Abstract
Objectives
The aim of this study was to evaluate the physical and mechanical properties of different dual functional cements.
Materials and methods
Three dual functional cements (Allcem Core (FGM), Rebilda DC (VOCO), and LuxaCore Z (DMG)), a luting resin cement (Rely X ARC (3 M ESPE)), and a Core Buildup composite resin GrandioSo (VOCO) were used. Flexural strength (n = 10) and film thickness (n = 6) were evaluated according to ISO 4049:2009. Flow (n = 6) was evaluated according to ISO 6876:2001. Degree of conversion (DC) was assessed immediately and 24 h after polymerization (n = 5). For resistance to dislodgment (RD) analysis, bovine teeth were prepared to receive fiber glass posts, and a push-out test (n = 12) was used.
Results
Luxacore Z presented lower flexural strength when compared to GrandioSo (p < 0.001). No statistical difference was found between cements for film thickness (p = 0.66). Reduced flow values were found for Allcem Core (p = 0.006). No statistical difference was found for immediate DC for different cements (p > 0.05). After 24 h, DC increased for all groups, except for Luxacore Z (p = 0.054). The RD did not differ from the control Rely X ARC, regardless of the root third (p > 0.05). Luxacore Z showed lower mean values in the apical third compared to the coronal third (p = 0.046).
Conclusions
The dual functional cements (Allcem Core and Rebilda DC) possessed similar physical and mechanical properties of luting resin cement (RelyX ARC) and Core Buildup composite resin (GrandioSo). Hence, they could be used for one-stage post and core buildup restorations.
Clinical relevance
The dual functional cements could be used for one-stage post and core buildup restorations since they possess similar physical and mechanical properties of luting resin cements and Core Buildup composite resin.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Rehabilitation of endodontically treated teeth is a challenge in dental practice due to extensive loss of dental tissue in radicular and coronal levels [1]. Limited access, visibility, moisture control, deposition of cementum and dentin, and a high C-factor are some factors that have to be considered when rehabilitation is needed [2]. Different post and core materials have been used to reconstruct root and coronal portions, and resin-fiber posts are the most suitable choice for this rehabilitation due to its physical properties, which are closer to dentin, reducing annual failure rates for this treatment [1, 3, 4].
Upon post-cementation, the rehabilitation of the coronary portion requires a core buildup that bonds to the radicular portion and creates a substrate for a total or partial crown [5]. The interaction between the core and luting material is important for better fracture resistance, and the major advantage of this system is its potential to enhance bond strength between the composite resin and a glass fiber post, creating a so-called mono-block structure with an elastic modulus similar to dentine [6]. This unit promotes a better dissipation of the functional loads when compared to cast posts [7, 8].
Core buildup is usually performed with composite resins with high filler content [9]. However, the objective in post endodontic treatment is to reconstruct the core with the luting agent used for cementation. This technique aims to reduce time necessary for the procedure, the number of materials, and technique sensitivity [10]. Also, possible incompatibilities between materials for luting and core buildup are avoided by using just one material for both applications [5]. To be applied in this technique, however, resin cements should have suitable mechanical properties to support masticatory loads and prevent damage to the remaining tooth structure [11]. To test the materials’ mechanical properties, flexural strength is frequently used [10] and is recommended by standards [12]. Although this technique presents time-saving advantages, the requirements for luting and coronary filling materials are different [12, 13], and some studies have shown controversial results for resin cement’s dual function application [10, 14].
Besides the material’s properties, dentin in the coronal portion and root presents several structural differences that can impair application of the same material [1]. Factors such as heterogeneity in the density and orientation of its tubules, presence of smear layer, moisture control inside the root canal, presence of remaining coronal tooth structure, and adhesive technique sensitivity explain the differences between these structures [2, 15]. The need for flow through the root canal system [16] and the limited light available for conversion of monomers [17] are a concern for successful cementation, and thus, these cements must present suitable physical properties for dual-function applications. Due to these differences, the application of resin cements for both root cementation and coronary filling is not well established. The aim of this study was to evaluate the physical and mechanical properties of core build-up cements.
Methods and materials
Study design
Cements were tested for post-cementation and coronary-filling purposes. For post cementation, Rely X ARC (3M ESPE, Sumaré, SP, Brazil) was used as control, while GrandioSo (VOCO, Germany) was used as control for the coronary filling. Allcem Core (FGM, Joinville, SC, Brazil), Rebilda DC (VOCO, Germany), and Luxacore Z (DMG, Hamburg, Germany) were tested as dual-function materials (post-cementation and coronary filling agents). The materials’ compositions are described in Table 1.
Flexural strength
Cements were tested as coronary filling materials for flexural strength. Ten rectangular specimens (n = 10) with 25 mm × 2 mm × 2 mm were prepared for each group (Allcem Core, Rebilda DC, Luxacore Z and GrandioSo) and stored in distilled water at 37 °C for 24 h before the tests, according to ISO 4049. [12] Flexural strength was determined with the three-point test at a cross-head speed of 0.75 mm/min in a universal testing machine (DL2000, EMIC, São José dos Pinhais, PR, Brazil) until the specimens fractured. Flexural strength was calculated from the following equation:
where F is the maximum load exerted on the specimen, Ɩ is the distance (mm) between the supports ± 0.01 mm, b is the width (mm) of the specimen immediately prior to testing, and h is the height (mm) of the specimen measured with a digital caliper immediately prior to testing.
Film thickness
Cements indicated for post-cementation were used in film-thickness analysis (n = 6) according to ISO 6876 [13]. Two glass plates with 200 mm2 and 5 mm thickness, respectively, were used. The thickness of paired glass plates was measured, and 0.02 ml of the cement was mixed and dispensed in the center of the inferior plate and then covered with the other, in the same orientation from the paired-glass measure. A constant load of (150 ± 2)N was applied centrally in the superior plate during (180 ± 10)s. The thickness of the plates was measured again, and the difference between first and second measurement was recorded as the film thickness.
Flow
Post-cementation materials were tested for flow ability (n = 6) according to ISO 6876 [13]. Two glass plates with 200 mm2 and 5 mm thickness, respectively, were used. Cements were mixed, and 0.05 (± 0.005) ml of cement was dispensed in the center of one plate and then covered with a second plate. A load (100 g) was applied for 10 min, the largest diameters of the cement were measured and the mean value was recorded.
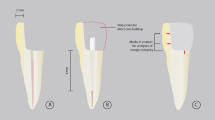
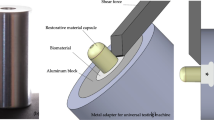
Resistance to dislodgment
Materials indicated for post-cementation were tested for resistance to dislodgment through a push-out test. Forty-eight freshly extracted bovine teeth were randomly assigned to each group (n = 12). Only teeth with straight roots, narrow canals, and a root length of at least 15 mm were selected for this analysis. External debris were removed with a periodontal curette, and the crown surfaces of each tooth were sectioned below the cement–enamel junction perpendicular to the long axis, using a slow-speed diamond disk under water coolant. The radicular pulp was removed using an no 30 K-file (Maillefer-Dentsply, Ballaigues, Switzerland) and irrigation with distilled water. The post space of each root was enlarged with an no 3 drill from the Exacto post system (Angelus, PR, Brazil), with a working length of 11 mm. The no 3 fiber post had 17 mm of length, 2 mm of cervical diameter, and 1.1 mm of apical diameter. Roots were protected with an aluminum blade prior to insertion of cement to protect them from external light energy during the posts’ cementation. The fiber posts were cleaned with 96% ethanol, and the silane (Angelus, PR, Brazil) was applied with disposable microbrush tips. Intracanal dentin was etched with 37% phosphoric acid for 15 s, rinsed with distilled water for 15 s and then gently dried with absorbent paper points. A 3-step total-etch adhesive system (Scotch Bond Multi-Purpose Plus, 3M ESPE) was applied to the moist dentin with a disposable microbrush. Afterward, the cement was dispensed into the post space with intra-oral tips from each cement system or with a Centrix syringe (Centrix Inc., Shelton, CT), and the fiber post was inserted. Light activation was performed through the cervical portion of the root for 20 s at the buccal and lingual surfaces, for a total of 40 s of light exposure, with 5 mm of distance between source and root. The resin cement and adhesive were light activated with an LED (Radii, SDI, Australia) under 1200 mW/cm2 light intensity. The power of the light-curing unit was gauged with a radiometer (Model 100, Demetron Research Group, Danbury, CT, USA). Roots were stored in 37 °C distilled water for 7 days and then serially sectioned into 0.7-mm-thick slices in a precision-cutting machine (Isomet Low Speed Saw, Buehler) under constant water cooling. Slices were stored in 37 °C distilled water for 24 h before push-out tests were performed. The cervical and apical diameter of the canal and the thickness of all of the slices were measured with a digital caliper. Each section was marked on its apical side and positioned on a base, with a central hole, in a universal testing machine (DL2000, EMIC, São José dos Pinhais, PR, Brazil). The push-out test was performed by applying a compressive load to the apical side of each slice by using a 0.7-mm diameter cylindrical plunger attached to the upper portion of the testing machine. A crosshead speed of 1 mm/min was applied until bond failure occurred. To express the bond strength in megapascals (MPa), the load upon failure was recorded in newtons (N) and divided by the bond area (mm2) [18].
Degree of conversion
All materials were tested for degree of conversion (DC) by Raman spectroscopy (SENTERRA Bruker Optics, Ettlingen, Germany), a diode laser of 785 nm wavelengths and 100 mW of intensity, for 5 s and 3 co-additions. Five specimens were prepared (n = 5). A total of 0.03 g of each material was dispensed in a 4 × 1 mm mold for monomer analysis. Then, the specimens were light cured for 40 s with an LED (Radii, SDI, Australia) under 1200 mW/cm2 light intensity and analyzed immediately and after 24 h. To calculate the degree of conversion, the absorbance in the spectrum peaks of aliphatic carbon bonds at 1640 cm−1 and aromatic carbon bonds 1610 cm−1 in the monomer and in the polymer spectrums was considered, with the equation:
Statistical analysis
The sample size for push-out tests, flexural strength, degree of conversion, film thickness, and flow was calculated in accordance with other studies that used similar tests [19,20,21] considering a study power of 80% and a significance level of 5%, with Sigma Plot 12.0. The normality of data was evaluated using the Shapiro-Wilk test. For flexural strength, film thickness and flow, a one-way ANOVA test was used. For the immediate and after 24 h DC, a one-way ANOVA test was used to compare the materials at the same time, and a Student’s paired t test was used to compare different times within the same material. The resistance to dislodgment data was submitted to a log transformation and to a two-way ANOVA test to compare different materials in the same root third and to compare different root thirds within the same material. Tukey was used as a post hoc test.
Results
Results for flexural strength in coronary-filling materials are shown in Table 2. Luxacore Z presented lower values for flexural strength when compared to GrandioSo (p < 0.001). No statistical difference was found between Allcem Core, Rebilda DC and GrandioSo (p > 0.05). For post-cementation materials, no statistical difference was found for film thickness (p = 0.66). Allcem Core presented a lower mean value in flow analysis (p = 0.006). No statistical difference was found for resistance to dislodgement between the different tested cements, as shown in Table 3. Within the same cement, Luxacore Z showed reduced push-out values in the apical third compared to the coronal third (p = 0.046). The most prevalent failure mode was at the dentine/cement interface (Fig. 1). Table 4 shows the DC results. No statistical difference between tested cements and control groups was found for immediate DC. After 24 h, Luxacore Z showed no increase when compared to immediate (p = 0.054).
Discussion
The application of resin cements as buildup core materials has been explored due to its potential to reduce the time of procedure and technique sensitivity. Despite the simplification advantages, differences in root and coronary dentin structure [2], and different requirements for each application [10], it is not well established whether resin cements can be used for both post-cementation and coronary filling. According to the results of the present study, all resin cements fulfilled the tested requirements. Similar results were found for these cements compared to the cement used for post-cementation (RelyX ARC) and a composite resin used for reconstruction of the coronary portion (GrandioSo).
To allow adhesive restoration of endodontically treated teeth in a post and core procedure, however, the mechanical properties of resin cements are not always as high as is required for this application [10]. In the present study, the flexural strength was tested as the ability of the cements to resist masticatory loads for coronary reconstruction. All tested cements in this study showed values greater than 80 MPa, which is the minimum recommended value for polymeric restorative materials [12], and thus, the mechanical properties are suitable for core build-up reconstruction. GrandioSo, as a condensable resin, was used as control and showed higher values due to the higher content of inorganic particles [22]. Despite the differences in the amount and type of filler (Table 1), all tested cements showed adequate values for flexural strength according to ISO 4049 [12]. Interestingly, the lowest value in flexural strength was found for Luxacore Z (82.94 Pa), which presented the highest amount of filler when compared to the other resin cements in Table 1. This result may be related to the zirconium dioxide used as filler in this cement, as the silanization process in this case may not be as efficient as for other fillers, influencing the mechanical strength of the material [23]. Increased filler content, however, is not always possible for cements when post-cementation is indicated because of the need for flow inside the root canal system [16].
The filler content in resin cements can influence flow and film thickness. The ability to flow through root structure and create a thin film in the dentin/post interface is required for better adaptation of the post. The cements used in the present study fulfilled the requirements of ISO 6876 [13], despite the differences found between commercial brands. Also, no statistical difference was found between the tested materials and the control group. Within a thick cement film, more monomers are available to react and convert into polymers, generating a higher polymerization shrinkage [24]. This is related to the quality of the adhesion between the tooth and the composite and impacts the mechanical load supported by the restoration [25]. As is known, the C-factor of the root canal is higher than it is in coronary restorations, exceeding 200, and the shrinkage stress could exceed the bond strength, causing debonding or gaps and voids [26]. This can result in failure and may be avoided by an adequate conversion of monomers inside the root canal.
The degree of conversion (DC) of resin cements is important for the treatment as, in the case of post cementation, conversion of monomers depends on both light curing and self-curing [27]. Contrary to opaque posts, translucent fiber posts can transmit light, increasing polymerization of dual-cured resin cements and also the curing depth. However, even translucent fiber posts can reduce light transmission to less than 40% and might not guarantee sufficient polymerization of resin cements [17]. To guarantee polymerization in the apical region, dual cements were used for fiber post-cementation. As seen in the DC results (Table 4), the immediate values were similar for all materials, and an increase was observed after 24 h. This increase can be assigned to the continuous chemical polymerization during this 24 h in dual cements [28]. This dual polymerization system is not found for composite resin GrandioSo, which showed reduced values for DC after 24 h. Besides the polymerization method, the increased filler content in this resin resulted in reduced mobility of the monomer chain [15], which can influence DC values. Although the value for GrandioSo was lower than the values for the cements, this did not influence its application for coronary reconstruction.
Push-out tests are recommended to determine the bond strength of fiber posts to root dentin because they are able to distribute stress more homogeneously and produce less variability in mechanical testing results, fewer pretest failures and lower standard deviation [29]. The push-out bond strength is related to the degree of conversion of monomers in deep regions of the canal system and to the ability of this cement’s to fill spaces between the post and the root dentin [30]. In the present study, bond strength was similar for cements in all root thirds, which was expected, as adequate properties were observed in DC, flow and film thickness. Luxacore Z, however, presented lower values for the apical third, which is related to the filler used in this material. Zirconia particles are used as filler for this cement, and its high opacity may reduce light transmission during photoactivation. This can lead to reduced monomer conversion in the apical region and reduced mechanical properties of the material, leading to a less-stable bonding [31]. A long-term analysis of resistance to dislodgement was not performed in the present study, but it could elucidate the influence of tested variables in the longitudinal bond strength [19].
Failure in cementation can be related to a gradual loss of retention and is exacerbated by the polymerization shrinkage of cementing agents [15], and this may influence the complete filling of the canal. In this study, All Cem Core presented lower values in the flow test, which may influence the fulfillment of the root canal. Despite the lower values, flow results are in accordance with ISO 6876 [13], and it is thus expected that this reduction will not impair the material’s function as a post-cementation agent. To avoid incomplete filling and minimize the inclusion of air bubbles, the cements were inserted into the post space using a syringe for push-out specimen preparation. These problems in cementation are associated with decreasing bond strength and, consequently, predisposing posts for dislodgment [32, 33]. Some studies have also reported that the reduction of bond strength from the cervical to the apical root third can be attributed to differences in root deep dentin, apical sclerosis, higher cavity configuration factor, the difficulty of visualization, and access to the apical part of the root canal as well as restricted flow of the resin core materials [2, 33]. Also, some factors related to the endodontic treatment can influence bond strength. The root canals were not endodontically treated before the post space preparation, and this can be a limitation for the present study. Remnants of sealers, eugenol, gutta-percha, and other intracanal medicine might interfere in the adhesive process, thus reducing bond strength [24]. Eugenol-based sealer reduces the immediate push-out bond strength of fiber posts luted to root canal with resin cement, regardless of the type of adhesive system or resin cement used [34]. Values for bond strength in the push-out test showed adequate results, and Allcem Core and Rebilda DC showed results comparable to the cementation control RelyX ARC.
Conclusion
The dual functional cements (Allcem Core and Rebilda DC) possessed similar physical and mechanical properties of luting resin cement (RelyX ARC) and Core Buildup composite resin (GrandioSo). Hence, they could be used for one-stage post and core buildup restorations.
References
Dietschi D, Duc O, Krejci I, Sadan A (2008) Biomechanical considerations for the restoration of endodontically treated teeth: a systematic review of the literature, part II (evaluation of fatigue behavior, interfaces, and in vivo studies). Quintessence Int Berl Ger 1985 39:117–129
Mjör IA, Smith MR, Ferrari M, Mannocci F (2001) The structure of dentine in the apical region of human teeth. Int Endod J 34:346–353
Bitter K, Noetzel J, Stamm O, Vaudt J, Meyer-Lueckel H, Neumann K, Kielbassa AM (2009) Randomized clinical trial comparing the effects of post placement on failure rate of postendodontic restorations: preliminary results of a mean period of 32 months. J Endod 35:1477–1482. https://doi.org/10.1016/j.joen.2009.07.026
Dietschi D, Duc O, Krejci I, Sadan A (2007) biomechanical considerations for the restoration of endodontically treated teeth: a systematic review of the literature--part 1. Composition and micro- and macrostructure alterations. Quintessence Int Berl Ger 1985 38:733–743
Cotes C, Cardoso M, de Melo RM et al (2015) Effect of composite surface treatment and aging on the bond strength between a core build-up composite and a luting agent. J Appl Oral Sci Rev FOB 23:71–78. https://doi.org/10.1590/1678-775720140113
Tay FR, Pashley DH (2007) Monoblocks in root canals: a hypothetical or a tangible goal. J Endod 33:391–398. https://doi.org/10.1016/j.joen.2006.10.009
Agrawal A, Mala K (2014) An in vitro comparative evaluation of physical properties of four different types of core materials. J Conserv Dent JCD 17:230–233. https://doi.org/10.4103/0972-0707.131782
Schmitter M, Rammelsberg P, Lenz J, Scheuber S, Schweizerhof K, Rues S (2010) Teeth restored using fiber-reinforced posts: in vitro fracture tests and finite element analysis. Acta Biomater 6:3747–3754. https://doi.org/10.1016/j.actbio.2010.03.012
Naumann M, Koelpin M, Beuer F, Meyer-Lueckel H (2012) 10-year survival evaluation for glass-fiber-supported postendodontic restoration: a prospective observational clinical study. J Endod 38:432–435. https://doi.org/10.1016/j.joen.2012.01.003
Bitter K, Schubert A, Neumann K, Blunck U, Sterzenbach G, Rüttermann S (2016) Are self-adhesive resin cements suitable as core build-up materials? Analyses of maximum load capability, margin integrity, and physical properties. Clin Oral Investig 20:1337–1345. https://doi.org/10.1007/s00784-015-1623-0
Sterzenbach G, Karajouli G, Tunjan R, Spintig T, Bitter K, Naumann M (2015) Damage of lithium-disilicate all-ceramic restorations by an experimental self-adhesive resin cement used as core build-ups. Clin Oral Investig 19:281–288. https://doi.org/10.1007/s00784-014-1263-9
ISO 4049 (2009) Dentistry - Polymer-based restorative materials. https://www.iso.org/standard/42898.html. Accessed 4 Feb 2018
ISO 6876 (2012) Dentistry - Root canal sealing materials. In: ISO. http://www.iso.org/iso/catalogue_detail.htm?csnumber=45117. Accessed 19 Jun 2016
Naumann M, Sterzenbach G, Rosentritt M, Beuer F, Meyer-Lückel H, Frankenberger R (2011) Self-adhesive cements as core build-ups for one-stage post-endodontic restorations? Int Endod J 44:195–202. https://doi.org/10.1111/j.1365-2591.2010.01797.x
Pulido CA, de Oliveira Franco APG, Gomes GM, Bittencourt BF, Kalinowski HJ, Gomes JC, Gomes OMM (2016) An in situ evaluation of the polymerization shrinkage, degree of conversion, and bond strength of resin cements used for luting fiber posts. J Prosthet Dent 116:570–576. https://doi.org/10.1016/j.prosdent.2016.02.019
Jager S, Balthazard R, Dahoun A, Mortier E (2016) Filler content, surface microhardness, and rheological properties of various Flowable resin composites. Oper Dent 41:655–665. https://doi.org/10.2341/16-031-L
Bahari M, Savadi Oskoee S, Kimyai S et al (2014) Effect of light intensity on the degree of conversion of dual-cured resin cement at different depths with the use of translucent Fiber posts. J Dent Tehran Iran 11:248–255
Zicari F, Couthino E, De Munck J et al (2008) Bonding effectiveness and sealing ability of fiber-post bonding. Dent Mater 24:967–977. https://doi.org/10.1016/j.dental.2007.11.011
Leitune VCB, Collares FM, Werner Samuel SM (2010) Influence of chlorhexidine application at longitudinal push-out bond strength of fiber posts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 110:e77–e81. https://doi.org/10.1016/j.tripleo.2010.04.046
Lopes C de CA, Rodrigues RB, Silva ALFE et al (2015) Degree of conversion and mechanical properties of resin cements cured through different all-ceramic systems. Braz Dent J 26:484–489. https://doi.org/10.1590/0103-6440201300180
Chávez-Lozada J, Urquía-Morales MDC (2014) In vitro evaluation of the film thickness of self-etching resin cements. Acta Odontol Latinoam AOL 27:145–150. https://doi.org/10.1590/S1852-48342014000300008
Rodrigues Junior SA, Zanchi CH, de Carvalho RV, Demarco FF (2007) Flexural strength and modulus of elasticity of different types of resin-based composites. Braz Oral Res 21:16–21
Provenzi C, Collares FM, Cuppini M et al (2018) Effect of nanostructured zirconium dioxide incorporation in an experimental adhesive resin. Clin Oral Investig:1–10. https://doi.org/10.1007/s00784-017-2311-z
Kremeier K, Fasen L, Klaiber B, Hofmann N (2008) Influence of endodontic post type (glass fiber, quartz fiber or gold) and luting material on push-out bond strength to dentin in vitro. Dent Mater 24:660–666. https://doi.org/10.1016/j.dental.2007.06.029
Rojpaibool T, Leevailoj C (2017) Fracture resistance of Lithium Disilicate ceramics bonded to enamel or dentin using different resin cement types and film thicknesses. J Prosthodont 26:141–149. https://doi.org/10.1111/jopr.12372
Tay FR, Loushine RJ, Lambrechts P et al (2005) Geometric factors affecting dentin bonding in root canals: a theoretical modeling approach. J Endod 31:584–589
Marques de Melo R, Bottino MA, Galvão RKH, Soboyejo WO (2012) Bond strengths, degree of conversion of the cement and molecular structure of the adhesive-dentine joint in fibre post restorations. J Dent 40:286–294. https://doi.org/10.1016/j.jdent.2012.01.003
Cerutti F, Acquaviva PA, Gagliani M, Ferrari M, Mangani F, Depero LE, Cerutti A (2011) Degree of conversion of dual-cure resins light-cured through glass-fiber posts. Am J Dent 24:8–12
Goracci C, Grandini S, Bossù M, Bertelli E, Ferrari M (2007) Laboratory assessment of the retentive potential of adhesive posts: a review. J Dent 35:827–835. https://doi.org/10.1016/j.jdent.2007.07.009
Bohrer TC, Fontana PE, Wandscher VF et al (2018) Endodontic sealers affect the bond strength of Fiber posts and the degree of conversion of two resin cements. J Adhes Dent:1–8. https://doi.org/10.3290/j.jad.a40301
Inokoshi M, Pongprueksa P, De Munck J et al (2016) Influence of light irradiation through zirconia on the degree of conversion of composite cements. J Adhes Dent 18:161–171. https://doi.org/10.3290/j.jad.a35842
Penelas AG, Piedade VM, Borges ACO d S, Poskus LT, da Silva EM, Guimarães JGA (2016) Can cement film thickness influence bond strength and fracture resistance of fiber reinforced composite posts? Clin Oral Investig 20:849–855. https://doi.org/10.1007/s00784-015-1568-3
Souza AC, Gonçalves Fde C, Anami LC, Melo RM, Bottino MA, Valandro LF (2015) Influence of insertion techniques for resin cement and mechanical cycling on the bond strength between fiber posts and root dentin. J Adhes Dent 17:175–180. https://doi.org/10.3290/j.jad.a33993
Altmann ASP, Leitune VCB, Collares FM (2015) Influence of eugenol-based sealers on push-out bond strength of Fiber post Luted with resin cement: systematic review and meta-analysis. J Endod 41:1418–1423. https://doi.org/10.1016/j.joen.2015.05.014
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
This study was not supported for source of founding.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Walcher, J.G., Leitune, V.C.B., Collares, F.M. et al. Physical and mechanical properties of dual functional cements—an in vitro study. Clin Oral Invest 23, 1715–1721 (2019). https://doi.org/10.1007/s00784-018-2598-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-018-2598-4