Abstract
This study aimed at evaluating the influence of glass-fiber post (GFP) relining with composites of different opacities on resin cement layer thickness (CLT), bond strength (BS) to root dentin, and resin cement degree of conversion (DC%). Standardized roots of 52 bovine incisors had their canals prepared and were distributed into 4 groups (n = 10 for CLT and BS; n = 3 for DC%) according to the post used: WP3 (Control)—Whitepost DC3; groups DE, EN and TR—Whitepost DC0.5 relined, respectively, with dentin, enamel, and translucent shade composites. After cementation, specimens were sectioned into six 1.0 mm-thick discs that were submitted to push-out BS test. CLT and failure pattern were evaluated using a stereomicroscope and DC% by micro-Raman spectroscopy. Data were analyzed by two-way ANOVA and Tukey test (α = 0.05). The control group showed greater CLT than all relined groups (p < 0.05), which did not differ from each other (p > 0.05). Groups relined with low opacity composites (TR; EN) showed the highest BS and DC% means (p < 0.05). BS was not different among root thirds (p > 0.05), while DC% decreased from cervical to apical third (p < 0.05). Adhesive failures between cement and dentin were predominant, except for group DE with frequent mixed failures. It could be concluded that composite opacity did not influence CLT, which was thinner when GFP were relined and that relining GFP with lower opacity composites led to higher BS and DC%.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since its introduction in the 1990s [1], the effectiveness and clinical success of fiber-reinforced posts towards the reconstruction of endodontically treated teeth with large impairment of the remaining structure have been reported [2, 3]. The elastic modulus similar to that of dentin [4], the luting likelihood with resin cements and composite, and the favorable aesthetics are advantages of these posts—particularly, quartz and glass-fiber posts (GFP)—turning the root-post and core assembly a more homogeneous structure in comparison to teeth restored with cast metal posts [5].
The clinical service life of these posts depends not only on post-bonding to the resin cement, but also on the effective bonding between the cement and the root dentin, since debonding is reported as the most frequent failure and is most frequently related to the cement–dentin interface [6, 7]. Adhesion to the root canal is affected by several factors, particularly the canal anatomical characteristics and high cavity configuration factor (C-factor), which may exceed 200 [8, 9]. Moreover, post-retention to root dentin can also be influenced by irrigating techniques and solutions [10], post-length [11], cementation technique (including the cement itself) [12], post-fit to root canal walls, and the consequent cement layer thickness (CLT) [13].
Since well-adapted posts afford higher bond strength (BS) values when compared to poorly adapted posts [13], the precise adaptation between post and root canal diameters exhibits a clinical challenging procedure. Although the post system drills provided by manufacturers for root canal preparation aim for a desirable post-fit to the canal walls, in elliptical-shaped root canals and canals flared by extensive caries, trauma, pulpal, and iatrogenic pathologies, post-adaptation can be compromised, excessively increasing the CLT. A thick cement layer may favor the incorporation of air bubbles [14], besides allowing an increase of the polymerization contraction stress at the dentin–post-bonding interface due to an increase in the amount of resin matrix [15], which could lead to a discontinuous structural formation with cracks and voids, thereby increasing the risk of post dislodgment [16]. A suitable response to this problem would be the relining of the post with restorative composites, which aims at decreasing the CLT, thereby achieving better post-adaptation to dentin intracanal walls [14, 17, 18], which would diminish the dependence on the adhesive technique itself [17].
Another relevant aspect concerns the degree of conversion (DC%) of the resin cement used for post-cementation, since a higher DC% may be related to higher BS values [19]. In addition, the DC% of composite materials may be affected by their thickness, by post opacity and root depth, which could be related to light transmission inside the root canal [20, 21]. Furthermore, since the degree of conversion of resin-based materials is influenced by the type of monomers, filler particles, and amount of photoinitiators, the composition of the resin cement also plays an important role in BS [22].
In spite of these insights aforementioned, no previous investigations surveyed the influence of the relining composite opacity on post-BS to the root dentin and on resin cement DC%. Therefore, this issue is still a gap for further investigation. Thus, this study aimed at evaluating the influence of composites with different opacities used for GFP relining on the CLT, BS to root dentin and on in situ DC% of the resin cement used for post-cementation. The null hypothesis tested is that the relined post and the opacity of the composite do not influence CLT, BS to root dentin and DC% of the resin cement.
Materials and methods
Specimen preparation
Fifty-two bovine incisors were used in this study [23]. After cleaning and disinfection by immersion in 0.5% chloramine aqueous solution for 7 days, the crowns were sectioned at the cementum–enamel junction (Isomet 1000, Buehler, Lake Bluff, IL, USA) and root length was standardized at 14.0 mm. The roots were selected according to the following inclusion criteria: absence of cracks, analyzed using a stereomicroscope (SZ61, Olympus, Tokyo, Japan), coronary root canal diameter less than or equal to 2.0 mm, and closed apical apices. All measurements were performed with a digital caliper (500–196-20B, Mitutoyo, São Paulo, Brazil) and roots were stored in distilled water at 37 °C for 24 h.
The root canals were first prepared and enlarged to a work length of 12.0 mm with a size sequence of Largo drills (#1, #2, and #3, Dentsply Maillefer, Ballaigues, Switzerland) and later with the drill supplied by the GFP Whitepost DC3 manufacturer (FGM, Joinville, Brazil), under irrigation with 2.5% sodium hypochlorite solution. Every 5 root canals prepared, the drill was discarded and replaced with a new one. The canal apices were sealed with Filtek Z350 XT composite (3 M ESPE, St. Paul, MN, USA) shade A3D and the roots were coated with black cosmetic nail varnish to avoid light propagation through the external root surface. To maintain the bond interface parallel to the longitudinal axis of the mechanical testing machine, the roots were embedded up to its cervical limit, in acrylic resin into PVC cylinders, using a dental surveyor (EDG, São Carlos, Brazil).
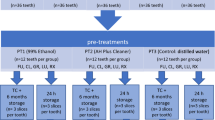
The roots were distributed into 4 groups (n = 10 for CLT and BS analyses and n = 3 for DC% analysis), according to the type of post used (Table 1): group WP3 (Control), where a GFP Whitepost DC3 was used under conventional technique; groups DE, EN, and TR, where a GFP Whitepost DC0.5 was relined with Filtek Z350 XT restorative composite, respectively, in shades A3D (dentin), A3E (enamel), and CT (translucent).
All GFP were ultrasonically cleaned (USC-800, Unique, Indaiatuba, Brazil) and conditioned with 24% hydrogen peroxide solution for 60 s [24], followed by an active application of an organosilane coupling agent (RelyX Primer, 3 M ESPE, St. Paul, USA). Posts from groups DE, EN, and TR were covered with their respective composite, inserted into the previously lubricated canal (K-Y Gel, Johnson & Johnson, São José dos Campos, Brazil), and photoactivated (800 mW/cm2 for 10 s, Radii-Cal, SDI, Victoria, Australia). After removal from the canal, photoactivation was further performed with two more 40 s irradiations on two opposing axial surfaces, aiming that all regions of the relining composite received the same radiant exposure. Irradiance was monitored with a radiometer (LED Radiometer, Demetron, SDS Kerr, Danbury, USA) every five irradiations. After water rinsing for lubricant excesses removal, the post-relined surface was air-abraded with 50.0 μm Al2O3 particles for 20 s (10.0 mm distance under 60 psi pressure/Microetcher ERC, Danville Engineering Inc., Danville, USA) and ultrasonically cleaned, and the organosilane coupling agent was actively applied for 60 s. For all groups, the root canals were washed with distilled water for 60 s and blot dried with an endodontic cannula (Ultradent Products Inc., South Jordan, USA) for 5 s, followed by a #80 absorbent paper point (Dentsply Maillefer, Ballaigues, Switzerland) for 1 s.
A self-adhesive resin cement (RelyX U200/3 M ESPE, St. Paul, USA) was manipulated according to the manufacturer's instructions and inserted into the canal with a syringe (Centrix/DFL, Rio de Janeiro, Brazil). Aiming to standardize the seating load, a 50.0 g brass cylinder was adapted on the top of the surveying arm, which was lowered towards the surveying platform, and the GFP was inserted into the root canal. The cement excesses were removed and photoactivation was carried out (800 mW/cm2 for 40 s). After cementation and prior to all analyses, the specimens were stored in distilled water at 37ºC for 24 h to keep the moisture of the roots and to release stresses derived from the resin cement polymerization.
To evaluate CLT, BS and the resin cement DC% at different root depths, specimens were sectioned, under refrigeration (Isomet 1000, Buehler, Lake Bluff, USA), perpendicularly to the post-long axis, obtaining 6 discs of 1.0 mm thickness [2 discs for each third – cervical (C), middle (M), and apical (A)]. Between each experimental procedure, discs were stored in distilled water at 37 °C. All analyses were performed immediately after removing the discs of the storage medium in a temperature-controlled laboratory (23 ± 1 °C).
CLT analysis
Before push-out test, specimens were photographed (40X) with a digital camera (UC30, Olympus, Munster, Germany) coupled to an optical stereomicroscope (SZ61, Olympus, Tokyo, Japan) and connected to a computer with an image capture software (AnalySIS getIT/Olympus Soft Image Solutions GmbH, Munster, Germany). An image analysis program (ImageJ 1.43u/Wayne Rasband National Institute of Health, Maryland, USA) was used to measure CLT, at four radial and equidistant sites on the cement film [25]. The CLT value at each site was obtained from the average of 3 subsequent measurements and the average of the 4 sites determined the specimen CLT (Fig. 1).
BS analysis
The BS analysis was undertaken by means of a push-out test. The test was performed by applying a compressive load on the apical side of the post (or post/relining composite set) of each disc using a cylindrical plunger attached to a universal testing machine (EMIC DL2000, Instron Brasil Equipamentos Científicos, São José dos Pinhais, Brazil), at a crosshead speed of 1.0 mm/min.
The BS was calculated by the formula: BS = F(N)/A, where F was the failure load and A was the area of the adhesive interface, which was calculated by the formula:
\(A= {\pi (R+r)[({h}^{2} + {(R-r)}^{2}]}^{0.5}\), where π = 3,1416, R = coronal diameter of the cement/post, r = apical diameter of the cement/post, and h = slice thickness.
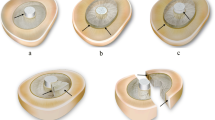
Failure pattern analysis
The specimens submitted to the push-out test were observed under an optical stereomicroscope (SZ61, Olympus, Tokyo, Japan) with a 40X increase, to determine the type of failure at the bonding interface. Failures were classified as: a) adhesive between cement and dentin (ACD); b) adhesive between cement and post/relined post (ACP); c) mixed, when it was possible to observe both patterns in the same specimen; d) cohesive, when the failure was verified in the bulk of the relining composite (Fig. 2).
DC% analysis
The disks submitted to the DC% analysis were wet-polished, sequentially, with 1500- and 2000-grit SiC papers for 20 s, and ultrasonically cleaned for 10 min in distilled water. Raman microspectroscopy analysis was used to assess the in situ DC% of the resin cement after photopolymerization. The micro-Raman spectrophotometer (Xplora, Horiba Jobin Yvon, Paris, France) was first calibrated using a silicon standard sample supplied by the manufacturer. HeNe laser with 3.2 mW power and 633 nm wavelength was employed with 1.5 µm spatial resolution, 2.5 cm−1 spectral resolution associated with 10X magnification lens (Olympus, London, UK) to position laser beam, approximately at the middle of the resin cement layer, equidistant from dentin walls and post or relining composite. DC% was calculated based in a previous investigation by means of the formula DC% = [1 – (Rpolymerized/Runpolymerized)] × 100, where R is the ratio between the heights of 1638 cm−1 and 1609 cm−1 peaks, after baseline correction, of uncured and polymerized cement material in root dentin specimens [26]. Three equidistant readings were undertaken at the cement layer on the topside of each specimen according to the experimental groups and root thirds.
Statistical analysis
After the sample normality and homoscedasticity were verified by means of Shapiro–Wilk and Levene test (p > 0.05), respectively, data obtained from each analysis were submitted to 2-way ANOVA (type of intracanal retainer: GFP and relined GFP; and root thirds: cervical, middle, and apical) and Tukey HSD test (α = 0.05) using Minitab software 17 (Minitab Inc., State College, USA). The sample size for both analyses was calculated based on the mean and standard deviation values obtained from the pilot study and considering a statistical test power of 0.80.
Results
The statistical analysis indicated that for CLT, BS, and DC% analyses, there was a statistically significant difference (p < 0.05) for the experimental groups. However, both the root third factor and the interaction (experimental group X root third) showed significant differences only for CLT and DC%. Table 2 presents the results of the interaction between the experimental groups and the root thirds for the CLT analysis. Analyzing separately each root third, it can be noted that, at the cervical third, while the CLT values of the WP3 group were only statistically higher than that of the TR group, at the middle and apical thirds, WP3 showed higher CLT than all further groups with relined GFP (DE, EN, and TR). Moreover, for all relined groups, CLT was not statistically different among root thirds, while for WP3, CLT of the cervical third was thinner than that of the apical.
The means and standard deviations of BS are reported in Table 3. In the “Main factor” column, it can be noted that groups EN and TR presented higher values than WP3 and DE. Moreover, there was no statistical difference between groups EN and TR and between WP3 and DE.
Figure 2 shows the failure pattern distribution after push-out test (A) and representative optical stereomicroscopy images of failed posts (B, C, and D). Adhesive failures between cement and root dentin (ACD) were the most frequent in all groups, except for the DE group. Slight percentage of cohesive failures was detected only in the TR group. No adhesive failures between the cement and the post were detected in any group.
Table 4 exhibits the results of the interaction between the experimental groups and the root thirds for the DC% analysis. For all root thirds, the DE group obtained the lowest values of DC% among all groups, whereas groups EN and TR showed the highest conversion. For all experimental groups, DC% was lower at the apical third than at the other thirds.
Discussion
The present investigation showed that CLT, BS to root dentin and resin cement DC% were influenced by post-relining. Furthermore, the opacity of the relining resin composite influenced BS and DC%. Therefore, the null hypothesis was rejected.
The choice of the resin composites employed for post-relining in the current experiment was based on a study that showed significant differences in the translucency parameter of these materials [27], which could affect post-retention to root dentin and DC% of the resin cement used for post fixation. Furthermore, to avoid a potential influence of different resin cement composition in the responses analyzed here, a widely worldwide resin cement, that could be considered a gold standard, was selected.
Regarding CLT, an expressive reduction was observed in the groups in which the GFP was relined in comparison to the one in which it was cemented without relining (Table 2). This result is supported by that of Souza et al.[14] and might be explained by a better post-adaptation to the root canal walls [16, 28, 29]. However, Souza et al.[14] showed a CLT increase from the cervical to apical region with relined posts, while in the present study, this variation was only observed for the conventional GFP without relining. This divergence may be related to methodological differences in post-relining techniques, which lacks standardization in the literature, and principally to the geometry of GFP used in both studies.
Comparing the CLT in each root third (Table 2), it can be noticed that for WP3 (non-relined group), there was a significant and progressive increase in CLT from 0.10 to 0.18 mm, a twofold increase that clearly characterize a poor adaptation of the GFP to the canal walls. Contrarily, for the relined groups, the CLT did not change in the three root thirds, suggesting that the relining protocol employed in the present study was capable of modeling the entire length of the post-space.
Well-adapted GFP to the canal walls has already been established to provide higher BS [13, 30]. That was the rationale to use a post with similar diameter to the root canal space as the control group. On the other hand, for the relined groups, a thinner post was used aiming at facilitating the insertion of a high viscosity material (the relining composite) in a very narrow space, which would be the case if the well-adapted post had been employed. Moreover, using the thinner post in a larger post-space intended to simulate a clinical condition in which flared root canals, which do not have a matching post, must be restored. Nevertheless, other studies had stated that BS was even greater when relined GFP were used [14, 18, 29, 31, 32], which supports the present outcomes (Table 3).
Among other aspects, reduced CLT favors the development of reduced polymerization shrinkage stress [16], which plays an important role in increasing BS of the relined posts to the canal walls. In the present investigation, there was no difference in BS among root canal thirds, as already mentioned. Using the same self-adhesive dual-cure resin cement of the current investigation, another study reported similar outcomes, but differences between root thirds were observed when a conventional resin cement was employed [33]. However, this topic does not seem consensual, as some findings corroborate with the present results [13, 25], while others do not [32, 34,35,36]. This divergence may be related to several factors, such as root canal morphological variations, which may explain the variability of the push-out test results, similar to those of other studies [37].
By analyzing the failure patterns after push-out test (Fig. 2), although ACD failures were predominant, as in accordance with previous studies [29, 31,32,33, 35, 36], the GFP relining increased the percentage of mixed failures. Furthermore, TR group, with posts relined with the lowest opacity composite (translucent shade), was the only one to exhibit cohesive failures. It is feasible to speculate that the low filler/matrix ratio of such composite [38] could contribute to these results, once posts relined with enamel and dentin shades (groups EN and DE) did not show cohesive failures.
Although the polymerization reaction of dual-cure resin cements is triggered by its chemical component, the contribution of the photoactivation to improve cement mechanical properties and DC% is also well established [39]. However, light transmission in the root canal is reduced as its depth increases. Thus, it is easily justified the use of translucent posts, theoretically capable of better transmitting the light to the root deepest region [13, 20, 25, 30]. While some studies have shown that these posts favored more efficient cement polymerization, which would be directly correlated to improved adhesion [35], others state that even translucent GFP would not substantially contribute to a better resin cement polymerization in the deepest root canal regions, which may lead to low bond strength values [34, 40]. These disagreements suggest that this issue still needs further investigation. Besides, the role of opacity of relining resin composite on resin cement DC% was also very little investigated.
In the present study, post-BS to root dentin (Table 3) and DC% of the resin cement (Table 4) were both influenced by the opacity of the resin composite used for post-relining, since low opacity composites (TR and EN) led to higher BS and DC% than the dentin-shade composite (DE), with the highest opacity. Analyzing the DC% of resin cements with different opacities through different ceramic materials, Mendonça et al. [41] showed that the more translucent cement presented higher DC% than an A2 shade one. The authors stated that the opacity of restorative materials influenced light transmittance, consequently jeopardizing the resin cements DC%. This finding is in agreement with another study [42] which showed that enamel shade and translucent resin composites (low opacity) presented higher DC% than dentin-shade/high opacity ones. Thus, it can be speculated that the less opaque composites (TR and EN) used could have facilitated light transmission during photoactivation [42], positively influencing DC% and BS to root dentin. Finally, based on the present results (Table 3), it is reasonable to infer that using a resin composite with low translucency could be not beneficial for improving GFP retention to root canal walls.
For all experimental groups, there was a reduction in the DC% from the cervical to the apical region. Furthermore, the DE group (dentin-shade composite) presented the lowest DC% in all root thirds (Table 4). These results are supported by previous studies showing a gradual reduction on the resin cements DC% in relation to the root depth [43, 44]. According to these authors, this is due to a substantial reduction in the light intensity in the root deepest regions, which diminishes the activation of camphorquinone, the light-curing component of polymerization. Interestingly, in the study of Kim et al. [44], the resin cement DC% with two translucent posts ranged from 69.7% to 46.5% and from 68.7% to 44.1% from the cervical to the apical third, values close to those observed for EN (79.9%–58.6%) and TR (76.5%–48.1%), less opaque resin composites, in the present study (Table 4). This finding suggests that GFP-EN and GFP-TR blocks behaved as monolithic structures regarding light transmission, positively impacting the DC%. The fact that WP3 (control group) presented a lower DC% than those of EN and TR in the apical third reinforces this assumption.
Considering that DC% is not the only determinant factor for the clinical success of a post-retained restoration and that relined GFP may partially compensate the dependence on the adhesive technique to the root canal [17, 45], it is reasonable to understand that, although the post had been relined with a high opacity composite and the resin cement had shown the worst DC% when compared to further groups, BS of the DE group was similar to the WP3s, even though the latter had higher DC%. This suggests that a thin resin CLT is as important as the adequate resin polymerization to attain optimal adhesion to root dentin [18, 29, 31, 32].
A threshold DC% has not yet been determined for methacrylate-based restorative materials, such as resin cements. Moreover, regarding their clinical performance, a negative correlation of resin composite abrasive wear in vivo and DC% [46] suggests that values above 55% could be taken as the minimum for this purpose. Thus, based on the present outcomes of posts relined with dentin-shade composite, attaining conversion lower than 55% in all root canal regions, it seems valid not to recommend GFP relining with high opacity composites, such as dentin and opaque shades.
This study adds important aspects regarding the influence of composites with different opacities used for GFP relining on the CLT, BS to root dentin and on in situ DC% of the resin cement used for post-cementation. Nevertheless, the use of only one resin cement could be considered a limitation of the current investigation, since resin cements with different compositions might influence the responses approached here. This aspect should be addressed in future investigations in this field.
Conclusions
Within the limitations of this study, it can be concluded that relined GFP provided a thinner cement layer. Moreover, retention was also improved when GFP were relined with more translucent composites, which, in turn, led to higher degree of conversion of resin cement than dentin-shade composite with high opacity. These findings indicate that less translucent resin composites provide no benefits for post-retention.
References
Duret PB, Reynaud M, Duret F. Un nouveau concept de reconstitution corono-radiculaire – le composipost (1). Chir Dent Fr. 1990;60:131–41.
Guldener KA, Lanzrein CL, Siegrist Guldener BE, Lang NP, Ramseier CA, Salvi GE. Long-term clinical outcomes of endodontically treated teeth restored with or without fiber post-retained single-unit restorations. J Endod. 2017;43:188–93. https://doi.org/10.1016/j.joen.2016.10.008.
Marchionatti AME, Wandscher VF, Rippe MP, Kaizer OB, Valandro LF. Clinical performance and failure modes of pulpless teeth restored with posts: a systematic review. Braz Oral Res. 2017;31: e64. https://doi.org/10.1590/1807-3107BOR-2017.vol31.0064.
Plotino G, Grande NM, Bedini R, Pameijer CH, Somma F. Flexural properties of endodontic posts and human root dentin. Dent Mater. 2007;23:1129–35. https://doi.org/10.1016/j.dental.2006.06.047.
Barjau-Escribano A, Sancho-Bru JL, Forner-Navarro L, Rodriguez-Cervantes PJ, Perez-Gonzalez A, Sanchez-Marin FT. Influence of prefabricated post material on restored teeth: fracture strength and stress distribution. Oper Dent. 2006;31:47–54. https://doi.org/10.2341/04-169.
Ferrari M, Vichi A, Mannocci F, Mason PN. Retrospective study of the clinical performance of fiber posts. Am J Dent. 2000;13:9B-13B.
Rasimick BJ, Wan J, Musikant BL, Deutsch AS. A review of failure modes in teeth restored with adhesively luted endodontic dowels. J Prosthodont. 2010;19:639–46. https://doi.org/10.1111/j.1532-849X.2010.00647.x.
Bouillaguet S, Troesch S, Wataha JC, Krejci I, Meyer JM, Pashley DH. Microtensile bond strength between adhesive cements and root canal dentin. Dent Mater. 2003;19:199–205. https://doi.org/10.1016/s0109-5641(02)00030-1.
Ferrari M, Mannocci F, Vichi A, Cagidiaco MC, Mjor IA. Bonding to root canal: structural characteristics of the substrate. Am J Dent. 2000;13:255–60.
Santana FR, Soares CJ, Silva JA, Alencar AH, Renovato SR, Lopes LG, Estrela C. Effect of instrumentation techniques, irrigant solutions and artificial accelerated aging on fiberglass post bond strength to intraradicular dentin. J Contemp Dent Pract. 2015;16:523–30. https://doi.org/10.5005/jp-journals-10024-1716.
Webber MB, Michida SM, Marson FC, de Oliveira GC, Silva CO. Analysis of bond strength by pull out test on fiber glass posts cemented in different lengths. J Int Oral Health. 2015;7:7–12.
Stockton LW. Factors affecting retention of post systems: a literature review. J Prosthet Dent. 1999;81:380–5. https://doi.org/10.1016/s0022-3913(99)80002-x.
Penelas AG, Piedade VM, Borges AC, Poskus LT, da Silva EM, Guimaraes JG. Can cement film thickness influence bond strength and fracture resistance of fiber reinforced composite posts? Clin Oral Investig. 2016;20:849–55. https://doi.org/10.1007/s00784-015-1568-3.
Souza NC, Marcondes ML, Breda RV, Weber JB, Mota EG, Spohr AM. Relined fiberglass post: an ex vivo study of the resin cement thickness and dentin-resin interface. Braz Oral Res. 2016;30: e7. https://doi.org/10.1590/1807-3107BOR-2016.vol30.0077.
Jongsma LA, Ir NDJ, Kleverlaan CJ, Feilzer AJ. Reduced contraction stress formation obtained by a two-step cementation procedure for fiber posts. Dent Mater. 2011;27:670–6. https://doi.org/10.1016/j.dental.2011.03.008.
Grandini S, Goracci C, Monticelli F, Borracchini A, Ferrari M. SEM evaluation of the cement layer thickness after luting two different posts. J Adhes Dent. 2005;7:235–40.
Faria-e-Silva AL, Pedrosa-Filho Cde F, Menezes Mde S, Silveira DM, Martins LR. Effect of relining on fiber post retention to root canal. J Appl Oral Sci. 2009;17:600–4. https://doi.org/10.1590/s1678-77572009000600012.
Macedo VC, Faria e Silva AL, Martins LR. Effect of cement type, relining procedure, and length of cementation on pull-out bond strength of fiber posts. J Endod. 2010;36:1543–6. https://doi.org/10.1016/j.joen.2010.04.014.
Pulido CA, de Oliveira Franco AP, Gomes GM, Bittencourt BF, Kalinowski HJ, Gomes JC, Gomes OM. An in situ evaluation of the polymerization shrinkage, degree of conversion, and bond strength of resin cements used for luting fiber posts. J Prosthet Dent. 2016;116:570–6. https://doi.org/10.1016/j.prosdent.2016.02.019.
Urapepon S. Degree of conversion of resin composite cured by light through a translucent fiber posts. J Adv Prosthodont. 2014;6:194–9. https://doi.org/10.4047/jap.2014.6.3.194.
Juloski J, Goracci C, Tsintsadze N, Carrabba M, Vichi A, Vulicevic ZR, Ferrari M. Influence of luting agent translucency on fiber post retention. Eur J Oral Sci. 2015;123:116–21. https://doi.org/10.1111/eos.12174.
da Silva EM, Poskus LT, Guimaraes JG. Influence of light-polymerization modes on the degree of conversion and mechanical properties of resin composites: a comparative analysis between a hybrid and a nanofilled composite. Oper Dent. 2008;33:287–93. https://doi.org/10.2341/07-81.
Soares FZ, Follak A, da Rosa LS, Montagner AF, Lenzi TL, Rocha RO. Bovine tooth is a substitute for human tooth on bond strength studies: a systematic review and meta-analysis of in vitro studies. Dent Mater. 2016;32:1385–93. https://doi.org/10.1016/j.dental.2016.09.019.
de Sousa MM, Queiroz EC, Soares PV, Faria-e-Silva AL, Soares CJ, Martins LR. Fiber post etching with hydrogen peroxide: effect of concentration and application time. J Endod. 2011;37:398–402. https://doi.org/10.1016/j.joen.2010.11.037.
Penelas AG, da Silva EM, Poskus LT, Alves AC, Simoes IIN, Hass V, et al. Development and characterization of biological bovine dentin posts. J Mech Behav Biomed Mater. 2019;92:197–205. https://doi.org/10.1016/j.jmbbm.2019.01.018.
Araujo-Neto VG, Nobre CFA, De Paula DM, Souza LC, Silva JC, Moreira MM, et al. Glycerol-dimethacrylate as alternative hydrophilic monomer for HEMA replacement in simplified adhesives. J Mech Behav Biomed Mater. 2018;82:95–101. https://doi.org/10.1016/j.jmbbm.2018.03.022.
Salgado VE, Rego GF, Schneider LF, Moraes RR, Cavalcante LM. Does translucency influence cure efficiency and color stability of resin-based composites? Dent Mater. 2018;34:957–66. https://doi.org/10.1016/j.dental.2018.03.019.
Caceres EA, Sampaio CS, Atria PJ, Moura H, Giannini M, Coelho PG, et al. Void and gap evaluation using microcomputed tomography of different fiber post cementation techniques. J Prosthet Dent. 2018;119:103–7. https://doi.org/10.1016/j.prosdent.2017.01.015.
Rocha AT, Goncalves LM, Vasconcelos AJC, Matos Maia Filho E, Nunes Carvalho C, De Jesus Tavarez RR. Effect of anatomical customization of the fiber post on the bond strength of a self-adhesive resin cement. Int J Dent. 2017;2017:5010712. https://doi.org/10.1155/2017/5010712.
Latempa AM, Almeida SA, Nunes NF, da Silva EM, Guimaraes JG, Poskus LT. Techniques for restoring enlarged canals: an evaluation of fracture resistance and bond strength. Int Endod J. 2015;48:28–36. https://doi.org/10.1016/j.fdj.2015.11.001.
Al-Assar RM, El-Ghani OSA, Mandour MH. Effect of relining, cement type, and thermocycling on push-out bond strength of fiber reinforced posts. Fut Dent J. 2015;1:13–22. https://doi.org/10.1111/iej.12272.
Marcos RM, Kinder GR, Alfredo E, Quaranta T, Correr GM, Cunha LF, et al. Influence of the resin cement thickness on the push-out bond strength of glass fiber posts. Braz Dent J. 2016;27:592–8. https://doi.org/10.1590/0103-6440201600886.
Conde DM, Rodrigues VP, de Carvalho Souza SF, Bauer JR, da Bramante FS, Linares Lima SN, et al. Influence of relining post on the bond strength of resin cements. J Contemp Dent Pract. 2015;16:559–64.
Kalkan M, Usumez A, Ozturk AN, Belli S, Eskitascioglu G. Bond strength between root dentin and three glass-fiber post systems. J Prosthet Dent. 2006;96:41–6. https://doi.org/10.5005/jp-journals-10024-1722.
Reginato CF, Oliveira AS, Kaizer MR, Jardim PS, Moraes RR. Polymerization efficiency through translucent and opaque fiber posts and bonding to root dentin. J Prosthodont Res. 2013;57:20–3. https://doi.org/10.1016/j.jpor.2012.05.003.
Rodrigues RV, Sampaio CS, Pacheco RR, Pascon FM, Puppin-Rontani RM, Giannini M. Influence of adhesive cementation systems on the bond strength of relined fiber posts to root dentin. J Prosthet Dent. 2017;118:493–9. https://doi.org/10.1016/j.prosdent.2017.01.006.
Putignano A, Poderi G, Cerutti A, Cury A, Monticelli F, Goracci C, et al. An in vitro study on the adhesion of quartz fiber posts to radicular dentin. J Adhes Dent. 2007;9:463–7.
3M ESPE Filtek Z350 XT Technical Product Profile (2010) https://multimedia.3m.com/mws/media/631547O/filtek-z350-xt-technical-product-profile.pdf. Accessed 29 July 2021.
Aguiar TR, de Oliveira M, Arrais CA, Ambrosano GM, Rueggeberg F, Giannini M. The effect of photopolymerization on the degree of conversion, polymerization kinetic, biaxial flexure strength, and modulus of self-adhesive resin cements. J Prosthet Dent. 2015;113:128–34. https://doi.org/10.1016/j.prosdent.2014.09.011.
dos Santos Alves Morgan LF, Peixoto RT, de Castro Albuquerque R, Santos Correa MF, de Abreu Poletto LT, Pinotti MB. Light transmission through a translucent fiber post. J Endod. 2008;34:299–302. https://doi.org/10.1016/j.joen.2007.12.007.
Mendonca LM, Ramalho IS, Lima L, Pires LA, Pegoraro TA, Pegoraro LF. Influence of the composition and shades of ceramics on light transmission and degree of conversion of dual-cured resin cements. J Appl Oral Sci. 2019;27: e20180351. https://doi.org/10.1590/1678-7757-2018-0351.
Gaglianone LA, Lima AF, Araujo LS, Cavalcanti AN, Marchi GM. Influence of different shades and LED irradiance on the degree of conversion of composite resins. Braz Oral Res. 2012;26:165–9. https://doi.org/10.1590/s1806-83242012005000002.
Faria e Silva AL, Arias VG, Soares LE, Martin AA, Martins LR. Influence of fiber-post translucency on the degree of conversion of a dual-cured resin cement. J Endod. 2007;33:303–5. https://doi.org/10.1016/j.joen.2006.11.015.
Kim YK, Kim SK, Kim KH, Kwon TY. Degree of conversion of dual-cured resin cement light-cured through three fibre posts within human root canals: an ex vivo study. Int Endod J. 2009;42:667–74. https://doi.org/10.1111/j.1365-2591.2009.01565.x.
De Souza G, Braga RR, Cesar PF, Lopes GC. Correlation between clinical performance and degree of conversion of resin cements: a literature review. J Appl Oral Sci. 2015;23:358–68. https://doi.org/10.1590/1678-775720140524.
Ferracane JL, Mitchem JC, Condon JR, Todd R. Wear and marginal breakdown of composites with various degrees of cure. J Dent Res. 1997;76:1508–16. https://doi.org/10.1177/00220345970760081401.
Funding
This study was supported by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior-Brazil (CAPES)-Finance Code 001 and by the Fundação Carlos Chagas Filho de Amparo à Pesquisa do Estado do Rio de Janeiro—FAPERJ (Grant Number 200888/2017).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Not applicable.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Penelas, A.G., da Silva, E.M., Fedozzi, J.M. et al. Glass fiber posts relining: can composite opacity influence retention to root canal dentin?. Odontology 110, 569–576 (2022). https://doi.org/10.1007/s10266-022-00693-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10266-022-00693-w