Abstract
The aims of this study were to identify differences in post-operative nausea and vomiting (PONV) and throat pain between throat packed and non-packed patient groups in nasal surgery. This was a prospective, double blind, randomised controlled trial. A water-soaked throat pack gauze was inserted in the mouth to occlude the oropharynx was used in the throat pack group. The second group received no throat pack. A validated PONV questionnaire was completed 6 h post-operatively. Visual analogue scores (VAS) for throat pain were completed in recovery, 2, and 6 h post-operatively. 80 patients were enrolled (40 into each group based on power calculation). With regard to the primary outcome measure, mean PONV score for the throat pack group was 2.75 [median 0, standard deviation (SD 10.86)] and the mean PONV score for the non-packed group was 0.36 (median 0, SD 1.39). The difference in PONV was not statistically significant [P value 0.375, 95% confidence interval (CI) −1.19 to 3.32]. With regard to throat pain VAS scores (our secondary outcome measure), in recovery, the mean throat pain VAS score for the throat packed group was 2.5 (median 1, SD 2.8) and the mean throat pain VAS score for the non-throat packed group was 1.3 (median 0, SD 2.5). Statistical analysis showed a significant difference between the two groups with the throat pack group experiencing more throat pain in recovery (P value 0.018 (95% CI 1.13–2.52). At 2 and 6 h post-operatively, the mean throat pain VAS scores for the throat packed group were 2.1 and 2.3, respectively, and the mean throat pain VAS score for the non-throat packed group was 2.3 and 1.4, respectively. Statistical analysis showed non-significant difference between the two groups at 2 and 6 h post-operatively. The use of throat packs in nasal surgery does not confer PONV reduction benefit. The use of throat pack, however, is associated with a small but statistically significant more throat pain in the initial recovery period from nasal operations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Water-soaked gauze throat packs are utilised in a large number of rhinological procedures in Ear, Nose and Throat (ENT) departments worldwide. The role of a throat pack is primarily to prevent contamination of the aerodigestive tract with blood and secretions. This theoretically prevents airway morbidity and also minimises post-operative nausea and vomiting (PONV) as a result of blood entering the stomach via the oesophagus.
It is well recognised that the use of throat packs can result in significant post-operative throat pain. Various studies suggest an incidence ranging from 15 to 61% [1,2,3]. Other side effects include injury to the underlying mucosa from insertion of the pack [4], risk of throat pack retention [5], and increased risk of aphthous stomatitis [6]. There appears to be no correlation with the duration of packing or number of intubations [7]. No trials have satisfactorily investigated the correlation between using a throat pack and post-operative nausea and vomiting [4].
A recent literature review highlighted the deficiencies in previous studies examining this topic. The review highlighted the paucity of adequately powered, well-designed trials investigating the relationship between the use of throat packs, and post-operative morbidity in terms of pain and PONV.
This study aimed to evaluate the effects of throat pack use in nasal surgery. Our primary outcome measure was difference in post-operative nausea and vomiting (PONV) between patients with and without throat packs during nasal surgery. Our secondary outcome measure was difference in throat pain levels in the same two groups.
Materials and methods
A double blind randomised controlled trial was conducted to investigate the association between the use of throat packs and post-operative morbidity (PONV and throat pain). Patients were randomly assigned to receive a throat pack or not by means of computer generated sequence. The operating surgeon, assessors, and patients were blinded to the group allocation.
The inclusion criteria of the study were all patients aged 18 and over and patients undergoing nasal surgery [including Functional Endoscopic Sinus Surgery (FESS), Septoplasty, Septorhinoplasty, Reduction of inferior turbinates, Nasal polypectomy and divisions of nasal adhesions] requiring general anaesthesia.
The exclusion criteria of the study were patients who were unable to provide informed consent, nasal surgery for malignant disease, and patients with history of post-operative nausea and vomiting.
All patients included in this study were anaesthetised according to a standard anaesthetic protocol. They were also managed post-operatively with a standardised anti-emetic regimen.
Anaesthetic protocol:
-
1.
Induction of anaesthesia with propofol and fentanyl.
-
2.
Muscle relaxant used—atracurium or rocuronium.
-
3.
Endotracheal intubation with an appropriately sized cuffed endotracheal tube [a laryngeal mask airway (LMA) was not used as we felt this would introduce bias from pain associated with the larger size of LMA compared with endotracheal tube].
-
4.
The nose was prepared with Moffett’s solution (a mixture of 10 ml of sterile water for injection, 2 ml of 10% cocaine solution, 2 ml of 1% sodium bicarbonate, and 1 ml of 1:1000 adrenaline). This was to achieve local anaesthesia, vasoconstriction, and decongestion.
-
5.
No anti-emetics and no long-acting opiates were given.
-
6.
All patients received paracetamol intravenously and non-steroidal anti-inflammatory drugs if there was no contraindication.
-
7.
The anaesthetist opened an envelope containing a randomly generated number allocating the patient to either receive a throat pack or no throat pack.
-
8.
If the patient was randomised to receive a throat pack, a water-soaked non-sterile X-ray detectable throat pack of size 10 × 180 cm was fully inserted into the mouth to occlude the oropharynx. The surgeon blinding was achieved by placing a throat pack label on the patient’s forehead for all cases whether throat pack was put in or not. If the patient was assigned to the throat pack group, the throat pack was fully inserted into the oropharynx and the oral cavity without any of the pack being visible to blind the surgeon to the arm the patient was in.
Nasal tampons were routinely used at the end of nasal surgeries that are usually associated with more blood loss that included FESS, FESS + polypectomy, endoscopic nasal polypectomy, and septoplasty for the first 4 h post-operatively in both groups. We anticipated that similar nasal procedures will be performed in each group. Although the use of nasal tampons would result in forced mouth opening and, in theory, potential throat pain, we hypothesised that as both groups received nasal tampons for the more blood losing operations and the same intubation method was used in both groups, the only variable is the throat pack use that may have an influence on any difference in the throat pain scores. The routine post-operative nasal packing in rhinology surgery is an individual surgeon’s preference, and this is reflected by the variation in practice in published surveys [9].
Post-operatively, patients filled out a validated questionnaire measuring degree of PONV based on four questions with a scoring system for each question response based on the study by Wengritzky et al. [8] (“Appendix 1”). The score reaches from 0 to 50. The questions were (1) have you vomited or had dry-retching? (2) Have you experienced a feeling of nausea? (3) Has your nausea been mostly varying or constant? (4) What was the duration of your feeling of nausea [in hours (whole or fraction)]? With regard to throat pain, a visual analogue scale was used ranging from 0 (no pain) to 10 (severe pain) with the patient putting a mark along the scale to point to the level of the pain that they are experiencing. Some patients also included a number to correspond to their mark. For the purpose of analysis, the mark was used to correspond with a number with up to one decimal point. The PONV questionnaire and throat pain scales were filled at the following specified time intervals:
-
PONV at 6 h post-operatively;
-
throat pain in recovery, 2 and 6 h post-operatively.
Ethical approval was obtained prior to the commencement of this study from the regional research ethics committee and from the local research and development department.
With regard to statistical analysis, we utilised a validated PONV scoring scale with an already calculated effect size based on the study by Wengritzky et al. [8]. In anticipation that we may get a normal distribution, a two-tail, t test with an effect size of 0.82 was used, and power calculation using IBM SPSS statistics version 19 showed that a sample size of 80 patients (40 per group) was required:
-
alpha set at 0.05 (standard);
-
power set at 0.95 (standard).
We performed a t test, because we hoped to get a normal distribution, and two-tailed, because we did not have a definite hypothesis about whether we will get more or less vomiting with the pack. A P value of less than <0.05 was considered statistically significant.
The results, however, showed that the data were non-parametric as it was not normally distributed, and the Mann–Whitney test (exact two-tailed) was subsequently used for the purpose of statistical analysis.
Results and analysis
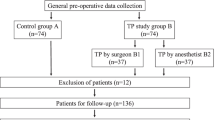
80 patients were enrolled over a 2-year period; 40 patients into each study arm. There were 57 males and 23 females. Age ranged from 18 to 72 years. Table 1 shows the patient demographics and operations that were performed for the throat pack and no throat pack groups.
With regard to the primary outcome measure, mean PONV score for the throat pack group was 2.75 [median 0, standard deviation (SD 10.86)] and the mean PONV score for the non-packed group was 0.36 (median 0, SD 1.39) (Fig. 1 shows the mean PONV for both groups). The difference in PONV was not statistically significant [P value 0.375, 95% confidence interval (CI) = −1.19 to 3.32].
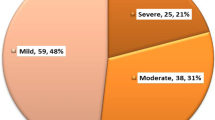
With regard to throat pain VAS scores (our secondary outcome measure), in recovery, the mean throat pain VAS score for the throat packed group was 2.5 (median 1, SD 2.8) and the mean throat pain VAS score for the non-throat packed group was 1.3 (median 0, SD 2.5). Statistical analysis showed a significant difference between the two groups with the throat pack group experiencing more throat pain in recovery (P value 0.018 (95% CI 1.13–2.52). At 2 h post-operatively, the mean throat pain VAS score for the throat packed group was 2.1 (median 1.25, SD 2.4) and the mean throat pain VAS score for the non-throat packed group was 2.3 (median 1.5, SD 2.8). Statistical analysis showed non-significant difference between the two groups at 2 h (P = 0.962 95% CI 1.64–2.81). At 6 h post-operatively, the mean throat pain VAS score for the throat packed group was 1.4 (median 1, SD 1.6) and the mean throat pain VAS scores for the non-packed group was 1.6 (median 0, SD 2.4). Statistical analysis showed non-significant difference between the two groups at 6 h (P = 0.546, 95% CI 1.02–1.93). Figure 2 shows mean values for the throat pain VAS scores. Table 2 summarises the PONV and throat pain VAS scores results.
Discussion
The questions on the effects of throat packs in nasal surgery with regard to post-operative nausea and vomiting and throat pain have been previously studied with randomised controlled trials [10,11,12,13]. Nonetheless, the methodological flaws of the previous randomised controlled trials have been highlighted by the review of the topic by Jaiswal et al. who recommended that further adequately powered studies are required in an attempt to confirm best practice. In this study, we present the results of an adequately powered randomised controlled trial using validated PONV and pain questionnaires.
The important theoretical reasons of using the throat packs in nasal surgery include reduction in aspirated and ingested blood into the airway and oesophagus, respectively. There were no airway morbidity events noted during this study. The lack of statistically significant difference in PONV intensity score contradicts the theoretical reason for using throat packs in nasal surgery. With regard to throat pain, although small in terms of difference, the only statistically significant event in this study was that throat pain in recovery was higher in the throat pack group. Inlight of the results of this study, weighing up the theoretical reasons for using throat packs whilst considering minimising the patient discomfort in the recovery period are important considerations in the decision whether to use throat packs or not. Furthermore, with the current drive in performing most rhinological procedures as day case surgeries for patient benefits, financial, and case turnover reasons, the use of throat packs could potentially delay the patient discharge due to throat pain.
The results of this study corroborate recently published literature addressing the subject of the effects of throat packs in nasal surgery with regard to PONV and throat pain scores [14]. However, our study differs from Karbasforushan et al. [14] study in that we used a published validated PONV questionnaire for measuring PONV.
Possible limitations of our study design could be the inclusion of a wide range of rhinological procedures in our study sample. However, we believe that the range of surgeries included is representative of most otorhinolaryngology units that offer a rhinology service who can then consider applying the conclusions of our study into their practice. Other limitations include the use of nasal packing post-operatively; however, as the nasal packing and the method of intubations were similar in both groups, the difference in throat pain should be in relation to the only variable which is the use of throat pack.
In conclusion, the routine use of throat packs in nasal surgery is a matter of debate. Their use is purported to prevent blood aspiration and ingestion into the airway and the gastrointestinal tract thereby reducing PONV. The results of this randomised controlled trial show no statistical difference between the packed and non-packed groups in terms of PONV. Throat pain scores were significantly higher in recovery in the throat packed group; however, there were low VAS scores at 2 and 6 h and those were not statistically significant. This randomised controlled trial, therefore, shows that throat packs in nasal surgery do not lower the risk of PONV and are associated with more throat pain in the immediate period after surgery. In the decision-making process whether to use a throat pack or not in nasal surgery, the clinician would need to consider the purposed rationale for using throat packs and the potentially small but statistically significant results of increased throat pain in recovery.
Summary
-
The current evidence for the benefits of the use of throat packs in nasal surgery is equivocal. Reviews of the topic concluded that adequately powered randomised controlled trials are needed to address this issue.
-
This randomised controlled trial concludes that throat packs do not lower the risk of post-operative nausea and vomiting and are associated with more throat pain in the immediate recovery period after nasal surgery.
References
Conway CM, Miller JS, Sugden FLH (1960) Sore throat after anaesthesia. Br J Anaesth 32:219–223
Edmuds-Seal J, Eve JH (1962) Minor sequelae anaesthesia: a pilot study. Br J Anaesth 34:44–48
Hartsell CJ, Stephen CR (1964) Incidence of sore throat following endotracheal intubation. Can J Anaesth 11:307–312
Jaiswal V, Bedford GC (2009) Review of nasal packs in nasal surgery. JLO 123:701–704
Colbert S, Jackson M, Turner M, Brennan PA (2012) Reducing the risk of retained throat packs after surgery. Br J Oral Maxillofac Surg 50:680–681
Erkalp K, Korkut YA, Meric A, Kahya V, Gedikli O, Su OK, Saitoglu L (2010) Pharyngeal packing is a predisposing factor for postoperative aphthous stomatitis in nasal surgery. Otolaryngol Head Neck Surg 142:672–676
Christensen AM, Willemoes-Larsen H, Lundby L, Jakobsen KB (1994) Postoperative throat complaints after tracheal intubation. Br J Anaesth 73:786–787
Wengritzky R, Mettho T, Myles PS, Burke J, Kakos A (2010) Development and validation of a postoperative nausea and vomiting intensity scale. Br J Anaesth 104:158–166
Repanos C, McDonald SE, Sadr AH (2009) A survey of postoperative nasal packing among UK ENT surgeons. Eur Arch Otorhinolaryngol 266:1575
Marais J, Prescott RJ (1993) Throat pain and pharyngeal packing: a controlled randomized double-blind comparison between gauze and tampons. Clin Otolaryngol 18:426–429
Elhakim M, Siam A, Rahsed I, Hamdy MH (2000) Topical tenox- icam from pharyngeal pack reduces post operative sore throat. Acta Anaesthesiol Scand 44:273–277
Basha SI, McCoy E, Ullah R, Kinsella JB (2006) The efficacy of pharyngeal packing during routine nasal surgery—a prospective randomised controlled study. Anaesthesia 61:1161–1165
Piltcher O, Levinksy M, de Oliverio Levinsky J, Basso PR (2007) Effectiveness of hypopharyngeal packing during nasal and sinus surgery in the prevention of PONV. Otolaryngol Head Neck Surg 137:552–554
Karbasforushan A, Hemmatpoor B, Makhsosi BR, Mahavar T, Golfam P, Khiabani B (2014) The Effect of Pharyngeal Packing during Nasal Surgery on the Incidence of Post Operative Nausea, Vomiting, and Sore Throat. Iran J Otorhinolaryngol 26:219–223
Acknowledgements
The authors would like to thank Dr. Suresh Yadlapalli and Dr. Naail Alzuhir for their help with the study design and statistical analysis, respectively.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflict of interest
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional guidelines on human experimentation [Cambridgeshire 3 research ethics committee (REC) and also the Peterborough City Hospital Research and Development department (R&D)] and with the Helsinki Declaration of 1975, as revised in 2008.
Appendix 1: PONV questionnaire
Appendix 1: PONV questionnaire
As adopted from the study by Wengritzky et al. [8]. 
Rights and permissions
About this article
Cite this article
Al-lami, A., Amonoo-Kuofi, K., Kulloo, P. et al. A study evaluating the effects of throat packs during nasal surgery: a randomised controlled trial. Eur Arch Otorhinolaryngol 274, 3109–3114 (2017). https://doi.org/10.1007/s00405-017-4589-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-017-4589-5