Abstract
Introduction
The bone-specific physical activity questionnaire (BPAQ) provides a bone-relevant index of physical activity participation according to the mechanical loads experienced across the life span.
Materials and methods
We aimed to examine relationships between historical bone-relevant physical activity and pQCT-derived parameters of bone strength. We recruited 532 healthy volunteers (277 males, 255 females) across a broad age range (4–97 years). Peripheral quantitative computed tomography (XCT-3000, Stratec, Germany) was used to examine volumetric bone density, area, and strength indices of the non-dominant tibia and radius. Exercise loading history from birth was determined using the past BPAQ (pBPAQ) score. Pearson correlation analysis was used to examine relationships between pBPAQ scores and pQCT parameters.
Results
Independent of sex, pBPAQ scores were associated with total density at the 38% and 66% tibial sites and the 66% radial site (r = 0.145–0.261, p ˂ 0.05), total area at the 38% tibial site and 4% and 66% radial sites (r = 0.129–0.156, p ˂ 0.05), and strength indices at all measured sites (r = 0.123–0.234, p < 0.05).
Conclusion
We conclude that, independent of sex, historical bone-relevant physical activity is associated with pQCT-derived indices of bone strength, indicating that pBPAQ captures the characteristics of bone loading history that are likely to be relevant adaptive stimuli. A larger sample is required to examine the influence of age on this relationship.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is well known that bone responds and adapts to chronic mechanical loading [1, 2]. Participation in physical activity that imparts large magnitude loads at fast loading rates, such as jumping and heavy resistance training, improves bone mass and strength [3, 4]. Neither duration of exercise nor aerobic intensity (e.g. metabolic equivalents (METs) or oxygen uptake) of physical activity are markedly influential on the adaptive response of bone [5, 6]. It is therefore unsurprising that generic physical activity measurement tools, such as pedometers and physical activity questionnaires that focus on duration and METs, do not provide a valid estimate of physical activity participation that is predictive of bone health or response of bone to exercise.
Unlike nutritional or pharmaceutical interventions which can increase systemic bone mineral density (BMD) measured by dual-energy X-ray absorptiometry (DXA), mechanical loading during exercise induces advantageous site-specific changes in bone size and shape [7, 8]. Even small increases in the size and shape of a bone impart exponential benefits to bone strength and fracture resistance. For instance, long bone bending strength is determined by the cross-sectional moment of inertia, which is related to the cortical cross-sectional area and its distribution about the neutral axis to the fourth power. Thus, any increase in the diameter of a long bone results in an exponentially greater resistance to bending [9, 10]. Peripheral quantitative computed tomography (pQCT) captures such geometric parameters and provides a true volumetric quantification of bone density (vBMD, g/cm3) of the bones of the forearm and leg and is therefore an important additional technology to DXA to detect bone responses to exercise intervention.
The bone-specific physical activity questionnaire (BPAQ) was developed to account for the influence of historical habitual mechanical loading on the skeleton. A simple two-page questionnaire is scored using algorithms incorporating load data for common activities. The questionnaire was designed to capture total lifetime bone-relevant physical activity (tBPAQ) participation, including current participation (i.e. previous year, cBPAQ) and past participation (i.e. from birth to one year prior to questionnaire administration, pBPAQ). We have previously shown that BPAQ scores predict DXA-derived bone mass at clinically important sites in young adults better than other more generic measures of physical activity [11], are related to cardiovascular disease risk factors [12] and exhibit high inter- and intra-rater reliability for all components (ICC = 0.86–0.97) [13]. However, the relationship of lifetime bone-relevant physical activity to important three-dimensional characteristics of bone size and density is yet to be established.
The primary aim of the current study was to examine the relationships between past BPAQ scores and pQCT-derived bone strength parameters for the tibia and radius in a broad sample of men and women across the age span. Secondary aims were to determine if the relationships are sex or age specific.
Materials and methods
Ethics statement
Ethical approval was granted by the Griffith University Human Research Ethics Committee (PES/12/05/HREC, PES/09/09/HREC, PES/25/11/HREC, AHS/07/14/HREC, and 2015/775). Written informed consent was obtained from each volunteer and in the case of child participants, from a parent or guardian. All research activities were conducted in accordance with the Declaration of Helsinki.
Study design
A cross-sectional study design was employed to examine the relationships between historical physical activity participation and pQCT-derived indices of bone strength in a broad sample of healthy male and female participants of all ages.
Subjects and subject selection
Participants older than 4 years of age were recruited from the Gold Coast community via posters, flyers, newspaper advertisements and word-of-mouth. Volunteers were included if they were of sound general health, fully ambulatory, and in the case of child volunteers, had the written consent of a parent or guardian. Participants were excluded if they had an endocrine disorder, metabolic disease, or chronic renal pathology, were taking medications known to affect the musculoskeletal system, or were recovering from lower limb injury requiring immobilisation in the past 12 months. We did not screen for common orthopaedic conditions (e.g. osteoarthritis), menstrual dysfunction, or cognitive impairment given their likely prevalence in a large sample of the general community to maintain the generalisability of the study results.
Biometrics
Height and weight were measured by a member of the research team following standard protocols with participants wearing loose-fitting lightweight clothing (i.e. shirt and shorts) and shoes removed. Height was measured to the nearest millimetre using the stretch-stature method with a wall-fixed stadiometer (HART Sport & Leisure, Brisbane, Australia). Participants stood with feet hip-width apart and back to the wall in front of the stadiometer, took a deep breath in and tucked their chin while the researcher lowered the stadiometer slider to touch the top of the head and recorded their height. Weight was measured to the nearest 0.1 kg using electronic scales (Soehnle Co., Nassau, Germany).
Physical activity
Each participant completed the bone-specific physical activity questionnaire (BPAQ) [11] to determine a past BPAQ score (pBPAQ) reflective of historical physical activity participation from birth. The BPAQ enables the calculation of an index of bone-relevant weight-bearing exercise history by incorporating the loading characteristics of magnitude, rate and frequency for each reported activity. Given the known limitations of subject recall, the questionnaire was designed as a simple document using block recording and checkboxes. Responses were scored using computer software (freely available for download at www.fithdysign.com/BPAQ/) developed using Microsoft® Visual Basic (Microsoft®, USA). Intra-class correlation coefficients for inter- and intra-tester reliability for the BPAQ are very high (0.92 and 0.97, respectively) [13]. Scores from the BPAQ have been demonstrated to predict indices of bone mass in young adults better than generic measures of physical activity [11].
Bone parameters
Immediately following questionnaire completion, parameters of tibial bone strength were measured using peripheral quantitative computed tomography (pQCT) using an XCT-3000 (Stratec Medizintechnik, Pforzheim, Germany) applying an in-plane pixel size of 0.5 × 0.5 mm and slice thickness of 2.3 mm. The automated tibial mask procedure was used to scan the skeletally non-dominant tibia (determined by preferred kicking leg) for each participant to calculate the total volumetric density (mg/cm3), total area (mm2), strength–strain index (SSI, mm3), and compressive bone strength index (BSI, g2/cm4) at 4%, 38% and 66% of the tibial length from the distal end. A sub-sample of participants additionally underwent scans of their non-dominant radius to determine those same parameters at the 4% and 66% radial sites. Quality control was accomplished by performing the automated daily calibration with a phantom of known density. Short-term measurement precision (CV) for repeated measures in our laboratory is 1.5% and 0.6% for total density at the 4% and 38% tibial sites, respectively.
Statistical analyses
Statistical analyses were performed using SPSS Version 26.0 for Windows (IBM Corporation, Somers, NY, USA). Pearson correlation analyses with adjustment for bone size were performed to determine relationships between past BPAQ scores and parameters of tibial bone strength. The influence of bone size on pQCT measures was addressed by adjusting for tibial length for lower limb measures and ulnar length for upper limb measures. Sex-specific analyses were conducted to identify the relationships between past BPAQ scores and bone strength measures for male and female participants. Relationships were also examined based on child (< 18 years) and adult (> 18 years) groupings. Statistical significance was determined at p ≤ 0.05.
Results
Subject characteristics
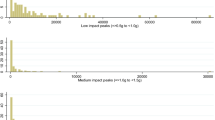
Five-hundred and thirty-two apparently healthy children and adults from the local community (277 males, 255 females) were included in the study. The sample represented a broad age range of 4–97 years (median 16.7 years, IQR 10.8–29.0 years) (Fig. 1). Height ranged from 1.05 to 1.98 m (median 1.61 m, IQR 1.44–1.72 m), weight ranged from 16.4 to 118.1 kg (median 53.5 kg, IQR 34.8–68.9 kg), while past BPAQ scores ranged from 0 to 310 (mean 57.7 ± 53.6).
BPAQ associations with pQCT-derived tibial bone measures
At the tibia (Table 1), pBPAQ scores were positively associated with total density at 38% and 66% sites (r = 0.234–0.261, p ˂ 0.05), total area at the 38% site (r = 0.148, p ˂ 0.05), and strength indices at all sites (r = 0.123–0.211, p ˂ 0.05) (Fig. 2). For males, pBPAQ scores were associated with all tibial pQCT measures examined (r = 0.226–0.430, p ˂ 0.05). For females, total density (r = 0.190, p = 0.032) and BSI (r = 0.179, p = 0.045) at the 38% tibial site were associated with pBPAQ scores.
BPAQ associations with pQCT-derived radial bone measures
At the radius (Table 2), pBPAQ scores were positively associated with total density at the 66% site (r = 0.145, p = 0.020), total area at both 4% and 66% sites (r = 0.129–0.156, p ˂ 0.05), and both strength indices at both 4% and 66% sites (r = 0.157–0.234, p ˂ 0.05) (Fig. 3). Past BPAQ scores were associated with all radial pQCT measures examined for males (r = 0.195–0.484, p ˂ 0.05), while only total area at the 4% radial site was associated with pBPAQ scores for females (r = 0.191, p = 0.031).
BPAQ associations with pQCT measures in children and adults
When the sample was parsed into child (< 18 years) and adult (> 18 years) groupings, only a few weak relationships could be observed between past BPAQ scores and pQCT-derived bone measures. For children, pBPAQ scores were positively associated with total density (r = 0.145, p = 0.033) and BSI (r = 0.138, p = 0.017) at the 38% tibial site (n = 306) and BSI (r = 0.131, p = 0.049) at the 66% radial site (n = 300). For adults, pBPAQ scores were associated with SSI (r = 0.151, p = 0.025) and BSI (r = 0.162, p = 0.015) at the 4% tibial site and total density (r = 0.420, p = 0.007) and BSI (r = 0.166, p = 0.013) at the 66% tibial site (n = 226); however, no relationships were observed at either radial site (n = 53).
Discussion
The current investigation sought to identify relationships between past BPAQ scores and pQCT-derived bone strength parameters for the tibia and radius and to observe age- and sex-specific associations. We found that past BPAQ scores held weak positive associations with pQCT-derived bone strength parameters at most tibial and radial sites. Significant associations were uniformly identified across all sites and parameters for males, while fewer significant associations were identified for females. With the group sub-classified into adults and children, a modest number of pQCT bone strength parameters (primarily tibial) showed relationships with past BPAQ scores.
The relatively weak relationships between physical activity participation and bone strength measures identified in this study must be interpreted in the context of other determinants of bone health. For example, genetic factors provide the strongest determinants of bone mass, accounting for up to 88% of variance [14]. A number of other influential factors contribute to bone health including nutrition (e.g. calcium and vitamin D), smoking, alcohol intake, and medication use. Thus, despite its known impact on bone health, physical activity participation can only be expected to account for a small amount of variance in bone strength measures. Nonetheless, data derived from the BPAQ instrument has allowed us to observe this subtle but significant relationship between physical activity and indices of bone strength in this and previous work, where generic measures of physical activity have failed.
In considering any relationship between physical activity participation and a change in bone strength, sufficient time for skeletal adaption is critical. For instance, during a remodelling cycle, the resorption period takes approximately 30–40 days and the subsequent formation period takes approximately 150 days [15]. Specifically, the lag in the time it takes newly laid osteoid to mineralise (primary mineral apposition) and the further prolonged secondary mineralisation [16], means that the time from bone stimulus (or exercise) to new bone detection with X-ray-based imaging is many months. Therefore, physical activity assessment methods, including modern accelerometers that capture characteristics of mechanical load, that rely on previous week, previous month, or even previous year ‘snapshots’ of activity fail to truly account for these delayed skeletal responses or the enduring effects of more historical physical activity participation [17]. Farr and colleagues [18] have investigated the relationships between BPAQ and pQCT-derived measures of bone and found no relationships, but examined only the current component (i.e. previous 12 months) of the measure and thus, important historical exposure to physical activity was overlooked. More recently, Kim and colleagues reported weak to moderate positive relationships between total BPAQ scores and pQCT measures of bone strength and geometry in young and middle-aged premenopausal women [19]. Therefore, to date, the ability of the BPAQ, and specifically its past component, to predict important indices of bone strength has not been examined.
The significant associations observed between past BPAQ scores, and pQCT-derived bone parameters were not confined to a particular regional site. Instead, the relationships were quite widespread and identified at most sites covering distal and mid shaft regions of both tibia and radius. In fact, the regional ubiquity of the observed associations suggests it exists both at sites that are predominantly cortical (e.g. 66% tibia and 66% radius) as well as sites that are predominantly trabecular in composition (e.g. 4% tibia and 4% radius). Our finding is consistent with those recently reported by Kim and colleagues [19] who found weak to moderate positive relationships between total BPAQ scores and pQCT-derived bone parameters at the 4%, 38%, and 66% tibial sites in their young adult female group. Interestingly, significant associations were limited to the 38% tibial site for their middle-aged premenopausal female group. Likewise, our findings are comparable to those of a recent high resolution pQCT study of young adult men and women, where BPAQ scores held positive relationships with most tibial bone parameters tested [20]. An earlier study of the relationships of bone loading scores to MRI-derived tibial and radial bone measures in adolescent females, found that BPAQ relationships extend to bone architecture, with moderate positive relationships reported for mid-tibial measures [21]. No BPAQ relationships, however, were observed at the radius in that study.
While our study revealed BPAQ relationships with pQCT-derived tibial bone strength measures for both males and females, those relationships were most numerous and notable for males. In fact, BPAQ was positively related to all reported bone measures for males, but only two tibial measures and one radial measure for females. Our apparently weaker findings for women might be a result of the very wide age range of our sample as other BPAQ studies of women with narrower age ranges have observed stronger and more numerous relationships [19, 21, 22]. Anecdotally, we have found that relationships between physical activity participation and pQCT outcomes can be influenced quite strongly by historical participation in activities at the highest end of the loading spectrum, such as gymnastics and ballet. Those activities tend to be most commonly undertaken by female participants, particularly during youth, and in the case where those participants have done very little osteogenic physical activity since childhood, a low or average bone strength measure can be strikingly disproportionate to a very large BPAQ score with the effect of weakening the observed group relationships—a phenomenon that can be visualised in Figs. 1 and 2 that show a small number of participants with only modest bone strength clustered at exceptionally high past BPAQ scores.
Although weak, we observed positive relationships between BPAQ scores and pQCT-derived bone measures in both children and adults. This result supports our previous findings of relationships of the BPAQ with other measures of bone health in children [8, 22] and adults [8, 11, 23]. Indeed, our adolescent data showed positive BPAQ relationships (r = 0.17–0.353) of a similar strength to our current findings for DXA- and quantitative ultrasonometry-derived measures of bone mass and quality [22]. However, others have reported no relationship of the BPAQ to bone measures in children. The study by Farr and colleagues [18] tested the current component of the BPAQ alongside other physical activity measures including pedometer steps, the 3-day physical activity recall (3DPAR) and the past year physical activity questionnaire (PYPAQ) for their examination of relationships with pQCT bone strength measures in 8- to 13-year-old girls. No associations were found for the BPAQ, while weak but significant positive associations were found for the other measures. Given that sustained loading activity over a prolonged period is necessary for a bone response and the lengthy time required for remodelling and mineralisation, it is perhaps not surprising that the ‘snapshot’ of physical activity considered by the most recent component of BPAQ (and indeed pedometers and 3-DPAR) did not relate strongly to bone outcomes. By contrast, our findings indicate that the past component of the BPAQ is capable of capturing exercise participation that is important to bone density, strength, and geometry and is applicable to both children and adults across all ages. It is likely that the influence of recent exercise during the relatively narrow pre- and peri-pubertal age range examined in the Farr study was confounded by the highly variable level of circulating bone-relevant hormones to which the pubescent skeleton is exposed, thereby masking an exercise relationship. Our much broader age range diluted the hormone influence.
Several study limitations warrant acknowledgement. Firstly, we recognise that pQCT measures include only peripheral skeletal sites and may not adequately represent bone strength at clinically relevant sites such as the femoral neck or vertebral bodies. Nonetheless, pQCT measures have advantages over DXA methods, such as providing a volumetric assessment of bone density as well as accounting for geometric aspects of bone strength. Furthermore, the distal radius is highly clinically relevant as it represents the most common osteoporotic fracture site [24] and is often a precursor to more consequential fractures later in life. Secondly, we acknowledge that subject recall over historical periods, particularly back to birth, is challenging for most and might impact the fidelity of our instrument. Nevertheless, the BPAQ has a simple design to facilitate block completion with an intuitive tick and flick approach and does not require fine details of physical activity participation for the past component (e.g. duration, frequency of participation, etc.). Moreover, the extensive historical account of skeletal loading exposure is an important strength of the BPAQ and sets it apart from most physical activity measurement tools that account only for a ‘snapshot’ (e.g. 7-day accelerometry) of exposure. Finally, our sample size for secondary analyses was somewhat disproportionate for adult and child groupings and particularly skewed to adults for measures at the radius. Such numbers may have precluded the detection of relationships in those groups; however, our sample size for whole group measures was robust and covered a very broad age demographic.
In conclusion, our findings of significant positive relationships between BPAQ scores and pQCT measures of bone strength mirror previous findings from other measurement modalities of bone mass and quality. Whilst many factors are important in the determination of bone strength, primarily genetic, the current findings strengthen the rationale for the use of the BPAQ to account for historical physical activity participation of relevance to bone geometry. Such exercise-induced geometric changes in bone can occur independently of changes in DXA-derived bone mass and are therefore a vital response of bone to exercise loading [25]. Our data also highlights that BPAQ scores are related, albeit weakly, to upper limb bone strength measures, despite not being a habitually weight-bearing region.
References
Rubin CT (1984) Skeletal strain and the functional significance of bone architecture. Calcif Tissue Int 36:S11-18
Turner CH, Owan I, Takano Y (1995) Mechanotransduction in bone: Role of strain rate. Am J Physiol 269:E438-442
Weeks BK, Beck BR (2008) Eight months of regular in-school jumping improves indices of bone strength in adolescent boys and girls: Results of the POWER PE study. J Bone Miner Res 23:1002–1011
Weeks BK, Beck BR (2012) Are bone and muscle changes from POWER PE, an 8-month in-school jumping intervention, maintained at three years? PLoS ONE 7:e39133
Robling AG, Hinant FM, Burr DB, Turner CH (2002) Shorter, more frequent mechanical loading sessions enhance bone mass. Med Sci Sports Exerc 34:196–202
Turner CH, Robling AG (2003) Designing exercise regimens to increase bone strength. Exerc Sport Sci Rev 31:45–50
Hamilton CJ, Swan VJ, Jamal SA (2010) The effects of exercise and physical activity participation on bone mass and geometry in postmenopausal women: a systematic review of pQCT studies. Osteoporos Int 21:11–23. https://doi.org/10.1007/s00198-009-0967-1
Rantalainen T, Weeks BK, Nogueira RC, Beck BR (2015) Effects of bone-specific physical activity, gender and maturity on tibial cross-sectional bone material distribution: a cross-sectional pQCT comparison of children and young adults aged 5–29years. Bone 72:101–108. https://doi.org/10.1016/j.bone.2014.11.015
Hart, N. H., Nimphius, S., Rantalainen, T., Ireland, A., Siafarikas, A., & Newton, R. U. (2017). Mechanical basis of bone strength: influence of bone material, bone structure and muscle action. J Musculoskelet Neuronal Interact, 17(3), 114–139. https://www.ncbi.nlm.nih.gov/pubmed/28860414
Currey JD (2001) Bone strength: what are we trying to measure? Calcif Tissue Int 68:205–210. https://doi.org/10.1007/s002230020040
Weeks, B. K., & Beck, B. R. (2008). The BPAQ: a bone-specific physical activity assessment instrument. Osteoporos Int, 19(11), 1567–1577. http://www.ncbi.nlm.nih.gov/pubmed/18414964
Weeks BK, Purvis M, Beck BR (2016) Physical activity estimated by the bone-specific physical activity questionnaire is also associated with cardiovascular risk. Eur J Sport Sci 16:1204–1211. https://doi.org/10.1080/17461391.2016.1153726
Weeks, B. K., Hirsch, R. D., Moran, D. S., & Beck, B. R. (2011). A useful tool for analysing the effects of bone-specific physical activity. Salud (i) Ciencia, 18(6), 538–542.
Brown LB, Streeten EA, Shapiro JR, McBride D, Shuldiner AR, Peyser PA, Mitchell BD (2005) Genetic and environmental influences on bone mineral density in pre- and post-menopausal women. Osteoporos Int 16:1849–1856. https://doi.org/10.1007/s00198-005-1948-7
Eriksen EF (2010) Cellular mechanisms of bone remodeling. Rev Endocr Metab Disord 11:219–227. https://doi.org/10.1007/s11154-010-9153-1
Boivin, G., & Meunier, P. J. (2003). Methodological considerations in measurement of bone mineral content. Osteoporos Int, 14 Suppl 5, S22–27; discussion S27–28. https://doi.org/10.1007/s00198-003-1469-1
Ahola R, Korpelainen R, Vainionpaa A, Leppaluoto J, Jamsa T (2009) Time-course of exercise and its association with 12-month bone changes. BMC Musculoskelet Disord 10:138. https://doi.org/10.1186/1471-2474-10-138
Farr JN, Lee VR, Blew RM, Lohman TG, Going SB (2011) Quantifying bone-relevant activity and its relation to bone strength in girls. Med Sci Sports Exerc 43:476–483. https://doi.org/10.1249/MSS.0b013e3181eeb2f2
Kim S, Baker BS, Sharma-Ghimire P, Bemben DA, Bemben MG (2018) Association between bone-specific physical activity scores and pQCT-derived measures of bone strength and geometry in healthy young and middle-aged premenopausal women. Arch Osteoporos 13:83. https://doi.org/10.1007/s11657-018-0495-8
Popp KL, Turkington V, Hughes JM, Xu C, Unnikrishnan G, Reifman J, Bouxsein ML (2019) Skeletal loading score is associated with bone microarchitecture in young adults. Bone 127:360–366. https://doi.org/10.1016/j.bone.2019.06.001
Kindler JM, Ross HL, Laing EM, Modlesky CM, Pollock NK, Baile CA, Lewis RD (2015) Load-specific physical activity scores are related to tibia bone architecture. Int J Sport Nutr Exerc Metab 25:136–144. https://doi.org/10.1123/ijsnem.2013-0258
Weeks, B. K., & Beck, B. R. (2010). The Relationship between Physical Activity and Bone during Adolescence Differs according to Sex and Biological Maturity. J Osteoporos, 2010, ID546593. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=20981148
Bolam KA, Beck BR, Adlard KN, Skinner TL, Cormie P, Galvao DA, Spry N, Newton RU, Taaffe DR (2014) The relationship between BPAQ-derived physical activity and bone density of middle-aged and older men. Osteoporos Int 25:2663–2668. https://doi.org/10.1007/s00198-014-2797-z
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17:1726–1733. https://doi.org/10.1007/s00198-006-0172-4
Fonseca H, Moreira-Goncalves D, Coriolano HJ, Duarte JA (2014) Bone quality: the determinants of bone strength and fragility. Sports Med 44:37–53. https://doi.org/10.1007/s40279-013-0100-7
Bolam KA, Beck BR, Adlard KN, Skinner TL, Cormie P et al (2014) The relationship between BPAQ-derived physical activity and bone density of middle-aged and older men. Osteoporos Int 25:2663–2668
Acknowledgements
Nil.
Author information
Authors and Affiliations
Contributions
BKW and BRB designed the study. All authors were involved in aspects of material preparation, data collection, and analysis. The first draft of the manuscript was written by BKW and all authors contributed to reviewing and editing subsequent drafts. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors report that there are no competing interests to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Weeks, B.K., Harding, A.T., Watson, S.L. et al. Bone-specific physical activity questionnaire-derived skeletal loading score predicts bone geometry, density, and strength indices: a cross-sectional study. J Bone Miner Metab 41, 492–500 (2023). https://doi.org/10.1007/s00774-023-01419-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-023-01419-w