Abstract
Introduction
In people living with HIV (PLWH), bone mineral density (BMD) discordance between the lumbar spine (LS) and femoral neck (FN) could be frequent given the high frequency of secondary osteoporosis, including HIV-related factors for bone disease.
Materials and methods
Retrospective cohort of PLWH with a dual X-ray absorptiometry scan. Hip–spine BMD discordance was defined as different T-score or Z-scores categories at LS and FN.
Results
Overall, 865 individuals (mean 49.5 years, female 27%) were included. Osteoporosis diagnosis was four-to-seven times lower when both skeletal sites were affected than when considering the lowest T-score at any site (overall, 21% vs 4%). Hip–spine BMD discordance was observed in 381 (44%) individuals, it increased with age (from 43 to 52%, P = 0.032), and it was mainly due to lower LS-BMD. A lower FN-BMD was associated with older age, lower BMI (P < 0.01), and HIV-related factors, such as low CD4 + T-cell counts, duration of HIV infection, and time on antiretroviral therapy (ART). In a multivariate regression analysis, sex male (Odds Ratio, OR 4.901), hyperparathyroidism (OR, 2.364), and time on ART (OR 1.005 per month) were independently associated with discordance. A higher estimated fracture risk by FRAX equation was observed in individuals with BMD discordance due to lower FN-BMD compared to those with lower LS-BMD (+ 36% for major osteoporotic fracture, P = 0.04; + 135% for hip fracture, P < 0.01).
Conclusion
Hip–spine BMD discordance is highly prevalent in PLWH and it is associated with classical and HIV-related risk factors, modifying the rate of osteoporosis and fracture risk estimation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a systemic disease characterized by low bone mineral density (BMD) and microarchitectural defects that increases the risk of fracture [1]. According to the World Health Organization, it is defined as a T-score ≤ − 2.5 (Z-score ≤ − 2 in individuals younger than 50 years) at the femoral neck and other skeletal sites (lumbar spine, total hip). Although BMD at different skeletal sites is correlated, the absolute BMD may differ between the lumbar spine and hip leading to different bone loss categories in the same individual, also known as hip–spine discordance [2, 3].
Several studies have shown that BMD discordance can affect the diagnosis of osteoporosis and cause decision-making problems in the general population [2, 4]. Among its causes, weight-bearing can lead to higher bone density in the hip and femur [5], age can affect trabecular and cortical bone differently, and importantly, BMD discordance could be secondary to disease or medication use [6]. To date, most etiologies of secondary osteoporosis first affect the spine, leading to a higher prevalence of lumbar osteoporosis [7].
Bone disease has become a major health problem in people living with HIV (PLWH), with a two-to-three times higher prevalence of osteoporosis than in uninfected individuals [8]. Nevertheless, no studies have assessed BMD discordance among PLWH, a relatively young population with a high prevalence of factors associated with secondary osteoporosis [9]. Thus, we evaluated the prevalence and characteristics of lumbar spine–femoral neck BMD discordance in PLWH and the impact of secondary osteoporosis factors, including HIV-related factors.
Materials and methods
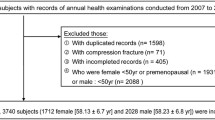
We collected dual X-ray absorptiometry (DXA) data from consecutive PLWH older than 30 years attending our HIV clinic at a tertiary university hospital from 2012 to 2020. In our unit, since 2012, DXA scan is performed as per clinical practice in all patients to assess bone status before and during antiretroviral therapy. PLWH with previous or current osteoporosis treatment or androgen therapy were excluded. Chronic supplementation with vitamin D was not considered exclusion criteria. Only the first DXA record of individuals with multiple records was used. The study was approved by our Institutional Review Board (EC 09/17), with a waiver for written informed consent because of the use of anonymized data.
At the time of DXA scan, age, sex, height, weight, and HIV-related variables such as risk practices for HIV acquisition, lymphocyte CD4 + T-cell count, time of HIV infection diagnosis, time on combined antiretroviral therapy (ART), and exposure to specific antiretroviral drugs such as tenofovir disoproxil fumarate (TDF) were collected. Additionally, in a subgroup of participants older than 40 years, data were collected on the presence of other clinical risk factors included in the FRAX equation, such as alcohol intake, smoking, parental history of hip fracture, personal history of fracture, glucocorticoids use, or diagnosis of rheumatoid arthritis, when available in their medical records.
Routine analytical test results were collected from the medical history to identify the presence of vitamin D deficiency (serum determination of 25-dihydroxyvitamin D by chemiluminescent microparticle immunoassay—CMIA—Architect 25 OH-vitamin D, Abbott Diagnostics, Germany), hyperparathyroidism (serum parathyroid hormone levels by electrochemiluminescence immunoassay—ECLIA, Cobas e411, Roche Diagnostics, Mannheim, Germany), chronic hepatitis C virus (HCV) coinfection, and chronic kidney disease (CKD).
At the time of DXA scan, we calculated body mass index (BMI) as weight in kilograms divided by the square of height in meters. Smoking was defined as current, active consumption. Alcohol intake was considered if there was a daily consumption of more than 30 gr. Glucocorticoid use was defined as exposure of more than 3 months at a dose of prednisolone ≥ 5 mg daily or equivalent before DXA scan. Hyperthyroidism was defined as TSH < 0.5 mU/L, independently of symptoms. Hypogonadism in men was defined as total testosterone level < 300 ng/dL. Vitamin D deficiency was defined as 25-dihydroxy vitamin D level of < 20 ng/mL. Secondary hyperparathyroidism was considered as parathyroid hormone levels > 65 pg/mL in the absence of serum calcium > 11 mg/dL. HCV coinfection was defined as positive HCV serum antibodies plus HCV-RNA positivity, or history of untreated infection. Estimated glomerular filtration rate (eGFR) was calculated by the CKD–epidemiology collaboration formula and CKD was defined as an eGFR < 60 ml/min/1.73 m2 in two determinations before the visit (stage ≥ 3) according to the National Kidney Foundation guidelines [7].
BMD at the lumbar spine (L1-L4) and the non-dominant femoral neck was assessed by DXA using a Hologic densitometer (Bedford, CA, USA). BMDs were measured in g/cm2 and converted into T-scores and Z-scores. According to the WHO criteria, osteoporosis was defined as a T-score ≤ − 2.5 standard deviations (SD) at the femoral neck and/or lumbar spine, osteopenia as a T-score between − 2.5 and − 1.0 SD, and normal bone mass as a T-score > − 1.0 SD. For individuals younger than 50 years or premenopausal women, we repeated the analysis by considering osteoporosis as a Z-score ≤ − 2 SD [3]. T-score or Z-score concordance indicated the agreement in the categories of T-score or Z-score at the lumbar spine (LS) and femoral neck (FN). T-score or Z-score discordance was defined as different T-score categories at LS and FN. Additionally, for T-score results, major discordance was defined as osteoporosis at one site, versus normal bone mass at the other site, whereas minor discordance referred to osteoporosis versus osteopenia, or osteopenia versus normal bone mass at different sites. To further characterize the differences between BMD at FN and LS, the discordant group was subdivided into lower LS-BMD (LS < FN) and lower FN-BMD (FN < LS).
In the subgroup with available data on clinical risk factors, the 10-year probability of major osteoporotic (wrist, humerus, spine, and hip) and hip fracture was estimated using FRAX equation calibrated for Spain, based on predisposing factors present at the time of DXA scan with the inclusion of FN-BMD data. We considered HIV infection as a cause of secondary osteoporosis; thus, this variable was filled for FRAX calculation in all participants.
Mean, median values and ranges, interquartile ranges (IQR), standard deviations (SD), or frequencies (%) for variables were calculated as appropriate. Comparisons were performed by Student’s t test or Mann–Whitney U test for continuous variables and Chi-squared test for categorical variables. Potential risk factors for discordance were entered into multivariate logistic regression analysis and the resulted odds ratios with 95% confidence intervals were reported. Significant variables in the univariate analysis, or those with close association (p < 0.1), were included in the model, considering T-score discordance as the dependent variable. The model was repeated using LS-BMD and FN-BMD discordance as dependent variables. Age, sex, and BMI were considered to be required covariates in all the models. Statistical significance was defined at a two-sided P value < 0.05. Analyses were performed with IBM SPSS Statistics version 18 (Chicago, IL, USA).
Results
The study population consisted of 865 individuals with complete data on the lumbar spine and femoral neck BMD. The mean age of the population was 49.5 years (range 20–83), 237 (27%) were female, and the mean BMI was 24 (range 14.7–37.7) Kg/m2. The characteristics of the population are displayed in Table 1.
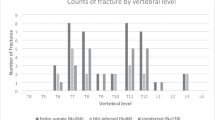
The prevalence of osteoporosis was 21% (183/865) using the lowest T-score at any site, 17% (149/865) in individuals with T-score discordance, and 4% (34/865) considering only concordant results. Of all individuals with osteoporosis at LS, 78% (122/156) had no diagnosis of osteoporosis at FN. Conversely, of 27 cases of osteoporosis at FN, the LS was not affected in 44%. The prevalence of osteoporosis considering the lowest T-score at any site increased with age: 15% (35/238) in individuals aged 30 to 40, 18% (70/400) in individuals aged 41 to 50, 34% (59/173) in individuals aged 51–60 years, and 35% (19/54) in individuals aged > 60 (Fig. 1). In the analysis by age strata, the diagnosis of osteoporosis was two-to-five times lower if considering the T-score at FN, and four-to-seven times lower when considering the presence of osteoporosis at both skeletal sites.
Overall, the prevalence of T-score discordance was 44% (381/865), corresponding to major discordance in 2% and minor discordance in 42%. According to sex, T-score discordance was more frequent among males (47 versus 37%, P = 0.02). Although mean age was similar in both sex categories (49.3 versus 50.0 years; P = 0.35), males had significantly higher mean BMI than females (24.3 ± 3.4 versus 23.1 ± 3.9 kg/m2, P < 0.01). Moreover, T-score discordance increased with age, affecting 43% of individuals in their third decade, 46% in their fifth decade, and reaching 52% in those older than 60 years (P = 0.032 in individuals aged < 40 versus ≥ 60 years).
T-score discordance due to lower LS-BMD was observed in 31% (268/865) individuals, whereas lower FN-BMD was found in 13% (113/865). Of note, even though BMD discordance was mainly due to lower LS-BMD in all age strata, lower FN-BMD increased with age, ranging from 10% in individuals aged 30–40 years to 22% in those over the age of 60 (Fig. 2).
Not surprisingly, the clinical characteristics of individuals with T-score discordance differed depending on the affected site (Table 1). In brief, in univariate analysis, discordant individuals with lower FN-BMD were older (P < 0.01), more frequently female (P = 0.01), and had lower mean BMI (P < 0.01). Secondary factors such as chronic kidney disease (P = 0.08), hyperparathyroidism (P = 0.08), and HCV coinfection (P = 0.07) were also more prevalent in these individuals. Of clinical interest, individuals with lower FN-BMD had lower CD4 + T-cell counts at inclusion (P = 0.05) and significantly longer duration of HIV infection (P < 0.01) and antiretroviral therapy (P = 0.03) than individuals with lower LS-BMD.
Considering the large proportion of young individuals in our cohort, we repeated the analysis using a Z-score ≤ − 2 SD as a cut-off point for the entire population with similar results. Indeed, osteoporosis at the LS was 2.5-to-6 times more frequent than at the FN, and concordance of osteoporosis in both sites was observed in only 2% of the cohort (Supplementary Fig. 1). Due to the use of a higher cut-off value, the rate of discordance was lower (overall, 20%, ranging from 18 to 29%) and predominantly driven by lower LS-BMD (Supplementary Fig. 2).
In the multivariate analysis using T-score discordance as the dependent variable, sex male, hyperparathyroidism, and time on antiretroviral therapy were associated with discordance (Table 2). To analyze the role of the secondary and HIV-related factors in the different anatomic sites, the analysis was repeated using discordance with lower LS-BMD and FN-BMD as dependent variables. As shown, sex male was consistently an independent variable for BMD discordance, whereas time on antiretroviral therapy, hyperparathyroidism, and time of HIV infection had a different impact on lumbar spine or femoral neck discordance.
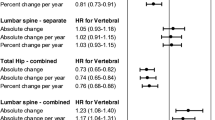
Finally, we analyzed the effect of discordance on the estimated risk of fracture. Complete data about clinical risk factors included in the FRAX equation and HIV-related variables that predispose to bone disease were available for 208 individuals. Mirroring the global data, PLWH with T-score discordance had distinctive characteristics according to the affected site: individuals with lower FN-BMD had a significantly higher prevalence of smoking (67 versus 36%, P = 0.01), HCV coinfection (54 versus 30%, P = 0.04), and longer duration of HIV infection (193.8 versus 127.7 months, P = 0.04), and antiretroviral therapy (169.9 versus 158.5 months, P = 0.01) than individuals with lower LS-BMD. Conversely, the prevalence of alcohol drinking, glucocorticoid use, hyperthyroidism, and hypogonadism were similar in both groups. Since BMD or T-score at the FN are the variables included in the model for fracture risk estimation, the 10-year estimated risk of fracture by FRAX was significantly higher among discordant PLWH with lower FN-BMD versus those with lower LS-BMD (2.44% versus 1.79%, P = 0.04, + 36% for major osteoporotic fracture, and 0.73% versus 0.31%, P < 0.01, + 135% for hip fracture) (Fig. 3).
Estimated risk of fracture by FRAX equation in a subgroup of 208 individuals with complete data on clinical risk factors: overall (black bars), discordant individuals with lower femoral neck-bone mineral density (FN-BMD, light grey bars), and discordant individuals with lower lumbar spine bone mineral density (LS-BMD, dark grey bars)
Discussion
To our knowledge, this is the first study evaluating the prevalence of hip–spine BMD discordance and the associated characteristics among PLWH. We found that 44% of HIV-infected individuals had discordance in the T-score categories at different sites, predominantly due to lower LS-BMD. Of clinical interest, we observed the key role of secondary causes of osteoporosis and HIV-related factors in producing FN osteoporosis and their contribution to discordance due to lower FN-BMD. Furthermore, the presence of discordance changed the overall prevalence of osteoporosis and the estimated risk of fracture by FRAX equation.
The differences in the frequency of osteoporosis between the hip and spine are not surprising. The rate of discordance in previous studies from the general population ranged between 10 and 46% according to the different definitions applied [3, 7], and in all studies, lower LS-BMD was more frequent. Although no direct reference to discordance was made, a meta-analysis including 29 studies in PLWH [8] described a prevalence of osteoporosis at LS consistently higher than at FN (7–28% versus 1–15%, respectively), suggesting the presence of BMD discordance. Moreover, we found that the rate of discordance was high and increased with age driven by a progressive increase in the rate of osteoporosis at the FN.
From a clinical point of view, the different rates of osteoporosis in the hip and spine could change the management of PLWH. We observed that the diagnosis of osteoporosis in our cohort was two-to-five times lower when considering the T-score at FN versus at LS, and four-to-seven times lower when both skeletal sites were affected. Indeed, only 4% of the individuals had osteoporosis at both sites, a lower rate than that reported in the general population (10–30%) [10, 11]. This fact confirms that risk factors for bone loss could impact BMD differently depending on the skeletal site and the population involved. As in the general population, BMI was lower among discordant PLWH with lower FN-BMD in our study [12]. It has been reported that BMD strongly correlates with load at weight-bearing bones, and thus, a reduced load at FN could predispose these individuals to a reduced FN-BMD [13]. Additionally, cortical bone resorption induced by hyperparathyroidism secondary to vitamin D deficiency or chronic kidney disease may determine a lower FN-BMD (a cortical-rich site) [14]. Likewise, we observed that HCV infection was more frequent, albeit not significantly, in individuals with lower FN-BMD. This finding is consistent with a previous study that found a higher prevalence of osteoporosis at FN (4–22%) versus LS (0–16%) in HCV mono-infected individuals, which was related to a high bone turnover [15]. Therefore, secondary causes of BMD loss can modify the rate of discordance [9].
In line with this, we found that HIV-related factors also affected BMD differently according to the skeletal site. In our population, discordant individuals with lower FN-BMD had lower CD4 T-cell counts at inclusion, and a longer duration of HIV infection and ART exposure. The role of HIV-related factors on bone loss pathogenesis is complex and poorly understood. An interplay between inflammatory cytokines, immune activation, and osteoclast differentiation has been described [16]. Moreover, ART initiation has been associated with bone loss, especially in individuals on TDF which characteristically affects FN-BMD [17].
To evaluate the role of secondary and HIV-related factors in discordance, we performed a multivariate analysis. Whereas age was no longer significantly associated with discordance in this young population, sex male, a secondary cause of osteoporosis such as hyperparathyroidism, and HIV-related factors such as time of HIV infection and time on antiretroviral therapy were independently associated with the emergence of discordance. These data confirm our hypothesis about the important role of these factors in this population.
The WHO defines the diagnosis of osteoporosis based on the lowest BMD measure [18]. Therefore, most current studies do not specify the skeletal site considered in their definition of osteoporosis. In the referred metanalysis in PLWH, only 3 out of 29 studies specified the site involved in the diagnosis of osteoporosis [8]. Nevertheless, our results suggest that BMD discordance in PLWH could point toward different factors causing bone loss, a piece of information that can be useful in the prevention or treatment of bone disease.
The impact of discordance on the risk of fracture estimation is controversial. Large cohort studies demonstrated that discordance could contribute to fracture risk, particularly when it is caused by lower LS-BMD [2]. Moreover, fracture discrimination significantly improved after combining FN and LS-BMD measures in women aged 50–64 years from a Canadian cohort [19]. Indeed, it has been suggested to adjust the estimated risk by FRAX in discordant individuals (i.e., modifying the risk by 10% per standard deviation of the difference between LS and FN T-scores) to improve fracture risk discrimination [20]. In our study, discordant individuals with lower FN-BMD had an estimated risk of major osteoporotic fracture 36% higher and an estimated risk of hip fracture 135% higher than those with lower LS-BMD, because only FN-BMD is included in the equation. These findings confirm the importance of considering T-score discordance for fracture risk estimation.
The current study has some limitations. First, we were not able to analyze the impact of discordance on the incidence of fractures, since we did not observe any non-pathological fractures during follow-up. Second, data on clinical risk factors considered by FRAX equation were available for a quarter of the population. Finally, we used T-score categories in individuals younger than 50 years to allow comparisons with the rest of the cohort and with other studies. In any case, we repeated the analysis using Z-scores with similar results.
In conclusion, T-score discordance was observed in 44% of PLWH, predominantly due to lower LS-BMD. However, lower FN-BMD was more relevant in older individuals and those with secondary causes of osteoporosis, including HIV-related factors. The presence of BMD discordance can affect the prevalence of osteoporosis and the estimated risk of fracture by FRAX equation ultimately affecting the management of bone disease. Therefore, studies of PLWH with osteoporosis should specify the diagnostic criteria (at both sites versus any site) and whether there is BMD discordance, since this can impact the decision-making process in terms of prevention and treatment.
References
Compston JE, McClung MR, Leslie WD (2019) Osteoporosis. Lancet 393:364–376. https://doi.org/10.1016/S0140-6736(18)32112-3
Johansson H, Kanis JA, Oden A, Leslie WD, Fujiwara S, Gluer CC, Kroger H, LaCroix AZ, Lau E, Melton LJ 3rd, Eisman JA, O’Neill TW, Goltzman D, Reid DM, McCloskey E (2014) Impact of femoral neck and lumbar spine BMD discordances on FRAX probabilities in women: a meta-analysis of international cohorts. Calcif Tissue Int 95:428–435. https://doi.org/10.1007/s00223-014-9911-2
Mounach A, Abayi DA, Ghazi M, Ghozlani I, Nouijai A, Achemlal L, Bezza A, El Maghraoui A (2009) Discordance between hip and spine bone mineral density measurement using DXA: prevalence and risk factors. Semin Arthritis Rheum 38:467–471. https://doi.org/10.1016/j.semarthrit.2008.04.001
Abrahamsen B, Stilgren LS, Hermann AP, Tofteng CL, Barenholdt O, Vestergaard P, Brot C, Nielsen SP (2001) Discordance between changes in bone mineral density measured at different skeletal sites in perimenopausal women–implications for assessment of bone loss and response to therapy: the danish osteoporosis prevention study. J Bone Miner Res 16:1212–1219. https://doi.org/10.1359/jbmr.2001.16.7.1212
Kohrt WM, Snead DB, Slatopolsky E, Birge SJ Jr (1995) Additive effects of weight-bearing exercise and estrogen on bone mineral density in older women. J Bone Miner Res 10:1303–1311. https://doi.org/10.1002/jbmr.5650100906
El Maghraoui A, Roux C (2008) DXA scanning in clinical practice. QJM 101:605–617. https://doi.org/10.1093/qjmed/hcn022
Hong AR, Kim JH, Lee JH, Kim SW, Shin CS (2019) Metabolic characteristics of subjects with spine-femur bone mineral density discordances: the Korean National Health and Nutrition Examination Survey (KNHANES 2008–2011). J Bone Miner Metab 37:835–843. https://doi.org/10.1007/s00774-018-0980-6
Goh SSL, Lai PSM, Tan ATB, Ponnampalavanar S (2018) Reduced bone mineral density in human immunodeficiency virus-infected individuals: a meta-analysis of its prevalence and risk factors: supplementary presentation. Osteoporos Int 29:1683. https://doi.org/10.1007/s00198-018-4379-y
Casado JL, Banon S, Andres R, Perez-Elias MJ, Moreno A, Moreno S (2014) Prevalence of causes of secondary osteoporosis and contribution to lower bone mineral density in HIV-infected patients. Osteoporos Int 25:1071–1079. https://doi.org/10.1007/s00198-013-2506-3
Woodson G (2000) Dual X-ray absorptiometry T-score concordance and discordance between the hip and spine measurement sites. J Clin Densitom 3:319–324. https://doi.org/10.1385/jcd:3:4:319
El Maghraoui A, Mouinga Abayi DA, Ghozlani I, Mounach A, Nouijai A, Ghazi M, Achemlal L, Bezza A (2007) Prevalence and risk factors of discordance in diagnosis of osteoporosis using spine and hip bone densitometry. Ann Rheum Dis 66:271–272. https://doi.org/10.1136/ard.2006.062372
Park KH, Lim JS, Kim KM, Rhee Y, Lim SK (2016) Z-score discordance and contributing factors in healthy premenopausal women with low bone mineral density: the Korean national health and nutrition examination survey 2008–9. J Bone Miner Metab 34:668–677. https://doi.org/10.1007/s00774-015-0715-x
Felson DT, Zhang Y, Hannan MT, Anderson JJ (1993) Effects of weight and body mass index on bone mineral density in men and women: the Framingham study. J Bone Miner Res 8:567–573. https://doi.org/10.1002/jbmr.5650080507
Lips P (2001) Vitamin D deficiency and secondary hyperparathyroidism in the elderly: consequences for bone loss and fractures and therapeutic implications. Endocr Rev 22:477–501. https://doi.org/10.1210/edrv.22.4.0437
Lin JC, Hsieh TY, Wu CC, Chen PJ, Chueh TH, Chang WK, Chu HC (2012) Association between chronic hepatitis C virus infection and bone mineral density. Calcif Tissue Int 91:423–429. https://doi.org/10.1007/s00223-012-9653-y
Weitzmann MN, Vikulina T, Roser-Page S, Yamaguchi M, Ofotokun I (2017) Homeostatic expansion of cd4+ T cells promotes cortical and trabecular bone loss, whereas cd8+ T cells induce trabecular bone loss only. J Infect Dis 216:1070–1079. https://doi.org/10.1093/infdis/jix444
McComsey GA, Kitch D, Daar ES, Tierney C, Jahed NC, Tebas P, Myers L, Melbourne K, Ha B, Sax PE (2011) Bone mineral density and fractures in antiretroviral-naive persons randomized to receive abacavir-lamivudine or tenofovir disoproxil fumarate-emtricitabine along with efavirenz or atazanavir-ritonavir: aids clinical trials group A5224s, a substudy of ACTG A5202. J Infect Dis 203:1791–1801. https://doi.org/10.1093/infdis/jir188
Kanis JA, Johnell O, Oden A, Johansson H, Eisman JA, Fujiwara S, Kroger H, Honkanen R, Melton LJ 3rd, O’Neill T, Reeve J, Silman A, Tenenhouse A (2006) The use of multiple sites for the diagnosis of osteoporosis. Osteoporos Int 17:527–534. https://doi.org/10.1007/s00198-005-0014-9
Leslie WD, Tsang JF, Caetano PA, Lix LM, Manitoba Bone Density P (2007) Number of osteoporotic sites and fracture risk assessment: a cohort study from the Manitoba Bone Density Program. J Bone Miner Res 22:476–483. https://doi.org/10.1359/jbmr.061112
Leslie WD, Lix LM, Johansson H, Oden A, McCloskey E, Kanis JA (2011) Spine-hip discordance and fracture risk assessment: a physician-friendly FRAX enhancement. Osteoporos Int 22:839–847. https://doi.org/10.1007/s00198-010-1461-5
Acknowledgements
We would like to thank Ana Abad for her important contribution to database management.
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
Conceptualization: PV and JLC; methodology: PV and JLC; formal analysis and investigation: PV, MR, JMR, AM, MJV, and JLC; writing–original draft: PV and JLC; writing–review, and editing: JMR; supervision: PV and JLC.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
This study was evaluated, exempted from written consent, and approved by the institutional review board of Ramon y Cajal University Hospital (EC 09/17).
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Vizcarra, P., Rosillo, M., del Rey, J.M. et al. Unravelling hip–spine bone mineral density discordance in people living with HIV. J Bone Miner Metab 40, 990–997 (2022). https://doi.org/10.1007/s00774-022-01365-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-022-01365-z