal transition; in contrast, irisin high dosage increases high glucose-induced matrix metalloproteinase expression by inducing MAPK (p38 and ERK) signaling and cardiac fibroblast proliferation and migration, thereby exerting a dose-dependent bidirectional effect on diabetic cardiomyopathy [126]. Regarding cardio-cerebrovascular disease, irisin diminishes ischemia-induced neuronal injury through the Akt and ERK1/2 signaling pathways activation and contributes to the physical exercise neuroprotective effect against cerebral ischemia, signifying that irisin might be a factor linking metabolism and cardio-cerebrovascular disease [127]. Likewise, irisin diminishes oxygen-glucose deprivation-induced neuronal injury in part through inhibiting reactive oxygen species-NOD-like receptor pyrin 3 inflammatory signaling pathway, suggesting a relative mechanism for irisin-induced therapeutic effect in ischemic stroke [128].
Recombinant irisin treatment has not been tested in human studies so far. In conclusion, irisin levels may represent a biomarker for CVD, including MI, as well as a promising treatment option for such conditions.
Irisin in PCOS
PCOS has been closely linked with obesity and other metabolic manifestations of IR syndrome, including NAFLD [129]. Data on circulating irisin levels between PCOS women and controls are to date derived from case-control studies and are inconclusive. Most studies have reported higher irisin levels in PCOS women than controls [130,131,132,133], whereas some other studies reported similar [134, 135] or lower [136] circulating irisin levels in PCOS women than controls. Irisin was higher in overweight/obese PCOS women than normal weight ones in some [131, 134, 137], but not all [135] studies having reported on this association. It should be highlighted that PCOS women had higher BMI than controls in all but two studies [133, 136], which implicates the interpretation of the results regarding irisin, since adiposity is a given confounder. In neither study irisin was higher in PCOS than controls [133, 136]. A recent meta-analysis suggested that irisin was higher in PCOS women, possibly independently of IR [138].
Some studies reported higher irisin levels in PCOS women with high-free androgen index (FAI) than those with low FAI, even after adjustment for potential confounders [137]. However, no correlation was observed between irisin and circulating androgens in another study [134]. Notably, a 6-month metformin treatment decreased circulating irisin in the PCOS women together with IR [131]. Furthermore, insulin infusion during euglycemic hyperinsulinemic clamp decreased irisin levels to a similar degree with the controls [131, 133]. These limited results may imply a possible role of irisin against IR or irisin resistance in PCOS women.
Differences in the populations and/or ELISA kits for irisin may partly explain the existing controversy. Further studies in cautiously selected populations and matched controls are needed.
Irisin in metabolic bone disease
Physical activity is a rather potent stimulus for bone formation, exerting beneficial effects both on bone mineral density (BMD) and fracture risk, although through yet unclear molecular mechanisms [139,140,141]. The association of exercise and skeletal health is further supported by the opposite condition of decreased physical activity and the invariable bone loss and profound increase in fracture risk in several conditions [142,143,144]. Since the discovery of irisin, as a myokine produced in response to exercise by the skeletal muscles, it has been suggested that this molecule might be the missing link for the cross-talk between muscles and bones [139, 145].
The hypothesis that bone tissue could be a source of FNDC5 and/or irisin upon exercise has been recently tested in 5-week-old mice: FNDC5 protein expression and irisin increased over 6-fold in bone tissue and in less extent in articular cartilage after exercise [16]. In addition, the osteogenic potential of irisin has been validated through the assessment of its effect on undifferentiated bone marrow stromal cells [146]. In this study, irisin increased osteoblast differentiation through the Wingless (Wnt)/β-catenin pathway [146], while more recently, in a study using both an anti-FNDC5 antibody and an irisin-ELISA Kit, irisin was reported to activate the p38 MAPK and ERK, thereby inducing the proliferation, differentiation, alkaline phosphatase activity, and mineralization of cultured osteoblasts [147]. In addition, the inhibition of p38 MAPK or pERK abolished the proliferative and upregulatory effects of irisin, confirming its direct effect on osteoblasts through these pathways [147]. Moreover, irisin has been reported to inhibit in vitro the receptor activator of nuclear factor-kappa B ligand (RANKL)/nuclear factor-activated T-cells (NFAT)c1 and consequently to suppress the formation of osteoclasts [148].
In the first pre-clinical in vivo study evaluating the effect of irisin on bone, recombinant irisin (100 mcg/kg/week) was administered in young healthy male mice for 4 weeks; bone formation was induced, notable reductions in osteoclast numbers were reported, cortical bone mass and strength was increased, although no effect on trabecular bone was found [139]. In addition, the expression of the most abundant bone matrix protein, namely osteopontin, was found higher, while the expression of the well-known inhibitor of Wnt/β-catenin pathway, sclerostin, was found significantly lower within the tibiae of mice treated with irisin [139]. As mechanical stimulation exerts the same effects on these bone molecules, it was speculated that irisin could be the mediator of loading-induced changes in bone [149]. Finally, it was recently reported that treatment with recombinant irisin prevented and restored bone loss and muscle atrophy in hind-limb suspended mice [150]. More specifically, micro-computed tomography analysis of femurs showed that recombinant irisin preserved both cortical and trabecular BMD, while preventing the dramatic decrease of the trabecular bone volume fraction [150].
In humans, irisin levels were also found to be inversely correlated with serum sclerostin levels among adults of variable ages in both genders [151]. Moreover and with regard to mechanical loading in the human skeleton, irisin levels in athletes were reported to be positively associated with BMD and strength [152], although it seems that acute strenuous rather than long-term exercise induces the incremental changes in serum irisin levels both in children and adults [30]. We have recently reported that irisin levels are inversely associated with previous osteoporotic fractures, independently from other factors affecting bone fragility, such as BMD, BMI, smoking, 25(OH)-vitamin D levels, and bone markers [153]. Regarding the effect of anti-osteoporotic treatment, irisin levels were not affected by a short-course treatment with either denosumab or teriparatide [153]. The inverse correlation of serum irisin levels and fragility fractures has been also confirmed in two recent studies among post-menopausal women [154, 155], suggesting that this myokine could potentially be a useful marker for the assessment of disorders of the muscle-bone unit and metabolic bone diseases [148].
In conclusion, more specifically designed studies are required to explore the possible exercise-mimetic potential of irisin against bone loss and to further determine whether this myokine could serve as a diagnostic marker and/or a novel medication for several disorders of the muscle-bone unit, including osteoporosis [148, 149]. If the results from mice are confirmed in human studies, one could envision an irisin-based treatment for physically disabled or bedridden patients.
Closing remarks
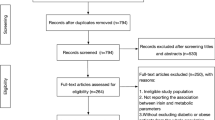
The main findings on irisin in metabolic diseases are summarized in Fig. 1, in which best evidence or currently predominant suggestive evidence are presented. It is highlighted that all clinical data are to date derived from observational studies, thereby lying lower at the pyramid of evidence.
The main findings on irisin in metabolic diseases as derived from human studies. Data represent best evidence or predominant tendency. All data are derived from observational studies. BMD bone mineral density, CVD cardiovascular disease, IR insulin resistance, NAFLD nonalcoholic fatty liver disease, PCOS polycystic ovary syndrome, T1DM type 1 diabetes mellitus, T2DM type 2 diabetes mellitus
Since the identification of irisin [2], great expectations have been arisen for the diagnosis and treatment of metabolic diseases, at least those known to improve with exercise [7]. Ideally, if irisin represented the link between the beneficial effects of exercise and improvement in metabolic diseases, treatment with recombinant irisin or with medications possibly able to upregulate the endogenous irisin would be a beneficial treatment, at least for those that are not able to regularly exercise, e.g., morbidly obese, physically disabled or bedridden handicapped patients. However, as with the identifications of other adipokines and myokines, for which there are initially high expectations for the diagnosis and treatment of metabolic diseases [156], deeper knowledge of the pathophysiology of irisin may subside our initial expectations. For example, irisin may finally prove to play a role in the pathogenesis of some but not all metabolic diseases, so the irisin treatment may not be a panacea for all metabolic diseases. The rational next step is the identifications of irisin receptor, which will shed light into its pathophysiology, but will also open a new window to related novel pharmacology. In this regard, it has been proposed that FNDC5 and irisin is subjected to glycosylation and dimerization, and therefore it remains largely unknown which is the functional isoform [88, 157]. It has been recently reported that N-glycosylation is required for FNDC5 stabilization and irisin secretion [88]. Although this remains to be further elucidated, we should cautiously consider studies with recombinant irisin use. Another issue needing cautious interpretation is the extrapolation of FNDC5 mRNA expression or circulating FNDC5 levels to irisin levels. There is weak association between mRNA and secreted proteins [158, 159], and, moreover, the enzyme(s) and the dynamics for the excision of irisin from FNDC5 remain largely unknown. For these reasons, we tried to distinguish evidence referring to circulating irisin levels from that referring to circulating FNDC5 levels or FNDC5 expression in this review.
Strong evidence favors that irisin is a true circulating protein [160], though owing to the aforementioned skepticism on the quality of commercially available ELISA kits for circulating FNDC5 and irisin [9, 10], current and future irisin ELISA kits need validation toward tandem mass spectrometry, considered to be the gold standard method [11]. As reviewed elsewhere, EK-067-52 (Phoenix Pharmaceuticals), EK-067-29 (Phoenix Pharmaceuticals), and AG-45A-0046EK-k101 (Adipogen) have been used in more than 90% of irisin studies [6]. EK-067-52 has been proposed as the best validated ELISA kit to date; nevertheless, owing to the limited availability of the former, EK-067-29 is regarded as the best currently available alternative [6]. However, for the gild to advance, most accurate antibody against irisin is needed.
Much are still needed to know about irisin and other myokines; this class of molecules remains appealing with a potential to bridge our knowledge gaps between exercise and the beneficial effects on metabolic diseases, and, most importantly, a potential to provide new weapons in our armamentarium to fight metabolic diseases.
References
S.A. Polyzos, J. Kountouras, K. Shields, C.S. Mantzoros, Irisin: a renaissance in metabolism? Metabolism 62, 1037–1044 (2013)
P. Bostrom, J. Wu, M.P. Jedrychowski, A. Korde, L. Ye, J.C. Lo, K.A. Rasbach, E.A. Bostrom, J.H. Choi, J.Z. Long, S. Kajimura, M.C. Zingaretti, B.F. Vind, H. Tu, S. Cinti, K. Hojlund, S.P. Gygi, B.M. Spiegelman, A PGC1-alpha-dependent myokine that drives brown-fat-like development of white fat and thermogenesis. Nature 481, 463–468 (2012)
A. Roca-Rivada, C. Castelao, L.L. Senin, M.O. Landrove, J. Baltar, A. Belen Crujeiras, L.M. Seoane, F.F. Casanueva, M. Pardo, FNDC5/irisin is not only a myokine but also an adipokine. PLoS ONE 8, e60563 (2013)
F. Villarroya, Irisin, turning up the heat. Cell Metab. 15, 277–278 (2012)
M.M. Reza, N. Subramaniyam, C.M. Sim, X. Ge, D. Sathiakumar, C. McFarlane, M. Sharma, R. Kambadur, Irisin is a pro-myogenic factor that induces skeletal muscle hypertrophy and rescues denervation-induced atrophy. Nat. Commun. 8, 1104 (2017)
N. Perakakis, G.A. Triantafyllou, J.M. Fernandez-Real, J.Y. Huh, K.H. Park, J. Seufert, C.S. Mantzoros, Physiology and role of irisin in glucose homeostasis. Nat. Rev. Endocrinol. 13, 324–337 (2017)
J.I. Castillo-Quan, From white to brown fat through the PGC-1alpha-dependent myokine irisin: implications for diabetes and obesity. Dis. Model Mech. 5, 293–295 (2012)
P. Puigserver, Z. Wu, C.W. Park, R. Graves, M. Wright, B.M. Spiegelman, A cold-inducible coactivator of nuclear receptors linked to adaptive thermogenesis. Cell 92, 829–839 (1998)
E. Albrecht, F. Norheim, B. Thiede, T. Holen, T. Ohashi, L. Schering, S. Lee, J. Brenmoehl, S. Thomas, C.A. Drevon, H.P. Erickson, S. Maak, Irisin—a myth rather than an exercise-inducible myokine. Sci. Rep. 5, 8889 (2015)
H.P. Erickson, Irisin and FNDC5 in retrospect: an exercise hormone or a transmembrane receptor? Adipocyte 2, 289–293 (2013)
S.A. Polyzos, H. Mathew, C.S. Mantzoros, Irisin: a true, circulating hormone. Metabolism 64, 1611–1618 (2015)
S.A. Polyzos, C.S. Mantzoros, An update on the validity of irisin assays and the link between irisin and hepatic metabolism. Metabolism 64, 937–942 (2015)
J.Y. Huh, G. Panagiotou, V. Mougios, M. Brinkoetter, M.T. Vamvini, B.E. Schneider, C.S. Mantzoros, FNDC5 and irisin in humans: I. Predictors of circulating concentrations in serum and plasma and II. mRNA expression and circulating concentrations in response to weight loss and exercise. Metabolism 61, 1725–1738 (2012)
T. Kurdiova, M. Balaz, M. Vician, D. Maderova, M. Vlcek, L. Valkovic, M. Srbecky, R. Imrich, O. Kyselovicova, V. Belan, I. Jelok, C. Wolfrum, I. Klimes, M. Krssak, E. Zemkova, D. Gasperikova, J. Ukropec, B. Ukropcova, Effects of obesity, diabetes and exercise on Fndc5 gene expression and irisin release in human skeletal muscle and adipose tissue: in vivo and in vitro studies. J. Physiol. 592, 1091–1107 (2014)
J.M. Moreno-Navarrete, F. Ortega, M. Serrano, E. Guerra, G. Pardo, F. Tinahones, W. Ricart, J.M. Fernandez-Real, Irisin is expressed and produced by human muscle and adipose tissue in association with obesity and insulin resistance. J. Clin. Endocrinol. Metab. 98, E769–E778 (2013)
J. Zhang, P. Valverde, X. Zhu, D. Murray, Y. Wu, L. Yu, H. Jiang, M.M. Dard, J. Huang, Z. Xu, Q. Tu, J. Chen, Exercise-induced irisin in bone and systemic irisin administration reveal new regulatory mechanisms of bone metabolism. Bone Res. 5, 16056 (2017)
Y. Zhang, R. Li, Y. Meng, S. Li, W. Donelan, Y. Zhao, L. Qi, M. Zhang, X. Wang, T. Cui, L.J. Yang, D. Tang, Irisin stimulates browning of white adipocytes through mitogen-activated protein kinase p38 MAP kinase and ERK MAP kinase signaling. Diabetes 63, 514–525 (2014)
S. Gao, F. Li, H. Li, Y. Huang, Y. Liu, Y. Chen, Effects and molecular mechanism of GST-Irisin on lipolysis and autocrine function in 3T3-L1 adipocytes. PLoS ONE 11, e0147480 (2016)
X.Q. Xiong, D. Chen, H.J. Sun, L. Ding, J.J. Wang, Q. Chen, Y.H. Li, Y.B. Zhou, Y. Han, F. Zhang, X.Y. Gao, Y.M. Kang, G.Q. Zhu, FNDC5 overexpression and irisin ameliorate glucose/lipid metabolic derangements and enhance lipolysis in obesity. Biochim. Biophys. Acta 1852, 1867–1875 (2015)
Z.D. Butt, J.D. Hackett, H. Volkoff, Irisin in goldfish (Carassius auratus): effects of irisin injections on feeding behavior and expression of appetite regulators, uncoupling proteins and lipoprotein lipase, and fasting-induced changes in FNDC5 expression. Peptides 90, 27–36 (2017)
L. Sundarrajan, C. Yeung, L. Hahn, L.P. Weber, S. Unniappan, Irisin regulates cardiac physiology in zebrafish. PLoS ONE 12, e0181461 (2017)
M. Schlogl, P. Piaggi, S.B. Votruba, M. Walter, J. Krakoff, M.S. Thearle, Increased 24-hour ad libitum food intake is associated with lower plasma irisin concentrations the following morning in adult humans. Appetite 90, 154–159 (2015)
J.Y. Huh, F. Dincer, E. Mesfum, C.S. Mantzoros, Irisin stimulates muscle growth-related genes and regulates adipocyte differentiation and metabolism in humans. Int. J. Obes. 38, 1538–1544 (2014)
S. Raschke, M. Elsen, H. Gassenhuber, M. Sommerfeld, U. Schwahn, B. Brockmann, R. Jung, U. Wisloff, A.E. Tjonna, T. Raastad, J. Hallen, F. Norheim, C.A. Drevon, T. Romacho, K. Eckardt, J. Eckel, Evidence against a beneficial effect of irisin in humans. PLoS ONE 8, e73680 (2013)
C. Zhang, Z. Ding, G. Lv, J. Li, P. Zhou, J. Zhang, Lower irisin level in patients with type 2 diabetes mellitus: a case-control study and meta-analysis. J. Diabetes 8, 56–62 (2016)
P. Lee, J.D. Linderman, S. Smith, R.J. Brychta, J. Wang, C. Idelson, R.M. Perron, C.D. Werner, G.Q. Phan, U.S. Kammula, E. Kebebew, K. Pacak, K.Y. Chen, F.S. Celi, Irisin and FGF21 are cold-induced endocrine activators of brown fat function in humans. Cell Metab. 19, 302–309 (2014)
A.B. Crujeiras, M. Pardo, R.R. Arturo, S. Navas-Carretero, M.A. Zulet, J.A. Martinez, F.F. Casanueva, Longitudinal variation of circulating irisin after an energy restriction-induced weight loss and following weight regain in obese men and women. Am. J. Hum. Biol. 26, 198–207 (2014)
C. Gutierrez-Repiso, S. Garcia-Serrano, F. Rodriguez-Pacheco, E. Garcia-Escobar, J.J. Haro-Mora, J. Garcia-Arnes, S. Valdes, M. Gonzalo, F. Soriguer, F.J. Moreno-Ruiz, A. Rodriguez-Canete, A. Martinez-Ferriz, J.S. Santoyo, V. Perez-Valero, E. Garcia-Fuentes, FNDC5 could be regulated by leptin in adipose tissue. Eur. J. Clin. Invest. 44, 918–925 (2014)
A.E. Huerta, P.L. Prieto-Hontoria, M. Fernandez-Galilea, N. Sainz, M. Cuervo, J.A. Martinez, M.J. Moreno-Aliaga, Circulating irisin and glucose metabolism in overweight/obese women: effects of alpha-lipoic acid and eicosapentaenoic acid. J. Physiol. Biochem. 71, 547–558 (2015)
D. Loffler, U. Muller, K. Scheuermann, D. Friebe, J. Gesing, J. Bielitz, S. Erbs, K. Landgraf, I.V. Wagner, W. Kiess, A. Korner, Serum irisin levels are regulated by acute strenuous exercise. J. Clin. Endocrinol. Metab. 100, 1289–1299 (2015)
M. Pardo, A.B. Crujeiras, M. Amil, Z. Aguera, S. Jimenez-Murcia, R. Banos, C. Botella, R. de la Torre, X. Estivill, A.B. Fagundo, J.M. Fernandez-Real, J.C. Fernandez-Garcia, G. Fruhbeck, J. Gomez-Ambrosi, R. Rodriguez, F.J. Tinahones, F. Fernandez-Aranda, F.F. Casanueva, Association of irisin with fat mass, resting energy expenditure, and daily activity in conditions of extreme body mass index. Int. J. Endocrinol. 2014, 857270 (2014)
A. Stengel, T. Hofmann, M. Goebel-Stengel, U. Elbelt, P. Kobelt, B.F. Klapp, Circulating levels of irisin in patients with anorexia nervosa and different stages of obesity—correlation with body mass index. Peptides 39, 125–130 (2013)
A.B. Crujeiras, M.A. Zulet, P. Lopez-Legarrea, R. de la Iglesia, M. Pardo, M.C. Carreira, J.A. Martinez, F.F. Casanueva, Association between circulating irisin levels and the promotion of insulin resistance during the weight maintenance period after a dietary weight-lowering program in obese patients. Metabolism 63, 520–531 (2014)
J. Huang, S. Wang, F. Xu, D. Wang, H. Yin, Q. Lai, J. Liao, X. Hou, M. Hu, Exercise training with dietary restriction enhances circulating irisin level associated with increasing endothelial progenitor cell number in obese adults: an intervention study. PeerJ 5, e3669 (2017)
B. Palacios-Gonzalez, F. Vadillo-Ortega, E. Polo-Oteyza, T. Sanchez, M. Ancira-Moreno, S. Romero-Hidalgo, N. Meraz, B. Antuna-Puente, Irisin levels before and after physical activity among school-age children with different BMI: a direct relation with leptin. Obesity 23, 729–732 (2015)
E. Nigro, O. Scudiero, M. Ludovica Monaco, R. Polito, P. Schettino, A. Grandone, L. Perrone, E. Miraglia Del Giudice, A. Daniele, Adiponectin profile and Irisin expression in Italian obese children: association with insulin-resistance. Cytokine 94, 8–13 (2017)
A. Gavrieli, G. Panagiotou, C.S. Mantzoros, Leptin administration in physiological or pharmacological doses does not alter circulating irisin levels in humans. Int. J. Obes. 40, 1461–1463 (2016)
L. Mo, J. Shen, Q. Liu, Y. Zhang, J. Kuang, S. Pu, S. Cheng, M. Zou, W. Jiang, C. Jiang, A. Qu, J. He, Irisin is regulated by CAR in liver and is a mediator of hepatic glucose and lipid metabolism. Mol. Endocrinol. 30, 533–542 (2016)
T.Y. Liu, C.X. Shi, R. Gao, H.J. Sun, X.Q. Xiong, L. Ding, Q. Chen, Y.H. Li, J.J. Wang, Y.M. Kang, G.Q. Zhu, Irisin inhibits hepatic gluconeogenesis and increases glycogen synthesis via the PI3K/Akt pathway in type 2 diabetic mice and hepatocytes. Clin. Sci. 129, 839–850 (2015)
A. Natalicchio, N. Marrano, G. Biondi, R. Spagnuolo, R. Labarbuta, I. Porreca, A. Cignarelli, M. Bugliani, P. Marchetti, S. Perrini, L. Laviola, F. Giorgino, The myokine irisin is released in response to saturated fatty acids and promotes pancreatic beta-cell survival and insulin secretion. Diabetes 66, 2849–2856 (2017)
J.J. Liu, M.D. Wong, W.C. Toy, C.S. Tan, S. Liu, X.W. Ng, S. Tavintharan, C.F. Sum, S.C. Lim, Lower circulating irisin is associated with type 2 diabetes mellitus. J. Diabetes Complicat. 27, 365–369 (2013)
M. Yang, P. Chen, H. Jin, X. Xie, T. Gao, L. Yang, X. Yu, Circulating levels of irisin in middle-aged first-degree relatives of type 2 diabetes mellitus—correlation with pancreatic beta-cell function. Diabetol. Metab. Syndr. 6, 133 (2014)
S. Qiu, X. Cai, H. Yin, M. Zugel, Z. Sun, J.M. Steinacker, U. Schumann, Association between circulating irisin and insulin resistance in non-diabetic adults: a meta-analysis. Metabolism 65, 825–834 (2016)
N.M. Al-Daghri, K.M. Alkharfy, S. Rahman, O.E. Amer, B. Vinodson, S. Sabico, M.K. Piya, A.L. Harte, P.G. McTernan, M.S. Alokail, G.P. Chrousos, Irisin as a predictor of glucose metabolism in children: sexually dimorphic effects. Eur. J. Clin. Invest. 44, 119–124 (2014)
G. Sesti, F. Andreozzi, T.V. Fiorentino, G.C. Mannino, A. Sciacqua, M.A. Marini, F. Perticone, High circulating irisin levels are associated with insulin resistance and vascular atherosclerosis in a cohort of nondiabetic adult subjects. Acta. Diabetol. 51, 705–713 (2014)
J.H. Huh, S.V. Ahn, J.H. Choi, S.B. Koh, C.H. Chung, High serum irisin level as an independent predictor of diabetes mellitus: a longitudinal population-based study. Medicine 95, e3742 (2016)
I. Ates, M.F. Arikan, K. Erdogan, M. Kaplan, M. Yuksel, C. Topcuoglu, N. Yilmaz, S. Guler, Factors associated with increased irisin levels in the type 1 diabetes mellitus. Endocr. Regul. 51, 1–7 (2017)
D. Espes, J. Lau, P.O. Carlsson, Increased levels of irisin in people with long-standing type 1 diabetes. Diabet. Med. 32, 1172–1176 (2015)
Y. Assyov, A. Gateva, A. Tsakova, Z. Kamenov, Irisin in the glucose continuum. Exp. Clin. Endocrinol. Diabetes 124, 22–27 (2016)
A. Shoukry, S.M. Shalaby, S. El-Arabi Bdeer, A.A. Mahmoud, M.M. Mousa, A. Khalifa, Circulating serum irisin levels in obesity and type 2 diabetes mellitus. IUBMB Life 68, 544–556 (2016)
W. Hu, R. Wang, J. Li, J. Zhang, W. Wang, Association of irisin concentrations with the presence of diabetic nephropathy and retinopathy. Ann. Clin. Biochem. 53, 67–74 (2016)
E.G. Khidr, S.S. Ali, M.M. Elshafey, O.A. Fawzy, Association of irisin and FNDC5 rs16835198 G>T gene polymorphism with type 2 diabetes mellitus and diabetic nephropathy. An Egyptian pilot study. Gene 626, 26–31 (2017)
Z. Li, G. Wang, Y.J. Zhu, C.G. Li, Y.Z. Tang, Z.H. Jiang, M. Yang, C.L. Ni, L.M. Chen, W.Y. Niu, The relationship between circulating irisin levels and tissues AGE accumulation in type 2 diabetes patients. Biosci. Rep. 37, (2017)
X.L. Du, W.X. Jiang, Z.T. Lv, Lower circulating irisin level in patients with diabetes mellitus: a systematic review and meta-analysis. Horm. Metab. Res. 48, 644–652 (2016)
B. Garcia-Fontana, R. Reyes-Garcia, S. Morales-Santana, V. Avila-Rubio, A. Munoz-Garach, P. Rozas-Moreno, M. Munoz-Torres, Relationship between myostatin and irisin in type 2 diabetes mellitus: a compensatory mechanism to an unfavourable metabolic state? Endocrine 52, 54–62 (2016)
N.M. Al-Daghri, A.K. Mohammed, O.S. Al-Attas, O.E. Amer, M. Clerici, A. Alenad, M.S. Alokail, SNPs in FNDC5 (irisin) are associated with obesity and modulation of glucose and lipid metabolism in Saudi subjects. Lipids Health Dis. 15, 54 (2016)
A. Akour, V. Kasabri, N. Boulatova, Y. Bustanji, R. Naffa, D. Hyasat, N. Khawaja, H. Bustanji, A. Zayed, M. Momani, Levels of metabolic markers in drug-naive prediabetic and type 2 diabetic patients. Acta Diabetol. 54, 163–170 (2017)
I.D. Duran, N.E. Gulcelik, M. Unal, C. Topcuoglu, S. Sezer, M.M. Tuna, D. Berker, S. Guler, Irisin levels in the progression of diabetes in sedentary women. Clin. Biochem. 48, 1268–1272 (2015)
Y.K. Choi, M.K. Kim, K.H. Bae, H.A. Seo, J.Y. Jeong, W.K. Lee, J.G. Kim, I.K. Lee, K.G. Park, Serum irisin levels in new-onset type 2 diabetes. Diabetes Res Clin. Pract. 100, 96–101 (2013)
J.J. Liu, S. Liu, M.D. Wong, C.S. Tan, S. Tavintharan, C.F. Sum, S.C. Lim, Relationship between circulating irisin, renal function and body composition in type 2 diabetes. J. Diabetes Complicat. 28, 208–213 (2014)
C. Wang, L. Wang, J. Liu, J. Song, Y. Sun, P. Lin, K. Liang, F. Liu, T. He, Z. Sun, X. Hou, L. Chen, Irisin modulates the association of interleukin-17A with the presence of non-proliferative diabetic retinopathy in patients with type 2 diabetes. Endocrine 53, 459–464 (2016)
H.H. Wang, X.W. Zhang, W.K. Chen, Q.X. Huang, Q.Q. Chen, Relationship between serum irisin levels and urinary albumin excretion in patients with type 2 diabetes. J. Diabetes Complicat. 29, 384–389 (2015)
L. Xiang, G. Xiang, L. Yue, J. Zhang, L. Zhao, Circulating irisin levels are positively associated with endothelium-dependent vasodilation in newly diagnosed type 2 diabetic patients without clinical angiopathy. Atherosclerosis 235, 328–333 (2014)
M. Zhang, P. Chen, S. Chen, Q. Sun, Q.C. Zeng, J.Y. Chen, Y.X. Liu, X.H. Cao, M. Ren, J.K. Wang, The association of new inflammatory markers with type 2 diabetes mellitus and macrovascular complications: a preliminary study. Eur. Rev. Med Pharmacol. Sci. 18, 1567–1572 (2014)
S. Shelbaya, M.M. Abushady, M.S. Nasr, M.M. Bekhet, Y.A. Mageed, M. Abbas, Study of irisin hormone level in type 2 diabetic patients and patients with diabetic nephropathy. Curr. Diabetes Rev. (2017). https://doi.org/10.2174/1573399813666170829163442
D.J. Li, F. Huang, W.J. Lu, G.J. Jiang, Y.P. Deng, F.M. Shen, Metformin promotes irisin release from murine skeletal muscle independently of AMP-activated protein kinase activation. Acta Physiol. 213, 711–721 (2015)
H. Duan, B. Ma, X. Ma, H. Wang, Z. Ni, B. Wang, X. Li, P. Jiang, M. Umar, M. Li, Anti-diabetic activity of recombinant irisin in STZ-induced insulin-deficient diabetic mice. Int. J. Biol. Macromol. 84, 457–463 (2016)
C. Xin, J. Liu, J. Zhang, D. Zhu, H. Wang, L. Xiong, Y. Lee, J. Ye, K. Lian, C. Xu, L. Zhang, Q. Wang, Y. Liu, L. Tao, Irisin improves fatty acid oxidation and glucose utilization in type 2 diabetes by regulating the AMPK signaling pathway. Int. J. Obes. 40, 443–451 (2016)
Z. Yang, X. Chen, Y. Chen, Q. Zhao, Decreased irisin secretion contributes to muscle insulin resistance in high-fat diet mice. Int. J. Clin. Exp. Pathol. 8, 6490–6497 (2015)
D. Zhu, H. Wang, J. Zhang, X. Zhang, C. Xin, F. Zhang, Y. Lee, L. Zhang, K. Lian, W. Yan, X. Ma, Y. Liu, L. Tao, Irisin improves endothelial function in type 2 diabetes through reducing oxidative/nitrative stresses. J. Mol. Cell Cardiol. 87, 138–147 (2015)
S. Liu, F. Du, X. Li, M. Wang, R. Duan, J. Zhang, Y. Wu, Q. Zhang, Effects and underlying mechanisms of irisin on the proliferation and apoptosis of pancreatic beta cells. PLoS ONE 12, e0175498 (2017)
Y. Pang, H. Zhu, J. Xu, L. Yang, L. Liu, J. Li, Beta-arrestin-2 is involved in irisin induced glucose metabolism in type 2 diabetes via p38 MAPK signaling. Exp. Cell Res. 360, 199–204 (2017)
O. Erol, N. Erkal, H.Y. Ellidag, B.S. Isenlik, O. Aydin, A.U. Derbent, N. Yilmaz, Irisin as an early marker for predicting gestational diabetes mellitus: a prospective study. J. Matern. Fetal Neonatal Med. 29, 3590–3595 (2016)
T. Ebert, H. Stepan, S. Schrey, S. Kralisch, J. Hindricks, L. Hopf, M. Platz, U. Lossner, B. Jessnitzer, S. Drewlo, M. Bluher, M. Stumvoll, M. Fasshauer, Serum levels of irisin in gestational diabetes mellitus during pregnancy and after delivery. Cytokine 65, 153–158 (2014)
M.K. Piya, A.L. Harte, K. Sivakumar, G. Tripathi, P.D. Voyias, S. James, S. Sabico, N.M. Al-Daghri, P. Saravanan, T.M. Barber, S. Kumar, M. Vatish, P.G. McTernan, The identification of irisin in human cerebrospinal fluid: influence of adiposity, metabolic markers, and gestational diabetes. Am. J. Physiol. Endocrinol. Metab. 306, E512–E518 (2014)
M. Kuzmicki, B. Telejko, D. Lipinska, J. Pliszka, M. Szamatowicz, J. Wilk, M. Zbucka-Kretowska, P. Laudanski, A. Kretowski, M. Gorska, J. Szamatowicz, Serum irisin concentration in women with gestational diabetes. Gynecol. Endocrinol. 30, 636–639 (2014)
U.M. Ural, S.B. Sahin, Y.B. Tekin, M.C. Cure, H. Sezgin, Alteration of maternal serum irisin levels in gestational diabetes mellitus. Ginekol. Pol. 87, 395–398 (2016)
N. Wawrusiewicz-Kurylonek, B. Telejko, M. Kuzmicki, A. Sobota, D. Lipinska, J. Pliszka, B. Raczkowska, P. Kuc, R. Urban, J. Szamatowicz, A. Kretowski, P. Laudanski, M. Gorska, Increased maternal and cord blood betatrophin in gestational diabetes. PLoS ONE 10, e0131171 (2015)
M.A. Yuksel, M. Oncul, A. Tuten, M. Imamoglu, A.S. Acikgoz, M. Kucur, R. Madazli, Maternal serum and fetal cord blood irisin levels in gestational diabetes mellitus. Diabetes Res Clin. Pract. 104, 171–175 (2014)
L. Zhao, J. Li, Z.L. Li, J. Yang, M.L. Li, G.L. Wang, Circulating irisin is lower in gestational diabetes mellitus. Endocr. J. 62, 921–926 (2015)
B. Usluogullari, C.A. Usluogullari, F. Balkan, M. Orkmez, Role of serum levels of irisin and oxidative stress markers in pregnant women with and without gestational diabetes. Gynecol. Endocrinol. 33, 405–407 (2017)
M. Hernandez-Trejo, G. Garcia-Rivas, A. Torres-Quintanilla, E. Laresgoiti-Servitje, Relationship between irisin concentration and serum cytokines in mother and newborn. PLoS ONE 11, e0165229 (2016)
K.E. Joung, K.H. Park, A. Filippaios, F. Dincer, H. Christou, C.S. Mantzoros, Cord blood irisin levels are positively correlated with birth weight in newborn infants. Metabolism 64, 1507–1514 (2015)
S. Aydin, T. Kuloglu, S. Aydin, M.N. Eren, A. Celik, M. Yilmaz, M. Kalayci, I. Sahin, O. Gungor, A. Gurel, M. Ogeturk, O. Dabak, Cardiac, skeletal muscle and serum irisin responses to with or without water exercise in young and old male rats: cardiac muscle produces more irisin than skeletal muscle. Peptides 52, 68–73 (2014)
S. Aydin, T. Kuloglu, S. Aydin, M. Kalayci, M. Yilmaz, T. Cakmak, S. Albayrak, S. Gungor, N. Colakoglu, I.H. Ozercan, A comprehensive immunohistochemical examination of the distribution of the fat-burning protein irisin in biological tissues. Peptides 61, 130–136 (2014)
J. Lv, Y. Pan, X. Li, D. Cheng, H. Ju, J. Tian, H. Shi, Y. Zhang, Study on the distribution and elimination of the new hormone irisin in vivo: new discoveries regarding irisin. Horm. Metab. Res. 47, 591–595 (2015)
M.J. Park, D.I. Kim, J.H. Choi, Y.R. Heo, S.H. Park, New role of irisin in hepatocytes: the protective effect of hepatic steatosis in vitro. Cell Signal. 27, 1831–1839 (2015)
Y. Nie, D. Liu, N-glycosylation is required for FDNC5 stabilization and irisin secretion. Biochem. J. 474, 3167–3177 (2017)
W.Y. So, P.S. Leung, Irisin ameliorates hepatic glucose/lipid metabolism and enhances cell survival in insulin-resistant human HepG2 cells through adenosine monophosphate-activated protein kinase signaling. Int. J. Biochem. Cell Biol. 78, 237–247 (2016)
H. Tang, R. Yu, S. Liu, B. Huwatibieke, Z. Li, W. Zhang, Irisin inhibits hepatic cholesterol synthesis via AMPK-SREBP2 signaling. EBioMedicine 6, 139–148 (2016)
S.A. Polyzos, J. Kountouras, C.S. Mantzoros, Leptin in nonalcoholic fatty liver disease: a narrative review. Metabolism 64, 60–78 (2015)
S.A. Polyzos, J. Kountouras, C. Zavos, Nonalcoholic fatty liver disease: the pathogenetic roles of insulin resistance and adipocytokines. Curr. Mol. Med. 9, 299–314 (2009)
S. Batirel, P. Bozaykut, E. Mutlu Altundag, N. Kartal Ozer, C.S. Mantzoros, The effect of irisin on antioxidant system in liver. Free Radic. Biol. Med. 75(Suppl 1), S16 (2014)
S. Aydin, M. Ogeturk, T. Kuloglu, A. Kavakli, S. Aydin, Effect of carnosine supplementation on apoptosis and irisin, total oxidant and antioxidants levels in the serum, liver and lung tissues in rats exposed to formaldehyde inhalation. Peptides 64, 14–23 (2014)
G. Shi, N. Tang, J. Qiu, D. Zhang, F. Huang, Y. Cheng, K. Ding, W. Li, P. Zhang, X. Tan, Irisin stimulates cell proliferation and invasion by targeting the PI3K/AKT pathway in human hepatocellular carcinoma. Biochem. Biophys. Res. Commun. 493, 585–591 (2017)
S.A. Polyzos, J. Kountouras, A.D. Anastasilakis, E.V. Geladari, C.S. Mantzoros, Irisin in patients with nonalcoholic fatty liver disease. Metabolism 63, 207–217 (2014)
D. Kraus, Q. Yang, D. Kong, A.S. Banks, L. Zhang, J.T. Rodgers, E. Pirinen, T.C. Pulinilkunnil, F. Gong, Y.C. Wang, Y. Cen, A.A. Sauve, J.M. Asara, O.D. Peroni, B.P. Monia, S. Bhanot, L. Alhonen, P. Puigserver, B.B. Kahn, Nicotinamide N-methyltransferase knockdown protects against diet-induced obesity. Nature 508, 258–262 (2014)
S. Petta, L. Valenti, G. Svegliati-Baroni, M. Ruscica, R.M. Pipitone, P. Dongiovanni, C. Rychlicki, N. Ferri, C. Camma, A.L. Fracanzani, I. Pierantonelli, V. Di Marco, M. Meroni, D. Giordano, S. Grimaudo, M. Maggioni, D. Cabibi, S. Fargion, A. Craxi, Fibronectin type iii domain-containing protein 5 rs3480 A>G polymorphism, irisin, and liver fibrosis in patients with nonalcoholic fatty liver disease. J. Clin. Endocrinol. Metab. 102, 2660–2669 (2017)
M. Shanaki, N. Moradi, S. Emamgholipour, R. Fadaei, H. Poustchi, Lower circulating irisin is associated with nonalcoholic fatty liver disease and type 2 diabetes. Diabetes Metab. Syndr. (2017). https://doi.org/10.1016/j.dsx.2017.03.037
E.S. Choi, M.K. Kim, M.K. Song, J.M. Kim, E.S. Kim, W.J. Chung, K.S. Park, K.B. Cho, J.S. Hwang, B.K. Jang, Association between serum irisin levels and non-alcoholic fatty liver disease in health screen examinees. PLoS ONE 9, e110680 (2014)
H.J. Zhang, X.F. Zhang, Z.M. Ma, L.L. Pan, Z. Chen, H.W. Han, C.K. Han, X.J. Zhuang, Y. Lu, X.J. Li, S.Y. Yang, X.Y. Li, Irisin is inversely associated with intrahepatic triglyceride contents in obese adults. J. Hepatol. 59, 557–562 (2013)
A. Viitasalo, M. Atalay, J. Pihlajamaki, J. Jaaskelainen, A. Korkmaz, D. Kaminska, V. Lindi, T.A. Lakka, The 148M allele of the PNPLA3 gene is associated with plasma irisin levels in a population sample of Caucasian children: the PANIC study. Metabolism 64, 793–796 (2015)
G. Mintziori, S.A. Polyzos, Emerging and future therapies for nonalcoholic steatohepatitis in adults. Expert Opin. Pharmacother. 17, 1937–1946 (2016)
M. Moreno, J.M. Moreno-Navarrete, M. Serrano, F. Ortega, E. Delgado, C. Sanchez-Ragnarsson, S. Valdés, P. Botas, W. Ricart, J.M. Fernández-Real, Circulating irisin levels are positively associated with metabolic risk factors in sedentary subjects. PLoS ONE 10, e0124100 (2015)
K.H. Park, L. Zaichenko, M. Brinkoetter, B. Thakkar, A. Sahin-Efe, K.E. Joung, M.A. Tsoukas, E.V. Geladari, J.Y. Huh, F. Dincer, C.R. Davis, J.A. Crowell, C.S. Mantzoros, Circulating irisin in relation to insulin resistance and the metabolic syndrome. J. Clin. Endocrinol. Metab. 98, 4899–4907 (2013)
S. Tang, R. Zhang, F. Jiang, J. Wang, M. Chen, D. Peng, J. Yan, S. Wang, Y. Bao, C. Hu, W. Jia, Circulating irisin levels are associated with lipid and uric acid metabolism in a Chinese population. Clin. Exp. Pharmacol. Physiol. (2015). https://doi.org/10.1111/1440-1681.12439
H.B. Jang, H.J. Kim, J.H. Kang, S.I. Park, K.H. Park, H.J. Lee, Association of circulating irisin levels with metabolic and metabolite profiles of Korean adolescents. Metabolism 73, 100–108 (2017)
G. Panagiotou, L. Mu, B. Na, K.J. Mukamal, C.S. Mantzoros, Circulating irisin, omentin-1, and lipoprotein subparticles in adults at higher cardiovascular risk. Metabolism 63, 1265–1271 (2014)
S. Oelmann, M. Nauck, H. Völzke, M. Bahls, N. Friedrich, Circulating irisin concentrations are associated with a favourable lipid profile in the general population. PLoS ONE 11, e0154319 (2016)
A.D. Anastasilakis, S.A. Polyzos, Z.G. Saridakis, G. Kynigopoulos, E.C. Skouvaklidou, D. Molyvas, M.F. Vasiloglou, A. Apostolou, T. Karagiozoglou-Lampoudi, A. Siopi, V. Mougios, P. Chatzistavridis, G. Panagiotou, A. Filippaios, S. Delaroudis, C.S. Mantzoros, Circulating irisin in healthy, young individuals: day-night rhythm, effects of food intake and exercise, and associations with gender, physical activity, diet and body composition. J. Clin. Endocrinol. Metab. 99, 3247–3255 (2014)
S. Mehrabian, E. Taheri, M. Karkhaneh, M. Qorbani, S. Hosseini, Association of circulating irisin levels with normal weight obesity, glycemic and lipid profile. J. Diabetes Metab. Disord. 15, 17 (2016)
I. Gouni-Berthold, H.K. Berthold, J.Y. Huh, R. Berman, N. Spenrath, W. Krone, C.S. Mantzoros, Effects of lipid-lowering drugs on irisin in human subjects in vivo and in human skeletal muscle cells ex vivo. PLoS ONE 8, e72858 (2013)
A.D. Anastasilakis, D. Koulaxis, N. Kefala, S.A. Polyzos, J. Upadhyay, E. Pagkalidou, F. Economou, C.D. Anastasilakis, C.S. Mantzoros, Circulating irisin levels are lower in patients with either stable coronary artery disease (CAD) or myocardial infarction (MI) versus healthy controls, whereas follistatin and activin A levels are higher and can discriminate MI from CAD with similar to CK-MB accuracy. Metabolism 73, 1–8 (2017)
T. Kuloglu, S. Aydin, M.N. Eren, M. Yilmaz, I. Sahin, M. Kalayci, E. Sarman, N. Kaya, O.F. Yilmaz, A. Turk, Y. Aydin, M.H. Yalcin, N. Uras, A. Gurel, S. Ilhan, E. Gul, S. Aydin, Irisin: a potentially candidate marker for myocardial infarction. Peptides 55, 85–91 (2014)
S. Aydin, S. Aydin, M.A. Kobat, M. Kalayci, M.N. Eren, M. Yilmaz, T. Kuloglu, E. Gul, O. Secen, O.D. Alatas, A. Baydas, Decreased saliva/serum irisin concentrations in the acute myocardial infarction promising for being a new candidate biomarker for diagnosis of this pathology. Peptides 56, 141–145 (2014)
W. Deng, Association of serum irisin concentrations with presence and severity of coronary artery disease. Med. Sci. Monit. 22, 4193–4197 (2016)
N. Hou, F. Han, X. Sun, The relationship between circulating irisin levels and endothelial function in lean and obese subjects. Clin. Endocrinol. 83, 339–343 (2015)
C. Xie, Y. Zhang, T.D. Tran, H. Wang, S. Li, E.V. George, H. Zhuang, P. Zhang, A. Kandel, Y. Lai, D. Tang, W.H. Reeves, H. Cheng, Y. Ding, L.J. Yang, Irisin controls growth, intracellular Ca2+signals, and mitochondrial thermogenesis in cardiomyoblasts. PLoS ONE 10, e0136816 (2015)
H. Wang, Y.T. Zhao, S. Zhang, P.M. Dubielecka, J. Du, N. Yano, Y.E. Chin, S. Zhuang, G. Qin, T.C. Zhao, Irisin plays a pivotal role to protect the heart against ischemia and reperfusion injury. J. Cell Physiol. 232, 3775–3785 (2017)
Y. Zhang, H. Song, Y. Zhang, F. Wu, Q. Mu, M. Jiang, F. Wang, W. Zhang, L. Li, L. Shao, S. Li, L. Yang, M. Zhang, Q. Wu, D. Tang, Irisin inhibits atherosclerosis by promoting endothelial proliferation through microrna126-5p. J. Am. Heart Assoc. 5, e004031 (2016)
Y. Zhang, Q. Mu, Z. Zhou, H. Song, Y. Zhang, F. Wu, M. Jiang, F. Wang, W. Zhang, L. Li, L. Shao, X. Wang, S. Li, L. Yang, Q. Wu, M. Zhang, D. Tang, Protective effect of irisin on atherosclerosis via suppressing oxidized low density lipoprotein induced vascular inflammation and endothelial dysfunction. PLoS ONE 11, e0158038 (2016)
H. Song, J. Xu, N. Lv, Y. Zhang, F. Wu, H. Li, L. Shao, Q. Mu, F. Wang, D. Tang, X. Fang, Irisin reverses platelet derived growth factor-BB-induced vascular smooth muscle cells phenotype modulation through STAT3 signaling pathway. Biochem. Biophys. Res. Commun. 479, 139–145 (2016)
F. Han, S. Zhang, N. Hou, D. Wang, X. Sun, Irisin improves endothelial function in obese mice through the AMPK-eNOS pathway. Am. J. Physiol. Heart Circ. Physiol. 309, 1501–1508 (2015)
J. Lu, G. Xiang, M. Liu, W. Mei, L. Xiang, J. Dong, Irisin protects against endothelial injury and ameliorates atherosclerosis in apolipoprotein E-Null diabetic mice. Atherosclerosis 243, 438–448 (2015)
M. Jiang, F. Wan, F. Wang, W. Qi, Irisin relaxes mouse mesenteric arteries through endothelium-dependent and endothelium-independent mechanisms. Biochem. Biophys. Res. Commun. 468, 823–836 (2015)
X. Liu, H. Mujahid, B. Rong, Q.H. Lu, W. Zhang, P. Li, N. Li, E.S. Liang, Q. Wang, D.Q. Tang, N.L. Li, X.P. Ji, Y.G. Chen, Y.X. Zhao, M.X. Zhang, Irisin inhibits high glucose-induced endothelial-to-mesenchymal transition and exerts a dose-dependent bidirectional effect on diabetic cardiomyopathy. J. Cell Mol. Med. (2017). https://doi.org/10.1111/jcmm.13360
D.J. Li, Y.H. Li, H.B. Yuan, L.F. Qu, P. Wang, The novel exercise-induced hormone irisin protects against neuronal injury via activation of the Akt and ERK1/2 signaling pathways and contributes to the neuroprotection of physical exercise in cerebral ischemia. Metabolism 68, 31–42 (2017)
J. Peng, X. Deng, W. Huang, J.H. Yu, J.X. Wang, J.P. Wang, S.B. Yang, X. Liu, L. Wang, Y. Zhang, X.Y. Zhou, H. Yang, Y.Z. He, F.Y. Xu, Irisin protects against neuronal injury induced by oxygen-glucose deprivation in part depends on the inhibition of ROS-NLRP3 inflammatory signaling pathway. Mol. Immunol. 91, 185–194 (2017)
S.A. Polyzos, D.G. Goulis, J. Kountouras, G. Mintziori, P. Chatzis, E. Papadakis, I. Katsikis, D. Panidis, Non-alcoholic fatty liver disease in women with polycystic ovary syndrome: assessment of non-invasive indices predicting hepatic steatosis and fibrosis. Hormones 13, 519–531 (2014)
C.L. Chang, S.Y. Huang, Y.K. Soong, P.J. Cheng, C.J. Wang, I.T. Liang, Circulating irisin and glucose-dependent insulinotropic peptide are associated with the development of polycystic ovary syndrome. J. Clin. Endocrinol. Metab. 99, E2539–E2548 (2014)
M. Li, M. Yang, X. Zhou, X. Fang, W. Hu, W. Zhu, C. Wang, D. Liu, S. Li, H. Liu, G. Yang, L. Li, Elevated circulating levels of irisin and the effect of metformin treatment in women with polycystic ovary syndrome. J. Clin. Endocrinol. Metab. 100, 1485–1493 (2015)
M.S. Bostanci, N. Akdemir, B. Cinemre, A.S. Cevrioglu, S. Ozden, O. Unal, Serum irisin levels in patients with polycystic ovary syndrome. Eur. Rev. Med. Pharmacol. Sci. 19, 4462–4468 (2015)
A. Adamska, M. Karczewska-Kupczewska, A. Lebkowska, R. Milewski, M. Gorska, E. Otziomek, A. Nikolajuk, S. Wolczynski, I. Kowalska, Serum irisin and its regulation by hyperinsulinemia in women with polycystic ovary syndrome. Endocr. J. 63, 1107–1112 (2016)
K. Pukajlo, L. Laczmanski, K. Kolackov, J. Kuliczkowska-Plaksej, M. Bolanowski, A. Milewicz, J. Daroszewski, Irisin plasma concentration in PCOS and healthy subjects is related to body fat content and android fat distribution. Gynecol. Endocrinol. 31, 907–911 (2015)
S. Gao, Y. Cheng, L. Zhao, Y. Chen, Y. Liu, The relationships of irisin with bone mineral density and body composition in PCOS patients. Diabetes Metab. Res. Rev. 32, 421–428 (2016)
R. Abali, I. Temel Yuksel, M.A. Yuksel, B. Bulut, M. Imamoglu, V. Emirdar, F. Unal, S. Guzel, C. Celik, Implications of circulating irisin and Fabp4 levels in patients with polycystic ovary syndrome. J. Obstet. Gynaecol. 36, 897–901 (2016)
H. Li, X. Xu, X. Wang, X. Liao, L. Li, G. Yang, L. Gao, Free androgen index and Irisin in polycystic ovary syndrome. J. Endocrinol. Invest. 39, 549–556 (2016)
C. Wang, X.Y. Zhang, Y. Sun, X.G. Hou, L. Chen, Higher circulating irisin levels in patients with polycystic ovary syndrome:a meta-analysis. Gynecol. Endocrinol. (2017). https://doi.org/10.1080/09513590.2017.1393065
G. Colaianni, C. Cuscito, T. Mongelli, P. Pignataro, C. Buccoliero, P. Liu, P. Lu, L. Sartini, M. Di Comite, G. Mori, A. Di Benedetto, G. Brunetti, T. Yuen, L. Sun, J.E. Reseland, S. Colucci, M.I. New, M. Zaidi, S. Cinti, M. Grano, The myokine irisin increases cortical bone mass. Proc. Natl. Acad. Sci. USA 112, 12157–12162 (2015)
A.D.G. Baxter-Jones, S.A. Kontulainen, R.A. Faulkner, D.A. Bailey, A longitudinal study of the relationship of physical activity to bone mineral accrual from adolescence to young adulthood. Bone 43, 1101–1107 (2008)
L. Giangregorio, R. El-Kotob, Exercise, muscle, and the applied load-bone strength balance. Osteoporos. Int. 28, 21–33 (2017)
S. Epstein, A.M. Inzerillo, J. Caminis, M. Zaidi, Disorders associated with acute rapid and severe bone loss. J. Bone Mineral. Res. 18, 2083–2094 (2003)
J.H. Keyak, A.K. Koyama, A. LeBlanc, Y. Lu, T.F. Lang, Reduction in proximal femoral strength due to long-duration spaceflight. Bone 44, 449–453 (2009)
B. Oppl, G. Michitsch, B. Misof, S. Kudlacek, J. Donis, K. Klaushofer, J. Zwerina, E. Zwettler, Low bone mineral density and fragility fractures in permanent vegetative state patients. J. Bone Mineral. Res. 29, 1096–1100 (2014)
G. Colaianni, S. Cinti, S. Colucci, M. Grano, Irisin and musculoskeletal health. Ann. N. Y. Acad. Sci. 1402, 5–9 (2017)
G. Colaianni, C. Cuscito, T. Mongelli, A. Oranger, G. Mori, G. Brunetti, S. Colucci, S. Cinti, M. Grano, Irisin enhances osteoblast differentiation in vitro. Int. J. Endocrinol. 2014, 902186 (2014)
X. Qiao, Y. Nie, Y. Ma, Y. Chen, R. Cheng, W. Yin, Y. Hu, W. Xu, L. Xu, Irisin promotes osteoblast proliferation and differentiation via activating the MAP kinase signaling pathways. Sci. Rep. 6, 18732 (2016)
H. Kaji, Effects of myokines on bone. Bone Rep. 5, 826 (2016)
G. Colaianni, M. Grano, Role of Irisin on the bone-muscle functional unit. Bone Rep. 4, 765 (2015)
G. Colaianni, T. Mongelli, C. Cuscito, P. Pignataro, L. Lippo, G. Spiro, A. Notarnicola, I. Severi, G. Passeri, G. Mori, G. Brunetti, B. Moretti, U. Tarantino, S.C. Colucci, J.E. Reseland, R. Vettor, S. Cinti, M. Grano, Irisin prevents and restores bone loss and muscle atrophy in hind-limb suspended mice. Sci. Rep. 7, 2811 (2017)
T. Klangjareonchai, H. Nimitphong, S. Saetung, N. Bhirommuang, R. Samittarucksa, S. Chanprasertyothin, R. Sudatip, B. Ongphiphadhanakul, Circulating sclerostin and irisin are related and interact with gender to influence adiposity in adults with prediabetes. Int. J. Endocrinol. 2014, 261545 (2014)
V. Singhal, E.A. Lawson, K.E. Ackerman, P.K. Fazeli, H. Clarke, H. Lee, K. Eddy, D.A. Marengi, N.P. Derrico, M.L. Bouxsein, M. Misra, Irisin levels are lower in young amenorrheic athletes compared with eumenorrheic athletes and non-athletes and are associated with bone density and strength estimates. PLoS ONE 9, e100218 (2014)
A.D. Anastasilakis, S.A. Polyzos, P. Makras, A. Gkiomisi, I. Bisbinas, A. Katsarou, A. Filippaios, C.S. Mantzoros, Circulating irisin is associated with osteoporotic fractures in postmenopausal women with low bone mass but is not affected by either teriparatide or denosumab treatment for 3 months. Osteoporos. Int. 25, 1633–1642 (2014)
A. Palermo, R. Strollo, E. Maddaloni, D. Tuccinardi, L. D’Onofrio, S.I. Briganti, G. Defeudis, M.De Pascalis, M.C. Lazzaro, G. Colleluori, S. Manfrini, P. Pozzilli, N. Napoli, Irisin is associated with osteoporotic fractures independently of bone mineral density, body composition or daily physical activity. Clin. Endocrinol. 82, 615–619 (2015)
J. Yan, H.J. Liu, W.C. Guo, J. Yang, Low serum concentrations of Irisin are associated with increased risk of hip fracture in Chinese older women. Joint Bone Spine (2017). https://doi.org/10.1016/j.jbspin.2017.03.011
S.A. Polyzos, J. Kountouras, C.S. Mantzoros, Adipokines in nonalcoholic fatty liver disease. Metabolism 65, 1062–1079 (2016)
M.A. Schumacher, N. Chinnam, T. Ohashi, R.S. Shah, H.P. Erickson, The structure of irisin reveals a novel intersubunit beta-sheet fibronectin type III (FNIII) dimer: implications for receptor activation. J. Biol. Chem. 288, 33738–33744 (2013)
M. Gry, R. Rimini, S. Stromberg, A. Asplund, F. Ponten, M. Uhlen, P. Nilsson, Correlations between RNA and protein expression profiles in 23 human cell lines. BMC Genom. 10, 365 (2009)
T. Maier, M. Guell, L. Serrano, Correlation of mRNA and protein in complex biological samples. FEBS Lett. 583, 3966–3973 (2009)
M.P. Jedrychowski, C.D. Wrann, J.A. Paulo, K.K. Gerber, J. Szpyt, M.M. Robinson, K.S. Nair, S.P. Gygi, B.M. Spiegelman, Detection and quantitation of circulating human irisin by tandem mass spectrometry. Cell Metab. 22, 734–740 (2015)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Stergios A. Polyzos, Athanasios D. Anastasilakis, Zoe A. Efstathiadou, Polyzois Makras, and Nikolaos Perakakis contributed equally to this work.
Rights and permissions
About this article
Cite this article
Polyzos, S.A., Anastasilakis, A.D., Efstathiadou, Z.A. et al. Irisin in metabolic diseases. Endocrine 59, 260–274 (2018). https://doi.org/10.1007/s12020-017-1476-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-017-1476-1