Abstract
Objectives
To evaluate the effect of electric current application on the resin composite-tooth bond strength and hybrid layer of three adhesive systems light-cured by two light-curing units (LCUs).
Materials and methods
Human molar teeth were distributed into 12 groups (n=6). Three adhesive systems were used: two-step etch-and-rinse (SB2; Adper Single Bond 2, 3M ESPE); two-step self-etch (CSE; Clearfil SE Bond, Kuraray); and one-step self-etch (SBU; Single Bond Universal, 3M ESPE) applied with (50μA) and without (control; conventional application) electric current, and light-cured with different LCUs. Resin composite blocks (Filtek Z350XT, 3M ESPE) were produced and cut into sticks (~1mm2) for microtensile bond strength (μTBS). Fracture patterns were analyzed on stereomicroscope and classified as cohesive-dentin, cohesive-resin, adhesive, or mixed. Specimens were prepared for scanning electron microscope observation. The hybrid layer analysis was carried out using a confocal laser scanning microscopy (n=2). Data were submitted to three-way ANOVA followed by Tukey’s post hoc test (α=0.05).
Results
The electric current increased the μTBS for all adhesive systems light-cured with single-emission peak and multiple-emission peak LCUs. Both LCUs presented similar μTBS values. CSE applied under electric current showed the highest μTBS mean values. The adhesive failure pattern was more frequently observed in all groups. The electric current formed long resin tags for all adhesive systems.
Conclusions
The adhesive systems applied under electric current increased the bond strength using single-emission peak and multiple-emission peak LCUs.
Clinical relevance
Electric current at 50μA applied throughout the dentin is a safe mode and results in better impregnation of the adhesive systems.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The dentin adhesion to resin composite has been a challenge to clinical procedures because the complexity of the molecular structure of the dentin [1]. The adhesive restoration failures are due to the incomplete penetration of resin monomers into demineralized collagen network. After phosphoric acid etching, the demineralized dentin must be filled by resin monomers in order to form a homogeneous hybrid layer and provide high bond strength. Otherwise, the matrix metalloproteinases (MMP) degrades the demineralized collagen fibers not infiltrated by the monomers, which promotes the destruction of the hybrid layer and loss of adhesion [2].
In the attempt to increase the bond strength, some procedures are used to improve the impregnation of the resin monomers into dentin, such as additional phosphoric acid etching in self-etch adhesive systems [3], use of one extra layer [4], application of multiple layers of hydrophobic adhesive [5], dentin pre-treatment with cross-linkers [6], and laser irradiation on dentin [7]. However, all of these procedures increase the number of clinical steps as well as the sensitivity of the restorative technique [8].
An electrical device has been developed to improve the application of adhesive systems using electric current [9] without increasing the number of clinical steps [8, 10,11,12,13]. However, there are previous studies [8, 10,11,12,13] evaluating the electric current parameters, and these studies present divergences, especially regarding the materials and methods (adhesive systems, curing lights, adhesion protocols, and so forth). Furthermore, there is no standardization about the intensity of the electric current that should be applied on tooth to ensure improvement in bond strength. The structure of the dentin (organic and inorganic matter, and water) is heterogeneous [1, 2, 8]. Thus, there are zones in the dentin with different electrical resistances, and, consequently, the intensity of the electric current applied on dentin may change [14, 15]. It should be important guarantee that the electric current applied is equally distributed (standardized) along the entire dentin.
Curing lights are also related to quality of the hybrid layer and bond strength [16], since the longevity of adhesive restorations depends on the photoinitiators and light-curing unit (LCU) [17]. The camphorquinone is the most commonly used photoinitiator in resin materials. It is compatible with wavelengths of blue light (~468nm) emitted by single-emission peak light-emitting diode (LED) LCU [17, 18]. The development of alternative photoinitiator systems changed the photoexcitation of some resin materials, requiring LCUs with a light emission spectrum ranging from 320 to 410nm. The multiple-emission peak LED LCU emits a main wavelength (blue light; ~460nm) and an additional peak (violet light; ~400nm) [19]. Furthermore, the irradiance is also important to the polymerization quality of the resin materials. When the irradiance of the LCU is ineffective, insufficient adhesive polymerization provides the build-up of residual monomers which, in addition to the cytotoxic action in the dentin-pulp complex, may lead to adhesive restoration failure [20, 21].
Thus, the aim of this study was to evaluate the microtensile bond strength (μTBS) and the hybrid layer quality of different adhesive systems applied on dentin using a standardized electric current and light-cured with two LUCs (single-emission peak and multiple-emission peak). The hypotheses would be that (i) constant electric current (50μA) promotes higher μTBS than conventional application, (ii) the adhesive systems tested show similar μTBS, and (iii) multiple-emission peak LCU has higher μTBS than single-emission peak LCU.
Materials and methods
Sample size calculation
This in vitro study involved a 3×2×2 factorial design. The factors were the type of the adhesive system (three levels: two-step etch-and-rinse, two-step self-etch, or one-step self-etch), application mode (two levels: conventional or electric current), and LUCs used (two levels: single-emission peak and multiple-emission peak). The sample size was calculated using α of 0.05 and power of 90%. The minimal sample size was 6 teeth for each group to μTBS test.
Sample preparation
Ninety six molars extracted for therapeutic reasons with complete root formation and no presence of caries or restorations were stored in distilled water at 4°C for utilization within 6 months after approval from the Ethics Committee (protocol: 94744218.3.1001.5501).
Teeth were sectioned 3.0mm above the cement-enamel junction from mesial surface to obtain a flat and deep dentin surface using a low-speed water-cooled diamond saw (IsoMet 1000, Buehler, Lake Bluff, IL, USA). Teeth with exposed pulp chamber were discarded. The coronal flat dentin surface was ground with wet 600-grit sandpaper for 30s to create a standardized smear layer.
Dentin samples were randomly divided into three main groups according the adhesive systems (SB2, Adper Single Bond 2, 3M ESPE, St. Paul, MN, USA; CSE, Clearfil SE Bond, Kuraray, Okayama, Japan; SBU, Single Bond Universal, 3M ESPE) (Table 1). The samples were divided into four subgroups regardless the mode of application of the adhesive systems (control, without electric current/conventional mode; experimental, with electric current set in 50μA) and the LCU (single-emission peak, Radii-cal, SDI, Victoria, Australia; multiple-emission peak, VALO Cordless, Ultradent, South Jordan, UT, USA). The light irradiance was measured and kept at 800mW/cm2 (single-emission peak LCU; 11.65mm diameter tip) and 1600mW/cm2 (multiple-emission peak LCU; 13.1-mm-diameter tip) using a radiometer (RD-7, ECEL, Ribeirão Preto, SP, Brazil).
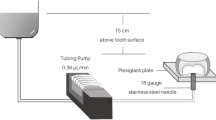
The samples were placed on moist sponges in order to simulate the moisture of the periodontal conditions [8, 22] and to create an electric circuit. The sponge-dentin sample set was connected to the experimental electric current device. The negative pole (cathode) and positive pole (anode) were attached to the sponge and to the tooth, respectively, creating an electric circuit. A micro brush was coupled to positive pole tip. Before the application of adhesive systems with the positive pole tip, the electric current was set in 50μA. This intensity of the electric current improve safely [15] the penetration of the adhesives into dentin. During the application of adhesive systems, at the same time, the experimental device measured the electrical resistance of each region of the dentin sample and delivered a standard electric current in the whole dentin surface. Before SB2 application, dentin surface was acid etched using phosphoric acid 35% (Ultra-Etch, Ultradent, South Jordan, UT, USA) for 15s. The application of adhesive systems occurred according to manufacturers’ recommendations, under constant electric current (50μA) (Table 1). For SB2, both two coats were applied under electric current. In CSE, the electric current was applied to adhesive. The micro brush coupled to positive pole tip was changed for each sample. For control groups, the adhesives were applied using the same tip but with the experimental device turned off (0μA) (Fig. 1). The light-curing of the adhesives was performed for 20s by single-emission peak LCU (800mW/cm2) and 10s by multiple-emission peak LCU (1,600mW/cm2), standardizing the radiant exposure in 16J/cm2 (800mW/cm2 × 20s and 1600mW/cm2 × 10s = 16,000mWs/cm2 or 16J/cm2). LCUs were kept as close as possible to the dentin surface.
Schematic illustration of the adhesive systems applied on dentin using electric current (50μA) for μTBS test. a Tooth; b tooth sectioned 3.0mm above the cement-enamel junction; c sample placed on moist sponge; d phosphoric acid etching (SB2 group); e remove the excess of water; f application of adhesive system (SB2, CSE and SBU groups) under constant electric current (50μA); g sample restored with resin composite; h removal of the root; i filling the pulp chamber with resin composite; j sample sectioned to obtain bar-shaped stick (~1mm2); and k stick submitted to microtensile bond strength test
Samples were restored with two 2.0-mm increments of nanofilled resin composite (Filtek Z350 XT, shade A1E, 3M ESPE, St. Paul, MN, USA). Each increment of resin composite was light-cured using the same LCUs for the respective time for each LCU mentioned for the adhesives. The samples were stored in distilled water for 24h at 37°C.
Microtensile bond strength
Each sample was sectioned to obtain dentin-resin composite rectangular bar-shaped stick (~1mm2) using a low-speed water-cooled diamond saw (IsoMet 1000, Buehler). The adhesive area is measured using a digital caliper (King Tools 150mm/6”, São Paulo, SP, Brazil). The sticks were analyzed in a stereomicroscope (×50; MZ75, Leica Microsystems, Wetzlar, Germany) to verify the defects occurred during sample cutting. These sticks were discarded. Sticks (~10 for each group) were stored in distilled water for 24h at 37°C.
After storage, the sticks were attached to jigs using cyanoacrylate glue (Loctite Super Bonder Power Flex Gel, Henkel, Rocky Hill, NY, USA) and catalyst spray (Zip Kicker, Zap, Rancho Cucamonga, CA, USA). The sticks were tested until failure in a universal testing machine (EZ Test, Shimadzu, Kyoto, Japan) using a 500N load cell at 1.0mm/min crosshead speed.
The adhesive area was measured (mm2) with a digital caliper (King Tools 150mm/6”). The μTBS was expressed in MPa following the equation: μTBS = F/A in which F is the force applied during the test (N) and A the sample bonded area (mm2).
Fracture pattern analysis
The fracture pattern were evaluated using a stereomicroscope (MZ75, Leica Microsystems) with ×50 magnification and classified as cohesive in dentin, cohesive in resin, adhesive (cohesive in adhesive or at adhesive interface), or mixed. Representative specimens from each fracture pattern were mounted in aluminum stubs, sputter coated with gold using a Desk II device (Denton Vacuum, Moorestown, NJ, USA) for 2 min. Then, the specimens were analyzed in scanning electron microscopy (SEM; JSM-5600LV, JEOL, Tokyo, Japan), operated under 15kV in different magnifications.
Confocal laser scanning microscopy interfacial characterization
Bonding restorative procedures were performed as described above; however, the adhesives were doped with 0.1wt% Rhodamine B (Sigma, St. Louis, MO, USA). Samples (n=2) were immediately placed in a container with a 0.1wt% aqueous solution of fluorescein (Sigma) for 3h, forming a 20cm column. After ultrasonic bath for 60s, the samples were sectioned into six 0.4-mm-thick mesio-distal slabs using a diamond saw (IsoMet 1000, Buehler) with constant distilled water irrigation. Each side of the resin composite-adhesive-tooth interface was slightly polished with 1200-grit sandpaper for 30s, followed by an ultrasonic bath for 60s [8]. The specimens were evaluated using a confocal laser scanning microscopy (Leica SP5, Leica Microsystems, Heidelberg, Germany).
Statistical analysis
The μTBS data were assessed for normality with the Kolmogorov-Smirnov test. The results were submitted to three-way ANOVA (adhesive system, application mode, and LCU) followed by Tukey’s post hoc test at the significance level of α=0.05. All statistical analyses were carried out using SPSS for Windows software (IBM SPSS Statistics 21).
Results
Three-way ANOVA revealed that only the LCU showed no significant influence in μTBS (ρ>0.05). However, the application mode as well as adhesive system showed significant influence in μTBS (ρ<0.05). There was a significant interaction between the three factors studied (ρ<0.01).
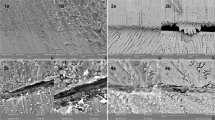
All adhesive systems applied under electric current showed significantly higher μTBS mean values than conventional mode when light-cured by single-emission peak and multiple-emission peak LCUs (ρ<0.05). For both LCUs, CSE and SB2 applied with electric current obtained the highest and the lowest μTBS mean values, respectively (ρ<0.05). SBU showed statistically similar μTBS values with CSE and SB2 (ρ>0.05). On other hand, all adhesive systems applied in conventional mode showed no statistical difference in μTBS values (ρ>0.05) (Table 2). Fracture pattern analysis predominantly presented adhesive failures for all groups (Fig. 2). Representative fracture patterns are presented in SEM images (Fig. 3).
SEM images depicting the fracture pattern analysis (15kV, ×80, 200μm). a Cohesive failure within the dentin, with the exposition of dentin tubules and remaining of residual adhesive; b cohesive failure within the resin composite; c adhesive failure, at adhesive interface; and d mixed failure (cohesive in dentin-CD, cohesive in resin-CR, and adhesive-AD)
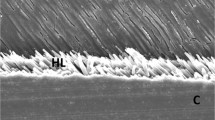
Confocal laser scanning microscopy images showed an improvement in the adhesive interface with the adhesive systems applied under electric current for both LCUs tested. All adhesive interfaces created with electric current showed greater adhesive infiltration into the dentin tubules with very dense formation of resin tags as well as in depth compared to conventional application mode. Despite the thickness of the hybrid layer, adhesives systems applied under electric current formed a pronounced hybrid layer throughout the adhesive interface. The hybrid layer formed by electric current groups was regular, uniform, and continuous with adhesive interface, without cracks/voids (Fig. 4).
Confocal laser scanning microscopy of the adhesive interface. a SB2 applied in conventional mode (0μA); b SB2 applied under electric current (50μA); c CSE applied in conventional mode (0μA); d CSE applied under electric current (50μA); e SBU applied in conventional mode (0μA); and f SBU applied under electric current (50μA). RT, resin tags; HL, hybrid layer; AD, adhesive layer
Discussion
The present study showed that the electric current set in 50μA significantly increased the μTBS for all adhesive systems tested and light-cured by the single-emission peak and multiple-emission peak LCUs (Table 2). Thus, the first hypothesis was accepted. However, the second and third hypotheses were rejected, since the adhesive systems showed different μTBS mean values when applied under electric current (Table 2) and the LCU did not influence the μTBS (Table 2).
Resin monomers can be attracted by an electric field, increasing its flow into demineralized dentin [8, 10,11,12,13]. Electric current causes dielectric dispersion in tooth, improving ion diffusion and interfacial polarization [23]. The adhesive systems contain resin monomers with high molecular weight that increase the viscosity of the adhesives. It seems that the application of adhesives systems under electric current set in 50μA was able to improve resin tags and μTBS (Table 2). The electric current breaks the surface tension of the adhesives and changes the molecular arrangement of resin monomers, increasing its flexibility. Furthermore, the electric current breaks also the hydrogen bridges on the dentin surface increasing its surface energy [8, 11]. The high wettability of the adhesives associated with the increase in surface energy on dentin provided better adhesive penetration into dentin and less bubble formation (Fig. 4) [13]. It is hypothesized that there is a decrease in water penetration into the hybrid layer, facilitating chemical interactions between the self-etch adhesives (CSE and SBU) and dentin, increasing the μTBS (Table 2). Improved μTBS results are also expected in enamel, since electric current improves the wettability which increases the surface energy of substrate [10, 11]. Moreover, unlike dentin, the structure of the enamel is homogeneous [1, 2, 8], supporting the electric current dispersion in the substrate [10, 11].
Electric current may facilitate the diffusion of the adhesive into dentin, since polar components present in the adhesives interact with the electric field [10]. Thus, adhesive systems with low amount of polar monomers are less influenced by the electric current. Also, water molecules contribute to the polar nature of the dentin [10, 13]. Hydrophilic (self-etch) adhesive systems applied on dentin are more influenced by electric current. This can explain the different μTBS results for the adhesive systems applied under current electric (Table 2). The electric current formed a homogeneous hybrid layer, with efficient infiltration of the resin monomers and, consequently, longer and many resin tags (Fig. 4).
Although both LEDs tested are compatible with the CQ photoinitiator spectrum, they have different waves and irradiances (single-emission peak, 800mW/cm2 and multiple-emission peak, 1600mW/cm2). Inadequate polymerization results in a surface layer with low-pH adhesive poorly polymerized by contact with oxygen and incompatible with the resin composite [24], jeopardizing the μTBS. Moreover, small changes in the tip diameter of the LCU interfere in the irradiance [17]. The single-emission peak LCU (Radii-cal, SDI) has a smaller diameter tip (11.65mm) than multiple-emission peak LCU (VALO Cordless, Ultradent) (13.1mm) [25]. In addition, different LED chips present in single- and multiple-emission peak LCUs promote differences in irradiance and spectral emission across the tip of the LCU. These differences between different regions (position and distance) of the LCU could have significant implications in μTBS results [26]. However, in this study, the light-curing of the adhesives was standardized in 16J/cm2 (800mW/cm2 for 20s and 1600mW/cm2 for 10s) and the tips of both LCUs completely covering the dentin surface. Thus, different LCUs tested showed no differences in the μTBS (Table 2), since 16J/cm2 is the minimum energy density to polymerize properly the resin-based materials [27].
It is important to emphasize that electrical resistance of the dentin influence the transmission of electric current through the dentin. The dentin is heterogeneous [1, 2] and different zones present different electrical resistances. Therefore, it is imperative that the electric current device creates a constant electric current intensity [22]. The experimental electric current device developed in this study measures the electrical resistance of the zone where the adhesive is being applied and at same time provides a constant electric current, previously adjusted (50μA). This standardizes a safe electric current applied throughout dentin [22]. The present study obtained favorable results in the impregnation of the adhesive systems applied with electric current on the dentin surface, corroborating with previous studies [8, 10,11,12,13]. Different intensities of the electric current could show different bonding performance, since the electric current dentin changes the biophysical and biochemical properties of the dentin [8, 10, 11]. Although the electric current increases the resin composite adhesion to dentin using different LCUs and adhesive systems, it is noteworthy that μTBS results of this study were obtained from the immediate (24h) analysis. Furthermore, the chemical formulation of adhesive systems, in specific the purity of the functional monomers (e.g. 10-MDP) in self-etch adhesive systems, plays an important role for the μTBS [28]. Therefore, the authors emphasize the importance of further studies to evaluate the effects of different intensities of the electric current on immediate and long-term μTBS as well as the application of the adhesive systems with different chemical composition (different brands) under electric current, since the μTBS is material-dependent [29].
Conclusions
The application of etch-and-rinse and self-etch adhesives systems under electric current set in 50μA significantly improved the μTBS and the bonding quality of the adhesive interface, regardless of the LCU used.
References
Nakabayashi N, Nakamura M, Yasuda N (1991) Hybrid layer as a dentin-bonding mechanism. J Esthet Dent 3:133–138
Miranda MEDSNG, Silva EMD, Oliveira MF, Simmer FS, Santos GBD, Amaral CM (2020) Resin-dentin bond stability of etch-and-rinse adhesive systems with different concentrations of MMP inhibitor GM1489. J Appl Oral Sci. 28:e20190499
Kim Y, Kim S, Jeong T, Son SA, Kim J (2017) Effects of additional acid etching on the dentin bond strengths of one-step self-etch adhesives applied to primary teeth. J Esthet Restor Dent 29:110–117
Ermis RB, Ugurlu M, Ahmed MH, Van Meerbeek B (2019) Universal adhesives benefit from an extra hydrophobic adhesive layer when light cured beforehand. J Adhes Dent. 21(2):179–188
Ito S, Tay FR, Hashimoto M, Yoshiyama M, Saito T, Brackett WW, Waller JL, Pashley DH (2005 Summer) Effects of multiple coatings of two all-in-one adhesives on dentin bonding. J Adhes Dent. 7(2):133–141
Castellan CS, Bedran-Russo AK, Antunes A, Pereira PN (2013) Effect of dentin biomodification using naturally derived collagen cross-linkers: one-year bond strength study. Int J Dent 918010
Zhang Y, Jiang A (2020) The influence of Er:YAG laser treatment on the shear bond strength of enamel and dentin: a systematic review and meta-analysis. Quintessence Int. 51(1):8–16
Guarda MB, Di Nizo PT, Abuna GF, Catelan A, Sinhoreti MAC, Vitti RP (2020) Effect of electric current-assisted application of adhesives on their bond strength and quality. J Adhes Dent. 22(4):393–398
Pasquantonio G, Breschi L, Petrone A (2003) A method and device for preparing the hard structures of teeth for the application of dental restorative materials. US Patent
Pasquantonio G, Tay FR, Mazzoni A, Suppa P, Ruggeri A Jr, Falconi M, Di Lenarda R, Breschi L (2007) Electric device improves bonds of simplified etch-and-rinse adhesives. Dent Mater 23:513–518
Breschi M, Fabiani D, Sandrolini L, Colonna M, Sisti L, Vannini M, Mazzoni A, Ruggeri A, Pashley DH, Breschi L (2012) Electrical properties of resin monomers used in restorative dentistry. Dent Mater 28:1024–1031
Mazzoni A, Visintini E, Vita F, Pasquantonio G, Saboia VP, Ruggeri A Jr, Di Lenarda R, Dorigo E, Breschi L (2009) ElectroBond improves immediate dentin microtensile bond strength of two etch-and-rinse adhesives. J Adhes Dent 11:27–33
Visintini E, Mazzoni A, Vita F, Pasquantonio G, Cadenaro M, Di Lenarda R, Breschi L (2008) Effects of thermocycling and use of ElectroBond on microtensile strength and nanoleakage using commercial one-step self-etch adhesives. Eur J Oral Sci. 116(6):564–570
Stein S, Gente M (2013) Construction and in vitro test of a new electrode for dentin resistance measurement. Biomed Tech (Berl). 58(5):469–474
Krizaj D, Jan J, Valencic V (2004) Modeling AC current conduction through a human tooth. Bioelectromagnetics 25:185–195
Arrais CA, Pontes FM, Santos LP, Leite ER, Giannini M (2007) Degree of conversion of adhesive systems light-cured by LED and halogen light. Braz Dent J. 18(1):54–59
Chen Y, Yao C, Huang C, Wang Y (2019) The effect of monowave and polywave light-polymerization units on the adhesion of resin cements to zirconia. J Prosthet Dent 121:549.e1-549.e7
Soares CJ, Rodrigues MP, Oliveira LRS, Braga SSL, Barcelos LM, Silva GRD, Giannini M, Price RB (2017) An evaluation of the light output from 22 contemporary light curing units. Braz Dent J 28:362–371
Segreto DR, Naufel FS, Brandt WC, Guiraldo RD, Correr-Sobrinho L, Sinhoreti MA (2016) Influence of photoinitiator and light-curing source on bond strength of experimental resin cements to dentin. Braz Dent J. 27(1):83–89
Kurt A, Altintas SH, Kiziltas MV, Tekkeli SE, Guler EM, Kocyigit A, Usumez A (2018) Evaluation of residual monomer release and toxicity of self-adhesive resin cements. Dent Mater J. 37(1):40–48
Wegehaupt FJ, Lunghi N, Belibasakis GN, Attin T (2016) Influence of light-curing distance on degree of conversion and cytotoxicity of etch-and-rinse and self-etch adhesives. BMC Oral Health. 17(1):12
Pethig R (1987) Dielectric properties of body tissues. Clin Phys Physiol Meas (Suppl A):5–12
Jastrzebska M, Kocot A (2004) Ionic diffusion and space charge polarization in structural characterization of biological tissues. Eur Phys J E Soft Matter 14:137–142
Hanabusa M, Mine A, Kuboki T, Momoi Y, Van Ende A, Van Meerbeek B, De Munck J (2012) Bonding effectiveness of a new ‘multi-mode’ adhesive to enamel and dentine. J Dent. 40:475–584
André CB, Nima G, Sebold M, Giannini M, Price RB (2018) Stability of the light output, oral cavity tip accessibility in posterior region and emission spectrum of light-curing units. Oper Dent. 43:398–407
Price RB, Labrie D, Rueggeberg FA, Sullivan B, Kostylev I, Fahey J (2014) Correlation between the beam profile from a curing light and the microhardness of four resins. Dent Mater. 30(12):1345–1357
Conte G, Panetta M, Mancini M, Fabianelli A, Brotzu A, Sorge R, Cianconi L (2017) Curing effectiveness of single-peak and multi-peak led light curing units on tpo-containing resin composites with different chromatic characteristics. Oral Implantol (Rome). 10(2):140–150
Carrilho E, Cardoso M, Marques Ferreira M, Marto CM, Paula A, Coelho AS (2019) 10-MDP based dental adhesives: adhesive interface characterization and adhesive stability-a systematic review. Materials (Basel). 12(5):790
Giannini M, Makishi P, Ayres AP, Vermelho PM, Fronza BM, Nikaido T, Tagami J (2015) Self-etch adhesive systems: a literature review. Braz Dent J. 26(1):3–10
Funding
The work was supported by the School of Dentistry, University of Taubate and Piracicaba Dental School, University of Campinas.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This article does not contain any studies with human participants or animals performed by any of the authors. All procedures performed involving human waste were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, formal consent is not required.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Maciel, C.M., da Rosa Rinhel, M.F., Abuna, G.F. et al. Resin composite adhesion to dentin using different curing lights and adhesive systems applied under electric current. Clin Oral Invest 25, 5181–5188 (2021). https://doi.org/10.1007/s00784-021-03824-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-021-03824-9