Abstract
Objectives
The aim of this study was to evaluate the retention forces (RFs) of zirconia double-crown systems, with primary and secondary crowns made from zirconia in vitro.
Materials and methods
Ten maxillary models with six abutment teeth were prepared. Sixty inner crowns were fabricated from pre-sintered zirconia with a taper of 0°. Ten 14-unit telescopic prostheses (removable partial dentures, RDPs) were fabricated, using the same computer-aided design/computer-aided manufacturing system as that used for the inner crowns. The removal test was performed in a standardized setup using a universal testing device at a crosshead speed of 10 mm/min. Ten separation cycles were carried out for each single primary crown as well as for each 14-unit RDP in the presence of artificial saliva. The results were imported into a statistic program and analysed by a one-way ANOVA and post hoc tests. The level of significance was set at 5 %.
Results
The mean RFs of the single double-crown systems were in the range of 0.611–2.895 N, whereas the RFs for the whole RDP varied between 8.1 and 13.6 N. RF was dependent on the abutment tooth (p < 0.001) and on the model (p < 0.001).
Conclusions
The results of this study indicate that the manufacturing of full-zirconia double-crown systems is possible as well as reproducible. The RFs are comparable to those reported from casted and electroformed double-crown systems.
Clinical relevance
It has been shown that the RFs of the presented telescopic system are comparable to existing double-crown systems.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Removable partial dentures (RDPs) have been a reliable and popular method for treating partially edentulous patients for decades [1–3]. Despite the popularity of this method, Hummel et al. reported that only one third of RDPs are considered satisfactory [4]. This is of paramount importance, especially because another study found that RDP quality influences individuals’ oral health-related quality of life to a clinically significant extent [5]. RDPs can be supported by various retentive elements. However, clasps or double-crown systems are the most popular elements and can be fabricated from different materials [2, 6–8]. Although clasp-retained dentures have been reported to have measurably lower failure rates, the repair costs are more than twice as high as those for double-crown systems [6]. Loss of cementation of the primary crowns was the most frequently reported clinical failure [3, 6]. Concerning double-crown systems, many different designs are used to cover different fields of application and to provide the necessary retention forces (RFs). Conical systems are based on the spring tension of the outer crown, due to the geometry of the surfaces and an occlusal gap of 10–80 μm between the inner and the outer crown [9]. RFs can be adjusted by varying the taper of the inner crown. In contrast, cylindrical telescopic systems use a taper of 0°, and the RFs are based on friction between the surfaces of the inner and outer crowns. The effect of the parallel-sided crowns can be compared to a piston/cylinder system, although the required casting precision is not achievable through analogue dental laboratory technology [9]. Weigl et al. reported a new telescopic system, consisting of zirconia primary crowns and electroformed secondary crowns, that uses adhesion instead of friction for the retention of the system [2, 7]. Although the system showed favourable tribological properties and was widely reproducible due to its automated electroforming process [2, 7], it should be considered that many different materials (ceramic, electroplated gold, bonding and CrCoMb alloy as the denture framework) are involved in this approach. This might lead to an issue of biocompatibility. Recent developments in the field of computer-aided design (CAD)/computer-aided manufacturing (CAM) have made it easier to process different materials of high quality, in particular ceramics [10–13]. The manufacturing of zirconia is becoming increasingly popular due to its high biocompatible and aesthetic potential as well as its high mechanical strength [11, 14–17]. It has a wide field of application and can be used for various sizes of frameworks [18–22], implant abutments, monolithic crowns [23], monolithic restorations [24] and primary crowns [25]. However, to the authors’ best knowledge, no literature is available on the use of all-zirconia double-crown systems without any galvanic elements. Therefore, the aim of this study was to manufacture an RDP with six zirconia primary crowns and a 14-unit zirconia secondary framework in order to determine the RFs of each single telescopic system as well as the RFs of the whole secondary framework.
The working hypothesis is that the RFs achieved by the present approach are in the same range as the RFs of standard double-crown systems reported in the literature.
Materials and methods
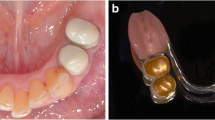
Ten maxillary models, each with six prepared teeth (FDI 17, 15, 13, 23, 25 and 27), were fabricated from class IV resin-reinforced (ISO type IV) die stone (Resin Rock, Whip Mix, Dortmund, Germany) and trimmed to a height of 18 mm. Each abutment tooth and each pontic were provided with two pins (Jet Pin 2.0 mm, Jan Langner GmbH, Schwäbisch-Gmünd, Germany), and the base of the cast was poured from an ISO type IV dental stone (Suppen-Sockler (G) Das Orginal, Picodent, Wipperfürth, Germany). The working models were finished by separating all abutment teeth, and the dies were trimmed to the preparation margins. All models were scanned with a white-light projector scanner (S600, Zirkonzahn, Gais, Italy). Sixty primary crowns were designed with special software (CAD/CAM telescopic crowns, Zirkonzahn), using the same parameters for each of the 10 models concerning the thickness of the cement spacer, the start of the cement spacer, the wall thickness and the height of the friction area. The details are provided in Table 1. The computer numeric control (CNC) data were sent to a 5 + 1 axes milling unit (M5, Zirkonzahn) and milled from semi-sintered zirconia blanks (ICE Zirkon Translucent 95H18, Zirkonzahn). The sintering was performed in a special furnace (600/V2, Zirkonzahn) at a temperature of 1,500 °C, using the standard sintering programme. All primary crowns were returned to the corresponding model and adapted according to the literature [12, 26]. In the case of incomplete seating, colour (Bite-X Artikulationspaste, Asami Tanaka Dental Enterprises Europe GmbH, Friedrichsdorf, Germany) was applied to the abutment teeth, and the primary crowns were placed cautiously. Red spots and traces on the inner surface of the primary crowns were removed by using a red ring diamond bur (#201 and #202, Zirkonzahn), until uniform contact between the inner crown and the abutment tooth was achieved. In order to maintain the same path of insertion for all six primary crowns of each model, each testing model was measured on a model table. A transmission device was used for the manufacturing of a milling base with resin dies (GC Pattern resin LS, GC Corp., Tokyo, Japan). The primary crowns were ground and polished by using two special bur kits for zirconia (sets 4439 and 4589, Komet, GEBR BRASSELER GmbH & Co KG, Lemgo, Germany) with a taper of 0°. The milling was conducted with an electric, high-speed hand piece (W&H Perfecta 900, W&H Dentalwerk Bürmoos GmbH, Bürmoos, Austria) with water cooling, mounted in a surveyor (F1, DeguDent, Hanau, Germany). Next, the primary crowns were set back to the abutment teeth of each model and were temporarily fixed (Fit-checker, GC Corp.). The primary crowns were coated with silicon adhesive, and each of the 10 models was duplicated (Adisil blau 9:1, Siladent, Goslar, Germany). Ten master casts were fabricated from pattern resin (GC Pattern Resin LS, GC Corp) dies and class IV resin-reinforced (ISO type IV) die stone (Resin Rock, Whip Mix), which fulfilled the requirement for a rigid model with no mobility of the abutment teeth. As the angle of 0° is prone to axis deviations, all primary crowns were set back into the master casts, and each model was placed on a model table in order to check the path of insertion. If deviations were detected, the primary crowns were ground and polished again (Set 4589, Komet). Furthermore, the transitions from the axial walls to the occlusal surfaces of all primary crowns were rounded and polished (Set zirconia polishers disc ZZ461, Zirkonzahn) to avoid edges and sharp corners. Finally, all primary crowns were polished with a special zirconia polishing paste (Organical Zirkon-Polierpaste, R+K CAD/CAM Technologie GmbH & Co KG, Berlin, Germany) to achieve the highest surface quality possible (Fig. 1). Next, all primary crowns were placed back in each master cast, and a thin layer of scan spray (Zirko Scanspray, Zirkonzahn) was applied to the model as well as to the outer surface of the primary crowns to reduce reflection. Each of the 10 models was scanned (S600, Zirkonzahn) using a multitooth scan and completed with single scans of each abutment tooth, in order to improve the data quality. The parameters used for the design of the secondary crowns as well as the frameworks are listed in Table 2. The 14-unit frameworks were designed in full contour, shrank by 0.8 mm, maintaining a minimum wall thickness of 0.5 mm, and were then transferred to the CAM program. Each of the 10 frameworks was milled for about 6 h (M5, Zirkonzahn) and then sintered to full density in a special furnace (600/V2, Zirkonzahn) as described above. After the sintering process, the sintering feet were removed, and the primary crowns were provided with pattern resin pins for easier handling during the adaptation process. First, each primary crown was adapted to the corresponding secondary crown using a special spray (Arti-Spray, Dr. Jean Bausch GmbH & Co KG, Köln, Germany). Second, the primary crowns of each model were set back into each master cast, and the whole framework was adapted by making a permanent side comparison and paying particular attention to the occlusal height. The adaptation process was carried out with diamond stones (#311, Zirkonzahn), diamond burs (#101 Flat End Taper, Zirkonzahn) and predominantly by polishing sticks (FINOPOL DIA Pinpolierer rough, middle and fine, FINO GmbH, Bad Bocklet, Germany). Finally, the adjustment of the retention forces was performed with special brushes (Polirapid Pinselbürsten Chungking black, Polirapid, Germany) and zirconia polishing paste (Organical Zirkon-Polierpaste, R+K CAD/CAM Technologie GmbH & Co KG) (Figs. 3, 4 and 5). The production of the primary crowns as well as the construction and the adjustment of the secondary frameworks were performed by the same calibrated dental technician.
For the testing of the RFs, both the single crowns and the whole framework of each model were measured separately. Special screws were attached (GC Pattern resin LS, GC Corp.) to the inner surface of the primary crowns (Fig. 2). The measurements of the RFs were carried out with a universal testing machine (Zwick Type 1445, Zwick/Roell, Ulm, Germany), using a 500-N load cell and a test speed of 10 mm/min. The inner surface of each abutment tooth of each framework was aligned parallel to the removal direction during the testing. Therefore, the secondary framework was embedded in light curing resin (Individo Lux bl.-opak OK 2402, VOCO, Cuxhaven, Germany) and then mounted on the especially designed model table shown in Fig. 3. This model table was equipped with a ball bearing system and a locking mechanism in the foot. When the inner surface of the secondary crown was axially aligned to the pulling direction, the locking mechanism in the foot was closed in order to fix this position during the testing procedure. Furthermore, a wire of 1 m was utilized to prevent horizontal tension on the primary crown and additionally to take advantage of self-alignment along the long axis. Ten separation cycles of each abutment tooth were performed in the presence of artificial saliva (Glandosane, cell pharm GmbH, Bad Vilbel, Germany). After the testing of the single crowns, all inner crowns were bonded (Panavia F 2.0, Kuraray Europe GmbH, Hattersheim am Main, Germany) to the abutment teeth of the corresponding testing models. The testing of the RFs of the whole frameworks was performed at least 24 h after bonding, as mentioned above. Therefore, each model was mounted on a special model table, in the centre of the machine that was especially constructed for the testing device (Zwick type 1445, Zwick/Roell) in order to align all the primary crowns of each model in the pulling direction and to avoid axis deviations. Three wires of about 1 m fixed the frameworks between 15 and 16, 11 and 21 as well as 25 and 26 and were united at the attachment of the load cell (Fig. 3). Ten separation cycles of each framework were carried out at a test speed of 10 mm/min in the presence of artificial saliva (Glandosane, cell pharm GmbH). The collected results were imported into a statistical program (SPSS 20.0, SPSS Inc., Munich, Germany) and analysed. Descriptive analysis was carried out to evaluate the RF of each abutment tooth, depending on the model as well as the range of RFs of each abutment tooth and of each model. Furthermore, statistical analysis, with a significance level of 5 %, was performed by a one-way ANOVA and a post hoc test (Student–Newman–Keuls, SNK), comparing the different abutment teeth.
Results
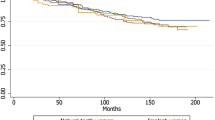
The mean RFs for the single telescopic systems were in the range of 0.611–2.895 N (Fig. 4). The values of the mean RFs for the whole secondary construction varied between 8.1 and 13.6 N. Comparing the abutment teeth separately, the model (p < 0.001) had a significant influence on the RFs according to the analysis of variance. The abutment teeth (p < 0.001) had a significant influence on the RFs. The cuspid showed significantly lower RF compared to the premolar (SNK, p = 0.213) and molar abutments. However, no differences between the premolar and molar abutments were detected (SNK, p = 0.213).
Discussion
The RFs of double-crown systems depend on several different factors and therefore range within a wide distribution of values. Considering the parameters affecting the RFs of double-crown systems, the material, the abutment height, the taper [25] as well as the saliva [27] have been reported to have influence. Bayer et al. reported median RFs of 1.93 N for double crowns with a taper of 1–2° from high-gold alloy [27], 3 N for 0° gold primary crowns and cast female parts and 6.54 N for 2° gold primary crowns and electroplated female parts [28]. Other studies that examined the mean RFs of zirconia primary crowns with electroformed secondary crowns reached RFs of 3.32 N [29] and 0.37–2.65 N [25]. The RFs in the present approach were in the range of 0.611–2.895 N, so the working hypothesis can be accepted, despite some restrictions. Most of the studies examined the RFs of single double crowns; however, this does not correspond to clinical reality, because an RDP normally consists of at least two double-crown systems. In the presented study, each double crown was first adapted individually, whereupon the whole framework consisting of six double crowns was adjusted as a unit. Although the individual fitting and the RF of each double crown seemed to be good, the fitting and RF of the whole framework was different and had to be further adapted. As the RF for the whole framework was usually too high, further adaptation induced lower RFs of each single double crown. Considering this effect, it can be assumed that the measured RFs of single double crowns in previous studies are higher than they are in reality, because they were not adapted within a compound structure of several double crowns.
The primary crowns fabricated for measurement in this study should ideally have had a taper of 0° to imitate the piston/cylinder effect (Fig. 5). The taper of 0° is of particular importance for ceramics, because a cone angle of the primary crowns would lead to tensions within the walls of the secondary crowns. As ceramics, in contrast to gold alloys, are susceptible to tensile stress, this would certainly induce crack formation within the secondary crowns and lead to the destruction of the secondary framework. However, the taper of 0° has often been associated with some fabrication difficulties [25, 27]. Therefore, a precise hand piece (W&H Perfecta 900, W&H Dentalwerk Bürmoos GmbH) with a concentricity of less than 20 μm was chosen. Particular attention was paid to the degree of wear of the diamond bur as well as low pressure during the milling process to avoid axis deviations of the bur.
During the fabrication of the secondary framework, two potential sources of errors can lead to problems concerning the fitting of the telescopic system. First, the scanning of the primary crowns is prone to errors because the reflections of the polished zirconia surfaces lead to scanning bugs, even though a thin layer of scan spray is applied. This causes partially rough areas in the inner surface of the secondary crown, which further complicates the adaptation process of the telescopic system. Second, pre-study trials detected the sintering shrinkage to be problematic. Therefore, one secondary framework was milled three times from the same CNC data and sintered to full density one after the other, using the same furnace and the same programme. Although the conditions for all frameworks were identical, the outcomes always slightly differed concerning the fitting and expanse of the telescopic crowns. This indicates that the sintering shrinkage is calculable to a certain extent, but not totally reproducible.
Full zirconia as well as electroformed double-crown systems [2, 7, 25, 29] and based on adhesion instead of friction and therefore need an aqueous medium, such as saliva, between the primary and the secondary crown. The viscosity as well as a homogenous wetting of the surfaces can influence the RFs of the adhesive system. For the measurement of the RFs, only one artificial saliva product was used; however, it can be assumed that an increase in the viscosity of the saliva would lead to higher RFs. This component should be taken into consideration by adapting the RFs of RDPs in clinical practice.
In this study, the RFs of all telescopic crowns and frameworks were adapted by one calibrated dental technician, because each of the 60 telescopic systems had to be adapted after the sintering of the secondary framework. Although the used CAD/CAM system worked reliably and precisely, each telescopic system required adaptation. However, this corresponds to clinical reality, in which the dental technician checks and determines the fitting of the RFs [27]. Comparing the different abutment teeth, the canines showed the lowest RFs. This effect can be explained by the complex geometry of the canines, which were difficult to adapt due to short palatal and large opposing friction surfaces. The geometry of the premolars and molars was very homogenous and therefore easier to adapt. The molars showed the highest SD due to the biggest surface of the primary crowns. Therefore, the molars needed more manual adaptation and exhibited a bigger range of retention forces due to the manual influence. Concerning the methodology of the measurement setup and the measurement itself, particular attention was paid to avoid any tilting of the single crowns as well as the frameworks during removal, because this would produce excessive RFs. Therefore, a wire of 1 m was utilized to prevent horizontal tensions and take advantage of self-alignment along the long axis. Furthermore, the insertion direction of the single crowns and the frameworks was aligned parallel to the removal direction, and the measurement of each specimen was performed 10 times. In case of any tipping of the telescopic crowns during the testing procedure, the removal test was repeated. As the sum of the mean RFs of the single abutments of each framework was close or identical to that of the RFs of the whole framework, it can be supposed that no tilting occurred during the removal process. The RFs of the presented concept are comparable to those of electroformed telescopic systems [25] and are reproducible within a small range. However, based on this study, no general statements of the long-term RF can be made. Therefore, the results would justify a clinical trial evaluating the presented concept in clinical practice and evaluate the long-term performance. However, it has to be taken into account that only frameworks were tested in this study. There are different options to veneer those frameworks. If a ceramic veneer is used, possible effects on the accuracy caused by the veneering process were discussed when the layering technique was used. Overpressing techniques for zirconia frameworks were introduced as a clinical alternative leading to higher mechanical stability of the whole restoration [17, 30]. Digital veneering with lithium disilicate represents a third option for ceramic veneering. However, the influence on the accuracy of the zirconia frameworks was not reported [31]. If resin-based materials were used for veneering zirconia frameworks, the influence on the accuracy might be of minor importance [32, 33]. Furthermore, most resin-based veneering materials were used for RDPs [34].
The following limitations apply to this study:
-
1.
Only one artificial saliva product was tested.
-
2.
The impact of wear on the RFs was not measured. However, because the presented telescopic system is based on adhesion instead of friction, it can be supposed that less wear occurs compared to conventional double-crown systems.
-
3.
Only one CAD/CAM system and one zirconia material were tested.
-
4.
The primary crowns were directly fabricated on a model without making impressions. Therefore, the presented protocol showed a difference to the clinical workflow.
-
5.
The removal tests were performed on the master model.
Conclusion
Considering the limitations of the study, the following conclusions can be drawn for RDPs fabricated in the described manner:
-
1.
The RFs of the presented approach are comparable to those of electroformed double-crown systems reported in the literature.
-
2.
The RFs of all-zirconia double-crown systems are reproducible.
References
Perel ML (1973) Telescope dentures. J Prosthet Dent 29:151–156
Weigl P, Lauer HC (2000) Advanced biomaterials used for a new telescopic retainer for removable dentures. J Biomed Mater Res 53:337–347
Behr M, Hofmann E, Rosentritt M, Lang R, Handel G (2000) Technical failure rates of double crown-retained removable partial dentures. Clin Oral Investig 4:87–90
Hummel SK, Wilson MA, Marker VA, Nunn ME (2002) Quality of removable partial dentures worn by the adult U.S. population. J Prosthet Dent 88:37–43
Inukai M, Baba K, John MT, Igarashi Y (2008) Does removable partial denture quality affect individuals’ oral health? J Dent Res 87:736–739
Hofmann E, Behr M, Handel G (2002) Frequency and costs of technical failures of clasp- and double crown-retained removable partial dentures. Clin Oral Investig 6:104–108
Weigl P, Hahn L, Lauer HC (2000) Advanced biomaterials used for a new telescopic retainer for removable dentures. J Biomed Mater Res 53:320–336
Koller B, Att W, Strub JR (2011) Survival rates of teeth, implants, and double crown-retained removable dental prostheses: a systematic literature review. Int J Prosthodont 24:109–117
Schunke S (2007) Prinzipielle Funktionsweisen der Doppelkronensysteme. Quintessence Zahntechnik 12:1496–1507
Beuer F, Steff B, Naumann M, Sorensen JA (2008) Load-bearing capacity of all-ceramic three-unit fixed partial dentures with different computer-aided design (CAD)/computer-aided manufacturing (CAM) fabricated framework materials. Eur J Oral Sci 116:381–386
Beuer F, Schweiger J, Edelhoff D (2008) Digital dentistry: an overview of recent developments for CAD/CAM generated restorations. Br Dent J 204:505–511
Beuer F, Aggstaller H, Edelhoff D, Gernet W, Sorensen J (2009) Marginal and internal fits of fixed dental prostheses zirconia retainers. Dent Mater 25:94–102
Abduo J, Lyons K, Swain M (2010) Fit of zirconia fixed partial denture: a systematic review. J Oral Rehabil 37:866–876
Bindl A, Mormann WH (2005) Marginal and internal fit of all-ceramic CAD/CAM crown-copings on chamfer preparations. J Oral Rehabil 32:441–447
Schmitter M, Mussotter K, Rammelsberg P, Gabbert O, Ohlmann B (2012) Clinical performance of long-span zirconia frameworks for fixed dental prostheses: 5-year results. J Oral Rehabil 39:552–557
Choi YS, Kim SH, Lee JB, Han JS, Yeo IS (2012) In vitro evaluation of fracture strength of zirconia restoration veneered with various ceramic materials. J Adv Prosthodont 4:162–169
Chaar MS, Witkowski S, Strub JR, Att W (2013) Effect of veneering technique on the fracture resistance of zirconia fixed dental prostheses. J Oral Rehabil 40:51–59
Quinn GD, Studart AR, Hebert C, VerHoef JR, Arola D (2010) Fatigue of zirconia and dental bridge geometry: design implications. Dent Mater 26:1133–1136
Salazar Marocho SM, Studart AR, Bottino MA, Bona AD (2010) Mechanical strength and subcritical crack growth under wet cyclic loading of glass-infiltrated dental ceramics. Dent Mater 26:483–490
Studart AR, Filser F, Kocher P, Gauckler LJ (2007) Fatigue of zirconia under cyclic loading in water and its implications for the design of dental bridges. Dent Mater 23:106–114
Studart AR, Filser F, Kocher P, Luthy H, Gauckler LJ (2007) Cyclic fatigue in water of veneer-framework composites for all-ceramic dental bridges. Dent Mater 23:177–185
Stawarczyk B, Ozcan M, Roos M, Trottmann A, Hammerle CH (2011) Fracture load and failure analysis of zirconia single crowns veneered with pressed and layered ceramics after chewing simulation. Dent Mater J 30:554–562
Stawarczyk B, Ozcan M, Schmutz F, Trottmann A, Roos M, Hammerle CH (2013) Two-body wear of monolithic, veneered and glazed zirconia and their corresponding enamel antagonists. Acta Odontol Scand 71:102–112
Rojas-Vizcaya F (2011) Full zirconia fixed detachable implant-retained restorations manufactured from monolithic zirconia: clinical report after two years in service. J Prosthodont 20:570–576
Beuer F, Edelhoff D, Gernet W, Naumann M (2010) Parameters affecting retentive force of electroformed double-crown systems. Clin Oral Investig 14:129–135
Beuer F, Aggstaller H, Edelhoff D, Gernet W (2008) Effect of preparation design on the fracture resistance of zirconia crown copings. Dent Mater J 27:362–367
Bayer S, Stark H, Mues S, Keilig L, Schrader A, Enkling N (2010) Retention force measurement of telescopic crowns. Clin Oral Investig 14:607–611
Bayer S, Kraus D, Keilig L, Golz L, Stark H, Enkling N (2012) Wear of double crown systems: electroplated vs. casted female part. J Appl Oral Sci 20:384–391
Engels J, Schubert O, Guth JF, Hoffmann M, Jauernig C, Erdelt K, Stimmelmayr M, Beuer F (2012) Wear behavior of different double-crown systems. Clin Oral Investig 17:503–510
Beuer F, Edelhoff D, Gernet W, Sorensen JA (2009) Three-year clinical prospective evaluation of zirconia-based posterior fixed dental prostheses (FDPs). Clin Oral Investig 13:445–451
Beuer F, Schweiger J, Eichberger M, Kappert HF, Gernet W, Edelhoff D (2009) High-strength CAD/CAM-fabricated veneering material sintered to zirconia copings—a new fabrication mode for all-ceramic restorations. Dent Mater 25:121–128
Ozcan M, Valandro LF, Pereira SM, Amaral R, Bottino MA, Pekkan G (2013) Effect of surface conditioning modalities on the repair bond strength of resin composite to the zirconia core/veneering ceramic complex. J Adhes Dent 15:207–210
Schweiger J, Neumeier P, Stimmelmayr M, Beuer F, Edelhoff D (2013) Macro-retentive replaceable veneers on crowns and fixed dental prostheses: a new approach in implant-prosthodontics. Quintessence Int 44:341–349
Nelson K, Hildebrand D, Mehrhof J (2008) Fabrication of a fixed retrievable implant-supported prosthesis based on electroforming: a technical report. J Prosthodont 17:591–595
Acknowledgments
The authors wish to thank Enrico Steger (Zirkonzahn, Gais, Südtirol, Italy) for supporting the study with the milling unit M5 and all necessary materials. The authors would like to sincerely thank Josef Schweiger (head of the dental laboratory) for his assistance whenever technical problems had to be resolved.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Groesser, J., Sachs, C., Heiß, P. et al. Retention forces of 14-unit zirconia telescopic prostheses with six double crowns made from zirconia—an in vitro study. Clin Oral Invest 18, 1173–1179 (2014). https://doi.org/10.1007/s00784-013-1093-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-013-1093-1