Abstract
Objectives
The aim of the present study was to test a self-adhesive resin cement used as core build-up material in comparison to two commercially available core build-up materials.
Materials and methods
Forty human anterior teeth were endodontically treated and fiber post insertion (RelyX Fiber posts) and core build-ups were performed using two core build-up materials applied with an etch-and-rinse adhesive approach (Luxacore Dual-LC and Clearfil Core-CC) and an experimental self-adhesive resin cement (SAR) in two application modes (SAR Handmix and SAR Automix). Samples were subjected to thermo-mechanical loading. Margin integrity was determined using scanning electron microscopy (SEM), and maximum load capability (Fmax) was evaluated. Physical properties of the tested materials were also examined.
Results
Fmax was significantly affected by the core build-up material (p < 0.0005; one-way ANOVA). CC [481 (158) N] revealed significantly higher Fmax compared to LC [226 (80) N], SAR Hand [205 (115), and SAR Automix [197 (134) N] (p < 0.05; Tukey-B). The percentage of margin quality “continuous margin” in enamel after thermo-mechanical loading (TML) differed significantly among groups (p < 0.0005; Kruskal-Wallis); CC demonstrated a significantly higher percentage of margin quality “continuous margin” compared to the other groups. Physical properties were significantly affected by the different core materials (p < 0.0005; ANOVA); CC and LC demonstrated significantly higher flexural strength compared to both SAR groups as well as significantly higher water sorption of both SAR groups compared to CC and LC.
Conclusion
Within the limitations of the present in vitro study, we conclude that the investigated experimental self-adhesive resin cement is not suitable as a core build-up material due to the lower maximum load capability, low margin quality, and the data of the mechanical properties.
Clinical relevance
The investigated experimental self-adhesive resin cement cannot be recommended as a core build-up material.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The restoration of endodontically treated teeth with adhesively luted fiber reinforced composite posts (FRC posts) gained more popularity, and prospective clinical investigations revealed promising results [1, 2].
Current developments tend to adhesively restore severely damaged endodontically treated teeth in a one-stage post-and-core procedure [3]. The core build-up will immediately follow post luting procedure using the same composite resin material in order to introduce a so-called secondary mono-block [4]. Such workflow could reduce the time necessary for the clinical procedure, the technique sensitivity, and possible incompatibilities between luting agent and core build-up material. A clinical observation demonstrated an annual failure rate of 4.6 % after 10 years [5] which indicates problems with adhesively luted FRC posts. The most common complications of adhesively luted endodontic posts are post debonding and endodontic lesions [6]. Thus, luting of posts inside the root canal is still a challenge due to the extremely high C-factor inside the root canal [7], limited access, visibility, moisture control, and deposition of cementum and secondary dentin [8]. The use of self-adhesive resin cements for luting fiber posts inside the root canal has been shown to be more reliable in vitro as demonstrated in a recently published review [9]. Additionally, these resin cements resulted in significantly higher bond strength to root canal dentin after thermo-mechanical loading [10] as well as less nanoleakage compared to other resin-based luting agents inside the root canal [11]. Moreover, a randomized controlled clinical trial (RCT) demonstrated high success rates over 90 % after 7 years for luting fiber and titanium posts using a self-adhesive resin cement [2]. Additionally, bond strengths to coronal dentin of self-adhesive resin cements have been shown to be as good as one- or two-step adhesives [12, 13]. Therefore, it would be desirable if self-adhesive resin cements could also serve as core build-up material used in a one-stage post-and-core procedure. Few studies have analyzed self-adhesive resin cements used as core build-up materials restored with ceramic crowns after simulated clinical function as well as after long-term incubation in vitro. These studies demonstrated no significant differences with respect to survival to chewing simulation and maximum load capability compared to resin-based core materials applied with a separate adhesive system [14, 15]. However, a recently published study revealed that self-adhesive resin cements that were used as core build-up for severely damaged endodontically treated teeth may have the potential to cause fracture of lithium disilicate crown restorations [16]. The authors speculated that hygroscopic expansion of self-adhesive resin cements may have an adverse impact on the longevity of lithium disilicate glass ceramic crowns. Consequently, the use of self-adhesive resin cements used as core build-up materials still remains controversial. Data on mechanical properties of some self-adhesive resin cements demonstrated comparable results to conventional composites with respect to modulus of elasticity, Vickers hardness, creep, and elastic-plastic deformation [17]. However, the knowledge on water sorption and hygroscopic expansion of self-adhesive resin cements is scarce.
Therefore, the aim of the present study was to analyze an experimental self-adhesive resin cement in two application modes used as core build-up material in comparison to two commercially available resin-based core build-up materials applied with an etch-and-rinse adhesive. The testing included the evaluation of margin integrity at the interface core material/tooth structure as well as the measurement of maximum load capability after thermo-mechanical loading (TML) as well as analyses of the physical properties of the investigated materials.
The null hypotheses were that neither maximum load capability, margin integrity, nor physical properties would be affected by the type of core material.
Materials and methods
Specimen preparation
Forty sound human maxillary central incisors were selected according to root length and bucco-lingual as well as mesial-distal extensions at the cemento-enamel junction (CEJ). Extremely small or large teeth were excluded. Teeth were obtained with written informed consent under an ethics-approved protocol (EA1/034/06) by the Ethical Review Committee of the Charité - Universitätsmedizin Berlin and stored in 0.5 % chloramine T solution for a maximum of 1 year after extraction. The crowns were partially removed except one residual mesial wall of 2-mm thickness including the incisal edge (Fig. 1a), and root canal preparations were performed at a working length of −1 mm from the apical foramen using a single length technique with MTwo rotary instruments (VDW, Munich, Germany) by one trained operator. Apical enlargement was performed to a size of 60/.02 using Flex Master rotary files (VDW). The canals were irrigated (Endoneedle; Vedefar, Dilbeek, Belgium) by using 1 mL of 1 % NaOCl solution after every change of file size. The teeth were then filled with warm, vertically condensed BeeFill®2in1 gutta-percha (VDW) and AH Plus sealer (Dentsply DeTrey, Konstanz, Germany), and stored in water for 24 h.
Specimen preparation of the present study. a Crown of tooth partly removed except one residual mesial wall of 2 mm thickness. b Fiber post insertion insertion depth was 8 mm; a strip crown was used for core build-up using different core materials. c Marks were applied vestibular and palatinal to define areas for analyses of marginal integrity
The teeth were randomly assigned to four groups (n = 10) according to the determined root length and bucco-lingual and mesial-distal extensions at the CEJ to assure a homogenous distribution among groups. All root canals were enlarged using the drill of the system RX Post size 2 (3M ESPE, Seefeld, Germany). The depth of the post space preparation was 8 mm, leaving at least 4 mm of gutta-percha inside the canal to guarantee an apical seal. The post space was checked for cleanliness using an operating microscope (magnification ×23, OPMI pico, Zeiss, Jena, Germany). Irrigation after post space preparation (Endoneedle; Vedefar, Dilbeek, Belgium) was performed in all groups using 5 mL 1 % sodium hypochlorite (NaOCl) for 1 min followed by 5 mL distilled water.
Adhesive post placement was conducted using fiber post RelyX Post Size 2 (3M ESPE) and the following four materials according to the manufacturers instructions: LuxaCore dual Smartmix (DMG, Hamburg, Germany) and the corresponding adhesive system LuxaBond-Total Etch (DMG)-Group (G) LC; an experimental self-adhesive resin cement SF Cem (3M ESPE) either mixed with an automix procedure—G SAR Automix—or a handmix procedure (called “Clicker” by the manufacturer)—G SAR Handmix; and an autopolymerizing core material Clearfil Core (Kuraray, Okayama, Japan) applied with the etch-and-rinse adhesive system New Bond (Kuraray)—G CC (Fig. 1b). The composition of the investigated materials is presented in Table 1. In group LC and CC, the post space and the coronal tooth portion was etched using phosphoric acid (Universal Etching Gel, 37 %, DMG) for 15 s prior to post placement. After rinsing using tap water and air drying, the adhesives were applied strictly following the manufactures instructions. After post placement in G LC, SAR Automix, and SAR Handmix, light curing on the top of the post for 40 s (1200 mW/cm2, Elipar Freeligth 2, 3M ESPE) was performed. In G CC, the post was inserted and kept in position for 3 min to guarantee complete setting of the material.
Opaque celluloid crowns (Frasaco strip crown, Frasaco GmbH, Tettnang, Germany) were used as matrices to form the core build-up. The strip crowns were filled with the respective core material, and manually fixed onto the tooth (Fig. 1c). Light curing was performed for 40 s from the buccal and palatal aspect, respectively, except for the solely chemically curing material Clearfil Core. After removing the strip crown, excess was removed using a diamond bur (862EF.314.012, Komet Dental, Lemgo, Germany) and the core build-up was polished using polishing discs (Sof-Lex discs, 3M ESPE). No further coronal restoration was performed. Small marks were placed using a diamond bur to define areas at the buccal and palatal site of the crown for the analyses of margin integrity (Fig. 1c).
Loading procedure
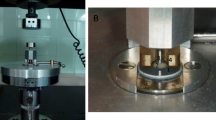
For the loading procedure, the roots were coated with a thin layer of wax (0.3 mm casting wax veined green, Dentaurum, Pforzheim, Germany), blocked out with wax 2 mm below the CEJ and mounted in an acrylic resin block (Technovit 4004, Heraeus Kulzer, Germany). To simulate the tooth mobility, roots were removed, cleaned, and coated with a thin layer of autopolymerizing acrylic resin (Paladur®, Heraeus Kulzer, Germany). An A-polysiloxane soft cushion material (Mollosil®, DETAX, Germany) was placed into the simulated socket, and specimens were relocated into the mold [18].
Thermal cycling and mechanical loading (TCML) were performed simultaneously (6000 thermal cycles, 5/55 °C, 2 min each cycle in dist. water; 1.2 × 106 mastication cycles with 50 N; 135°; 3 mm below the incisal edge on the palatal surface of the crown). Afterwards, the specimens were stored for 6 weeks in distilled water at 37°.
Specimen preparation for margin integrity
Before and after TML and water storage, impressions of the crowns were taken using an A-silicone (Honigum Light, DMG) using individually made silicone molds. The impressions were poured out with epoxy resin (Stycast 1266, Emerson & Cuming, Westerlo, Belgium), and sputter-coated with gold (Sputter Coaster SCD 030; Detax, Ettlingen, Deutschland). All specimens were examined for quantitative margin analysis with a scanning electron microscope (Cam Scan Maxim 2040; Cam Scan Maxim Elektron Optics, Cambridge, UK) in low vacuum mode (10 kV and ×200 magnification) by one examiner, who was blinded with respect to the group assignment of the specimens. All specimens were examined for “continuous” margins (no gap, no interruption of continuity) and imperfect “noncontinuous” margins (gap due to adhesive or cohesive failure; restoration or enamel fractures related to restoration margins), and the percentage of continuous margin in enamel was calculated at defined areas (Fig. 1c).
Testing of maximum load capability and analyses of failure modes
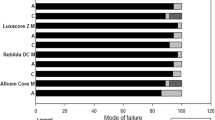
After TML and impressions for the analyses of margin integrity, the specimens were loaded at 135° in a universal testing machine (Zwick 1446; Zwick, Ulm, Germany; v = 1 mm min1) until failure. Failure detection was set at 10 % loss of the maximum force (Fmax). After testing the maximum load capability, each specimen was observed to determine the failure mode. A scoring system was applied according to the failure modes: (1) adhesive failure showing adhesive fracture between tooth and core material; (2) mixed failure demonstrating adhesive fracture between tooth and core material as well as cohesive fracture inside the core material, (3) fracture of the tooth at crown level, and (4) horizontal fracture of the root in the cervical third.
Testing of physical properties
Light-cured specimens were prepared as described in the following using a halogen curing device (Spectrum 800, Dentsply DeTrey GmbH, Konstanz, Germany). The output of the curing device was routinely checked (Bluephase meter, Ivoclar Vivadent AG, Schaan, Liechtenstein), and no significant decrease in the output was observed.
Flexural strength, flexural modulus
Specimens (25 ± 2 × 2 ± 0.1 × 2 ± 0.1 mm) were made according to ISO 4049 [19] and cured in five 40-s steps (overlapping half the light guide’s diameter) from each side (400 s in total). After 24 h of water storage at 37°, the three-point-bending test (universal testing machine, crosshead speed of 0.75 mm min−1, Model 106.L, Test GmbH, Erkrath, Germany) was conducted. Flexural strength was calculated by σ = (3FL)/(2bh2) and flexural modulus by E = (L 3/4bh3) × (F/Y), both expressed in MPa with F = maximum strength, L = distance between the rests (20 mm), b = width of the specimen, h = height of the specimen, and F/Y = slope of the linear part of the stress-strain curve.
Polymerization shrinkage
Polymerization shrinkage was calculated from the densities measured according to the Archimedes’ principle with the commercial Density Determination Kit of the analytical balance Mettler Toledo XS (Mettler Toledo GmbH, Greifensee, Switzerland). The specimens were weighed in air and in water, and the density was calculated in grams per cubic centimeter by the software of the Mettler Toledo XS balance by D = (A/(A − B)) × (D 0 − D L) + D L with D = density of sample, A = weight of sample in air, B = weight of sample in water, D 0 = density of water at the exactly measured temperature in °C according to the density table of distilled water, and D L = air density (0.0012 g cm−3). An internal balance correction factor (0.99985) took air buoyancy of the adjustment weight into account.
From each uncured material, spherical specimens, each of approximately 0.1 g, were carefully formed so that trapped air bubbles were avoided. Each specimen was put on a polyester film (thickness 0.05 mm), fixed on the special holder of the balance, of which the masses in air and in water were known and the masses of the whole assembly in air and in water were weighed. Since the weighing process was very fast (approximately 10 s), there was no water uptake or flow of the material. It was observed that the uncured specimens were optimally wetted. The mass of each specimen was calculated by subtracting the mass of the polyester film from the mass of the whole assembly, and the density of the uncured material (D un) was computed. Next ten discs (diameter 10 ± 0.1 mm, thickness 1 ± 0.1 mm) of each material were prepared and polymerized for 40 s from each side. Then, the masses in air, m1, and in water and the densities (D 1) were evaluated and the polymerization shrinkage in percent was calculated by ΔV = ((1/D 1) − (1/D un)) × (1/D un) × 100.
Hygroscopic expansion and water sorption
Cylindrical specimens of each material (diameter 10 ± 0.1 mm, thickness 1 ± 0.1 mm) were polymerized for 40 s on each side. The mass m 1 and density D 1 of each specimen were determined after 15 min of dry and dark storage at room temperature (see polymerization shrinkage) and the volume V 1 was calculated by V 1 = m1/D 1. After 30 days dark storage in water at 37 ± 1 °C, the masses m 2 and densities D 2 were measured again and the respective volumes were calculated by V 2 = m 2/D 2. The hygroscopic expansion ΔV was calculated by subtracting V 2 from V 1, and the results were expressed in percent. Water sorption W Sp was calculated by W Sp = (m 2 − m 1)/V. Prior to each measurement, the specimens were tempered to room temperature in a water bath for 10 min. Before weighing the specimens in the air, they were blot-dried with a cellulose pad.
Curing depth
Dual- and light-curing materials were filled in a white polyoxymethylen mold (length 15 ± 1 mm, diameter 4 ± 0.1 mm) and polymerized for 40 s from one side. Immediately after irradiation and removal from the mold, the unpolymerized parts were scraped off and the length of the cured material was measured with a mechanical caliper (Special Caliper, accuracy of 0.02 mm, MIB Messzeuge GmbH, Spangenberg, Germany).
Statistical analysis
Margin quality was expressed as a percentage of continuous margins over the investigated margin length (100 % = no discontinuous aspects) both before and after TML at previously defined areas. Differences in margin integrity between the investigated materials were calculated using Kruskal-Wallis test with following pairwise comparisons using non-parametric permutation test, and a Bonferroni adjustment of α = 0.00183 was applied. The effect of core material on maximum load capability was analyzed using a one-way ANOVA followed by post hoc test Tukey-B (IBM SPSS version 21.0 software, Chicago, IL, USA). Analysis of the failure modes was conducted using crosstabs and chi-square test.
For analyses of the physical properties, means and standard deviations were calculated. Normal distribution was tested by the Kolmogoroff-Smirnoff test. Univariate ANOVA and post hoc test Tukey-B were performed separately for each of the different mechanical properties to reveal differences between the materials. Statistical significance for all tests was considered as p < 0.05.
Results
Maximum load capability [mean (SD)] was significantly affected by the core material (p < 0.0005; one-way ANOVA). G CC [481 (158) N] revealed significantly higher maximum load capability compared to G LC [226 (80) N], G SAR Hand [205 (115), and G SAR Automix [197 (134) N] (p < 0.05; Tukey-B). The analyses of the failure modes revealed significant differences among the groups (p < 0.0005; chi-square test); G CC demonstrated significantly more failures of type III and IV (Table 2).
Analyses of margin integrity in enamel [median (Q1/Q3)] after TML and water storage demonstrated significant differences between groups (p < 0.0005; Kruskal-Wallis test). G CC [63,4 (38,7/85,6) %] demonstrated significantly more percentage of continuous margins in enamel compared to G LC [30 (16,6/34,9) %], G SAR Handmix [0,6 (0/5,9) %], and G SAR Automix [0 (0/7,6) %] (Table 3).
The physical properties flexural strengths, flexural modulus, curing depths, polymerization shrinkage, hygroscopic expansion, and water sorption were significantly affected by the investigated materials (all p < 0.005; ANOVA). Differences in the physical properties according to the post hoc tests are presented in Table 4.
Discussion
The present study intended to analyze the suitability of an experimental self-adhesive resin cement as core build-up material and post luting material in a one-stage post-and-core procedure to restore partially damaged central maxillary incisors with one remaining cavity wall. The present study set-up focused on the analyses of the maximum load capability and the margin integrity of the core build-up materials. For that reason, the inclusion of a final restoration, such as a crown, with a ferrule effect, was omitted by purpose. In this way, we could solely test the effect of the core material, whilst excluding any strengthening effect of the crown and the ferrule preparation on the tooth-core build-up that has been clearly shown in the literature [20].
The hypotheses of the present study have to be rejected, because maximum load capability, margin integrity, and physical properties differed significantly between core materials.
Clearfil Core as a specific autopolymerizing core build-up material applied with an etch-and-rinse adhesive system was included in this study, because this material revealed also good results in recently published clinical trials [1, 2] and has been used several times for maximum load capability analyses [14, 21–23]. The dual-curing material LuxaCore dual has been additionally tested in vitro for maximum load capability tests [14] and exhibits the same curing mode as the investigated SAR cement and was therefore selected. The investigated experimental SAR cement was analyzed in two application modes, i.e., hand mix and automix. Since the suitability of the application for the use of the SAR cement as core build-up material was not clear at the beginning of this study, this should be additionally evaluated in the present study.
Results of maximum load capability testing revealed significant differences among groups. The chemical curing core build-up material Clearfil Core demonstrated significant higher fracture load compared to LuxaCore dual and both experimental SAR cement groups. Another study that analyzed nearly the same materials did not show any significant difference regarding maximum load capability of the different core build-up materials [14]. However, the Clearfil Core group was the only one where all specimens survived thermo-mechanical loading. Moreover, in the mentioned study, all teeth were restored using all-ceramic full crowns, which was a different experimental set-up compared to the present study [14].
Despite the testing of various core materials in the present study, the same FRC post (RelyX Post, 3M ESPE) was used in all groups, which is epoxy resin based. Consequently, possible effects of the post type on maximum load capability could be excluded. However, chemical interaction in forms of co-polymerizing between methacrylate-based resins of the luting agents and the highly cross-linked epoxy resin matrix of the posts is less likely [24]. Recently published data indicate that the degree of which both micro-mechanical interlocking and chemical bonding contribute to bond strength between fiber posts and resin cements is currently not known [25]. However, it is assumed that micro-mechanical interlocking that is basically depending on the post-surface topography might be the most contributing factor [25]. Consequently, the use of one type of fiber post might be more reliable.
In this study, the evaluation of margin integrity at the interface between core material and tooth was performed with the scanning electron microscope (SEM) which is used for identification and quantification of different margin qualities [26]. This quantification method relies on imaging of precision replicas of the restored teeth and on quantitative quality analysis of the entire margin length. The replica technique is non-destructive to the natural-tooth samples and thus the margins can be assessed and defects at the margins detected and compared before and after applying different stresses to the tooth specimens. The high sensitivity of this method, due to the SEM’s excellent detail reproduction, is a great advantage for evaluating the adaptation of the care materials to tooth substrate [27].
With respect to the interpretation of failure modes, it can be concluded that the detected failure modes are in agreement with the results of the maximum load capability testing. Clearfil Core demonstrated significantly higher maximum load capability compared to all other groups and was the only group that demonstrated crown and root fractures, indicating a strong adhesion between tooth and core material. All other investigated groups also demonstrated adhesive failure between core material and tooth structure as well as mixed failure, indicating a weaker adhesion between the materials and the tooth compared to Clearfil Core and the adhesive system Clearfil New Bond.
The results for maximum load capability are supported by the analyses of the margin integrity of the core materials. Again, Clearfil Core demonstrated a significant higher percentage of continuous margins compared to Luxacore dual; the SAR cements revealed a negligible percentage of continuous margins after thermo-mechanical loading. This is supported by previously published data that demonstrated that SAR cements revealed significantly more gaps in dentin when used for elevation of the proximal boxes using the proximal box elevation technique and restorations with ceramic inlays [28]. In the present investigation, the percentage of continuous margins for the SAR cements was even lower compared to the mentioned study; in the present experimental set-up, no coronal restoration was performed and therefore the effects of the thermo-mechanical loading on margin integrity are suspected to be very strong. Fabrication of the core build-ups were performed using strip crowns. It has been demonstrated in the literature that higher seating force could enhance bond strengths of SAR cements to coronal dentin [29]. However, a recently published study about the performance of SAR cements as core build-up material after long-term incubation speculated that the core build-up technique using strip crowns might lead to a high core volume that includes inner parts of the material with a lower conversion rate and therefore reduced mechanical properties [30].
Concerning the results of mechanical properties testing the data of flexural strengths, water sorption and curing depths of all investigated materials met the criteria of ISO 4049 [19]; nevertheless, the SAR materials demonstrated significantly lower flexural strength and higher water sorption. Significantly lower polymerization shrinkage of Clearfil Core as well as a significantly higher elastic modulus of this material compared to the other materials might serve as an explanation for the high load capability of this material. Both tested SAR cements revealed significantly higher water sorption compared to the other investigated core materials and similar behavior with respect to hygroscopic expansion. These results corroborate data of a previous study that indicated fracture of lithium disilicate glass ceramic crowns after long-term incubation with SAR core build-ups [31]. Furthermore, the significant differences concerning water sorption and hygroscopic expansion might serve as another explanation for the insufficient results of the margin integrity of the SAR materials.
Conclusions from in vitro data regarding the clinical performance of endodontically treated teeth must be drawn with caution. Artificial ageing is known to have a considerable impact on the data generated in maximum load capability tests [32]. For this reason, thermo-mechanical loading of the specimens prior maximum load capability testing and analyses of margin integrity was applied in the present study. Furthermore, simulation of the periodontal ligament was performed with the aim to mimic the oral cavity [18]. Nevertheless, the reduced maximum load capability of the SAR cement when used as core build-ups as well as the low margin integrity may implicate that the use of SAR cements as build-up materials cannot been recommended. This is supported by the results of the mechanical properties testing.
Conclusions
Within the limitations of the present in vitro study and experimental set-up, we conclude that the investigated experimental self-adhesive resin cement used in this study is not suitable as a core build-up material due to the lower maximum load capability, the low margin quality at the tooth-core build-up material interface, and the data of the mechanical properties.
References
Bitter K, Noetzel J, Stamm O, Vaudt J, Meyer-Lueckel H, Neumann K, Kielbassa AM (2009) Randomized clinical trial comparing the effects of post placement on failure rate of postendodontic restorations: preliminary results of a mean period of 32 months. J Endod 35(11):1477–1482. doi:10.1016/j.joen.2009.07.026
Sterzenbach G, Franke A, Naumann M (2012) Rigid versus flexible dentine-like endodontic posts-clinical testing of a biomechanical concept: seven-year results of a randomized controlled clinical pilot trial on endodontically treated abutment teeth with severe hard tissue loss. J Endod 38(12):1557–1563. doi:10.1016/j.joen.2012.08.015
Bitter K, Glaser C, Neumann K, Blunck U, Frankenberger R (2014) Analysis of resin-dentin interface morphology and bond strength evaluation of core materials for one stage post-endodontic restorations. PLoS ONE 9(2), e86294. doi:10.1371/journal.pone.0086294
Tay FR, Pashley DH (2007) Monoblocks in root canals: a hypothetical or a tangible goal. J Endod 33(4):391–398. doi:10.1016/j.joen.2006.10.009
Naumann M, Koelpin M, Beuer F, Meyer-Lueckel H (2012) 10-year survival evaluation for glass-fiber-supported postendodontic restoration: a prospective observational clinical study. J Endod 38(4):432–435. doi:10.1016/j.joen.2012.01.003
Rasimick BJ, Wan J, Musikant BL, Deutsch AS (2010) A review of failure modes in teeth restored with adhesively luted endodontic dowels. J Prosthodont 19(8):639–646. doi:10.1111/j.1532-849X.2010.00647.x
Tay FR, Loushine RJ, Lambrechts P, Weller RN, Pashley DH (2005) Geometric factors affecting dentin bonding in root canals: a theoretical modeling approach. J Endod 31(8):584–589
Mjör IA, Smith MR, Ferrari M, Mannocci F (2001) The structure of dentine in the apical region of human teeth. Int Endod J 34(5):346–353
Sarkis-Onofre R, Skupien JA, Cenci MS, Moraes RR, Pereira-Cenci T (2014) The role of resin cement on bond strength of glass-fiber posts luted into root canals: a systematic review and meta-analysis of in vitro studies. Oper Dent 39(1):E31–44. doi:10.2341/13-070-LIT
Bitter K, Perdigao J, Exner M, Neumann K, Kielbassa A, Sterzenbach G (2012) Reliability of fiber post bonding to root canal dentin after simulated clinical function in vitro. Oper Dent 37(4):397–405. doi:10.2341/11-066-L
Bitter K, Perdigao J, Hartwig C, Neumann K, Kielbassa AM (2011) Nanoleakage of luting agents for bonding fiber posts after thermomechanical fatigue. J Adhes Dent 13(1):61–69. doi:10.3290/j.jad.a18442
De Munck J, Vargas M, Van Landuyt K, Hikita K, Lambrechts P, Van Meerbeek B (2004) Bonding of an auto-adhesive luting material to enamel and dentin. Dent Mater 20(10):963–971
Hikita K, Van Meerbeek B, De Munck J, Ikeda T, Van Landuyt K, Maida T, Lambrechts P, Peumans M (2007) Bonding effectiveness of adhesive luting agents to enamel and dentin. Dent Mater 23(1):71–80. doi:10.1016/j.dental.2005.12.002
Naumann M, Sterzenbach G, Rosentritt M, Beuer F, Frankenberger R (2010) In vitro performance of self-adhesive resin cements for post-and-core build-ups: influence of chewing simulation or 1-year storage in 0.5% chloramine solution. Acta Biomater 6(11):4389–4395. doi:10.1016/j.actbio.2010.05.023
Naumann M, Sterzenbach G, Rosentritt M, Beuer F, Meyer-Luckel H, Frankenberger R (2011) Self-adhesive cements as core build-ups for one-stage post-endodontic restorations? Int Endod J 44(3):195–202. doi:10.1111/j.1365-2591.2010.01797.x
Sterzenbach G, Karajouli G, Tunjan R, Spintig T, Bitter K, Naumann M (2015) Damage of lithium-disilicate all-ceramic restorations by an experimental self-adhesive resin cement used as core build-ups. Clin Oral Investig 19(2):281–288. doi:10.1007/s00784-014-1263-9
Ilie N, Simon A (2012) Effect of curing mode on the micro-mechanical properties of dual-cured self-adhesive resin cements. Clin Oral Investig 16(2):505–512. doi:10.1007/s00784-011-0527-x
Sterzenbach G, Kalberlah S, Beuer F, Frankenberger R, Naumann M (2011) In-vitro simulation of tooth mobility for static and dynamic load tests: a pilot study. Acta Odontol Scand 69(5):316–318. doi:10.3109/00016357.2011.563244
EN ISO 4049 Dentistry—polymer-based filling, restorative and luting materials
Juloski J, Radovic I, Goracci C, Vulicevic ZR, Ferrari M (2012) Ferrule effect: a literature review. J Endod 38(1):11–19. doi:10.1016/j.joen.2011.09.024
Naumann M, Preuss A, Frankenberger R (2006) Load capability of excessively flared teeth restored with fiber-reinforced composite posts and all-ceramic crowns. Oper Dent 31(6):699–704
Naumann M, Preuss A, Frankenberger R (2007) Reinforcement effect of adhesively luted fiber reinforced composite versus titanium posts. Dent Mater 23(2):138–144. doi:10.1016/j.dental.2006.01.002
Naumann M, Sterzenbach G, Rosentritt M, Beuer F, Frankenberger R (2008) Is adhesive cementation of endodontic posts necessary? J Endod 34:1006–1010
Kallio TT, Lastumaki TM, Vallittu PK (2001) Bonding of restorative and veneering composite resin to some polymeric composites. Dent Mater 17(1):80–86
Zicari F, De Munck J, Scotti R, Naert I, Van Meerbeek B (2012) Factors affecting the cement-post interface. Dent Mater 28(3):287–297. doi:10.1016/j.dental.2011.11.003
Blunck U, Zaslansky P (2007) Effectiveness of all-in-one adhesive systems tested by thermocycling following short and long-term water storage. J Adhes Dent 9(Suppl 2):231–240
Blunck U, Zaslansky P (2011) Enamel margin integrity of Class I one-bottle all-in-one adhesives-based restorations. J Adhes Dent 13(1):23–29. doi:10.3290/j.jad.a18445
Frankenberger R, Hehn J, Hajto J, Kramer N, Naumann M, Koch A, Roggendorf MJ (2013) Effect of proximal box elevation with resin composite on marginal quality of ceramic inlays in vitro. Clin Oral Investig 17(1):177–183. doi:10.1007/s00784-012-0677-5
Goracci C, Cury AH, Cantoro A, Papacchini F, Tay FR, Ferrari M (2006) Microtensile bond strength and interfacial properties of self-etching and self-adhesive resin cements used to lute composite onlays under different seating forces. J Adhes Dent 8(5):327–335
Sterzenbach G, Karajouli G, Tunjan R, Spintig T, Bitter K, Naumann M (2014) Self-adhesive resin cements damage lithium disilicate all-ceramic restorations when used as core build-ups. Clin Oral Investig in press
Sterzenbach G, Karajouli G, Tunjan R, Spintig T, Bitter K, Naumann M (2014) Damage of lithium-disilicate all-ceramic restorations by an experimental self-adhesive resin cement used as core build-ups. Clin Oral Investig. doi:10.1007/s00784-014-1263-9
Sterzenbach G, Rosentritt M, Frankenberger R, Paris S, Naumann M (2012) Loading standardization of postendodontic restorations in vitro: impact of restorative stage, static loading, and dynamic loading. Oper Dent 37(1):71–79. doi:10.2341/10-355-L
Acknowledgments
The present study was partly financially supported by 3M ESPE.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Bitter, K., Schubert, A., Neumann, K. et al. Are self-adhesive resin cements suitable as core build-up materials? Analyses of maximum load capability, margin integrity, and physical properties. Clin Oral Invest 20, 1337–1345 (2016). https://doi.org/10.1007/s00784-015-1623-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-015-1623-0