Abstract
Degenerative diseases of lumbar spine commonly noted in elderly people may affect their lumbar spine bone mineral density (BMD). The aim of this study is to determine whether the degree of degenerative spinal diseases is correlated with lumbar spine and femoral neck BMD. This study included 630 women age 60 years or over (mean age 73.3 ± 6.9 years) visiting the Osteoporosis Outpatient Clinic at the Tokyo Metropolitan Geriatric Medical Center. Subjects underwent anteroposterior and lateral X-rays of the lumbar spine. The score of degenerative spinal diseases for each subject was calculated according to the scores for the Kellgren-Lawrence method, osteophyte formation, bone sclerosis, disk space narrowing, and spondylolisthesis involving L1-L2 through L4-L5 interspaces. Moreover, the number of vertebral fractures at L2 through L4 was recorded. The BMD of the second to fourth lumbar spine from anteroposterior projections and femoral neck were measured using an Expert-5000 (GE Lunar, Madison, WI USA). Most subjects had degenerative diseases of the lumbar spine. Scores for the Kellgren-Lawrence method, osteophyte formation, bone sclerosis, disk space narrowing, and spondylolisthesis were positively correlated with lumbar spine BMD, while they were not correlated with femoral neck BMD. Multiple regression analysis indicated that the scores for osteophyte formation, bone sclerosis, and disk space narrowing were independently correlated with lumbar spine BMD. Thus, in this study, the scores for degenerative spinal diseases were correlated with lumbar spine BMD, while they were not correlated with femoral neck BMD. This discrepancy indicates that degenerative spinal diseases are associated with increased lumbar spine BMD measurements. Femoral neck BMD therefore may be more appropriate than lumbar spine BMD in evaluating osteoporosis in elderly women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis has been a serious problem in an aging society. Measurement of the lumbar spine bone mineral density (BMD) by dual-energy X-ray absorptiometry is now accepted as a standard means for the evaluation of osteoporosis. However, most elderly people have degenerative diseases of the spine, such as osteophyte formation, bone sclerosis, disk space narrowing, spondylolisthesis, and vertebral fractures, which were reported to affect their lumbar spine BMD [1, 2, 3, 4, 5]. However, review of the literature indicated that many previous studies were performed based just on the presence or absence of degenerative spinal diseases [1, 3, 4] or that only one degenerative item was used to evaluate the effect of degenerative spinal disease on lumbar spine BMD [2, 5]. In reality, the degree of degenerative spinal disease may also affect lumbar spine BMD, and degenerative spinal diseases such as osteophyte formation, bone sclerosis, disk space narrowing, spondylolisthesis, and vertebral fractures may be correlated with one another. The aim of this study is to determine whether the grade of the Kellgren-Lawrence method, osteophyte formation, bone sclerosis, disk space narrowing, spondylolisthesis, and the number of vertebral fractures are correlated with each other, and whether lumbar spine BMD is correlated with the degree of each item, using multiple regression analysis.
Subjects and methods
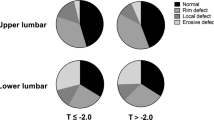
This study included 630 women age 60 years or over who visited the Osteoporosis Outpatient Clinic at the Tokyo Metropolitan Geriatric Medical Center from April 1999 to October 2000. Women who had femoral neck fractures, osteoarthritis of the hip, and hemiplegia, which affect femoral neck BMD, were excluded from this study. The mean age of the subjects was 73.3 ± 6.9 years. Upon entry into this study, body height and weight were measured, and body mass index (BMI) was calculated. Subjects underwent anteroposterior and lateral X-rays of the lumbar spine including L1 to L5. The score of degenerative spinal diseases for each subject was calculated according to grade in the Kellgren-Lawrence method [6], osteophyte formation, bone sclerosis, disk space narrowing, and spondylolisthesis involving L1-L2 through L4-L5 interspaces. Osteophyte formation was categorized into five grades (0–4) according to the Nathan classification [7]. Bone sclerosis was categorized into three grades of 0 (none), 1 (slight), and 2 (severe). The width of bone sclerosis from the endplate of the vertebral body was measured at the widest site. As for L1-L2 and L4-L5, the width of bone sclerosis was measured at the upper side of L2 and the bottom side of L4, respectively. As for L2-L3, it was measured at both the bottom side of L2 and the upper side of L3, and the wider side was chosen as the width of bone sclerosis at L2-L3, and as for L3-L4, it was measured in the same way. Grade 1 sclerosis was defined as less than 2 mm of the vertebrae and grade 2 sclerosis as at least 2 mm of the vertebrae. Disk space narrowing was categorized into three grades of 0 (none), 1 (slight), and 2 (severe). Grade 1 narrowing was less than 2 mm loss of disk space and grade 2 narrowing was at least 2 mm loss of disk space. Spondylolisthesis was categorized into five grades (0–4) according to the Meyerding method [8]. The radiographs were read to identify the presence and severity of each item at the L1-L2 through L4-L5 interspaces, and the sum of the scores for each item was calculated. The lateral radiographs were read to identify the number of vertebral fractures at L2 through L4. Vertebral fracture was assessed in terms of three findings: a wedge, biconcave, or crush appearance [9]. A wedge appearance was defined as a site where the anterior height of the vertebra was 75% or less than its posterior height, a biconcave appearance was where the height of the center part of a vertebra was 80% or less than that of the anterior and posterior parts of the vertebra, and a crush appearance was where the height of the anterior, center, and posterior parts of an axial vertebra were all reduced to 80% or less of the normal value. The grade of degenerative diseases was read by one observer (S.M.). To assess the intraobserver reproducibility and interobserver reliability of these methods, 40 radiographs were read by the same observer 3 months later, and 130 radiographs were read by another observer (S.Y.). BMD of the lumbar spine and femoral neck were measured using the Expert-5000 (GE Lunar, Madison, WI, USA). Measurements were obtained from anteroposterior projections of the second to fourth lumbar vertebrae and femoral neck. Statistical analysis was performed using Statview 5.0 (Abacus Concepts, Berkeley, CA, USA). Weighted κ statistic was used to examine intraobserver reproducibility and interobserver reliability. Linear regression analysis was used to determine the correlation of the lumbar spine and femoral neck BMD with age. Spearman rank correlation coefficient was used to determine the association among the scores from the Kellgren-Lawrence method, osteophyte formation, bone sclerosis, disk space narrowing, and spondylolisthesis, and the number of vertebral fractures. Multiple regression analysis was used to determine the correlation of the lumbar spine and femoral neck BMD with the scores for the Kellgren-Lawrence method, osteophyte formation, bone sclerosis, disk space narrowing, and spondylolisthesis, and the number of vertebral fractures after adjustment for age and BMI. Furthermore, the independent effects of age, BMI, and the score for each degenerative item, on BMD were analyzed using multiple regression analysis. On the basis of the multiple regression analysis, adjusted lumbar spine BMD was calculated, and the correlation between age and adjusted lumbar spine BMD was determined using linear regression analysis. Furthermore, The correlation coefficient between observed lumbar spine BMD and femoral neck BMD, and between adjusted lumbar spine BMD and femoral neck BMD, was compared using analysis of variance. Statistical significance was defined as P<0.05.
Results
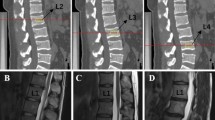
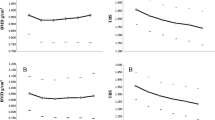
Table 1 shows the characteristics of the subjects. Intraobserver and interobserver agreement of these methods were high (Table 2). Lumbar spine BMD had no correlation with age, while femoral neck BMD had a significant correlation with age (r=0.02, P=0.9669; r=−0.303; P=<0.0001, respectively). Degenerative spinal diseases were noted in virtually all of the subjects (Table 3). The scores for the Kellgren-Lawrence method, osteophyte formation, bone sclerosis, and disk space narrowing had a moderate or strong correlation with one another, though the number of vertebral fractures and the score for spondylolisthesis had no or weak correlation with the score for other items (Table 4). Figure 1 shows lumbar spine and femoral neck BMD by the severity of each degenerative disease. The scores for the Kellgren-Lawrence method, osteophyte formation, bone sclerosis, disk space narrowing, and spondylolisthesis were positively correlated with lumbar BMD, though they were not correlated with femoral neck BMD (Table 5). The number of vertebral fractures was negatively correlated with both lumbar spine and femoral neck BMD (Table 5). In multiple regression analysis, the scores for osteophyte formation, bone sclerosis, and disk space narrowing, and the number of vertebral fractures were correlated with the BMD of the lumbar spine; however, the scores for spondylolisthesis were not (Table 6). The score for the Kellgren-Lawrence method was not included in the multiple regression analysis, because it was strongly correlated with osteophyte formation, bone sclerosis, and disk space narrowing. On the basis of this multiple regression analysis, osteophyte formation, bone sclerosis, and disk space narrowing were selected as degenerative spinal diseases that significantly increased lumbar spine BMD measurements, and a degenerative score for each subject was calculated as follows: degenerative score = the score for osteophyte formation + the score for bone sclerosis + the score for disk space narrowing. Eleven (1.7%) subjects had zero points for a degenerative score. The degenerative score was positively correlated with age (Fig. 2) and lumbar spine BMD (Fig. 3A), though it was not correlated with femoral neck BMD (Fig. 3B). The value for lumbar spine BMD after adjustment for osteophyte formation, bone sclerosis, and disk space narrowing can be predicted as follows: adjusted lumbar spine BMD = observed lumbar spine BMD – [0.006 x (the score for osteophyte formation)] – [0.02 x (the score for bone sclerosis)] – [0.011 x (the score for disk space narrowing)]. Adjusted lumbar spine BMD had a weak correlation with age (r=0.138, P<0.01). The correlation coefficient between adjusted lumbar spine BMD and femoral neck BMD was 0.597, which was not significantly higher than that between observed lumbar spine BMD and femoral neck BMD.
A Kellgren-Lawrence method, B osteophyte formation, C bone sclerosis, D disk space narrowing, E spondylolisthesis, F vertebral fracture. Lumbar spine and femoral neck BMD by the severity of each degenerative disease. Subjects were divided into five categories by the score for each degenerative disease. In the case of spondylolisthesis, the number of subjects with a score of two or more was small, so subjects were divided into three categories. In the case of vertebral fracture, subjects were divided into four categories
Discussion
This study demonstrated that degenerative diseases of the lumbar spine commonly occurred among elderly people age 60 years or over. However, the subjects in this study were patients admitted to Tokyo Metropolitan Geriatric Medical Center, and thus the proportion of those who had degenerative diseases of the spine might be larger than in the general population.
Lumbar spine BMD was positively correlated with the scores for the Kellgren-Lawrence method, osteophyte formation, bone sclerosis, disk space narrowing, and spondylolisthesis. In contrast, femoral neck BMD was not significantly correlated with the score for degenerative spinal diseases. This discrepancy indicates that degenerative spinal diseases increase lumbar spine BMD measurements. Thus, in subjects with severe degenerative spinal diseases, osteoporosis may be underestimated if assessed by lumbar spine BMD.
Lumbar spine BMD has been reported to fall with age in postmenopausal women [10], although no such correlation was noted in this study. This may be mainly due to degenerative diseases of the lumbar spine. In fact, the correlation between age and lumbar spine BMD was improved after adjustment with the score for degenerative spinal diseases. However, the correlation coefficient between the adjusted lumbar spine BMD and femoral neck BMD was not significantly higher than that between the observed lumbar spine BMD and femoral neck BMD, which may indicate that the differences between lumbar spine and femoral neck BMD were not only due to degenerative spinal diseases.
This study showed that the number of vertebral fractures was negatively correlated with both lumbar spine and femoral neck BMD, which do not indicate that vertebral fractures decreased lumbar spine BMD measurements but that subjects with vertebral fractures had more severe osteoporosis.
Multiple regression analysis in this study showed that the scores for osteophyte formation, bone sclerosis, and disk space narrowing were independently correlated with lumbar spine BMD. Using multiple regression analysis, adjusted lumbar spine BMD was calculated in this study as follows: adjusted lumbar spine BMD = observed lumbar spine BMD − [0.006 x (the score for osteophyte formation)] − [0.020 x (the score for sclerosis)] − [0.011 x (the score for disk space narrowing)]. The number of vertebral fractures was also significantly correlated with lumbar spine BMD. However, the number of vertebral fractures was not included in the formula for adjusted lumbar spine BMD, for the aforementioned reason. Applying the mean score in each degenerative spinal disease to the formula resulted in adjusted lumbar spine BMD being 0.119 g/cm2 lower than observed lumbar spine BMD. This amount was 15.0% of the mean lumbar spine BMD of the subjects in this study, which is not a negligible amount. Elderly women age 60 or over are predisposed to degenerative spinal diseases that greatly affect lumbar spine BMD measurements. This should be taken into account in the evaluation of the lumbar spine BMD, or the risk of osteoporosis may be overlooked.
The most harmful problem caused by osteoporosis was hip fractures. Hip fractures lower ADL and QOL and also increase mortality [11, 12, 13]. Mandatory evaluation of the risk of hip fractures is thus required. Measurement of the lumbar spine BMD is now commonly accepted as the standard means for the evaluation of osteoporosis, especially in Japan. However, since (1) elderly people are predisposed to degenerative spinal diseases as evidenced in this study, (2) degenerative spinal diseases greatly affect lumbar spine BMD measurements, and (3) femoral neck BMD was shown to be the better [14, 15, 16] and total neck BMD the best site [17] to evaluate risk for hip fracture, osteoporosis may be better evaluated by means of femoral neck or total neck BMD in principle. Only if subjects have diseases of hip joints, such as osteoarthritis of the hip, and femoral neck fractures, should lumbar spine BMD be used in the evaluation of osteoporosis. In conclusion, the scores for the Kellgren-Lawrence method, osteophyte formation, bone sclerosis, and disk space narrowing were strongly correlated with one another. The scores for the Kellgren-Lawrence method, osteophyte formation, bone sclerosis, disk space narrowing, and spondylolisthesis were positively correlated with lumbar spine BMD. The scores for osteophyte formation, bone sclerosis, and disk space narrowing were independently correlated with lumbar spine BMD.
References
Paiva LC, Filardi S, Pinto-Neto AM et al (2002) Impact of degenerative radiographic abnormalities and vertebral fractures on spinal bone density of women with osteoporosis. Sao Paulo Med J 120(1):9–12
Dalle Carbonare L, Giannini S, Sartori L et al (2000) Lumbar osteoarthritis, bone mineral density, and quantitative ultrasound. Aging (Milan) 12(5):360–365
Kinoshita H, Tamaki T, Hashimoto T et al (1998) Factors influencing lumbar spine bone mineral density assessment by dual-energy X-ray absorptiometry: comparison with lumbar spinal radiogram. J Orthop Sci 3(1):3–9
Rand T, Schneider B, Grampp S et al (1997) Influence of osteophytic size on bone mineral density measured by dual X-ray absorptiometry. Acta Radiol 38(2):210–213
Vogt MT, Rubin DA, San Valentin R et al (1999) Degenerative lumbar listhesis and bone mineral density in elderly women: the study of osteoporotic fractures. Spine 24(23):2536–2541
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16:494–502
Nathan H, Israel J (1962) Osteophytes of the Vertebral Column. J Bone Joint Surg 44:243–268
Meyerding HW (1932) Spondylolisthesis. Surg Gynec Obstet 54:371–377
Inoue T (1990) [Clinical features and findings: osteoporosis] (in Japanese). Bone 4:39–47
Fujiwara S, Fukunaga M, Nakamura T et al (1998) Rates of change in spinal bone density among Japanese women. Calcif Tissue Int 63(3):202–207
Fisher ES, Baron JA, Malenka DJ et al. Hip fracture incidence and mortality in New England. Epidemiology 1991; 2(2):116–22
Magaziner J, Simonsick EM, Kashner TM et al (1989) Survival experience of aged hip fracture patients. Am J Public Health 79(3):274–278
Pitto RP (1994) The mortality and social prognosis of hip fractures: a prospective multifactorial study. Int Orthop 18(2):109–113
Bouxsein ML, Palermo L, Yeung C et al (2002) Digital X-ray radiogrammetry predicts hip, wrist and vertebral fracture risk in elderly women: a prospective analysis from the study of osteoporotic fractures. Osteoporos Int 13(5):358–365
Cummings SR, Bates D, Black DM (2002) Clinical use of bone densitometry: scientific review. JAMA 288(15):1889–1897
Kanis JA (2002) Diagnosis of osteoporosis and assessment of fracture risk. Lancet 359:1929–1936
Kanis JA (2000) An update on the diagnosis and assessment of osteoporosis with densitometry. Osteoporos Int 11:192–202
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Muraki, S., Yamamoto, S., Ishibashi, H. et al. Impact of degenerative spinal diseases on bone mineral density of the lumbar spine in elderly women. Osteoporos Int 15, 724–728 (2004). https://doi.org/10.1007/s00198-004-1600-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-004-1600-y