Abstract
Purpose
To evaluate the utility of vertebral Hounsfield unit (HU) values from computed tomography (CT) in cancer staging as a supplementary screening tool for bone health among prostate cancer (PCa) patients.
Methods
T-scores of bone mineral density (BMD) in each lumbar vertebra (L1–L4) and hip for newly diagnosed PCa patients (N = 139) were measured using dual-energy X-ray absorptiometry (DXA). The degenerative changes in each lumbar vertebra were assessed, and the HU values of trabecular bone in axial CT images of each vertebral body (vertebral CT-HU value) were measured using staging CT.
Results
556 vertebrae were analyzed. 326 of 556 (59%) lumbar vertebrae had degenerative changes. The vertebral CT-HU value was positively correlated with the lumbar BMD T-score, with higher correlation coefficients observed in vertebrae without degenerative changes (r = 0.655, N = 230) when compared to vertebrae with degenerative changes (r = 0.575, N = 326). The thresholds matching BMD T-scores of − 2.0 and − 1.5 set by cancer treatment-induced bone loss guidelines were 95 HU and 105 HU, respectively. Based on the intervention threshold (lumbar BMD T-score < − 1.5), 15.1% of PCa patients required osteoporosis treatment; and, this value increased to 30.9% when L1–L4 CT-HU thresholds that corresponded to BMD T-score < − 1.5 were used.
Conclusion
Lumbar BMD values from DXA may not reflect true bone health in PCa patients who often have lumbar degenerative diseases. Thresholds based on the vertebral CT-HU value can be used as a supplementary method to identify PCa patients who need anti-osteoporosis drugs.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Prostate cancer (PCa), whose incidence increases with age, is one of the most common cancers occurring in elderly men[1]. Androgen deprivation therapy (ADT) is one of the important treatments for PCa. However, ADT interferes with normal androgen-dependent physiological functioning in organs, resulting in various adverse events. One of the serious adverse events in ADT is bone loss (the so-called cancer treatment-induced bone loss [CTIBL]) and an increase in fragility fractures[2, 3]. ADT for 12 months reduces bone mineral density (BMD) by 2–5% and increases the risk of fracture by nearly two-fold[2, 3]. Similarly, a longer duration of ADT is associated with a greater decrease in the lumbar and hip BMD[4].
Recent advances in surgical techniques using robotic surgical systems have provided significant benefits to older adults who may not withstand conventional surgery. Therefore, the routine management of locally advanced PCa using radiation therapy combined with ADT can be replaced by robot-assisted radical prostatectomy, which does not require ADT[5]. This approach is suitable for newly diagnosed PCa patients with low bone mass. Therefore, we should consider both the adverse events caused by ADT and its anticancer properties when selecting treatment options for localized PCa.
BMD measurement by dual-energy X-ray absorptiometry (DXA) has been highly recommended in various published CTIBL treatment manuals for all patients starting ADT[6,7,8]. The resultant BMD T-score considerably affects a patient’s treatment algorithm[6,7,8]. However, BMD values obtained from lumbar DXA are reported to be often overestimated in elderly persons with concurrent lumbar degenerative diseases[9]. There are no studies that have investigated the proportion of PCa patients with spinal degenerative diseases, such as degenerative arthritis, osteophyte formation, and bone sclerosis.
Several studies have reported that the vertebral Hounsfield unit (HU) measured using computed tomography (CT) could be used as a complementary method to assess bone health. A positive correlation between vertebral HU value obtained from CT (vertebral CT-HU value) and BMD from DXA supports the use of the vertebral CT-HU value in evaluating bone health[10,11,12,13]. Because patients diagnosed with PCa routinely undergo staging CT, including spinal lesions, the vertebral CT-HU value can be obtained at no additional costs and without further exposure to radiation. To the best of our knowledge, previous research has not investigated whether the vertebral CT-HU value in PCa staging can be used as a supplementary method to identify bone health of PCa patients who need anti-osteoporosis drugs.
In this study, we examined the relationships between the lumbar BMD T-score from DXA and the PCa staging CT-assessed lumbar spine degenerative changes. Additionally, we evaluated the utility of vertebral CT-HU as a supplementary screening tool for bone health in patients with PCa.
Materials and Methods
Eligibility criteria and enrollment
This prospective study enrolled consecutive male patients newly diagnosed with PCa at our institute from November 2018 to May 2020. All patients had both abdominal CT and DXA measurement within a month of prostate biopsy. Furthermore, all patients routinely underwent pelvic MRI for the local staging of PCa and bone scintigraphy to identify PCa bone metastasis.
The study’s inclusion criteria were 1) men aged over 50 years 2) who had both abdominal CT and DXA done within a month of prostate biopsy. Patients with a history of spinal surgery, or a benign spinal tumor, or who had spinal metastasis were ineligible for inclusion.
This study was conducted in accordance with the Declaration of Helsinki and approved by the ethical review board of our institution (IRB number 202001069). The board waived the requirement for patients’ informed consent by posting the opt-out information on the hospital’s homepage.
BMD measurements
BMD (measured in g/cm2) was measured using DXA (Horizon W; Hologic, Inc., Marlborough, MA, USA), beginning with the areal BMD for the first (L1) to the fourth lumbar vertebra (L4), and left hips (femoral neck and total hip). BMD T-score was then calculated by the difference between a patient’s measured BMD and the mean BMD in healthy young Japanese men. We set our intervention thresholds based on CTIBL treatment manuals as follows: patients with BMD T-scores of < − 1.5 were eligible for interventions for bone loss induced by ADT[7, 14]. The position statement of the Japanese Society of Bone and Mineral Research (JSBMR) in their CTIBL treatment manual recommends anti-osteoporosis drug treatment for patients with BMD − 2.0 ≤ T-score < − 1.5 and either a family history of hip fracture, or ≥ 15% of 10-year probability of major osteoporotic fractures based on a fracture risk assessment tool; or in patients with BMD T-score < − 2.0[7].
CT analysis for lumbar degenerative changes
Using Revolution EVO (GE Healthcare Japan, Tokyo, Japan) CT scans, multi-planar reconstruction (MPR) CT images were created. The settings used for each scan included a slice thickness of 1.25 mm, a tube voltage of 120 kVp, and an automatic exposure tube current of 50–250 mA. A spine surgeon (K.T.) who was blinded to patients’ clinical outcomes measured the parameters obtained from MPR CT images (window width, 2000; window level, 300) on a flat monitor using in-built imaging software (Synapse; Fujifilm Medical Co, Ltd., Tokyo, Japan).
We assessed the presence of lumbar degenerative changes in each lumbar vertebra (L1–L4) using methods employed in a previous study[13]. A lumbar vertebra was defined as a vertebral bone with degenerative changes (Fig. 1): (A) it featured third-degree osteophytes in the shape of a bird’s beak or fourth-degree osteophytes appearing as a bone bridge according to the four-degree classification system of osteophytes; (B) it had adjacent fourth-degree disk degeneration according to the University of California at Los Angeles Grading Scale [[15]], (C) it had narrowed facet joint(s) with large osteophytes, or (D) there was obvious vertebral compression (≥ 25% loss of height).
Examples of vertebrae with degenerative changes (A, C, E) and vertebrae without degenerative changes (B, D, F). A osteophytes in the shape of bird’s beak and bony bridge around vertebral body (white arrows) and sclerotic change of bony endplate (white arrow head) in the coronal plane. C osteophytes in the shape of bird’s beak and bony bridge around vertebral body (white arrows), sclerotic change of vertebral endplate (white arrow head), and osteophytes in facet joints (black arrows) in the sagittal plane. E Osteophytes on the facet joints (black arrows) and the narrowing of facet joint space
Vertebral CT-HU measurements
Vertebral CT-HU measurements for each lumbar vertebra (L1–L4) were performed using the method described by Schreiber et al.[12]. We then reconstructed precise MPR CT axial images parallel to the coronal and sagittal plane of each vertebral body, and the largest possible oval regions of interest (ROI) in the trabecular bone area of the vertebral body were set up so as not to include the cortical shell (Fig. 2A). The average CT-HU value within this click-and-drag ROI was calculated automatically using an in-built imaging software. The average CT-HU value was measured on the axial images at L1 through L4 at three separate locations: 1) immediately inferior to the superior vertebral end plate, 2) in the middle of the vertebral body, and 3) immediately superior to the inferior vertebral end plate (Fig. 2B). The average CT-HU values from the three axial images obtained at these three separate locations described the mean CT-HU value for each lumbar vertebra (L1-4).
Vertebral CT-HU measurements using multi-planar reconstruction computed tomography images. A The reconstructed axial image in the third lumbar vertebral body. The largest possible oval region of interest in the trabecular bone area of vertebral body was set up and the average HU within the ROI was automatically measured. B Slice (1) was set immediately inferior to the superior vertebral end plate, slice (2) was set in the middle of vertebral body, and slice (3) was set immediately superior to the inferior vertebral end plate
Statistical analysis
Statistical analyses were performed using the JMP software (version 12.2.0; SAS Institute, Inc., Cary, NC, USA). The three groups were assessed using one-way analysis of variance followed by the Tukey–Kramer honestly test for multiple comparisons. P value of < 0.05 was considered statistically significant. Associations between continuous variables were expressed using the Pearson’s correlation coefficient test. To assess the utility of vertebral CT-HU, we plotted receiver operating characteristic (ROC) curves to compute the largest area under the curve (AUC).
Results
Participant selection and participant characteristics
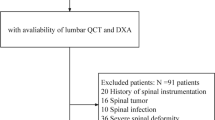
Altogether, 150 consecutive men diagnosed with PCa were enrolled in the study. Two men with metastasis in the lumbar spine and nine men with incomplete data were excluded, leaving 139 men who were included in the final analysis (Supplemental Fig. 1). The baseline characteristics are shown in Table 1. The mean age was 73.4 years (range 52–90). The mean serum testosterone level was 5.15 ng/mL (range 1.43–12.2). ADT as a future PCa treatment was prescribed for 78 patients (56%).
BMD and BMD T-score measurements
The mean values of BMD and BMD T-score in the lumbar spine (L1-L4) and left hips are shown in Supplemental Table 1. BMD T-scores gradually increased as the lumbar level progressed from L1 to L4.
Comparing patient groups by patient characteristics, BMD and vertebral CT-HU score
All 556 vertebrae (4 for each patient) belonging to the 139 patients were assessed for the presence of lumbar degenerative changes. There were 326 vertebrae (59%) with degenerative changes observed in L1 (51%), L2 (57%), L3 (58%), and L4 (68%). Based on the number of vertebral bones between L1 and L4 with degenerative changes, all patients were divided into three groups. Fifty-one patients (Group B, 37%) had one or two vertebrae with degenerative changes, 68 patients (Group C, 49%) had three or four lumbar vertebrae with degenerative changes, and only 20 patients (Group A, 14%) had no lumbar degenerative changes (Table 2).
Patients with a higher vertebral degenerative change were older (p = 0.013). When comparing individual groups, the L1–L4 BMD and BMD T-score values significantly differed by patient group (p < 0.001). No significant differences were observed among the three groups regarding hip BMD values and vertebral CT-HU values, which are less affected by degenerative changes (Table 2).
Validity of vertebral CT-HU
The vertebral CT-HU was positively correlated with lumbar BMD T-score with higher correlation coefficients in vertebrae without degenerative changes (r = 0.655, N = 230) than in vertebrae with degenerative changes (r = 0.575, N = 326) (Fig. 3A). The ROC curves and AUC results for predicting a BMD T-score of < − 1.5 and < − 2.0 in 230 vertebrae without degenerative changes are shown in Fig. 3B. The optimal cut-off vertebral CT-HU corresponding to < − 1.5 was 105 HU with 68.4% and 75.0% sensitivity and specificity, respectively (AUC = 0.782 [95%CI, 0.710 − 0.853]). The optimal cut-off vertebral CT-HU corresponding to < − 2.0 was 95 HU with 76.9% and 77.6% sensitivity and specificity, respectively (AUC = 0.808 [95% CI, 0.703 − 0.914]).
A The correlation between lumbar T-score from DXA and vertebral CT-HU value with scatter plots and regression lines for both vertebral without degenerative changes (DC) and vertebral with DC. B Receiver operating characteristic (ROC) curves in 230 vertebrae without degenerative changes for both DXA-derived BMD T-score = − 1.5 (A) and DXA-derived BMD T-score = − 2.0 (B). The area under the curve (AUC) was calculated for each ROC curve
Proportion of patients in need of anti-osteoporosis treatment
We compared the percentages of PCa patients in need of anti-osteoporosis treatment based on the JSBMR treatment algorithm and several types of bone health thresholds (Table 3). Using the lumbar BMD T-score < − 1.5, the percentage of patients with PCa who needed osteoporosis treatment was 15.1%, and this percentage increased to 30.9% based on the L1 − L4 CT-HU threshold, which corresponded to a BMD T-score < − 1.5. The percentages of patients with no need of osteoporosis treatment as evaluated by the L1 − L4 CT-HU threshold (69.1%) did not differ from that evaluated by DXA-derived BMD T-score obtained from both lumbar spine and hips (68.3%). Based on a lumbar BMD T-score < − 2.0, the percentage of PCa patients who were highly in need of osteoporosis treatment was 10.1% and this percentage was 25.9% using the L1 − L4 CT-HU threshold, which corresponded to a BMD T-score of − 2.0.
Using the lowest T-score from both lumbar and hip BMD T-score < − 1.5, the percentage of patients with PCa who needed osteoporosis treatment was 31.7%, and this percentage increased to 44.6% based on the L1 − L4 CT-HU threshold combined with BMD T-score obtained from both lumbar spine and hips, which corresponded to a BMD T-score < − 1.5. Twenty-two patients (15.8%) showed the discordance between hip BMD value and L1 − L4 CT-HU threshold. In these patients, the hip BMD value was normal (T-score > − 1.5), but the L1 − L4 CT-HU threshold showed lower bone mass (T-score < − 1.5).
Discussion
This is the first prospective study to evaluate the accuracy of lumbar BMD values measured by DXA and the utility of vertebral CT-HU value based on PCa staging CT. This study showed that lumbar degenerative disease frequently occurs in patients with PCa, which has an impact on lumbar BMD values. Bone health screening using the vertebral CT-HU value is a supplementary tool to identify PCa patients in need of CTIBL prevention.
BMD measurement using DXA is the gold standard for diagnosis of osteoporosis and is recommended for all patients starting ADT[6,7,8, 16,17,18]. However, lumbar BMD measurements from DXA have some limitations especially in patients with lumbar degenerative disease[9, 19, 20]. Muraki et al. reported that lumbar degenerative disease increases lumbar spine DXA-derived BMD by 15% [19]. Tenne et al. argued that degenerative changes that are very common among elderly persons frequently increase from vertebrae L1 to L4 resulting in the under-diagnosis of osteoporosis [20]. In this study, 119 of 139 (86%) patients and 326 of 556 (59%) lumbar vertebrae in PCa patients (the mean age: 73.4 years) had obvious degenerative changes. There was a significant relationship between the number of vertebrae with degenerative changes and L1-4 BMD T-scores from DXA. Similar to previous reports, this study also revealed that lumbar degenerative disease is a common comorbidity in elderly PCa patients, and lumbar DXA-derived BMD may be overestimated.
The International Society for Clinical Densitometry recommends that BMD should be measured in both lumbar vertebrae and hips, and the lowest T-score is used to diagnose osteoporosis [21]. Although hip BMD is used as an alternative to lumbar BMD, hip BMD measurement is wrought with challenges, such as a lower reproducibility of measurement and discordance between hip and lumbar BMD measurements [22,23,24]. In this study, 22 patients (15.8%) showed the discordance between hip BMD value and L1 − L4 CT-HU threshold. Diagnosing osteoporosis on the basis of hip BMD is likely to fail to identify PCa patients in need of CTIBL prevention. Re-analysis of lumbar BMD values by exclusion of the vertebra with fractures or degenerative changes and understanding the discordance between hip and lumbar BMD may be challenging for urologists who are not conversant with diagnosing osteoporosis. Therefore, developing a simple method to evaluate bone health is required.
In this study, vertebral CT-HU measurements which show bone density of trabecular bone within the cortical shell were performed using a simple method described by Schreiber et al.[12]. They reported the excellent reliability for the reproducibility of measurements that intra-observer and inter-observer intra-class correlation coefficients were 0.964 and 0.975, respectively. Choi et al. performed a retrospective study using DXA and CT, and categorized 110 patients into the degenerative group and the non-degenerative group similar to how we did it[25]. They reported a higher correlation between mean L1–L4 CT-HU value and BMD T-score in the non-degenerative group (r = 0.734) when compared to the degenerative group. Zou et al. also reported a positive and higher correlation (r > 0.7) between vertebral CT-HU values and BMD T-score in the non-degenerative group when compared to the degenerative group [13]. In this study, the correlation coefficient of lumbar BMD T-score and vertebral CT-HU was 0.655 in vertebrae without degenerative changes. Our correlation coefficient was slightly lower than that reported in previous studies [13, 25] since all our subjects were men who were more likely to have spinal diseases with more severe degenerative changes.
We identified lumbar DXA-derived BMD T-score and vertebral CT-HU thresholds matching BMD T-score of − 2.0 and − 1.5 from linear regression equations in vertebrae without degenerative changes. All previous studies have identified a vertebral CT-HU threshold for distinguishing osteoporosis (T ≤ − 2.5) from osteopenia (− 2.5 < T < − 1)[26]. Pickhardt et al., in a study of 1,867 participants, reported the L1 thresholds which matched a BMD T-score of − 2.5 was 135 HU[10]. Zou et al. reported that the vertebral CT-HU thresholds matching a T-score of − 2.5 were 110, 100, 85 and 80 HU for L1, L2, L3 and L4, respectively [13]. The vertebral CT-HU thresholds obtained from our study are similar to that obtained from previous studies [12, 13, 25]. However, it is impossible to directly compare the validity of the thresholds obtained from the present study to that of previous studies because of the present study’s BMD T-scores < − 1.5 and − 2.0 set as the intervention thresholds for CTIBL[7, 14].
In this study, osteoporosis treatment targets were selected in all patients, including patients with lumbar degeneration. The percentage of patients in need of osteoporosis treatment as determined by lumbar DXA-derived BMD was about half that evaluated using both lumbar and hip BMD from DXA or vertebral CT-HU value. These data may indicate that assessment of lumbar DXA-derived BMD alone underestimates the number of patients who need anti-osteoporosis treatment in PCa patients, who have a high frequency of lumbar degeneration. The vertebral CT-HU measurement has several advantages, including: 1) being a simple and easy measurement for urologists to assess using the routine PCa staging CT, 2) accurate measurement by exclusion of regions with obvious spinal degeneration or aorta calcification, 3) finely distinguishing between cortical bone which is less affected by osteoporosis and trabecular bone that is more affected by osteoporosis[27,28,29,30], and 4) it can be available at no additional costs and without additional radiation exposure.
There were some limitations in this study. This study had a small sample size. Second, this study only included Japanese patients; thus, its results may not be generalizable to other populations. Third, the relationship between the CT-HU value and fracture risk were not evaluated in this study. Further studies with larger sample size are necessary to investigate whether the lumbar CT-HU values can predict fracture risk and be used as a complementary screening tool for bone health.
In conclusion, lumbar degenerative disease is a common comorbidity in elderly PCa patients, and lumbar DXA-derived BMD may be overestimated. The vertebral CT-HU value provides additive information to better identify PCa patients who need CTIBL prevention.
References
Rebbeck TR, Haas GP (2014) Temporal trends and racial disparities in global prostate cancer prevalence. Can J Urol 21:7496–7506
Shahinian VB, Kuo YF, Freeman JL, Goodwin JS (2005) Risk of fracture after androgen deprivation for prostate cancer. N Engl J Med 352:154–164. https://doi.org/10.1056/NEJMoa041943
Abrahamsen B, Nielsen MF, Eskildsen P, Andersen JT, Walter S, Brixen K (2007) Fracture risk in Danish men with prostate cancer: a nationwide register study. BJU Int 100:749–754. https://doi.org/10.1111/j.1464-410X.2007.07163.x
Kato S, Kawase M, Kato D, Ishida T, Uno M, Fujimoto Y, Masue T, Masue N, Deguchi T (2019) Decrease of bone mineral density in Japanese patients with non-metastatic prostate cancer treated with androgen deprivation therapy. J Bone Miner Metab 37:72–80. https://doi.org/10.1007/s00774-017-0897-5
Hager B, Kraywinkel K, Keck B, Katalinic A, Meyer M, Zeissig SR, Scheufele R, Wirth MP, Huber J (2017) Increasing use of radical prostatectomy for locally advanced prostate cancer in the USA and Germany: a comparative population-based study. Prostate Cancer Prostatic Dis 20:61–66. https://doi.org/10.1038/pcan.2016.43
Hadji P, Aapro MS, Body JJ, Gnant M, Brandi ML et al (2017) Management of Aromatase Inhibitor-Associated Bone Loss (AIBL) in postmenopausal women with hormone sensitive breast cancer: Joint position statement of the IOF, CABS, ECTS, IEG, ESCEO IMS, and SIOG. J Bone Oncol 7:1–12. https://doi.org/10.1016/j.jbo.2017.03.001
Fukumoto S, Soen S, Taguchi T, Ishikawa T, Matsushima H, Terauchi M, Horie S, Yoneda T, Sugimoto T, Matsumoto T (2020) Management manual for cancer treatment-induced bone loss (CTIBL): position statement of the JSBMR. J Bone Miner Metab 38:141–144. https://doi.org/10.1007/s00774-020-01087-0
Cianferotti L, Bertoldo F, Carini M, Kanis JA, Lapini A, Longo N, Martorana G, Mirone V, Reginster JY, Rizzoli R, Brandi ML (2017) The prevention of fragility fractures in patients with non-metastatic prostate cancer: a position statement by the international osteoporosis foundation. Oncotarget 8:75646–75663. https://doi.org/10.18632/oncotarget.17980
Baim S, Binkley N, Bilezikian JP, Kendler DL, Hans DB, Lewiecki EM, Silverman S (2008) Official Positions of the International Society for Clinical Densitometry and executive summary of the 2007 ISCD Position Development Conference. J Clin Densitom 11:75–91. https://doi.org/10.1016/j.jocd.2007.12.007
Pickhardt PJ, Pooler BD, Lauder T, del Rio AM, Bruce RJ, Binkley N (2013) Opportunistic screening for osteoporosis using abdominal computed tomography scans obtained for other indications. Ann Intern Med 158:588–595. https://doi.org/10.7326/0003-4819-158-8-201304160-00003
Pickhardt PJ, Lee LJ, del Rio AM, Lauder T, Bruce RJ, Summers RM, Pooler BD, Binkley N (2011) Simultaneous screening for osteoporosis at CT colonography: bone mineral density assessment using MDCT attenuation techniques compared with the DXA reference standard. J Bone Miner Res 26:2194–2203. https://doi.org/10.1002/jbmr.428
Schreiber JJ, Anderson PA, Rosas HG, Buchholz AL, Au AG (2011) Hounsfield units for assessing bone mineral density and strength: a tool for osteoporosis management. J Bone Jt Surg Am 93:1057–1063. https://doi.org/10.2106/jbjs.J.00160
Zou D, Li W, Deng C, Du G, Xu N (2019) The use of CT Hounsfield unit values to identify the undiagnosed spinal osteoporosis in patients with lumbar degenerative diseases. Eur Spine J 28:1758–1766. https://doi.org/10.1007/s00586-018-5776-9
Gralow JR, Biermann JS, Farooki A, Fornier MN, Gagel RF, Kumar R, Litsas G, McKay R, Podoloff DA, Srinivas S, Van Poznak CH (2013) NCCN Task Force Report: Bone Health In Cancer Care. J Natl Compr Canc Netw 11:S1-50. https://doi.org/10.6004/jnccn.2013.0215 (quiz S51)
Kim JY, Ryu DS, Paik HK, Ahn SS, Kang MS, Kim KH, Park JY, Chin DK, Kim KS, Cho YE, Kuh SU (2016) Paraspinal muscle, facet joint, and disc problems: risk factors for adjacent segment degeneration after lumbar fusion. Spine J 16:867–875. https://doi.org/10.1016/j.spinee.2016.03.010
Mohler JL, Armstrong AJ, Bahnson RR, D’Amico AV, Davis BJ et al (2016) Prostate cancer, version 1.2016. J Natl Compr Canc Netw 14:19–30. https://doi.org/10.6004/jnccn.2016.0004
Alibhai SM, Rahman S, Warde PR, Jewett MA, Jaffer T, Cheung AM (2006) Prevention and management of osteoporosis in men receiving androgen deprivation therapy: a survey of urologists and radiation oncologists. Urology 68:126–131. https://doi.org/10.1016/j.urology.2006.01.054
Alibhai SM, Yun L, Cheung AM, Paszat L (2012) Screening for osteoporosis in men receiving androgen deprivation therapy. JAMA 307:255–256. https://doi.org/10.1001/jama.2011.2022
Muraki S, Yamamoto S, Ishibashi H, Horiuchi T, Hosoi T, Orimo H, Nakamura K (2004) Impact of degenerative spinal diseases on bone mineral density of the lumbar spine in elderly women. Osteoporos Int 15:724–728. https://doi.org/10.1007/s00198-004-1600-y
Tenne M, McGuigan F, Besjakov J, Gerdhem P, Åkesson K (2013) Degenerative changes at the lumbar spine-implications for bone mineral density measurement in elderly women (in eng). Osteoporos Int 24:1419–1428. https://doi.org/10.1007/s00198-012-2048-0
Lewiecki EM, Kendler DL, Kiebzak GM, Schmeer P, Prince RL, El-Hajj Fuleihan G, Hans D (2004) Special report on the official positions of the International Society for Clinical Densitometry. Osteoporos Int 15:779–784. https://doi.org/10.1007/s00198-004-1677-3
El Maghraoui A, Mouinga Abayi DA, Rkain H, Mounach A (2007) Discordance in diagnosis of osteoporosis using spine and hip bone densitometry. J Clin Densitom 10:153–156. https://doi.org/10.1016/j.jocd.2006.12.003
Woodson G (2000) Dual X-ray absorptiometry T-score concordance and discordance between the hip and spine measurement sites. J Clin Densitom 3:319–324. https://doi.org/10.1385/jcd:3:4:319
Mounach A, Abayi DA, Ghazi M, Ghozlani I, Nouijai A, Achemlal L, Bezza A, El Maghraoui A (2009) Discordance between hip and spine bone mineral density measurement using DXA: prevalence and risk factors. Semin Arthritis Rheum 38:467–471. https://doi.org/10.1016/j.semarthrit.2008.04.001
Choi MK, Kim SM, Lim JK (2016) Diagnostic efficacy of Hounsfield units in spine CT for the assessment of real bone mineral density of degenerative spine: correlation study between T-scores determined by DEXA scan and Hounsfield units from CT. Acta Neurochir (Wien) 158:1421–1427. https://doi.org/10.1007/s00701-016-2821-5
Prevention and management of osteoporosis (2003) (in eng). World Health Organ Tech Rep Ser 921:1–164, back cover
Link TM, Lang TF (2014) Axial QCT: clinical applications and new developments. J Clin Densitom 17:438–448. https://doi.org/10.1016/j.jocd.2014.04.119
Lenchik L, Shi R, Register TC, Beck SR, Langefeld CD, Carr JJ (2004) Measurement of trabecular bone mineral density in the thoracic spine using cardiac gated quantitative computed tomography. J Comput Assist Tomogr 28:134–139. https://doi.org/10.1097/00004728-200401000-00023
Mueller DK, Kutscherenko A, Bartel H, Vlassenbroek A, Ourednicek P, Erckenbrecht J (2011) Phantom-less QCT BMD system as screening tool for osteoporosis without additional radiation. Eur J Radiol 79:375–381. https://doi.org/10.1016/j.ejrad.2010.02.008
Yu EW, Bouxsein ML, Roy AE, Baldwin C, Cange A, Neer RM, Kaplan LM, Finkelstein JS (2014) Bone loss after bariatric surgery: discordant results between DXA and QCT bone density. J Bone Miner Res 29:542–550. https://doi.org/10.1002/jbmr.2063
Acknowledgements
The authors wish to thank the investigators, their staff, and the affiliated institutions for their important contributions to this study at Toyonaka Municipal Hospital: Dr. Hiromu Horitani; Tetsuya Yamamoto; Yuta Oki.
Author information
Authors and Affiliations
Contributions
M.S., M.K., S.K., H.Y. and O.M. contributed to conception and design of the study. M.S., M.K. and T.K. contributed to analysis and interpretation of data. M.S., A.M., R.M., M.A., N.U., J.N., N.T. and O.M. contributed to collection and assembly of data. M.S., M.K., N.U., H.Y. and O.M. contributed to drafting of the article. All the authors contributed to critical revision of the article for important intellectual content and final approval of the article.
Corresponding author
Ethics declarations
Conflict of interest
Mototaka Sato, Masafumi Kashii, Atsuki Matsukawa, Ryoya Mizuno, Mai Akiyama, Takashi Kamatani, Satoshi Kamido, Norichika Ueda, Jiro Nakayama, Norihide Tei, Hideki Yoshikawa and Osamu Miyake declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Sato, M., Kashii, M., Matsukawa, A. et al. Assessment of bone health in patients with prostate cancer using cancer staging computed tomography. J Bone Miner Metab 40, 648–656 (2022). https://doi.org/10.1007/s00774-022-01328-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-022-01328-4