Abstract
Introduction
Throat packs (TP) are used in upper airway surgery to avoid accumulation and aspiration of blood, foreign bodies, and fluids. But side effects such as sore throat and TP retention have been reported and challenge the standardized use of TP. The aim of this study is to compare benefits and side effects of TP versus no TP for upper airway procedures in intubation anesthesia.
Material and methods
One hundred forty-eight patients with surgical interventions at the upper airway under intubation anesthesia were included. Of those, n = 74 each were treated without (A, control) and with (B) TP. Study group B was subdivided whether TP was placed by the surgeon (B1; n = 37) or by the anesthesiologist (B2; n = 37). TP-related side effects such as sore throat, foreign body sensation, hoarseness, dyspnea, difficulty of swallowing, nausea, retching, nausea, aspiration, and pneumonia as well as the influence of TP design and the applicant (surgeon or anesthetist) were analyzed.
Results
A significantly increased rate of difficulty of swallowing (p = 0.045), intensity of sore throat (p = 0.04), and foreign body sensation (p = 0.024) was found in group B when compared to group A. There was no correlation between hoarseness, dyspnea, nausea, retching, and TP. No case of aspiration or pneumonia was seen but one TP was accidentally forgotten in the patient. B2 showed an increased frequency of difficulty swallowing, followed by A and B1. B1 led to the highest incidence of nausea followed by the A and B2.
Conclusion
The use of TP led to a high rate of side effects without showing the propagated advantages.
Clinical relevance
The use of TP must be considered critically and cannot generally be recommended without specific reasons, such as high aspiration risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Throat packs (TP) are used in oral and maxillofacial surgery, otorhinolaryngology, pediatric- and neurosurgery, and other surgical specialties for upper airway interventions under general intubation anesthesia [1, 2]. TP are applicated before surgery by either the surgeon or the anesthesiologist and are in the pharyngeal region (naso-, oro-, or hypopharynx) causing temporary occlusion. After the surgical procedure, they are immediately removed before withdrawal of the tracheal tube [1, 3]. TP usually consist of surgical compresses or swabs, and they can be fixed using a thread to prevent dislocation into the larynx, trachea, and esophagus. Thread fixation also enables easy TP removal after completion of surgery. The thread can additionally be attached to a surgical clamp or anything else comparable as a visible reminder [4]. Alternatively, TP fixation to the tracheal tube was postulated [5]. Ideally, TP have a radio-opaque structure in order to detect retained or dislocated TP radiologically [6].
One of the potential main advantages of TP is the prevention of accumulation of foreign bodies in the pharynx and/or larynx as well as aspiration into the stomach or the lungs [6, 7]. In detail, this includes liquids (such as saliva, blood, disinfection and irrigation fluids), surgical instruments and/or materials (such as drills, osteosynthesis plates, and screws), or other items such as bone or tooth fragments [8, 9]. Even if a cuffed tube is applicated by the anesthesiologist, TP are said to ensure an extra level of security against swallowing and aspiration that might cause severe pneumonia and other major complications. Further, TP may fix and seal the tracheal tube, for example in cases of tube leakage, in pediatrics where uncuffed tubes are frequently used, as well as in cases when tubes are used in prone position [2, 10]. Next, TP have been reported to prevent a contamination of the upper aerodigestive tract [11]. This might additionally prevent postoperative nausea and vomiting (PONV) [12]. On contrary, TP were associated with an increased discomfort and relevant postoperative side effects for the patient. One of the most relevant complications is the accidental forgetting of TP in the patient, for example caused by miscommunication between the surgeon and the anesthesiologist [13]. Further, a lack of standardized protocols for TP application and its removal might be responsible [14]. According to Knepil et al., organizational failures, errors of omission, routine violation, and rule-based errors can be the cause. Recommended solutions to this serious problem are organizational protocols, joint agreements to applicate TP, persons designated to applicate and remove TP, pharyngeal cleanings as well as recording TP removal in swab count, and training personnel to consider retained TP [15]. In brief, forgetting TP could cause significant airway obstruction and, in the worst case, death [2, 7, 16,17,18]. Another relevant side effect that could cause dangerous or life-threatening situations is TP aspiration and ingestion [2, 7, 15, 17, 19,20,21,22]. This could be possible especially in situations where uncuffed tubes or TP without thread fixation are used. Next, mechanical irritations and wounds caused by TP application and removal, sore throat, foreign body sensation, hoarseness, dyspnea, difficulty swallowing, nausea, gag reflex, and vomiting were reported [2, 11]. Especially the severity of sore throat feelings was significantly increased by TP application [23]. Next, tongue swellings and injury of the pharyngeal plexus after TP usage were descripted [18, 24, 25]. Other authors associated TP with the development of painful oral aphthous lesions and an increased frequency of severe pharyngitis [26, 27].
Overall, the data for or against the use of TP are controversial. Consequently, the application of TP is critically discussed [1, 27,28,29,30,31,32]. To summarize, with respect to different TP advantages and side effects, a conclusive evidence-based assessment concerning the use of TP for upper airway surgery under intubation anesthesia is not yet possible. Therefore, the aim of this randomized prospective clinical study was to analyze advantages and side effects of TP in upper airway surgery under intubation anesthesia. The null hypothesis was that there are no differences by means of complications and side effects when using TP in comparison to no TP.
Material and methods
Study population and design
This study was designed as a prospective randomized controlled clinical trial. In total, 148 patients were initially included during the period from November 2018 to May 2019 at the Department of Oral and Maxillofacial Surgery at the University Medical Center Mainz, Germany. Inclusion criteria were age > 18 years and an upper airway surgical intervention in case of a pathology of the oral cavity and/or the hypopharynx. Patients unable to give informed consent and patients in which a surgical tracheotomy was to be expected were excluded from study participation. The protocol of the study was approved by the local ethics committee (No. 2018–13556) of the Federal State Rhineland-Palate (Germany) and all individuals provided written informed consent for study participation. Clinical trial registration was performed (DRKS00027415). Two groups (n = 74 each) were randomly designed without (A, control) and with TP application (B, test). Group B was further randomly subdivided whether TP was placed by the surgeon (B1; n = 37; TP size 10 × 40 cm) or by the anesthesiologist (B2; n = 37; TP size 6 × 200 cm). Randomization was achieved using a free online random number generator (https://rechneronline.de/zufallszahlen/). Figure 1 is a flow chart of the randomized study population illustrating different groups and subgroups.
Flow chart of the randomized study population including the different groups and subgroups (TP, throat pack). One hundred forty-six patients were originally included to the study. Twelve patients were excluded by several reasons in the follow-up (8 patients due to missing answers in the preoperative questionnaire, 1 patient since surgery was switched to a local anesthesia, and 3 patients because of a surgical tracheotomy). One hundred thirty-six patients were included to the follow-up and 128 to the final data analysis, since 8 patients were excluded with postoperative side effects based on feeding tubes
For preoperative data evaluation, a non-dynamic questionnaire was created. Here, possible parameters were recorded which, after reviewing the literature [16], could influence the side effects of TP. A multi-step internal evaluation process was performed to test the suitability and practicability of the questionnaire that was filled out by the surgeon for each patient the day before surgery analyzing potential preoperative risk factors influencing the postoperative development and manifestation of TP side effects. In detail, data were collected about patients’ age, gender, smoking behavior, information about postoperative nausea and vomiting (PONV), ASA (American Society of Anesthesiologists) classification (I–IV), the planned kind of intubation (oral or nasal), whether a TP was placed or not, and the TP applicant (surgeon or anesthetist). From the surgical and anesthesiologic records, data on the exact TP position (nasopharynx, visible over or under the tongue base), the TP material (gauze bandage or surgical compress), TP materials’ state of application (dry or wet, e.g., hydrated in 0.9% saline solution), perioperative complications (e.g., TP left in the patient), difficult airway, aspiration, dislocation of TP to the esophagus or the stomach, PONV within 24 h, pneumonia within 48 h after surgery, and death were obtained.
On the first day after the operation, a second non-dynamic questionnaire was used to document postoperative TP-related side effects. The following information was recorded: sore throat, foreign body sensation, hoarseness, shortness of breath, difficulty swallowing, PONV, and gag reflex. The parameters sore throat, difficulty swallowing, and nausea were further evaluated by a visual analogue scale (VAS) ranging from 1 to 10. Further, it was documented if pneumonia and/or aspiration were detected and whether patients got a feeding tube.
Statistics
In a review concerning benefits of throat packs in upper airway surgery, Anderson et al. listed a total of 13 studies that were included in the review. Here, the number of analyzed patients ranged from 45 to 201 with a mean of 91.2 [8]. In accordance, a case numer of n > 100 was aimed at. Data was collected in Microsoft Excel (Microsoft Office, version 16.3; Microsoft Co., Redmond, WA, USA). SPPS software (IBA SPSS statistics version 25; IBM, Armonk, NY, USA) was used for statistical analysis using the chi-square test, Fisher’s exact test, Student’s T-test, and univariate ANOVA. Frequency values (normal scaled values for side effects) were presented by cross tables and analyzed by the chi-square test. Results were presented in tables and in bar charts including the mean (M) and the standard deviation (SD). Primary endpoints were the analysis on qualitative differences concerning sore throat, difficulty swallowing, and nausea with respect to a possible influence of the TP design and the TP applicator on them.
Results
Descriptive data
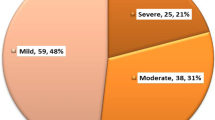
In total, 148 patients who planned for upper airway surgical procedures were initially included to the study. Eight patients were excluded due to missing answers in the preoperative questionnaire. One patient was excluded since the surgical procedure was switched from the originally planned general intubation anesthesia to a local anesthesia and 3 patients were excluded because of an intraoperative decision for a surgical tracheotomy. Therefore, 136 patients were included to the follow-up after surgery. In 8 of 13 patients with feeding tubes, postoperative side effects were based on feeding tubes that disappeared after the postoperative removal of the tubes. These patients were excluded from further data analysis. In total, 128 patients were included to the final data analysis (Fig. 1). Table 1 summarizes the descriptive data from the preoperative data evaluation (n = 136) at the follow-up including 8 patients with feeding tube side effects.
Incidence of side effects
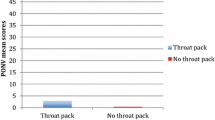
Concerning difficulty of swallowing, significant differences were analyzed in 29 patients with and in 20 patients without TP (p = 0.045). The intensity of difficulty of swallowing, analyzed by VAS, was around 0.43 VAS-units (95% confidence interval (CI) [− 0.67, 1.51]) higher in the TP group (mean (M) = 3.9, standard deviation (SD) = 1.9) compared to the group without TP (M = 3.5, SD = 1.8) without any significance (p = 0.439) (Fig. 2). Sore throat was found in 14 patients with and in 14 patients without TP. The intensity of sore throat was further analyzed by VAS (Fig. 3) and was around 0.89 VAS-units (95% CI [− 0.81, 2.6]) significantly higher in the group with TP (M = 4.3, SD = 2.4) compared to the group without TP (M = 3.4, SD = 2.0; p = 0.04). Nausea was detectable in 9 of the patients with and in 5 of the patients without TP (p > 0.05). The intensity of nausea was decreased in the group without TP (M = 6.6, SD = 3.5) by around 0.16 VAS-units (95% CI [− 3.89, 3.58]) compared to the group with TP (M = 6.4, SD = 2.8; p > 0.05) (Fig. 4). Next, foreign body sensation was found in 13 of the patients with and in 5 of the patients without TP (p = 0.024). Concerning hoarseness, 14 patients with and 11 patients without TP developed this side effect postoperatively (p > 0.05). Shortness of breath was analyzed in 4 of the patients with and in 2 of the patients without TP (p > 0.05). Retching related to 4 patients with and 3 patients without TP and vomiting to 5 patients with and 2 patients without TP (each p > 0.05). No case of pneumonia and/or aspiration was detected in all patients but in one case, a TP was accidentally forgotten and removed afterwards.
Side effects dependent from the applicant
Difficulty of swallowing was largest in group B2 with an increased intensity (M = 4.6, SD = 2) compared to groups A (M = 3.5, SD = 1.8) and B1 (M = 3.2, SD = 1.7). Between B2 and B1, this difference was significant (p = 0.032; Fig. 5). The intensity of sore throat demonstrated the highest values in group B2 (M = 4.9, SD = 2.2), followed by B1 (M = 3.4, SD = 2.7) and A (M = 3.4, SD = 2). Once again, the difference between B2 and B1 but also between B2 and A was significant (p = 0.021 and p = 0.034; Fig. 6). Nausea was highest in group B1 with an increased intensity (M = 7.3, SD = 3.1) compared to groups A (M = 6.6, SD = 3.5) and B2 (M = 5.8, SD = 2.8) but without significant differences (Fig. 7).
TP side effects depending on different variables
Gender-dependent differences were seen concerning the frequency of sore throat, shortness of breath, difficulty of swallowing, and nausea, in woman more than in men, respectively. There was a higher incidence of hoarseness when TP was applicated visible over the tongue ground. No correlation was found concerning TP side effects for smokers and patients with PONV in patients’ history as well as in dependence of the TP status (dry or wet).
Discussion
The use of TP including its benefits and potential side effects and risks is discussed critically in all surgical specialties dealing with upper airway surgery. While some authors prefer TP use due to the already listed advantages such as aspiration protection, others refuse TP application [16, 33]. In this context, Anderson et al. performed a systematic review concerning TP use and found no evidence for supporting TP use. The authors concluded that there is no indication for a routinely TP application in dental- and oral and maxillofacial surgery as well as otorhinolaryngology [8]. Contrary, further systematic reviews and clinical trials demonstrated that postoperative sore throat is seen after intubation anesthesia in nearly 60% of the cases [34, 35]. The influence of TP on postoperative sore throat was confirmed in numerous other studies [1, 11, 16, 36,37,38,39]. Even the influence of TP on postoperative nausea was part of some reviews [1, 3, 11, 12, 16, 23, 31, 37, 39,40,41]. The theory that TP can reduce the frequency of PONV could not be confirmed up to date. Contrary, a clear trend that TP increases these side effects was found [1, 3, 11, 12, 16, 23, 31, 37, 39,40,41]. There were different results between the nasopharyngeal and hypopharyngeal TP positioning [3, 41]. In this context, there is some evidence that TP is not a sufficient barrier against blood aspiration [42]. Contrary, some authors strongly recommended the use of TP since it can reduce the risk of blood aspiration [43, 44]. A study by Curran et al. analyzed TP use in cleft surgery in the UK and Ireland and found that about 75% of the participating surgeons currently used TP [45]. This high number might give evidence that TP benefits, such as aspiration protection, might predominate possible TP side effects and risks, such as TP retention. Overall, there is more literature that is not recommending a general TP use compared to literature recommending this procedure. An evidence-based decision concerning TP use might be difficult since the current data situation is inhomogeneous.
The findings of this study demonstrated that sore throat, difficulty of swallowing, and foreign body sensations were the most frequent TP side effects. Especially in oral and maxillofacial surgery (OMFS), these side effects might cause further relevant complications that are uncommon in other surgical specialties. In OMFS traumatology and orthognathic surgery, intermaxillary fixation (IMF) with wires or elastics is frequently used [46]. Even if these patients are treated with a PONV drug treatment, there is still an increased risk for IMF-caused PONV that might be additionally supported by postoperative TP side effects such as sore throat, foreign body sensation, and difficulty swallowing. PONV in IMF patients is very critical since these patients are prone to vomit and even suffocate in cases where IMF cannot be opened quickly enough [47]. Especially in these cases, supportive treatment options, e.g., for postoperative sore throat, are discussed. The automatization of bFGF (beta fibroblast growth factor) and dexamethasone and ketamine gargle were recommended as potential sore throat preventions [48,49,50]. Another study investigated lidocaine lubrication of tubes to prevent sore throat but there was no significant benefit [51]. Using locally applied non-steroidal antiphlogistics, sore throat could be significantly reduced [40, 52]. A reduction of TP-associated sore throat demonstrated significant differences after the use of 0.2% tenoxicam and CHX (chlorhexidine) and benzydamine solution [40, 52]. Next, the use of dezocine was reported [53].
Concerning the causes of sore throat after TP usage, exclusively the used TP material was investigated [38, 54]. In this context, the findings of the current study demonstrated that different TP materials and designs have an influence on TP-related side effects. A possible reason for the increased frequency of TP side effects in the present study might be the longer dimension of the TP used by the anesthesiologists. This structure might enable a deeper insertion into the pharyngeal region that might cause more side effects. Therefore, if TP is necessary, shorter and broader compresses should be favored like used by the surgeons in this study. Next, applicators (surgeons or anesthesiologists) showed an influence on TP-related side effects that were more frequently seen for anesthesiologists. The reasons are unclear, but it might be possible that TP is deeper and more strongly applicated by anesthesiologists into the pharyngeal region when compared to surgeons. According to a meta-analysis, no benefits were found for the patient using a TP applicated by the anesthesiologists [16].
With a special respect to TP use in OMFS, the influence of TP in orthognathic surgery was investigated concerning the prevention of postoperative sore throat, PONV, and dysphagia. While significant differences without TP were found for sore throat and dysphagia, no discrepancies were found regarding PONV [55]. Another systematic review even concluded that there is no evidence for TP benefits and its routine use in OMFS and otorhinolaryngology [8]. A prospective randomized controlled trial analyzed the influence of pharyngeal TP on sore throat and postoperative PONV after oral surgery. Here, TP were placed in one group via video guidance system, unguided in another group, and no TP was used in a control group. Concerning the control and the two experimental groups, significant differences were seen, especially in terms of higher postoperative throat pain in the TP groups [39]. In palatine cleft surgery, in the UK, 75% of the hospitals are using TP and the risk of remaining TP was overall estimated low. The authors concluded that the inclusion of TP into the surgical swab count is a safe procedure to prevent TP remaining [56]. Another study analyzed TP use and early postoperative complications in palatine cleft surgery in children. The results of this study showed that TP in cleft surgery is not associated with an increased postoperative complication rate. Nevertheless, there was a longer hospitalization time in the group with TP [36]. Finally, there is still not sufficient evidence of TP use in OMFS. In contrary, even if the present study was undertaken in a controlled setting, one TP was accidentally forgotten and might have resulted in severe complications.
Even cuffed tubes, as frequently used in OMFS, might be associated with side effects such as postoperative stridor that has not been finally clarified [57, 58]. It might be of interest whether side effects such as sore throat are increased by using uncuffed tubes and a TP or even by exclusively using cuffed tubes without TP since these side effects were exclusively analyzed in cuffed tubes up to date [59]. Though, as there is a high risk of aspiration in OMFS, cuffed tubes might prevent this complication without a need for TP. Postoperatively, the hypopharynx can be sufficiently viewed to remove remaining liquids and/or solids. In this context, Fields and Schow recommended the development of patient identification algorithms to detect predisposing factors and situations, an individualized patient positioning, pharyngeal screening, and the correct choice of surgical instruments to prevent remaining liquids and solids [60].
As a possible limitation, no power analysis has been performed in this study to detect even rare but dangerous and potentially lethal side effects, such as a missed or forgotten TP in the patient. Within the present study, in one out of 74 patients, a TP was missed, which indicated this to be a rare but potentially lethal complication.
Furthermore, since no routine chest X-ray was performed in this study—due to the lack of ethical justifiability of this procedure—it is possible that we overlooked potential side effects of missing TP application in terms of pneumonia, and thus the value of TP is underestimated. On the other hand, the postoperative clinical examinations (despite the fact that these routine assessments in our hospital were not included in the study) did not show any suspicion of an increased pneumonia rate in any of the groups.
With respect to the study design, it might have been possible to exclusively perform and analyze one single standardized intervention, such as wisdom teeth extraction. This might be suitable to reduce possible confounding factors, such as variation in operation time, different position of the tube, or a need for feeding tubes. Contrary, focusing on one single standardized intervention might even cause an observation error. Furthermore, the confounding influence of feeding tubes must be critically discussed. In this study, patients (with feeding tubes) were excluded from data analysis where side effects were directly associated to the feeding tubes.
In conclusion, the scientific literature contains numerous propagated advantages and disadvantages of TP, which is why this clinical study critically addressed this issue. The aim was to investigate the side effects of TP application compared to the propagated advantages and to weigh them up against each other in relation to the scientific literature. Considering the lack of side effects of surgery without TP and considering the high frequency of side effects when using it, it can be concluded from this study that the number of patients in whom TP would have to be applied to avoid an event (aspiration, pneumonia, etc.) is so high that the occurring side effects cannot be justified. The current study identified sore throat, difficulty of swallowing, and foreign body feeling to be the most frequent TP-related side effects. The use of TP must be considered critically and cannot be recommended generally in OMFS. The use of TP therefore should be restricted to certain indications, such as a high risk of aspiration.
References
Jin HJ, Kim S, Hwang SH (2019) Can pharyngeal packing prevent postoperative nausea and vomiting in nasal surgery? Laryngoscope 129(2):291–298. https://doi.org/10.1002/lary.27189
Smith J, Reddy E (2017) Aspiration of Nasopore nasal packing. Case Reports BMJ Case Rep 2017:bcr2017221969. https://doi.org/10.1136/bcr-2017-221969
Alfiky MG, Margalani OA, Rajeh AF, Alghamdi FE, Abu Suliman OA, Muathen SH, Elmorsy SA (2018) Nasopharyngeal versus hypopharyngeal packing during sino-nasal surgeries: randomised controlled trial. Randomized Controlled Trial Clin Otolaryngol 43(5):1235–1241. https://doi.org/10.1111/coa.13132
Stone JP, Collyer J (2003) Aide-memoir to pharyngeal pack removal. Anesth Analg 96(1):304. https://doi.org/10.1097/00000539-200301000-00067
Scheck PA (1981) A pharyngeal pack fixed on to the tracheal tube. Anaesthesia 36(9):892–895. https://doi.org/10.1111/j.1365-2044.1981.tb08865.x
Cousin G, Markose G (2020) The incidental finding of a retained ‘throat pack.’ Ann R Coll Surg Engl 102(6):e125. https://doi.org/10.1308/rcsann.2020.0047
Basha MS (2018) Missing pharyngeal pack endoscopically retrieved: an avoidable complication. Ann Maxillofac Surg 8(2):342–343. https://doi.org/10.4103/ams.ams_188_18
Anderson CR, Premakumar Y, Navaratnam AV, Rouhani M, Singh A (2020) The use of throat packs in ear, nose and throat, oral and dental surgery: a systematic review. Rhinology 58(4):306–313. https://doi.org/10.4193/Rhin19.308
Norman B (2018) An indication for a throat pack? Anaesthesia 73(8):1037. https://doi.org/10.1111/anae.14372
Bradford KE, Siegelman LI, Psoter WJ (2018) The effects of mouth opening and throat pack placement on uncuffed nasal endotracheal tube leakage and delivered tidal volumes in mechanically ventilated pediatric patients undergoing dental procedures. Anesth Prog 65(4):237–243. https://doi.org/10.2344/anpr-65-03-13
Jaiswal V, Bedford GC (2009) Review of the use of throat packs in nasal surgery. J Laryngol Otol 123(7):701–704. https://doi.org/10.1017/s0022215109004356
Korkut AY, Erkalp K, Erden V, Teker AM, Demirel A, Gedikli O, Saidoglu L (2010) Effect of pharyngeal packing during nasal surgery on postoperative nausea and vomiting. Randomized Controlled Trial Otolaryngol Head Neck Surg 143(6):831–836. https://doi.org/10.1016/j.otohns.2010.08.030
Baranger V, Bon Mardion N, Dureuil B, Compere V (2016) Human error in throat pack management: report of two cases. A A Case Rep 6(12):397–398. https://doi.org/10.1213/XAA.0000000000000348
Gupta A, Sarma R, Gupta N, Kumar R (2021) Current practices and beliefs regarding the use of oropharyngeal throat pack in India: a nationwide survey. Indian J Anaesth 65(3):241–247. https://doi.org/10.4103/ija.IJA_1376_20
Knepil GJ, Blackburn CW (2008) Retained throat packs: results of a national survey and the application of an organisational accident model. Br J Oral Maxillofac Surg 46(6):473–476. https://doi.org/10.1016/j.bjoms.2008.02.005
Athanassoglou V, Patel A, McGuire B, Higgs A, Dover MS, Brennan PA, Banerjee A, Bingham B, Pandit JJ (2018) Systematic review of benefits or harms of routine anaesthetist-inserted throat packs in adults: practice recommendations for inserting and counting throat packs: an evidence-based consensus statement by the Difficult Airway Society (DAS), the British Association of Oral and Maxillofacial Surgery (BAOMS) and the British Association of Otorhinolaryngology, Head and Neck Surgery (ENT-UK). Anaesthesia 73(5):612–618. https://doi.org/10.1111/anae.14197
Crawford BS (1977) Prevention of retained throat pack. BMJ 2(6093):1029. https://doi.org/10.1136/bmj.2.6093.1029
Abell D, Saju S, Wadhwani RN (2013) Throat pack and associated complications: not just about retention of packs after procedure. Br J Oral Maxillofac Surg 51(2):180–181. https://doi.org/10.1016/j.bjoms.2012.10.008
Gue S (2004) Images of interest. Gastrointestinal: ingested throat pack. J Gastroenterol Hepatol 19(12):1418. https://doi.org/10.1111/j.1440-1746.2004.03731.x
To EW, Tsang WM, Yiu F, Chan M (2001) A missing throat pack. Anaesthesia 56(4):383–384. https://doi.org/10.1046/j.1365-2044.2001.01976-19.x
Walton SL (1997) Postextubation foreign body aspiration: a case report. AANA J 65(2):147–149
Najjar MF, Kimpson J (1995) A method for preventing throat pack retention. Anesth Analg 80(1):208–209. https://doi.org/10.1097/00000539-199501000-00041
Karbasforushan A, Hemmatpoor B, Makhsosi BR, Mahvar T, Golfam P, Khiabani B (2014) The effect of pharyngeal packing during nasal surgery on the incidence of post operative nausea, vomiting, and sore throat. Iran J Otorhinolaryngol 26(77):219–223
Mermer RW, Zwillenberg D, Maron A, Brill CB (1990) Unilateral pharyngeal plexus injury following use of an oropharyngeal pack during third-molar surgery. J Oral Maxillofac Surg 48(10):1102–1104. https://doi.org/10.1016/0278-2391(90)90297-f
Sharma PK, Bhakta P, Srinivasan S, Khan RM, Kaul N (2012) Acute tongue enlargement secondary to pharyngeal packing after tracheal intubation–a case report. Middle East J Anaesthesiol 21(5):761–764
Fine J, Kaltman S, Bianco M (1988) Prevention of sore throat after nasotracheal intubation. J Oral Maxillofac Surg 46(11):946–947. https://doi.org/10.1016/0278-2391(88)90331-x
Erkalp K, Korkut YA, Meric A, Kahya V, Gedikli O, Su OK, Saitoglu L (2010) Pharyngeal packing is a predisposing factor for postoperative aphthous stomatitis in nasal surgery. Otolaryngol Head Neck Surg 142(5):672–676. https://doi.org/10.1016/j.otohns.2009.12.040
Bailey CR, Nouraie R, Huitink JM (2018) Have we reached the end for throat packs inserted by anaesthetists? Anaesthesia 73:535–548. https://doi.org/10.1111/anae.14168
Green R, Konuthula N, Sobrero M, Saini A, Parasher A, Pool C, Levine AI, DeMaria S, Tufts R, Govindaraj S, Iloreta AM (2017) Use of pharyngeal packs in functional endoscopic sinus surgery: a randomized controlled trial. Laryngoscope 127(11):2460–2465. https://doi.org/10.1002/lary.26651
Basha SI, McCoy E, Ullah R, Kinsella JB (2006) The efficacy of pharyngeal packing during routine nasal surgery–a prospective randomised controlled study. Anaesthesia 61(12):1161–1165. https://doi.org/10.1111/j.1365-2044.2006.04868.x
Arta S-A, Ghavimi M-A, Rahbar M, Ali-Maddadi Y, Zarandi A (2019) Effect of pharyngeal pack on postoperative nausea and throat pain in patients undergoing rhinoplasty. Pesquisa Brasileira em Odontopediatria e Clínica Integrada 19(1):1–8. https://doi.org/10.4034/pboci.2019.191.56
Chogyoji Y, Watanabe S (2020) Impact of subglottic saline irrigation on reducing bacterial contamination for oral surgery patients. Anesth Prog 67(2):79–85. https://doi.org/10.2344/anpr-66-04-07
Sexton J, Dohlman L (1989) Benefits of the pharyngeal pack. J Oral Maxillofac Surg 47(8):891. https://doi.org/10.1016/s0278-2391(89)80056-4
El-Boghdadly K, Bailey CR, Wiles MD (2016) Postoperative sore throat: a systematic review. Anaesthesia 71(6):706–717. https://doi.org/10.1111/anae.13438
Lipp M, Brandt L, Daublander M, Peter R, Barz L (1988) Frequency and severity of throat complaints following general anesthesia with the insertion of various endotracheal tubes. Anaesthesist 37(12):758–766
Smarius BJA, Guillaume C, Jonker G, van der Molen ABM, Breugem CC (2018) The use of throat packs in pediatric cleft lip/palate surgery: a retrospective study. Clin Oral Investig 22(9):3053–3059. https://doi.org/10.1007/s00784-018-2387-0
Razavi M, Taghavi Gilani M, Bameshki AR, Behdani R, Khadivi E, Bakhshaee M (2015) Pharyngeal packing during rhinoplasty: advantages and disadvantages. Iran J Otorhinolaryngol 27(83):423–428
Griffiths DP, Lindop MJ, Samuels SI, Roberts GD (1973) Pharyngeal packs and the incidence of post-operative sore throat. Anaesthesia 28(3):320–324. https://doi.org/10.1111/j.1365-2044.1973.tb00456.x
Al-Jandan BA, Syed FA, Zeidan A, Marei HF, Farooq I (2018) Pharyngeal pack placement in minor oral surgery: a prospective, randomized, controlled study. Ear Nose Throat J 97(3):E18-e21. https://doi.org/10.1177/014556131809700303
Vural C, Yurttutan ME, Sancak KT, Tuzuner AM (2019) Effect of chlorhexidine/benzydamine soaked pharyngeal packing on throat pain and postoperative nausea & vomiting in orthognathic surgery. J Craniomaxillofac Surg 47(12):1861–1867. https://doi.org/10.1016/j.jcms.2019.11.014
Rizvi MM, Singh RB, Rasheed MA, Sarkar A (2015) Effects of different types of pharyngeal packing in patients undergoing nasal surgery: a comparative study. Anesth Essays Res 9(2):230–237. https://doi.org/10.4103/0259-1162.156347
Powell K, Amin D, Sesanto R, Bryant A, Kukreja P, Waite P (2022) Do oropharyngeal throat packs prevent fluid ingestion during orthognathic surgery? Int J Oral Maxillofac Surg 51(3):366–370. https://doi.org/10.1016/j.ijom.2021.07.011
Bajwa SJ (2012) Prevention of aspiration of blood with a unique pharyngeal packing method. Anesth Essays Res 6(2):251–252. https://doi.org/10.4103/0259-1162.108361
Khan RM, Kaul N, Sharma PK, Haris A, Nair S (2018) Throat packs inserted by anaesthetists. Anaesthesia 73(9):1174. https://doi.org/10.1111/anae.14405
Curran TA, Narayan N, Fenner L, Thornburn G, Swan MC, Fallico N (2022) The throat pack debate: a review of current practice in UK and Ireland cleft centers. Cleft Palate Craniofac J 59(2):185–191. https://doi.org/10.1177/10556656211000553
Khiabani K, Zinhaghayegh B, Amirzade-Iranaq MH (2021) Does dynamic intermaxillary fixation with elastics improve outcomes following unilateral condylar fracture? J Oral Maxillofac Surg 79(1):192–199. https://doi.org/10.1016/j.joms.2020.08.040
Frost CM, Frost DE (1983) Nursing care of patients in intermaxillary fixation. Heart Lung 12(5):524–528
Liu B, Jiang YH, Xiao J, Li XK (2016) Efficacy of bFGF atomization inhalation on postoperative sore throat following oral and maxillofacial surgery under general anesthesia. Shanghai Kou Qiang Yi Xue 25(4):497–499
Thomas S, Beevi S (2007) Dexamethasone reduces the severity of postoperative sore throat. Can J Anaesth 54(11):897–901. https://doi.org/10.1007/BF03026793
Mayhood J, Cress K (2015) Effectiveness of ketamine gargle in reducing postoperative sore throat in patients undergoing airway instrumentation: a systematic review. JBI Database System Rev Implement Rep 13(9):244–278. https://doi.org/10.11124/jbisrir-2015-2045
Kori K, Muratani T, Tatsumi S, Minami T (2009) Influence of endotracheal tube cuff lubrication on postoperative sore throat and hoarseness. Masui 58(3):342–345
Elhakim M, Siam A, Rashed I, Hamdy MH (2000) Topical tenoxicam from pharyngeal pack reduces postoperative sore throat. Acta Anaesthesiol Scand 44(6):733–736. https://doi.org/10.1034/j.1399-6576.2000.440612.x
Jiao L, Liu RC (2014) Effects of dezocine on postoperative sore throat after maxillofacial procedures: a comparison with flurbiprofen axetil. Beijing Da Xue Xue Bao Yi Xue Ban 46(1):104–106
Marais J, Prescott RJ (1993) Throat pain and pharyngeal packing: a controlled randomized double-blind comparison between gauze and tampons. Clin Otolaryngol Allied Sci 18(5):426–429. https://doi.org/10.1111/j.1365-2273.1993.tb00607.x
Faro TF, de Oliveira ESED, Campos GJ, Duarte NM, Caetano AMM, Laureano Filho JR (2021) Effects of throat packs during orthognathic surgery: a double-blind randomized controlled clinical trial. Int J Oral Maxillofac Surg 50(3):349–355. https://doi.org/10.1016/j.ijom.2020.05.020
Curran TA, Narayan N, Fenner L, Thornburn G, Swan MC, Fallico N (2021) The throat pack debate: a review of current practice in UK and Ireland cleft centers. Cleft Palate Craniofac J: 10556656211000553. https://doi.org/10.1177/10556656211000553
De Orange FA, Andrade RG, Lemos A, Borges PS, Figueiroa JN, Kovatsis PG (2017) Cuffed versus uncuffed endotracheal tubes for general anaesthesia in children aged eight years and under. Cochrane Database Syst Rev 11:CD011954. https://doi.org/10.1002/14651858.CD011954.pub2
Shi F, Xiao Y, Xiong W, Zhou Q, Huang X (2016) Cuffed versus uncuffed endotracheal tubes in children: a meta-analysis. J Anesth 30(1):3–11. https://doi.org/10.1007/s00540-015-2062-4
Stenqvist O, Nilsson K (1982) Postoperative sore throat related to tracheal tube cuff design. Can Anaesth Soc J 29(4):384–386. https://doi.org/10.1007/BF03007531
Fields RT Jr, Schow SR (1998) Aspiration and ingestion of foreign bodies in oral and maxillofacial surgery: a review of the literature and report of five cases. J Oral Maxillofac Surg 56(9):1091–1098. https://doi.org/10.1016/s0278-2391(98)90263-4
Acknowledgements
This study contains parts, data, and results of the dental doctoral thesis (Dr. med. dent.) of Dr. med. Daniel Müller, Department of Oral and Maxillofacial Surgery, University Medical Center Mainz, Germany.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The study was conducted according to the principles of the Declaration of Helsinki. The study was approved by the local ethics committee (No. 2018–13556) of the Federal State Rhineland-Palate (Germany) and all individuals provided written informed consent for study participation.
Participation to the study was on a voluntary basis and data collection was conducted anonymously. This article does not contain any studies on animals performed by any of the authors.
Informed consent
All individuals provided written informed consent for study participation.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pabst, A., Müller, D., Thiem, D.G.E. et al. Effects of throat packs in upper airway surgery under intubation anesthesia: a randomized controlled trial. Clin Oral Invest 26, 6795–6804 (2022). https://doi.org/10.1007/s00784-022-04641-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-022-04641-4