Abstract
Objectives
The aim of the present study was to evaluate the bonding effectiveness of two resin core buildup systems using conventional methods in the field of adhesive dentistry and a new non-destructive method.
Materials and methods
Twenty-four single-rooted human teeth were built up with dual-cure one-step self-etch adhesive and composite systems (SY1: Clearfil DC bond and Clearfil DC core automix, SY2: Clearfil bond SE one and Clearfil DC core automix one). The prepared samples were sectioned into approximately 1 × 1-mm-thick beams and subjected to micro-tensile bond strength (μTBS) testing (n = 24). The fractured beams after μTBS testing were analyzed by SEM and energy-dispersive X-ray (EDX) spectrometry. The three teeth filled with each resin core system were sectioned and embedded in epoxy resin to observe the dentin–bonding interface under TEM (n = 6). Moreover, three of each resin core-filled teeth without any processing were examined using μCT (n = 6).
Results
Two-way ANOVA revealed that the two factors “root region” (p < 0.001, F = 15.22) and “system” (SY1 < SY2; p < 0.001, F = 22.52) had a significant influence. The μTBS gradually decreased from the coronal side to the apical side of the root canal. Morphological evaluation revealed that SY2 was superior in terms of resin curing at the apical side. μCT non-destructive evaluation clearly revealed gap formation in SY1.
Conclusion
SY2, which included a new light-independent catalyst, showed better bonding effectiveness and adhesive interface to dentin compared to that of SY1.
Clinical relevance
The new catalyst, which is activated by contact with adhesive and resin composite, can be used for resin core buildup restorations.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Since the 1990s, resin core buildup systems have been employed more frequently to restore endodontically treated teeth that are extensively broken down. The major advantage of resin core materials is their elastic moduli which are similar to dentin [1], producing a stress field similar to that of natural teeth and reducing the risk of root fracture and subsequent tooth extraction [2, 3], whereas cast metal post and core restorations exhibit high stress concentration at the post-dentin interface [4]. Some clinical studies also showed that the survival rate of direct resin core restorations with prefabricated post was significantly higher than that of cast metal core [5]. On the other hand, post debonding has emerged as the most frequent failure mode of resin core buildup restorations in the clinical setting [6]. Various reasons for failure have been pointed out. For example, bonding to root canal dentin is hampered by limited visibility, morphological characteristics [7], unfavorable conditions regarding the application of adhesive techniques [8], and a comparably high configuration factor inside the root canal [9].
Previously, our research group had evaluated the bonding effectiveness of one resin core buildup system bonded to root canal dentin in terms of micro-tensile bond strength (μTBS) and interfacial characterization [10]. The study revealed that the bond strength gradually decreased from the coronal to the apical sides of the root canal, and morphological observation clarified that polymerization and moisture control at the apical portion of the root canal were insufficient. The degree of polymerization of the adhesive resin may decrease because the accessibility of light energy passing through the deep and narrow post space is low [11, 12]. To address this concern, dual-cure adhesives are generally used for bonding to root canal dentin, owing to their ability to self-polymerize even if light is absent. Nevertheless, it has been reported that dual-cure resins have lower bond strength compared with light-cured resins [13]. Recently, a new catalyst which is light-independent was introduced. The catalyst is activated by contact with adhesive and resin composite. With this system, the adhesion to the root canal dentin might be more sufficient, but there are few reports about the bonding effectiveness of the system.
Measuring μTBS is the major test to detect bonding effectiveness of adhesives in the field of adhesive dentistry. This method has a higher discriminative power than other testing methods, such as shear testing [14]. However, pre-testing failure (PTF; fracture of specimen before testing) may occur in μTBS test when the bonding interfaces are mechanically weak. This finding suggests that artifacts can easily develop during morphological observation of the same material set. Micro-computed tomography (μCT) has been introduced as a “non-destructive” method in recent years [15–17]. The greatest advantage of μCT is that samples are not subjected to any load during sample preparation. Therefore, this new non-destructive evaluation approach using μCT can also be applied in the field of adhesive dentistry.
The aim of the present study was to evaluate the adhesion between two different dual-cure resin core materials and dentin using conventional methods and non-destructive observation using μCT. The established null hypothesis was that there is no difference in the bonding effectiveness between the two different systems, and this was tested by (1) Measuring the μTBS to root dentin, (2) characterizing the interfacial interaction with root dentin using electron microscopy, and (3) non-destructive observation of the dentin–resin interface and root canal inside.
Materials and methods
Tooth preparation and resin core buildup
Thirty-six single-rooted human teeth including incisors and premolars were used in the present study. All teeth were extracted due to periodontal or orthodontic reasons and stored in Hank’s balanced salt solution (HBSS) at 4 °C. The experimental protocol was approved by the Ethics Committee of the Osaka University Faculty of Dentistry.
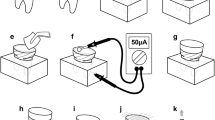
The experimental setup is schematically presented in Fig. 1. The crown of each tooth was cut at the cementoenamel junction using a low-speed diamond wheel saw under water-cooling. Root canals were endodontically instrumented by means of K-file (K-file, MANI, Tochigi, Japan). Each canal was finally shaped with a size 80-K file to the working length and obturated by lateral condensation using gutta-percha points and non-eugenol sealer (Canals N, Showa Yakuhin Kako, Tokyo, Japan). The teeth were then stored in distilled water at 37 °C for 24 h. After immersion, the root canals were enlarged with low-speed preparation drills (Tokuyama FR drill, Tokuyama Dental, Tokyo, Japan) to a working length of 10 mm from the cementoenamel junction. Then, the canal surfaces were precisely checked by optical microscope. Following preparation, the canals were rinsed with 3 % EDTA solution (Smear Clean, Nipponshika Yakuhin, Yamaguchi, Japan) for 2 min and 10 % sodium hypochlorite gel (AD gel, Kuraray Noritake, Tokyo, Japan) for 1 min. The canals were finally irrigated with distilled water and then dried well with paper points.
Schematic illustration of the resin core buildup and testing procedures. a The crown was removed. b The root canal was prepared and obturated. c The root canal was enlarged. d The adhesive was applied and light cured. The post space was filled with dual-cure resin composite core material. e The specimen was stored in water for 24 h at 37 °C
Two kinds of dual-cure one-step self-etch adhesive systems were used in this study and the materials used for post-core restorations are listed in Table 1. One system was the set of Clearfil DC bond (Kuraray Noritake) and Clearfil DC core automix (Kuraray Noritake) referred to as system 1 (SY1), and the other system was the set of Clearfil bond SE one and Clearfil DC core automix one (Kuraray Noritake) referred to as system 2 (SY2). In handling these materials, the manufacturer’s instructions were followed (Table 1). After the bonding procedure, excess adhesive resin at the bottom of the canal was removed using a paper point. The adhesive was light-cured for 20 s with a cordless light-emitting diode curing light (Mini LED3, SATELEC, Merignac, France) which had a maximal light density of 2200 mW/cm2. Then, the prepared post spaces were filled with dual-cure resin composite. The tip of the filling nozzle was inserted to the bottom of the post space, and composite core material was injected carefully without removing the tip from the material. Care was taken to avoid entrapment of bubbles. The coronal surface of the root was covered with plastic strips to squeeze out any excess resin. The specimens were light-cured for 40 s and then stored in water for 24 h at 37 °C.
μTBS test
Twenty-four teeth, 12 teeth in each system, were sectioned perpendicular to the long axis into a series of 1-mm-thick slices under water-cooling, and six slabs were obtained from each tooth. Then, each slice was transversely sectioned through the middle part of the post space into approximately 1 × 1-mm-thick beams. The cross-sectional area of each beam was measured using digital calipers (Mitsutoyo CD15, Mitsutoyo, Tokyo, Japan). The beams were attached to a jig using cyanoacrylate glue (Model repair, Dentsply Sankin, Tokyo, Japan) and subjected to tensile force at a crosshead speed of 1 mm/min using a table top testing machine (EZ test, Shimadzu, Kyoto, Japan). The values of bond strength, initially in kilogram-force per square millimeter, were calculated to millipascal. PTF samples were included as the data of 0 MPa.
The μTBS data were analyzed using two-way ANOVA and Scheffé’s method. All statistical analyses were performed at a 95 % level of confidence with SPSS IBM version 21.0.
SEM observation and EDX analysis
After μTBS testing, the fractured beams (both dentin and resin sides) were mounted with carbon adhesion tape on a specimen holder to check the dentin–bonding interface. The samples were then coated with osmium to 5-nm thickness. Then, they were analyzed with a field-emission scanning electron microscope (SEM, S5200, Hitachi, Tokyo, Japan) and energy-dispersive X-ray spectrometry (EDX, GENESIS, EDAX Japan, Tokyo, Japan) at an accelerating voltage of 20 kV and magnification of ×1500–2500.
TEM observation
Six teeth filled with resin core systems, three teeth for each system, were serially sectioned perpendicular to the long axis into 400-μm-thick slices under water-cooling. Then, each slice was additionally sectioned into small blocks involving the dentin–bonding interface and fixed in 4 % paraformaldehyde and 5 % glutaraldehyde overnight. Samples were then dehydrated in a graded ethanol series and embedded in epoxy resin (Quetol812 NissinEM, Tokyo, Japan). The embedded specimens were sectioned to 70–90-nm thickness using a diamond knife (Nanotome thick, Sakai Advanced Electron Microscope Research Center, Saitama, Japan) on an ultramicrotome (Ultrotome V, LKB, Stockholm, Sweden). The sections were mounted on copper grids and observed using a transmission electron microscope (TEM, H-800, Hitachi) at an accelerating voltage of 200 kV.
Non-destructive μCT observation
Six teeth filled with resin core systems, three teeth for each system, were prepared. Then, the root-filled teeth were observed by micro-focus X-ray CT system (SMX-100CT-SV3, Shimadzu) without any processing. The μCT operated at 65 kV of tube voltage and 32 μA of tube current. Picture size was 512 × 512 pixels, and the pixel equivalent length of the image was 7.8 μm/pixel.
Results
μTBS test
Two-way ANOVA revealed that the two factors “root region” (p < 0.001, F = 15.22) and “materials” (p < 0.001, F = 22.52) had a significant influence (Fig. 2). Six slices were obtained from each tooth; the edge of the coronal side was indicated as no. 1, and the edge of the apical side was indicated as no. 6. The μTBS gradually decreased from the coronal side to the apical side of the root canal. There was no significant difference between nos. 1 and 2 (p = 0.18), nos. 2 and 3 (p = 0.094), and nos. 3, 4, 5, and 6 (p = 0.99 ∼ <1.00). Regarding materials, the bond strength of SY2 was significantly higher than that of SY1 (p = 0.003).
Similar tendencies were clearly seen in the number of PTF. The PTF increased on the apical side of the root canal (no. 1: 0/24, no. 2: 3/24, no. 3: 5/24, no. 4: 9/24, no. 5: 10/24, no. 6: 7/24), and SY1 group had more PTF than SY2 group (SY1: 21/72, SY2: 13/72).
SEM observation and EDX analysis, TEM observation
SEM observation of the post-μTBS test specimens revealed the difference between SY1 and SY2. Resin core material existed on the dentin surface of SY1 and penetrated into the dentinal tubules; on the other hand, the bonding layer could be seen on the dentin surface of SY2 and no composite resin existed in the dentinal tubules (Fig. 3a). The same tendency could be confirmed with the results of elemental analysis performed by EDX. Barium (i.e., core material) was identified inside dentin tubules in SY1, but it was not detected in any of the SY2 specimens (Fig. 3b, c). Such differences between SY1 and SY2 were detected more at the apical side compared to the coronal side.
Morphological evaluation of the dentin–bonding composite interface using SEM, EDX, and TEM. a SEM image of dentin–SY2 interface after the μTBS test. The dentin surface was covered with a bonding layer. b EDS element mapping of C, O, Si, and Ca; images were taken from the same spot of a. c EDX spectrum of spot a; barium (i.e., core material, see Table 1) was not detected, contrary to its presence in SY1 (see Fig. 3 of ref. 10). d Dentin–bonding composite interface of SY1; the coronal side of the post space, disclosing a tight, void, and gap-free interface. e, f The apical side of the post space of SY1; a lot of bubbles in the bonding layer and gap formation between dentin and bonding layer were observed. g Typical TEM image of SY2 specimen; the bonding filler penetration into dentinal tubule can be seen. B bonding layer, Bu bubble, CR composite resin, D dentin, DT dentinal tubule, G gap
For TEM observation, over all, since the canals were treated with EDTA solution and sodium hypochlorite gel, smear layer and plug did not exist on the dentin–bonding interface. At the coronal side, a tight, void, and gap-free interface with bonding permeation into dentinal tubules was observed in both systems SY1 and SY2 (Fig. 3d, 3g). On the contrary, numerous bubbles in the bonding layer and the interface were observed on the apical side in SY1 (Fig. 3e). Moreover, a gap was detected between the dentin and bonding layer in SY1 (Fig 3f).
Non-destructive μCT observation
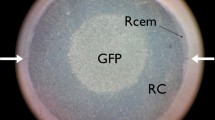
Gaps were observed at the bottom of the post space in SY1 sample (Fig.4a, b). On the other hand, resin core materials almost closely filled the whole post space in the SY2 sample (Fig 4c, 4d). Some bubbles were detected inside the resin composite in both SY1 and SY2 samples. The SY1 had more gaps compared to SY2 at the adhesive interface. The gap formations varied in location or width even in the same slice.
Non-destructive evaluation of the resin core material bonded to post-space dentin using μCT. a μCT overview image of SY1 sample; gaps were observed at the bottom of the post space and some bubbles were detected inside the resin composite. b1–4 Cross-sectional image of a; gaps were clearly observed. c μCT overview image of SY2 sample; resin core materials were closely filled in the post space but some bubbles were detected inside the resin composite. d1–4 Cross-sectional image of f; resin core materials closely filled the whole post space. Bu bubble, CR composite resin, D dentin, G gap, GP gutta–percha point
Discussion
The bonding effectiveness of two direct buildup resin core systems was mechanically evaluated by μTBS test, and the findings of this study were as follows: (1) bonding effectiveness gradually decreased from the coronal side to the apical side of the root canal and (2) bonding effectiveness of SY2 was significantly higher than that of SY1. The null hypothesis that there was no difference in the bonding effectiveness between the two different systems was rejected. The most common methods for detecting bonding effectiveness to root dentin are micro-tensile [18, 19], push-out tests [20], or pull-out tests. [21]. As the evaluation area of pull-out and push-out test samples is larger than micro-tensile samples, the micro-tensile test is more desirable to assess the mutual interaction between mechanical strength and morphological characteristics. Moreover, the micro-tensile test appeared to have a larger discriminative power than the other tests [14]. Therefore, we conducted a micro-tensile test to evaluate the bond strength between resin core materials and post-space dentin. Insertion of a post in post space is a common procedure in the clinical situation. However, using posts doubles the number of adhesive interfaces (i.e., dentin–resin and resin–post), so it would be difficult to focus solely on the interface between dentin and resin core materials. Hence, we decided not to use a post in this study.
This study revealed the reduction of μTBS from the coronal side to the apical side in both systems. We have reported this bond strength reduction when using SY1 in a previous study [10]. Some studies also reported that the reduction of bond strength can be attributed to various factors such as the less dense dentinal tubular configuration in the apical portion of the root canal system [22], apical sclerosis, the cavity configuration factor [7], the difficulty of visualization and access to the apical part of the root canal as well as restricted flow of the resin core materials [23]. SEM observation and EDX analysis revealed that core material penetrated into the dentinal tubules without bonding layer formation in SY1. This fact suggested that the bonding layer was not sufficiently cured in SY1 as reported previously [10]. TEM observation of SY1 indicated the existence of another inhibition factor of adhesive on the apical side, namely there were lots of bubbles in the bonding layer (Fig. 3e) and gap formation between dentin and bonding layer (Fig. 3f) at the apical side. These bubbles were considered to arise from residual water at the bottom of the post space. We used paper points and air blow to dry the post space, but the drying method might have been inadequate. On the other hand, favorable adhesive conditions were observed at the coronal side of SY1 and both sides of SY2 (Fig. 3d, 3g).
Different from our previous study, we examined two sets of resin core buildup systems. Interestingly, the bond strength of SY2 was significantly higher than that of SY1. Some studies reported that micro-tensile outcome differed depending on the variety of the composite resin [24, 25]. This is because the μTBS is affected by a difference in filler content followed by polymerization shrinkage. However, both bonding agents used in this study include the same 10-methacryloyloxydecyl dihydrogen phosphate (MDP) compound and also both composite resins possess almost the same filler content. Hence, it can be considered that the influence of the disparity of materials on bond strength would be minimal. There were differences between SY1 and SY2 in some aspects. First of all, the bonding agent of SY2 contained a newly developed catalyst, which promotes polymerization of bonding in SY2 more than that in SY1 with the same amount of light. In the present study, SEM observation and EDS analysis clearly showed a bonding layer on the dentin surface of the SY2 apical side specimen (Fig. 3a), which suggests that the curing of bonding layer in SY2 is better than that of SY1 as previously reported [10]. Second, SY2 contains an active ingredient. The “accelerators” are mainly responsible for the polymerization in SY2. The bonding agent includes a chemical cure accelerator that is stable even when it is under acidic environment. And, the composite resin (paste B) includes another newly developed accelerator that can promote polymerization of MDP in the bonding layer. Both the accelerators promote the interface polymerization between the bonding layer and composite resin. These characteristics may explain the better action of SY2. We had previously suggested that the main reason for the lower bonding effectiveness in the apical region of the post space is insufficient light energy [10]. Some studies reported that the curing mode did not affect the bond strength, as no differences in μTBS were observed when dual-cure adhesive was either light-activated or chemical-cured [26]. But other studies have demonstrated chemical cure alone in dual-cure adhesives exhibited lower bond strength than when photo-cured [27]. Furthermore, another study suggested that sufficient light energy resulted in higher bond strength to dentin because the double-bond conversion of resin monomers in the adhesive may be enhanced following polymerization reaction [28]. As for the third difference between SY1 and SY2, the bonding agent of SY2 consists of a one bottle type of adhesive, so-called all-in-one adhesive; on the other hand, the agent for SY1 is mixed from two bottles. Since there is no need to mix the agent in SY2, it might reduce the technical error. A previous study also reported that reducing operative procedures makes the one-step systems more effective in minimizing technique sensitivity than two-step systems [29]. Thus, SY2 is superior in the abovementioned three material characteristics, and these might contribute to the higher bond strength of SY2.
The bonding potential of ‘mild’ self-etch adhesives may be compromised due to smear interference, as they may not dissolve/penetrate the smear layer effectively due to their relatively low acidity [30]. In the present study, EDTA solution and sodium hypochlorite gel were used for dentin pre-treatment. This means that smear layer and demineralized dentin would be absent on dentin surface, and TEM observation revealed adhesive and/or core resin filler penetration in dentin tubules. Dentin pre-treatment results in better bonding effectiveness and also simplifies the dentin-bonding interface observation. Moreover, the experiment was conducted without post insertion to focus on what happens at the interface between dentin and resin. Post insertion as in the real clinical situation results in a small amount of core material, and shrinkage stress could be small.
PTF is one of the most serious problems encountered in the μTBS testing method. The test involves a cutting process (in other words “destructive” procedure) during specimen preparation. In both previous and present studies, many PTF samples were obtained especially on the apical side of SY1. There is some debate over whether the PTF samples should be included in data as 0 MPa [18, 31] or the lowest value, or be eliminated from the data [19, 32] and we adopted it as 0 MPa. Including the PTF samples’ value into data analysis could make up the number, and handling these data as 0 MPa is the severest outlook [32, 33]. Not only mechanical evaluation but also morphological evaluation also might result in artifacts if the specimen has a fragile interface. Basically, we cannot have a perfect intact image because specimen preparation for interface analysis involves a destructive procedure. Therefore, destructive evaluation needs adequate bond effectiveness and morphological evaluation of resin–tooth interface can be considered to be a kind of bond strength test.
The μCT helps to observe the overall length of post spaces. It is also possible to figure out the total image of the root canal and evaluate the condition of the core materials. The greatest advantage of μCT observation is that samples are not subjected to any load during specimen preparation. Therefore, μCT observation enables evaluation of this weak adhesion part as in PTF samples. There were lots of bubbles inside the composite resin and obvious space between the core materials and the dentin at the bottom of post space. In this situation, it is difficult to evaluate this part by using μTBS, SEM, or TEM. Thus, using μCT would be effective and innovative.
The difference in quality between two different resin core buildup systems was confirmed in this study. As we mentioned previously, a matter of concern with resin core materials is “debonding.” Today, many practitioners strive to overcome this problem, giving extra care to avoid failures such as development of fracture and/or extrusion of root and investing longer posts or extra preparation to get better fit of core materials. The long post makes impression taking difficult, and the risk of perforation of tooth substance becomes higher when the core material has to be removed for retreatment of root canal. Well-established adhesion of root canal dentin is equivalent to realization of short post or no post at all. Within the limits of this study, it is still difficult to state whether this would be possible. Further investigations regarding adhesion in post-space dentin are thus required.
Conclusion
• Bonding effectiveness of two direct buildup resin core systems was mechanically evaluated by μTBS test. It was shown that (1) bonding effectiveness gradually decreased from the coronal side to the apical side of the root canal and (2) bonding effectiveness of SY2 was significantly higher than that of SY1.
• Morphological evaluation revealed that SY2 including a new catalyst is superior in terms of bonding resin curing on the apical side.
• μCT non-destructive evaluation clearly revealed the gap and bubble formation in the post core space without any invasion.
References
Asmussen E, Peutzfeldt A, Heitmann T (1999) Stiffness, elastic limit, and strength of newer types of endodontic posts. J Dent 27:275–278
Pegoretti A, Fambri L, Zappini G, Bianchetti M (2002) Finite element analysis of a glass fibre reinforced composite endodontic post. Biomaterials 23:2667–2682
Matsuda K, Ikebe K, Enoki K, Tada S, Fujiwara K, Maeda Y (2011) Incidence and association of root fractures after prosthetic treatment. J Prosthodont Res 55:137–140
Isidor F, Odman P, Brondum K (1996) Intermittent loading of teeth restored using prefabricated carbon fiber posts. Int J Prosthodont 9:131–136
Hikasa T, Matsuka Y, Mine A, Minakuchi H, Hara ES, Van Meerbeek B, Yatani H, Kuboki T (2010) A 15-year clinical comparative study of the cumulative survival rate of cast metal core and resin core restorations luted with adhesive resin cement. Int J Prosthodont 23:397–405
Rasimick BJ, Wan J, Musikant BL, Deutsch AS (2010) A review of failure modes in teeth restored with adhesively luted endodontic dowels. J Prosthet Dent 19:639–646
Mjor I, Nordahl I (1996) The density and branching of dentinal tubules in human teeth. Arch Oral Biol 41:401–412
Serafino C, Gallina G, Cumbo E, Ferrari M (2004) Surface debris of canal walls after post space preparation in endodontically treated teeth: a scanning electron microscopic study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 97:381–387
Tay FR, Loushine RJ, Lambrechts P, Weller RN, Pashley DH (2005) Geometric factors affecting dentin bonding in root canals: a theoretical modeling approach. J Endod 31:584–589
Matsumoto M, Miura J, Takeshige F, Yatani H (2013) Mechanical and morphological evaluation of the bond–dentin interface in direct resin core build-up method. Dent Mater 29:287–293
Wu H, Hayashi M, Okamura K (2009) Effects of light penetration and smear layer removal on adhesion of post-cores to root canal dentin by self-etching adhesives. Dent Mater 25:1484–1492
Goracci C, Corciolani G, Vichi A, Ferrari M (2008) Light-transmitting ability of marketed fiber posts. J Dent Res 87:1122–1126
Foxton RM, Nakajima M, Tagami J, Miura H (2003) Bonding of photo and dual-cure adhesives to root canal dentin. Oper Dent 28:543–551
Munck D, Mine A, Poitevin A, Van Ende A, Cardoso MV, Van Landuyt KL, Peumans M, Van Meerbeek B (2012) Meta-analytical review of parameters involved in dentin bonding. J Dent Res 91:351–357
Meleo D, Manzon L, Pecci R, Zuppante F, Bedini R (2012) A proposal of microtomography evaluation for restoration interface gaps. Ann Ist Super Sanita 48:83–88
Huang SH, Lin LS, Rudney J, Jones R, Aparicio C, Lin CP, Fok A (2012) A novel dentin bond strength measurement technique using a composite disk in diametral compression. Acta Biomater 8:1597–1602
Yun X, Li W, Ling C, Fok A (2013) Effect of artificial aging on the bond durability of fissure sealants. J Adhes Dent 15:251–258
Bouillaguet S, Troesch S, Wataha JC, Krejci I, Meyer JM, Pashley DH (2003) Microtensile bond strength between adhesive cements and root canal dentin. Dent Mater 19:199–205
Aksornmuang J, Nakajima M, Foxton RM, Tagami J (2006) Effect of prolonged photo-irradiation time of three self-etch systems on the bonding to root canal dentin. J Dent 34:389–397
Zicari F, De Munck J, Scotti R, Naert I, Van Meerbeek B (2012) Factors affecting the cement-post interface. Dent Mater 28:287–297
Ebert J, Leyer A, Günther O, Lohbauer U, Petschelt A, Frankenberger R, Roggendorf MJ (2011) Bond strength of adhesive cements to root canal dentin tested with a novel pull-out approach. J Endod 37:1558–1561
Mjör IA, Smith MR, Ferrari M, Mannocci F (2001) The structure of dentine in the apical region of human teeth. Int Endod J 34:346–353
Zicari F, Couthino E, De Munck J, Poitevin A, Scotti R, Naert I, Van Meerbeek B (2008) Bonding effectiveness and sealing ability of fiber-post bonding. Dent Mater 24:967–977
Miyazaki M, Hinoura K, Onose H, Moore BK (1991) Effect of filler content of light-cured composites on bond strength to bovine dentine. J Dent 19:301–303
Ilie N, Kunzelmann KH, Hickel R (2006) Evaluation of micro-tensile bond strengths of composite materials in comparison to their polymerization shrinkage. Dent Mater 22:593–601
Okuma M, Nakajima M, Hosaka K, Itoh S, Ikeda M, Foxton RM, Tagami J (2010) Effect of composite post placement on bonding to root canal dentin using 1-step self-etch dual-cure adhesive with chemical activation mode. Dent Mater J 29:642–648
Thitthaweerat S, Nakajima M, Foxton RM, Tagami J (2012) Effect of waiting interval on chemical activation mode of dual-cure one-step self-etching adhesives on bonding to root canal dentin. J Dent 40:1109–1118
Shimizu Y, Tsujimoto A, Furuichi T, Suzuki T, Tsubota K, Miyazaki M, Platt JA (2014) Influence of light intensity on surface free energy and dentin bond strength of core build-up resins. Oper Dent 39:1–9
Toledano M, Osorio R, de Leonardi G, Rosales-Leal JI, Ceballos L, Cabrerizo-Vilchez MA (2001) Influence of self-etching primer on the resin adhesion to enamel and dentin. Am J Dent 14:205–210
Mine A, De Munck J, Cardoso MV, Van Landuyt KL, Poitevin A, Ende AV, Matsumoto M, Yoshida Y, Kuboki T, Yatani H, Van Meerbeek B (2014) Dentin-smear remains at self-etch adhesive interface. Dent Mater 30:1147–1153
Wang YJ, Raffaelli O, Zhang L, Chen JH, Ferrari M (2007) Effect of different bonding procedures on micro-tensile bond strength between a fiber post and resin-based luting agents. J Oral Sci 49:155–160
Mine A, De Munck J, Cardoso MV, Van Landuyt KL, Poitevin A, Kuboki T, Yoshida Y, Suzuki K, Lambrechts P, Van Meerbeek B (2009) Bonding effectiveness of two contemporary self-etch adhesives to enamel and dentin. J Dent 37:872–883
Mine A, De Munck J, Cardoso MV, Van Landuyt KL, Poitevin A, Kuboki T, Yoshida Y, Suzuki K, Van Meerbeek B (2012) Effect of low-shrinking composite on the bonding effectiveness of two adhesives in occlusal class-I cavities. Dent Mater J 31:418–426
Acknowledgments
This work was supported by KAKENHI Grant-in Aid for Scientific Research (B) (26293410). The authors would like to express our gratitude to Kuraray Noritake Dental for the generous donation of materials, and, in part, by the Nanotechnology Platform of the Ministry of Education, Culture, Sports, Science and Technology (MEXT) at the Research Center for Ultra-High Voltage Electron Microscopy, Osaka University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors. The use of extracted human teeth was approved by the ethical committee of the Osaka University Faculty of Dentistry.
Conflict of interest
The authors declare that they have no conflicts of interest.
Funding
This work was supported by KAKENHI Grant-in Aid for Scientific Research (B) (26293410).
Informed consent
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Matsumoto, M., Mine, A., Miura, J. et al. Bonding effectiveness and multi-interfacial characterization of two direct buildup resin core systems bonded to post-space dentin. Clin Oral Invest 21, 309–317 (2017). https://doi.org/10.1007/s00784-016-1792-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-016-1792-5