Abstract
Objective
To analyze the influence of an oral bisphosphonate and compare the potency to intravenous bisphosphonates on various cell types as regards the rarity of bisphosphonate-associated osteonecrosis of the jaw (BP-ONJ) caused by oral bisphosphonate.
Materials and methods
A viability assay (MTT), a migration assay (Boyden chamber), and an apoptosis assay (Caspase-Glo® 3/7) were performed to analyze the effect of bisphosphonates on human fibroblasts, umbilical vein endothelial cells (HUVEC), and osteoblasts.
Results
Alendronate and intravenous bisphosphonates suppressed cell viability and migration, and induced apoptosis in all tested cell types. Alendronate had a greater impact than ibandronate on the characteristics in fibroblasts and osteoblasts but not as strong as zoledronate.
Conclusions
The incidence of BP-ONJ in oral bisphosphonate treatment is reported to be much lower than that in intravenous bisphosphonates. However, the influences of alendronate on human cells were at least as strong as ibandronate, although it was lower than zoledronate.
Clinical relevance
Alendronate showed strong enough effects to suppress human somatic cells and was comparable to certain intravenous bisphosphonates in potency. This study suggests that the lower incidence of BP-ONJ in alendronate treatment is not originated by its potency, but might be due to the low bioavailability of alendronate, lower dosing on a daily basis, and having no additional therapies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bisphosphonates decrease bone resorption by their anti-osteoclastic activity. Their avid affinity to bone tissue and anti-resorption activity have made bisphosphonates a popular choice for treatment of bone diseases, such as osteoporosis, Paget’s disease, multiple myeloma, and several tumors metastasizing into the bone tissue [1,2,3,4,5]. The anti-tumor property of bisphosphonates depends on anti-resorptive and anti-angiogenic effects and induction of tumor cell apoptosis [6,7,8]. Because of these effects, bisphosphonates are prescribed for bone malignancies as an effective treatment to reduce skeletal complications and the need for additional radiotherapy and chemotherapy and stabilizing operations [4]. Moreover, since alendronate was approved for postmenopausal osteoporosis prevention and treatment in 1995, bisphosphonates became more widely used. The number of prescriptions for oral bisphosphonates was almost 15 million in the USA in 2012 [9].
The most common adverse effects of bisphosphonates are gastrointestinal effects, renal impairment, acute-phase reactions, and bisphosphonate-associated osteonecrosis of the jaw (BP-ONJ) [10]. There have been many attempts to identify and explore the nature of BP-ONJ since Marx reported the intraoral necrotic bony lesions in patients exposed to bisphosphonates in 2003 [11].
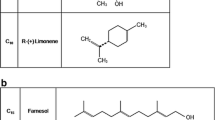
Bisphosphonates affect several types of somatic cells including keratinocytes, fibroblasts, human umbilical endothelial cells (HUVEC), endothelial progenitor cells, and osteoblasts, as well as osteoclasts [12,13,14] so that soft tissues and vessels surrounding bone are also compromised. Given that nitrogen-containing bisphosphonates suppress the mevalonate pathway by inhibiting enzymes involved in the synthesis of farnesyl diphosphate (FPP) [15] and that non-nitrogen-containing bisphosphonates are metabolically converted into cytotoxic analogues of adenosine triphosphate (ATP) [16, 17], it is reasonable to assume that bisphosphonates influence various cell types by the same process as in osteoclasts. Compromised functions in those cells may suppress bone formation and wound healing, and restrict the supply of nutrients. Therefore, bone and surrounding tissue viability may decline, contributing to the occurrence of BP-ONJ.
However, the occurrence of BP-ONJ in oral bisphosphonate treatment is reported to be much lower than that in intravenous bisphosphonates [18,19,20,21,22,23,24,25,26,27,28]. Therefore, it is important to explore the influence of oral bisphosphonate and compare the potency to intravenous bisphosphonates on various cell types to clarify the rarity of BP-ONJ caused by alendronate. This study investigated the differences between the potency of oral and intravenous bisphosphonates on human somatic cells and the effects of those bisphosphonates. Four bisphosphonates (alendronate, zoledronate, ibandronate, and clodronate) were chosen to compare their effects on cell viability, migration, and apoptosis. Human fibroblasts, human osteoblasts, and HUVEC were selected because of their role in bone remodeling and wound healing.
Materials and methods
Cell culture
Human periodontal ligament fibroblasts (Lonza, Basel, Switzerland: No. CC-7049), HUVEC (Lonza, Basel, Switzerland: No. CC-2517A), and human osteoblasts (Promocell, Heidelberg, Germany: No. C-12720) were purchased from the respective companies. Cells were cultured according to the manufacturer’s instructions. Growth medium was changed every 2–3 days and subcultured with Accutase solution (Sigma-Aldrich, St. Louis, USA) when they reached 70–80% confluence. Cells of passages 4 to 7 were used in experiments. Human periodontal ligament fibroblasts were cultivated with growth medium consisting of Dulbecco’s modified Eagle’s medium (DMEM; Life Technologies, CA, USA), 1% penicillin-streptomycin-neomycin antibiotic mixture (PSN), 1% L-glutamine, 10% fetal calf serum (FCS), and 1 ng/ml basic fibroblast growth factor (bFGF). HUVEC were grown with endothelial basal medium (EBM2; Lonza, Basel, Switzerland), supplemented with EGM-2 SingleQuot™ Kit (Lonza, Basel, Switzerland). Human osteoblasts were cultured with Osteoblast Growth Medium (Promocell, Heidelberg, Germany) with SupplementMix (Promocell, Heidelberg, Germany). Cells were maintained in a humidified incubator with 5% CO2 and 95% air at 37 °C.
Bisphosphonates
Zometa (zoledronate, Novartis Pharma, Basel, Switzerland), Bonviva (ibandronate, Roche, Basel, Switzerland), and Alendron (alendronate, Hexal AG; Novartis group, Holzkirchen, Germany) were used as nitrogen-containing bisphosphonates and Bonefos (clodronate, Bayer, Leverkusen, Germany) was used as a non-nitrogen-containing bisphosphonate. The alendronate tablet was pulverized and dissolved in phosphate-buffered saline (PBS) and then the pH of the solution was adjusted and sterilized by filtration. Control was incubated with the growth medium mentioned above only.
Cell viability test
MTT colorimetric assay (Sigma-Aldrich, Saint Louis, USA) was performed to evaluate the effects of bisphosphonates on cell viability. Cells were seeded into 12- or 24-well plates with densities of 10,000 cells/cm2 for fibroblasts, 15,000 cells/cm2 for HUVEC, and 13,000 cells/cm2 for osteoblasts. The assay was conducted in triplicate with four replicates for each experiment. Twenty-four hours later, phenol-free growth medium was added to the wells with increasing concentrations (0, 5, 50, 100, 200, and 500 μM) of each bisphosphonate (zoledronate, ibandronate, alendronate, clodronate). Seventy-two hours after the addition of bisphosphonates, MTT solution was supplemented to each well and incubated for another 4 h. Afterwards, the wells were rinsed and cell lysis buffer (isopropanol and 2 N HCL, 49:1) was added to lyse the cells in each well. After 30 min of incubation, the contents of the wells were photometrically measured by a microplate reader (Synergy HT; BioTek, Winooski, USA) at 570 nm.
Cell migration test
The Boyden chamber assay system (24-well ThinCertTM, Greiner Bio-One, Kremsmünster, Austria) was performed to analyze the migration ability. Twenty-five-square centimeter flasks were used with seeding densities of 10,000 cells/cm2 for fibroblasts, 15,000 cells/cm2 for HUVEC, and 13,000 cells/cm2 for osteoblasts. The assay was conducted in triplicate with three replicates for each experiment. Twenty-four hours after the seeding, fresh growth medium containing 0 and 50 μM bisphosphonate (zoledronate, ibandronate, alendronate, clodronate) was added. After 72 h of incubation, the cells were harvested and the final cell number for each group was adjusted to 5 × 105 cells/ml in serum-free medium. Each well was filled with 600 μl of cell culture medium with chemoattractant (fetal calf serum) and 24-well ThinCert™ cell culture inserts were placed in the wells. Then 200 μl of cell suspension was added to the 24-well ThinCert™ cell culture insert and maintained in cell incubator for 24 h. After the staining with Calcein-AM fluorescent dye (Invitrogen, MA, USA), the cells in the upper and lower compartments were carefully washed with PBS and the inserts were transferred into a new black 24-well plate filled with 500 μl of Accutase (Sigma-Aldrich, St. Louis, USA). Ten minutes later, the cells on the bottom of the lower chamber were detached and the quantification of fluorescence was determined by a microplate fluorescence reader (Synergy HT; BioTek, Winooski, USA) at an excitation wavelength of 485 nm and an emission wavelength of 520 nm.
Apoptosis test
Caspase 3/7 activity was measured with the Caspase-Glo® 3/7 Assay (Promega, Madison, WI, USA) to evaluate the effects of bisphosphonates on cell apoptosis. Cells were seeded into transparent 96-well plates with densities of 15,000 cells/cm2 for fibroblasts, 20,000 cells/cm2 for HUVEC, and 15,000 cells/cm2 for osteoblasts. The assay was conducted in triplicate with six replicates for each experiment. After 24 h of incubation, each well was rinsed with PBS and further incubated for 72 h with fresh culture medium containing 0 and 50 μM bisphosphonate (zoledronate, ibandronate, alendronate, clodronate). Afterwards, the Caspase-Glo® substrate and buffer mixture was added to each well of the plates and incubated for 1 h at room temperature. The content in each well of the transparent 96-well plate was transferred into a new white-walled 96-well plate and the luminescence was measured by a microplate reader (Synergy HT; BioTek, Winooski, USA) according to the manufacturer’s protocol.
Statistical analysis
The results were analyzed by analysis of variance (ANOVA) with the post hoc test Tukey or Kruskal-Wallis test followed by Mann-Whitney test as post hoc test, with SPSS statistic software 15.0. The α-level was set to 0.05 in ANOVA and it was set to 0.005 by the Bonferroni correction in case of Kruskal-Wallis with Mann-Whitney test. Each box plot shows values between the 25th and 75th percentile and the median value was expressed as the black line within the box. Whiskers indicate 1.5 times the value of interquartile range (IQR) and circles represent outliers within 3 IQR, while x represents outliers over 3 IQR.
Results
Cell viability (Fig. 1 and Table 1)
In fibroblasts, the zoledronate group was the most affected one, followed by alendronate and ibandronate. However, no significance was found between zoledronate and alendronate (P = 0.146), and alendronate was significantly more potent than ibandronate (P = 0.047). The alendronate and ibandronate groups showed significant differences to control at 50 μM and higher (P ≤ 0.001), while the zoledronate group showed a difference at 5 μM (P = 0.016) and higher. At 500 μM, the cell viability in the zoledronate, alendronate, ibandronate, and clodronate group decreased by 61, 53, 46, and 21%, respectively.
Cell viability test in fibroblasts (a), HUVEC (b), and osteoblasts (c). Relative optical densities (OD) were expressed compared to the control group set to 1.0. Vertical bars represent standard deviations and asterisks indicate statistical significance between groups or compared to the control group (P < 0.05). The concentrations higher than the asterisks displayed significant differences compared to the control group
In HUVEC, ibandronate was more potent than alendronate except at 500 μM (P < 0.001). Alendronate was the third most potent bisphosphonate to decrease the viability. However, no significance was observed between them at 500 μM (P = 0.336). Alendronate and ibandronate significantly affected HUVEC viability at 50 μM (P ≤ 0.001) and higher, whereas 5 μM zoledronate significantly suppressed cell viability (P = 0.034). The influence of zoledronate was the most potent, with 87% decreased cell viability at 500 μM compared to the control group.
In osteoblasts, zoledronate also showed the strongest influence and reduced the cell viability by 55% at 500 μM compared to control. Alendronate and ibandronate were statistically similar in their effects (P = 0.998). Cell viability decreased by 43% by alendronate, 45% ibandronate, and 27% clodronate, at 500 μM.
Cell migration (Fig. 2 and Table 2)
In fibroblasts, zoledronate was the most effective; the migration rate was reduced by 51% compared to the control group (P < 0.001). Alendronate was the second strongest, reducing cell migration rate by 27%, following zoledronate. However, alendronate was statistically indifferent from ibandronate (P = 0.796), which decreased the migration rate by approximately 26%. Clodronate failed to decrease the migration of fibroblasts.
The migration of HUVEC in the zoledronate group was significantly higher than that in the alendronate and ibandronate groups (P < 0.001). The migration rate decreased by 88%, followed by ibandronate (58%), alendronate (27%), and clodronate (2%). Ibandronate was significantly more potent than alendronate (P < 0.001).
In osteoblasts, although no statistical significance was found between alendronate and ibandronate (P = 0.043), alendronate was more potent than ibandronate. Alendronate decreased the migration rate by 39% compared to the control group, 54% for zoledronate, and 29% for ibandronate.
Cell apoptosis (Fig. 3 and Table 3)
In fibroblasts, zoledronate was the strongest bisphosphonate at increasing the apoptosis. It increased fivefold compared to the control group and was significantly different compared to all the other bisphosphonates (all P < 0.001). Alendronate produced a threefold increase (P < 0.001), followed by ibandronate and clodronate.
In HUVEC, increased apoptotic enzyme activity was also found. Zoledronate produced a 2.5-fold increase, followed by ibandronate, clodronate, and alendronate (P < 0.001). However, there was no significant difference between zoledronate and ibandronate (P = 0.226). Alendronate failed to show a significant difference compared to control (P = 0.192) and clodronate (P = 0.265).
In osteoblasts, alendronate increased apoptotic enzyme activity 6.9-fold, following 7.9-fold in zoledronate, compared to control. No statistical significance was found between zoledronate and alendronate. Ibandronate was less effective than alendronate. The influence of clodronate was the weakest and it was not statistically significant compared to control (P = 0.239).
Discussion
Bisphosphonates primarily target osteoclast activities and aim to control abnormal bone metabolism caused by various bone malignancies or osteoporosis and therefore change the bone turnover. As one of the side effects of bisphosphonates, BP-ONJ was reported, and the etiology has been investigated. One of the causes next to the impaired bone turnover is the influence of bisphosphonates on several cell types around bone tissue [29,30,31]. Bisphosphonates that have currently been taken or dissociated from the underlying bone during resorption [17] compromise the function of fibroblasts and vessel cells, subsequently impairing re-epithelialization of oral mucosa and nutrition supply. Along with the fragile and vulnerable oral environment, due to thin mucosal coverage, microflora, eating, and frequent dental procedures, compromised cell functions and viability are considered to contribute to the occurrence of BP-ONJ. Therefore, fibroblasts, osteoblasts, and HUVEC were chosen to verify the effects of alendronate and compare with intravenous bisphosphonates.
The bisphosphonate-associated osteonecrosis usually occurs after the intake of nitrogen-containing bisphosphonates. But the frequency in patients taking alendronate, that is administered orally, is surprisingly low [25,26,27,28].
Alendronate prescriptions comprised over 1.3 × 108 of the total of 2 × 108 bisphosphonate defined daily doses in Germany in 2011 [32, 33], and the total annual administered dose of alendronate is much higher than oncologic doses of zoledronate and ibandronate [34, 35]. Nevertheless, the incidence of BP-ONJ in patients treated using oral bisphosphonates (0.0007–0.34%) [25,26,27,28] is much lower than that in patients receiving intravenous bisphosphonates (1.2–18.6%) [18,19,20,21,22,23,24]. Considering these facts, the potency of alendronate can be presumed much lower than that of intravenous bisphosphonates; however, alendronate had strong inhibitory effects that are enough to compromise cell viability and migration capacity, and induce cell apoptosis in this study. Alendronate was even more potent than ibandronate in fibroblasts and osteoblasts, although ibandronate showed stronger influences in HUVEC and zoledronate was measured as the most potent bisphosphonate throughout the experiment. McLeod et al. reported that alendronate suppressed cell proliferation at 100 μM in human fibroblasts and 10 μM in oral keratinocytes, although zoledronate showed stronger effects on both cell types [14]. Martins et al. also found that alendronate inhibited the proliferation of human fibroblasts and human osteogenic sarcoma cells at over 10 μM with the incubation of 24 h [36].
Based on these findings, it can be surmised that there could be several contributing factors involved in the rarity of BP-ONJ caused by alendronate. First, because of the low bioavailability of alendronate, which is assumed approximately 0.6% and varies according to the conditions upon drug use and the gastric pH [37], the amount of alendronate absorbed decreases considerably compared to the initial dose of alendronate. Second, considering the low daily dosing of alendronate, it takes an extended time to accumulation in bone tissue to a level that is high enough to induce BP-ONJ, while dissociation of the bisphosphonates from the bone occurs simultaneously during the administration period. On the other hand, zoledronate is usually administered intravenously once every 3–4 weeks with high dose for tumor patients so that the initial impact from the bisphosphonate could be more tremendous and might reach the level to induce BP-ONJ, although dissociation of the drug molecules occurs afterwards. Therefore, these factors may affect the low incidence of BP-ONJ caused by alendronate, regardless of its drug potency. Lastly, chemotherapy and radiotherapy in tumor patients may also help explain the higher incidence of BP-ONJ in intravenous bisphosphonate therapy, in case these additional therapies had been accompanied, because of suppressed immune system and bone viability.
The results from this study suggest that the potency of alendronate in compromising various cell activities as oral bisphosphonate is comparable to certain intravenous bisphosphonates. Thus, these findings address that the rarity of BP-ONJ in alendronate treatment may be caused by not only its potency, but also the low bioavailability of alendronate [37], lower dosing of alendronate on a daily basis, and having no additional therapies. Additionally, this study is also in agreement with the theory that bisphosphonates detrimentally affect not only osteoclasts, but also several other somatic cell types. These negative influences may act as a critical factor in the pathogenesis of BP-ONJ and the strongest negative effects of zoledronate help understand the higher incidence of BP-ONJ in tumor patients receiving intravenous bisphosphonates.
References
Black DM, Bauer DC, Schwartz AV, Cummings SR, Rosen CJ (2012) Continuing bisphosphonate treatment for osteoporosis—for whom and for how long? N Engl J Med 366(22):2051–2053. https://doi.org/10.1056/NEJMp1202623
Terpos E, Kleber M, Engelhardt M, Zweegman S, Gay F, Kastritis E, van de Donk NW, Bruno B, Sezer O, Broijl A, Bringhen S, Beksac M, Larocca A, Hajek R, Musto P, Johnsen HE, Morabito F, Ludwig H, Cavo M, Einsele H, Sonneveld P, Dimopoulos MA, Palumbo A, European Myeloma N (2015) European Myeloma Network guidelines for the management of multiple myeloma-related complications. Haematologica 100(10):1254–1266. https://doi.org/10.3324/haematol.2014.117176
Hald JD, Evangelou E, Langdahl BL, Ralston SH (2015) Bisphosphonates for the prevention of fractures in osteogenesis imperfecta: meta-analysis of placebo-controlled trials. J Bone Miner Res 30(5):929–933. https://doi.org/10.1002/jbmr.2410
Van Acker HH, Anguille S, Willemen Y, Smits EL, Van Tendeloo VF (2016) Bisphosphonates for cancer treatment: mechanisms of action and lessons from clinical trials. Pharmacol Ther 158:15824–15840. https://doi.org/10.1016/j.pharmthera.2015.11.008
Choi WS, Lee JI, Yoon HJ, Min CK, Lee SH (2017) Medication-related osteonecrosis of the jaw: a preliminary retrospective study of 130 patients with multiple myeloma. Maxillofac Plast Reconstr Surg 39(1):1. https://doi.org/10.1186/s40902-016-0099-4
Green J, Lipton A (2010) Anticancer properties of zoledronic acid. Cancer Investig 28(9):944–957. https://doi.org/10.3109/07357907.2010.512598
Tamura T, Shomori K, Nakabayashi M, Fujii N, Ryoke K, Ito H (2011) Zoledronic acid, a third-generation bisphosphonate, inhibits cellular growth and induces apoptosis in oral carcinoma cell lines. Oncol Rep 25(4):1139–1143. https://doi.org/10.3892/or.2011.1152
Stresing V, Fournier PG, Bellahcene A, Benzaid I, Monkkonen H, Colombel M, Ebetino FH, Castronovo V, Clezardin P (2011) Nitrogen-containing bisphosphonates can inhibit angiogenesis in vivo without the involvement of farnesyl pyrophosphate synthase. Bone 48(2):259–266. https://doi.org/10.1016/j.bone.2010.09.035
Wysowski DK, Greene P (2013) Trends in osteoporosis treatment with oral and intravenous bisphosphonates in the United States, 2002-2012. Bone 57(2):423–428. https://doi.org/10.1016/j.bone.2013.09.008
Diel IJ, Bergner R, Grotz KA (2007) Adverse effects of bisphosphonates: current issues. J Support Oncol 5(10):475–482
Marx RE (2003) Pamidronate (Aredia) and zoledronate (Zometa) induced avascular necrosis of the jaws: a growing epidemic. J Oral Maxillofac Surg 61(9):1115–1117. https://doi.org/10.1016/S0278-2391(03)00720-1
Acil Y, Moller B, Niehoff P, Rachko K, Gassling V, Wiltfang J, Simon MJ (2012) The cytotoxic effects of three different bisphosphonates in-vitro on human gingival fibroblasts, osteoblasts and osteogenic sarcoma cells. J Craniomaxillofac Surg 40(8):e229–e235. https://doi.org/10.1016/j.jcms.2011.10.024
Marolt D, Cozin M, Vunjak-Novakovic G, Cremers S, Landesberg R (2012) Effects of pamidronate on human alveolar osteoblasts in vitro. J Oral Maxillofac Surg 70(5):1081–1092. https://doi.org/10.1016/j.joms.2011.05.002
McLeod NM, Moutasim KA, Brennan PA, Thomas G, Jenei V (2014) In vitro effect of bisphosphonates on oral keratinocytes and fibroblasts. J Oral Maxillofac Surg 72(3):503–509. https://doi.org/10.1016/j.joms.2013.08.007
Amin D, Cornell SA, Gustafson SK, Needle SJ, Ullrich JW, Bilder GE, Perrone MH (1992) Bisphosphonates used for the treatment of bone disorders inhibit squalene synthase and cholesterol biosynthesis. J Lipid Res 33(11):1657–1663
Rogers MJ, Russell RG, Blackburn GM, Williamson MP, Watts DJ (1992) Metabolism of halogenated bisphosphonates by the cellular slime mould Dictyostelium discoideum. Biochem Biophys Res Commun 189(1):414–423. https://doi.org/10.1016/0006-291X(92)91574-A
Rogers MJ, Crockett JC, Coxon FP, Monkkonen J (2011) Biochemical and molecular mechanisms of action of bisphosphonates. Bone 49(1):34–41. https://doi.org/10.1016/j.bone.2010.11.008
Kyle RA, Yee GC, Somerfield MR, Flynn PJ, Halabi S, Jagannath S, Orlowski RZ, Roodman DG, Twilde P, Anderson K, American Society of Clinical O (2007) American Society of Clinical Oncology 2007 clinical practice guideline update on the role of bisphosphonates in multiple myeloma. J Clin Oncol 25(17):2464–2472. https://doi.org/10.1200/JCO.2007.12.1269
Boonyapakorn T, Schirmer I, Reichart PA, Sturm I, Massenkeil G (2008) Bisphosphonate-induced osteonecrosis of the jaws: prospective study of 80 patients with multiple myeloma and other malignancies. Oral Oncol 44(9):857–869. https://doi.org/10.1016/j.oraloncology.2007.11.012
Walter C, Al-Nawas B, Grotz KA, Thomas C, Thuroff JW, Zinser V, Gamm H, Beck J, Wagner W (2008) Prevalence and risk factors of bisphosphonate-associated osteonecrosis of the jaw in prostate cancer patients with advanced disease treated with zoledronate. Eur Urol 54(5):1066–1072. https://doi.org/10.1016/j.eururo.2008.06.070
Kos M (2015) Incidence and risk predictors for osteonecrosis of the jaw in cancer patients treated with intravenous bisphosphonates. Arch Med Sci 11(2):319–324. https://doi.org/10.5114/aoms.2015.50964
Bamias A, Kastritis E, Bamia C, Moulopoulos LA, Melakopoulos I, Bozas G, Koutsoukou V, Gika D, Anagnostopoulos A, Papadimitriou C, Terpos E, Dimopoulos MA (2005) Osteonecrosis of the jaw in cancer after treatment with bisphosphonates: incidence and risk factors. J Clin Oncol 23(34):8580–8587. https://doi.org/10.1200/JCO.2005.02.8670
Hoff AO, Toth BB, Altundag K, Johnson MM, Warneke CL, Hu M, Nooka A, Sayegh G, Guarneri V, Desrouleaux K, Cui J, Adamus A, Gagel RF, Hortobagyi GN (2008) Frequency and risk factors associated with osteonecrosis of the jaw in cancer patients treated with intravenous bisphosphonates. J Bone Miner Res 23(6):826–836. https://doi.org/10.1359/jbmr.080205
Dimopoulos MA, Kastritis E, Anagnostopoulos A, Melakopoulos I, Gika D, Moulopoulos LA, Bamia C, Terpos E, Tsionos K, Bamias A (2006) Osteonecrosis of the jaw in patients with multiple myeloma treated with bisphosphonates: evidence of increased risk after treatment with zoledronic acid. Haematologica 91(7):968–971
Mavrokokki T, Cheng A, Stein B, Goss A (2007) Nature and frequency of bisphosphonate-associated osteonecrosis of the jaws in Australia. J Oral Maxillofac Surg 65(3):415–423. https://doi.org/10.1016/j.joms.2006.10.061
Ulmner M, Jarnbring F, Torring O (2014) Osteonecrosis of the jaw in Sweden associated with the oral use of bisphosphonate. J Oral Maxillofac Surg 72(1):76–82. https://doi.org/10.1016/j.joms.2013.06.221
American Dental Association Council on Scientific A (2006) Dental management of patients receiving oral bisphosphonate therapy: expert panel recommendations. J Am Dent Assoc 137(8):1144–1150
Kwon JW, Park EJ, Jung SY, Sohn HS, Ryu H, Suh HS (2015) A large national cohort study of the association between bisphosphonates and osteonecrosis of the jaw in patients with osteoporosis: a nested case-control study. J Dent Res 94(9 Suppl):212S–219S. https://doi.org/10.1177/0022034515587862
Walter C, Pabst A, Ziebart T, Klein M, Al-Nawas B (2011) Bisphosphonates affect migration ability and cell viability of HUVEC, fibroblasts and osteoblasts in vitro. Oral Dis 17(2):194–199. https://doi.org/10.1111/j.1601-0825.2010.01720.x
Misso G, Porru M, Stoppacciaro A, Castellano M, De Cicco F, Leonetti C, Santini D, Caraglia M (2012) Evaluation of the in vitro and in vivo antiangiogenic effects of denosumab and zoledronic acid. Cancer Biol Ther 13(14):1491–1500. https://doi.org/10.4161/cbt.22274
Manzano-Moreno FJ, Ramos-Torrecillas J, De Luna-Bertos E, Ruiz C, Garcia-Martinez O (2015) High doses of bisphosphonates reduce osteoblast-like cell proliferation by arresting the cell cycle and inducing apoptosis. J Craniomaxillofac Surg 43(3):396–401. https://doi.org/10.1016/j.jcms.2014.12.008
Schwabe UPD (2012) Arzneiverordnungs-Report 2012: Aktuelle Daten, Kosten, Trends und Kommentare. Springer, Heidelberg. https://doi.org/10.1007/978-3-642-29242-2
Walter C, Sagheb K, Bitzer J, Rahimi-Nedjat R, Taylor KJ (2014) Analysis of reasons for osteonecrosis of the jaws. Clin Oral Investig 18(9):2221–2226. https://doi.org/10.1007/s00784-014-1205-6
Fisher JE, Rosenberg E, Santora AC, Reszka AA (2013) In vitro and in vivo responses to high and low doses of nitrogen-containing bisphosphonates suggest engagement of different mechanisms for inhibition of osteoclastic bone resorption. Calcif Tissue Int 92(6):531–538. https://doi.org/10.1007/s00223-013-9711-0
Otto S, Pautke C, Opelz C, Westphal I, Drosse I, Schwager J, Bauss F, Ehrenfeld M, Schieker M (2010) Osteonecrosis of the jaw: effect of bisphosphonate type, local concentration, and acidic milieu on the pathomechanism. J Oral Maxillofac Surg 68(11):2837–2845. https://doi.org/10.1016/j.joms.2010.07.017
Martins CA, Leyhausen G, Volk J, Geurtsen W (2015) Effects of alendronate on osteoclast formation and activity in vitro. J Endod 41(1):45–49. https://doi.org/10.1016/j.joen.2014.07.010
Gertz BJ, Holland SD, Kline WF, Matuszewski BK, Freeman A, Quan H, Lasseter KC, Mucklow JC, Porras AG (1995) Studies of the oral bioavailability of alendronate. Clin Pharmacol Ther 58(3):288–298. https://doi.org/10.1016/0009-9236(95)90245-7
Acknowledgements
The part of this work was presented in thesis form for the doctoral dissertation for Junho Jung from Johannes-Gutenberg University Mainz.
Funding
This study was funded by the International Team for Implantology (ITI) scholarship program (to the first author).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent is not required for this study.
Rights and permissions
About this article
Cite this article
Jung, J., Park, J.S., Righesso, L. et al. Effects of an oral bisphosphonate and three intravenous bisphosphonates on several cell types in vitro. Clin Oral Invest 22, 2527–2534 (2018). https://doi.org/10.1007/s00784-018-2349-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-018-2349-6