Abstract
Purpose
The increased social and economic burdens make osteoporosis in men an emerging public health issue. However, the quality of life among men with osteoporosis is still unclear. This systematic review and meta-analysis aimed to evaluate the health-related quality of life (HRQoL) among men with osteoporosis or osteoporotic fracture.
Methods
PubMed, EMBASE, and the Cochrane Library database were systematically searched from inception to May 2021. Studies were included if they used validated questionnaires to measure HRQoL among osteoporotic men. A meta-analysis was performed using a random-effects model or fixed-effects model to calculate the standard mean difference (SMD) or mean difference (MD) with 95% confidential interval (95% CI).
Results
14 studies involving 6338 male participants were chosen for systematic review, of which 10 were included in the meta-analysis. Men with osteoporosis had poorer global HRQoL and multiple dimensions of HRQoL than men without osteoporosis. Hip fracture, vertebral fractures, or wrist fractures dramatically impaired HRQoL of men, and physical function was declined even before hip fracture (SMD = −0.60, 95% CI, −0.82 to −0.39). Femoral and lumbar BMD was positively correlated with HRQoL, and a number of fragility fractures and time since fracture had negative effects on HRQoL. Effective anti-osteoporotic drugs could improve HRQoL of men.
Conclusion
The health-related life quality of men was significantly impaired by osteoporosis and fracture of the hip, vertebral, or wrist. We should pay more attention to the diagnosis and treatment of male osteoporosis to improve the life quality of men.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a systemic skeletal disease characterized by low bone mass and microarchitectural deterioration of bone tissue with a high risk of bone fracture. With a rapid population aging in China, osteoporosis has become a significant public issue not only in women but also in men. It is estimated 133.9 million men over 50 years old in China, and the prevalence of osteoporosis was 6.0% in men [1, 2]. Osteoporotic vertebral fracture and hip fracture were found in 17.0% and 2.1% of men of China [3, 4]. For Chinese men aged 50–90 years, approximately 8.7% of men would sustain a major osteoporotic fracture during their remaining lifetime [5]. Men tended to have more osteoporosis-related complications and higher mortality after osteoporotic fracture than women [6]. Approximately one-third of men would die of complications of bone fracture within the first year after a hip fracture [7]. Although the prevalence of osteoporosis and osteoporotic fracture were fairly high and their consequences were quite serious, osteoporosis remained under-recognized and undertreated in men.
Osteoporosis had negative effects on health status, which was mainly reflected from the assessment of the health-related quality of life (HRQoL) among postmenopausal women with osteoporosis. HRQoL was an individual’s ability to carry out some pre-defined activities and an individual’s subjective sense of well-being in physical, mental, and social domains of health [8]. HRQoL measurement was of great significance to evaluate the impacts of chronic diseases on patients and the cost-effectiveness of different therapies. Although osteoporosis had obvious adverse impacts on men, men with osteoporosis scarcely received an assessment of HRQoL, even after the fragility fractures. Previous systematic reviews and meta-analysis reported patients with osteoporotic fractures had significant decrements in overall health state utility values, an index which was used to measure health preferences and often used for economic evaluations [9, 10]. Another meta-analysis also demonstrated vertebral fractures had adverse effects on HRQoL of older patients, especially in the physical domain [11]. However, all the studies only included a paucity of male patients. There was also little information about what effects osteoporosis-related conditions had on male patients and which domain of HRQoL was preferentially affected. As far as we know, there was no meta-analysis focusing on the effects of osteoporosis or osteoporotic fracture on the HRQoL of male patients.
Therefore, we performed a systematic review and meta-analysis about the impacts of osteoporosis or osteoporotic fractures on men to (1) evaluate the differences in HRQoL between men with and without osteoporosis, (2) identify the effects of osteoporotic fracture-related conditions on an overall and different dimension of HRQoL among men, (3) analyze the potential factors associated with HRQoL outcomes among men with osteoporosis, (4) investigate whether anti-osteoporotic therapies could improve the HRQoL of men.
Methods
This study was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. The protocol was registered on PROSPERO (https://www.crd.york.ac.uk/PROSPERO), the international prospective register of systematic reviews (CRD42020199627).
Search strategy
A systematic literature search was performed in PubMed, EMBASE, and the Cochrane Library from the inception of each database to May 2021. Bibliographies of included studies were manually checked for any pertinent studies. The following terms were used to identify the targeted population: osteoporosis, osteopenia, low-trauma fracture, low-energy fracture, fragility fracture, in combination with male, man, and men. We used the following terms to identify HRQoL: health-related quality of life, HRQoL, QoL, life quality, and health status.
Eligibility criteria
We applied inclusion and exclusion criteria to select studies of interest. Studies were eligible if they aimed to measure HRQoL using a validated questionnaire among men with osteoporosis or osteoporotic fracture. We included observational studies and intervention trials that reported the baseline HRQoL of men with osteoporosis. Osteoporosis was defined as low bone mineral density (BMD) with T-score ≤ −2.5, or with fragility fractures according to the criteria of the World Health Organization [12] or using the specific, validated criteria by clinicians. Low-trauma fracture of the hip, spine, proximal humerus, or distal forearm was included. If the same population was used by multiple articles with the same study design, the one with the most relevant data was included.
Studies were excluded if they were: (1) focusing on secondary osteoporosis caused by glucocorticoid therapy, rheumatoid arthritis, hyperparathyroidism, renal disease, malabsorption disease, hereditary bone disease, and so on; (2) concentrating on high-energy fractures; (3) conference abstracts, case studies or review; (4) written in language that could not be translated into English; (5) reporting only aggregate HRQoL values for osteoporotic groups without separate data of men.
Data extraction
Titles and abstracts of articles identified by the search were independently screened by two reviewers. Potentially eligible studies were subsequently assessed for inclusion based on a full-text review. One reviewer extracted data from the included study which was validated by the second reviewer. The collected data included the first author, publication year, country, study design, participant characteristics, methods for the diagnosis of osteoporosis and osteoporotic fracture, HRQoL tools, factors associated with HRQoL outcomes, significant results, and conclusion.
Methodological quality assessment
The methodological quality and bias of the included studies were assessed by two independent researchers according to the Newcastle–Ottawa Scale (NOS) adapted for observational studies [13, 14]. Studies were rated as good quality when they scored more than half of the total score. However, studies were incorporated for analysis, irrespective of NOS scores.
Meta-analysis
It was previously hypothesized that there would be a significant discrepancy between HRQoL instruments applied in the included studies. Consequently, when it came to pool the results from the different questionnaires, the following procedures were conducted to resolve this question: (1) synthesizing the subscales and overall HRQoL scores with good internal consistency; (2) ensuring uniformity of the direction of scale [11]; (3) using standardized mean difference (SMD) with corresponding 95% confidential interval (95% CI) to render them comparable irrespective of differences in the underlying constructs of the instruments [15]. Correspondingly, a random-effects model was used to calculate this effect size as different assessment tools may have various sensitive detection abilities to measure the impact of osteoporosis-related conditions [15]. An SMD of 0.80 was classified as a large difference between the two groups for comparison; 0.50, a moderate difference; and 0.20, a small difference [16]. We also calculated statistical heterogeneity by using Cochran’s chi-square test (Q test) and I2 statistic [17]. However, the mean difference with 95% CI was calculated using a fixed-effects model when combining the HRQoL outcomes measured by the same assessment tool and low heterogeneity existing among study results, which was considered as P > 0.1 and an I2 statistic below 50% [17]. The weight given to each study was the inverse of the variance of the effect estimate. Mean and standard deviation (SD) were estimated from sample size and interquartile range using a standard mathematical method when these were unavailable [15]. Meta-analysis results about the effects of osteoporosis or osteoporotic fracture on HRQoL were presented as forest plots. All statistical analyses were performed using Review Manager 5.4.1. All tests were two-tailed, and P < 0.05 was regarded as statistically significant.
Results
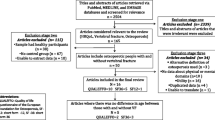
Studies selection
The initial database search for systematic reviews or meta-analyses yielded a total of 4601 records. An additional 16 studies were selected for inclusion in this review after screening reference lists of the retrieved articles and 527 duplicates were eliminated. 4074 records were screened based on titles and abstracts, of which 114 articles remained for full-text analysis. Finally, a total of 14 articles met the inclusion criteria of the systematic review. Studies were excluded from meta-analysis due to the unavailability of the mean, SD, or sample size, which could not be calculated manually. Thus, a total of 10 studies were incorporated into meta-analysis (Supplementary Fig. 1).
Characteristics of the included studies
Design, setting, and participants
All the eligible studies were consisting of three prospective cohort studies [18,19,20], four case-control studies [21,22,23,24], five cross-sectional studies [25,26,27,28,29], and two prospective cohort studies with cross-sectional data regarding HRQoL [30, 31] (Table 1). These articles originated from 11 countries: Mexico [18], Spain [19, 20], Turkey [21], China [22], USA [23], Japan [25, 29], UK [24, 31], Norway [26], Germany [27], Australia [28], and Iceland [30]. These clinical studies involved 6338 men, among which 1469 men were diagnosed with osteoporosis or osteoporotic fractures. There were 489 and 276 men experiencing vertebral or hip fractures, respectively. The mean age of men varied from 60.5 to 77 years [23, 25, 29,30,31]. Two studies recruited participants aged 40 years and older [21, 29], and most studies were conducted with the age of 50 years as the lower age limit for inclusion.
Diagnosis of osteoporosis or osteoporotic fractures
In five studies [21,22,23, 27, 31], osteoporosis was diagnosed according to the WHO criteria [12]. The osteoporotic fractures were defined based on the International Classification of Diseases, Tenth Revision (ICD10) diagnostic codes [30]. Five studies [22, 25, 26, 28, 29] focused on the association between vertebral fractures and HRQoL, which used Japanese Society of Bone and Mineral Research criteria, McCloskey–Kanis criteria [32], a quantitative morphometric method [33], Genant’s semi-quantitative method [34] to identify the vertebral fracture. Four studies recruited patients with low-energy fractures without mentioning the diagnosis criteria in detail [18,19,20, 24].
HRQoL instruments
Four generic measures and four disease-specific questionnaires were utilized. Descriptions of the reported HRQoL questionnaires were shown in Supplementary Table 1.
Risk of bias within studies
The overall bias risks of included studies were moderate (Supplementary Table 2). Patients in the most included studies were representatives of a community or population or recruited consecutively from the monocenter. Nearly all studies adjusted for at least one important confounder (Table 2).
Synthesis of results
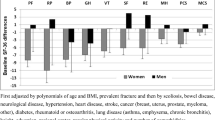
Differences in HRQoL between men with and without osteoporosis
Compared with men with normal BMD or representative group of males, osteoporotic men had poorer HRQoL [21, 27, 31] (Table 1, Supplementary Table 3). Osteoporosis in men had poorer outcomes of global HRQoL, physical function, general health, and bodily pain domains of SF-36. After accounting for age, BMI, physical activity, social class, cigarette and alcohol consumption, and comorbidities, osteoporosis was still correlated with increased odds for poorer general health (odds ratio, OR = 3.14, P = 0.03) and physical function (OR = 3.39, P = 0.03) of men [31]. Since there were no more related studies in China, we briefly compared HRQoL outcomes of patients from the included Chinese study [22] with a generally healthy population in China [35], and found an impaired mental health status in Chinese osteoporotic men, which was consistent with another study that found pain/discomfort and anxiety/depression were the most impacted dimension of EQ-5D [27].
Differences in HRQoL between men with and without osteoporotic fracture
Five studies reported the overall HRQoL in men with and without osteoporotic fracture [22, 26, 27, 29, 30]. Pooled results of these studies indicated a reduced HRQoL in the fracture group (SMD = −0.53, 95% CI, −1.01 to −0.05) but with substantial heterogeneity (I2 = 95%, P < 0.01) (Fig. 1).
Hip fracture dramatically impaired HRQoL of men [18, 20, 24]. Compared with men without fracture, patients had great declines in physical function score and mental function score within 6 months after hip fracture, especially in physical function score (fracture versus non-fracture: −9.21 ± 0.95 versus 3.11 ± 1.42, P < 0.001) [20]. The mean accumulated HRQoL loss for EQ-5D-5L utilities was 0.30 (0.22–0.37) during the first year after hip fracture [18]. Within the two years of hip fracture, physical function scores deteriorated to more than 1.7 SD below the national mean [24]. Moreover, a meta-analysis of studies indicated fracture cohort already had worse physical function even before hip fracture (SMD = −0.60, 95% CI, −0.82 to −0.39, I2 = 0%, P = 0.64) (Fig. 2).
Subsequently, an analysis of the impacts of vertebral fracture on HRQoL was conducted. Osteoporotic vertebral compressed fractures (OVCF) alone had attenuated but non-significant effects on overall HRQoL (SMD = −0.57, 95% CI, −1.28 to 0.15), along with high heterogeneity (I2 = 96%, P < 0.01) [22, 26, 29, 30]. Fixed-effects meta-analyses of EQ-5D scores in patients with vertebral fractures yielded similar results (MD = −0.01, 95% CI, −0.03 to 0.01) with low heterogeneity (I2 = 0%, P = 0.43). However, analysis of different dimensions indicated that vertebral fracture led to a significant decline in physical function (SMD = −0.35, 95% CI, −0.63 to −0.08, I2 = 0%, P = 0.90) [22, 29] and physical component scores (SMD = −0.64, 95% CI, −0.86 to −0.42, I2 = 0%, P = 0.94) [22, 25, 29] compared with control groups (Fig. 3). The results were consistent with another study, in which men with morphometric vertebral fractures were more than twice as likely to have a lower physical function (age-adjusted odds ratio: 2.51, 95% CI, 1.32–4.79) [28]. Bodily pain, mental health, and mental component scores domains had no significant difference between groups with and without vertebral fracture.
Similarly, men with wrist fracture also had significantly lower scores of physical components than men without wrist fracture (fracture versus non-fracture: −4.84 ± 1.07 versus 0.96 ± 1.76, P = 0.005) [19].
Factors associated with HRQoL outcomes of men with osteoporosis
A total of six predictors of HRQoL outcomes of male patients were reported, including femoral BMD, lumbar BMD, time since fracture, and number, type, and severity of fractures [21, 24, 26, 27, 31] (Table 2). Higher femoral BMD was associated with better HRQoL of patients in two studies, more predominantly in domains of physical function, social function, and general health [21, 31]. A similar correlation was also found between lumbar BMD and HRQoL [21]. A significant negative correlation was found between the number of fragility fractures or time since fracture and HRQoL (Table 2), while the number, type, and severity of vertebral fractures were thought to have no prominent effects on HRQoL loss [26]. Health status seemed to gradually deteriorate with time after fracture [24].
Anti-osteoporotic therapies and HRQoL
Researches about the effects of anti-osteoporotic therapy on HRQoL of men were extremely scarce. We only identified a 2-year longitudinal study that compared the efficacy of denosumab and alendronate in improving HRQoL of men with osteoporosis and non-metastatic prostate cancer who were receiving androgen deprivation therapy [36]. After receiving denosumab or alendronate treatment, patients in two groups had a significant improvement in their health conditions. The mean increases in mental component scores were 2.43 (95% CI: 1.71–3.03) and 2.52 (95% CI: 1.75–3.07), respectively, with an increase of 4.48 (95% CI: 3.71–5.25) or 4.53 (95% CI: 3.74–5.19) in the physical component score (Fig. 4).
Discussion
We systematically reviewed the literature pertaining to HRQoL of men with osteoporosis, to meta-analytically investigate the impacts of osteoporosis or osteoporotic fractures on HRQoL of men. Our results revealed that osteoporosis would obviously impair multiple dimensions of HRQoL of men. Physical function was the most affected after fragility fractures. Femoral and lumbar BMD was positively correlated with HRQoL of men, and the frequencies of all sites of fragility fracture were associated with HRQoL of men. Effective anti-osteoporotic drugs, such as denosumab and alendronate, were able to improve the life quality of men.
Osteoporosis and osteoporotic fractures were extremely harmful to the physical function and mental health status of men, which could be related to the following aspects. Firstly, bone loss with aging could not only reduce bone mass, but also damage bone microstructure, which led to increased cortical porosity, decreased cortical bone width and trabecular thickness, and increased trabecular separation [37, 38]. Secondly, low bone mass and deteriorated bone microstructure of men would result in impaired bone strength, which could induce low-energy fractures and re-fractures. Bone fracture would lead to bone pain, bone deformity, and trigger a series of serious consequences, such as decreased living abilities, anxiety and depression, cardiovascular and cerebrovascular complications, and so on, which were incredibly harmful to HRQoL of patients [39]. Thirdly, men with osteoporosis or fragility fractures usually had a prominent loss of muscle mass and strength, which would lead to functional impairment, high risk of fall, further endangering the life quality of men [40]. Moreover, men often had inappropriate lifestyles, such as smoking, alcohol addiction, sedentary lifestyle, lack of sunlight exposure, which would impair bone health and further damage the life quality of men [41].
Hip fracture was the most dangerous consequence of osteoporosis which could threaten HRQoL from several aspects. Hip fracture directly gave rise to limited mobility, high risk of deep venous thrombosis, even cardiovascular and cerebrovascular events, which not only reduced the HRQoL of men but also increased mortality [6]. Moreover, long-term bed rest, social deprivation, and high medical costs also contributed to the decline of HRQoL [42, 43]. Hip fracture patients were found to perceive poorer health status even prior to the fracture, which was regarded as a strong predictor of excessive mortality and poor outcome after hip fracture [44].
OVCF was one of the most common fractures, which were closely related to the decline of the physical function of HRQoL. As the majority of OVCF patients only received conservative treatments, OVCF could induce persistent bone pain, kyphosis or scoliosis, mobility limitation, which impaired the HRQoL of men [45]. Because OVCFs were usually asymptomatic, moderate, or severe vertebral deformities did not receive enough attention [46], and the impact of OVCF on the quality of life of men was often ignored. Because of the increased risk of refracture after vertebral fracture, it was of great clinical significance to diagnose OVCF early and take measures to prevent vertebral refracture in order to improve the life quality of men.
In this study, we found many factors correlating to HRQoL. Men with higher femoral and lumbar BMD were more prone to have better HRQoL. The correlation between BMD and HRQoL still existed after controlling for age and comorbidity [31]. Lower BMD indicated a compromised bone structure and strength, which was a strong predictor of fracture in men [47]. The frequencies of all sites of fragility fracture were associated with poorer HRQoL of men. Fear of undesirable consequences like falling, fractures, and immobility might be attributable to impaired HRQoL [48]. HRQoL was greatly declined in the shorter time after fracture and recovered afterward [49], but HRQoL of patients with fracture could hardly rebound to the previous level [50]. Continuous decline of health conditions may exist after fracture [24].
As osteoporotic men had remarkable decrements in HRQoL, increased morbidity and mortality, treatment for men with osteoporosis or osteoporotic fractures was necessary. Treatment for male osteoporosis included anti-resorptive and anabolic agents, which were represented by bisphosphonates, denosumab, and teriparatide. However, few studies observed the effects of anti-osteoporotic drugs on HRQoL of men. Only a study about androgen deprivation therapy for men with non-metastatic prostate cancer showed that denosumab and alendronate could significantly increase BMD of the patients and improve their health status. The results suggested a positive correlation between the anti-osteoporotic treatment and HRQoL outcomes of the patients [36]. It is necessary to conduct studies to evaluate the life quality of men with osteoporosis to establish an effective therapeutic strategy.
We thoroughly evaluated the HRQoL for the first time in men with osteoporosis or osteoporotic fractures through systematic review and meta-analysis. However, there were several limitations in this study. First, the included questionnaire of HRQoL was different and utilized among different groups. Hence, limited data could be synthesized and effect size estimate measured as SMD should be interpreted with cautions. Second, the sample size of prospective study about the impact of osteoporotic fracture on HRQoL of men was small. Third, included studies about the effects of anti-osteoporotic therapy on HRQoL of men were very rare, whether effective anti-osteoporotic agents could improve HRQoL of men was worth further study.
Conclusion
In this meta-analysis of clinical studies, osteoporosis and fragility fractures of the hip, spine, or wrist were demonstrated to remarkably reduce the physical and mental health status of men. Femoral and lumbar BMD was positively correlated with HRQoL, and a significant negative correlation was found between a number of fragility fractures and time since fracturing with HRQoL. Effective anti-osteoporotic drugs, such as denosumab and alendronate, may improve the life quality of men. In the future, large sample studies to evaluate the life quality of men with osteoporosis, especially the effects of anti-osteoporotic treatment on the life quality of men, still need to be carried out.
Data availability
All data generated or analyzed during this study are included in this published article.
References
The Chinese medical association of osteoporosis and bone mineral salt disease branch, The epidemiological survey of osteoporosis in China and the results of the “Healthy Bones” campaign were released. Chin J Osteoporos Bone Mineral Res 12, 317–318 (2019)
Bureau of Statistics of the People’s Republic of China. China Statistical Yearbook-2019 (2019). China Statistics Press, Beijing
Y. Ren, J. Hu, B. Lu, W. Zhou, B. Tan, Prevalence and risk factors of hip fracture in a middle-aged and older Chinese population. Bone 122, 143–149 (2019)
C. Gao, Y. Xu, L. Li, W.Q. Gu, C.T. Yi et al. Prevalence of osteoporotic vertebral fracture among community-dwelling elderly in Shanghai. Chin Med J 132, 1749–1751 (2019)
L. Si, T.M. Winzenberg, M. Chen, Q. Jiang, A.J. Palmer, Residual lifetime and 10 year absolute risks of osteoporotic fractures in Chinese men and women. Curr Med Res Opin 31, 1149–1156 (2015)
P. Haentjens, J. Magaziner, C.S. Colón-Emeric, D. Vanderschueren, K. Milisen et al. Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med 152, 380–390 (2010)
T. Tran, D. Bliuc, L. Hansen, B. Abrahamsen, J. van den Bergh et al. Persistence of excess mortality following individual nonhip fractures: a relative survival analysis. J Clin Endocrinol Metab 103, 3205–3214 (2018)
M. Karimi, J. Brazier, Health, health-related quality of life, and quality of life: what is the difference? Pharmacoeconomics 34, 645–649 (2016)
J.E. Brazier, C. Green, J.A. Kanis, A systematic review of health state utility values for osteoporosis-related conditions. Osteoporos Int 13, 768–776 (2002)
L. Si, T.M. Winzenberg, B. de Graaff, A.J. Palmer, A systematic review and meta-analysis of utility-based quality of life for osteoporosis-related conditions. Osteoporos Int 25, 1987–1997 (2014)
U.A. Al-Sari, J. Tobias, E. Clark, Health-related quality of life in older people with osteoporotic vertebral fractures: a systematic review and meta-analysis. Osteoporos Int 27, 2891–2900 (2016)
Assessment of fracture risk and its application to screening for postmenopausal osteoporosis, Report of a WHO Study Group. World Health Organ Tech Rep Ser 843, 1–129 (1994)
P.A. Modesti, G. Reboldi, F.P. Cappuccio, C. Agyemang, G. Remuzzi et al. Panethnic differences in blood pressure in Europe: a systematic review and meta-analysis. PLoS ONE 11, e0147601 (2016)
GA Wells, B Shea, D O'Connell, J Peterson, V. Welch, M. Losos, P. Tugwell, The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses (2011). Available from http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (eds). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane, 2019. Available from www.cochrane-handbook.org
J. Cohen, Statistical Power Analysis for the Behavioural Science, 2nd edn. (Lawrence Erlbaum Associates, Mahwah, NJ, 1988).
T.B. Huedo-Medina, J. Sánchez-Meca, F. Marín-Martínez, J. Botella, Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol Methods 11, 193–206 (2006)
L. Guirant, F. Carlos, D. Curiel, J.A. Kanis, F. Borgström et al. Health-related quality of life during the first year after a hip fracture: results of the Mexican arm of the International Cost and Utility Related to Osteoporotic Fractures Study (MexICUROS). Osteoporosis Int 29, 1147–1154 (2018)
N. González, U. Aguirre, M. Orive, J. Zabala, S. García-Gutiérrez et al. Health-related quality of life and functionality in elderly men and women before and after a fall-related wrist fracture. Int J Clin Pract 68, 919–928 (2014)
M. Orive, U. Aguirre, S. García-Gutiérrez, C. Las Hayas, A. Bilbao et al. Changes in health-related quality of life and activities of daily living after hip fracture because of a fall in elderly patients: a prospective cohort study. Int J Clin Pract 69, 491–500 (2015)
Y. Çalik, A.F. Çalik, The effect of bone mineral density on quality of life in men with osteoporosis. Turk Osteoporoz Derg 21, 10–14 (2015)
L. Xu, W. Sun, X. Qin, X. Zhu, Y. Qiu et al. The reliability and validity of the simplified Chinese version of Male QUALEFFO-26. Rheumatol Int 36, 489–494 (2016)
S.L. Solimeo, S.L. Silverman, A.D. Calderon, A. Nguyen, D.T. Gold, Measuring health-related quality of life (HRQOL) in osteoporotic males using the Male OPAQ. Osteoporos Int 23, 841–852 (2012)
I. Pande, D.L. Scott, T.W. O’Neill, C. Pritchard, A.D. Woolf et al. Quality of life, morbidity, and mortality after low trauma hip fracture in men. Ann Rheum Dis 65, 87–92 (2006)
M. Ichinohe, K. Wada, G. Kumagai, S. Tanaka, T. Asari et al. Prevalence and associated factors of radiographic vertebral fractures in men: rural population cross-sectional observation study in Japan. J Orthop Sci, S0949-2658, (0920):30207–30204. (2020)
S. Waterloo, A.J. Søgaard, L.A. Ahmed, E. Damsgård, B. Morseth et al. Vertebral fractures and self-perceived health in elderly women and men in a population-based cross-sectional study: the Tromsø Study 2007–08. BMC Geriatr 13, 102 (2013)
K. Voigt, S. Taché, M. Hofer, C. Straßberger, H. Riemenschneider et al. Health related quality of life in male patients with osteoporosis: results of a cross sectional study. Aging Male 15, 220–226 (2012)
J.A. Pasco, M.J. Henry, S. Korn, G.C. Nicholson, M.A. Kotowicz, Morphometric vertebral fractures of the lower thoracic and lumbar spine, physical function and quality of life in men. Osteoporos Int 20, 787–792 (2009)
S. Muraki, T. Akune, H. Oka, Y. En-Yo, M. Yoshida et al. Health-related quality of life with vertebral fracture, lumbar spondylosis and knee osteoarthritis in Japanese men: the ROAD study. Arch Osteoporos 5, 91–99 (2010)
K. Siggeirsdottir, T. Aspelund, B.Y. Jonsson, B. Mogensen, L.J. Launer et al. Effect of vertebral fractures on function, quality of life and hospitalisation the AGES-Reykjavik study. Age Ageing 41, 351–357 (2012)
E.M. Dennison, H.E. Syddall, C. Statham, A. Aihie Sayer, C. Cooper, Relationships between SF-36 health profile and bone mineral density: the Hertfordshire Cohort Study. Osteoporos Int 17, 1435–1442 (2006)
B.C. Lentle, J.P. Brown, A. Khan, W.D. Leslie, J. Levesque et al. Recognizing and reporting vertebral fractures: reducing the risk of future osteoporotic fractures. Can Assoc Radiol J 58, 27–36 (2007)
L. Ferrar, G. Jiang, J. Adams, R. Eastell, Identification of vertebral fractures: an update. Osteoporos Int 16, 717–728 (2005)
H.K. Genant, C.Y. Wu, C. van Kuijk, M.C. Nevitt, Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8, 1137–1148 (1993)
L. Li, H.M. Wang, Y. Shen, Chinese SF-36 Health Survey: translation, cultural adaptation, validation, and normalisation. J Epidemiol Community Health 57, 259–263 (2003)
C. Doria, G.R. Mosele, F. Solla, G. Maestretti, M. Balsano et al. Treatment of osteoporosis secondary to hypogonadism in prostate cancer patients: a prospective randomized multicenter international study with denosumab vs. alendronate. Minerva Urol Nefrol 69, 271–277 (2017)
K.M. Nicks, S. Amin, E.J. Atkinson, B.L. Riggs, L.J. Melton 3rd et al. Relationship of age to bone microstructure independent of areal bone mineral density. J Bone Miner Res 27, 637–644 (2012)
D. Sundh, D. Mellström, M. Nilsson, M. Karlsson, C. Ohlsson et al. Increased cortical porosity in older men with fracture. J Bone Miner Res 30, 1692–1700 (2015)
E.J. Samelson, K.E. Broe, H. Xu, L. Yang, S. Boyd et al. Cortical and trabecular bone microarchitecture as an independent predictor of incident fracture risk in older women and men in the Bone Microarchitecture International Consortium (BoMIC): a prospective study. Lancet Diabetes Endocrinol 7, 34–43 (2019)
M.R. Laurent, L. Dedeyne, J. Dupont, B. Mellaerts, M. Dejaeger et al. Age-related bone loss and sarcopenia in men. Maturitas. 122, 51–56 (2019)
T. Porcelli, F. Maffezzoni, L.C. Pezzaioli, A. Delbarba, C. Cappelli et al. MANAGEMENT OF ENDOCRINE DISEASE: male osteoporosis: diagnosis and management—should the treatment and the target be the same as for female osteoporosis? Eur J Endocrinol 183, R75–r93 (2020)
R. Patel, A. Bhimjiyani, Y. Ben-Shlomo, C.L. Gregson, Social deprivation predicts adverse health outcomes after hospital admission with hip fracture in England. Osteoporos Int 32, 1129–1141 (2021)
S. Williamson, F. Landeiro, T. McConnell, L. Fulford-Smith, M.K. Javaid et al. Costs of fragility hip fractures globally: a systematic review and meta-regression analysis. Osteoporos Int 28, 2791–2800 (2017)
J.T. Schousboe, M.L. Paudel, B.C. Taylor, A.M. Kats, B.A. Virnig et al. Pre-fracture individual characteristics associated with high total health care costs after hip fracture. Osteoporos Int 28, 889–899 (2017)
P.M. Cawthon, T.L. Blackwell, L.M. Marshall, H.A. Fink, D.M. Kado et al. Physical performance and radiographic and clinical vertebral fractures in older men. J Bone Miner Res 29, 2101–2108 (2014)
A. El Maghraoui, A. Mounach, A. Rezqi, L. Achemlal, A. Bezza et al. Vertebral fracture assessment in asymptomatic men and its impact on management. Bone 50, 853–857 (2012)
S.R. Cummings, P.M. Cawthon, K.E. Ensrud, J.A. Cauley, H.A. Fink et al. BMD and risk of hip and nonvertebral fractures in older men: a prospective study and comparison with older women. J Bone Miner Res 21, 1550–1556 (2006)
S. Wilson, C.A. Sharp, M.W. Davie, Health-related quality of life in patients with osteoporosis in the absence of vertebral fracture: a systematic review. Osteoporos Int 23, 2749–2768 (2012)
J.E. Tarride, N. Burke, W.D. Leslie, S.N. Morin, J.D. Adachi et al. Loss of health related quality of life following low-trauma fractures in the elderly. BMC Geriatr 16, 84 (2016)
X.L. Griffin, N. Parsons, J. Achten, M. Fernandez, M.L. Costa, Recovery of health-related quality of life in a United Kingdom hip fracture population. The Warwick Hip Trauma Evaluation—a prospective cohort study. Bone Jt J 97-b, 372–382 (2015)
Funding
This work is supported by National Key R&D Program of China (2018YFA0800801), National Natural Science Foundation of China (Nos. 81873668, 82070908), and Beijing Natural Science Foundation (7202153).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Hu, J., Zheng, W., Zhao, D. et al. Health-related quality of life in men with osteoporosis: a systematic review and meta-analysis. Endocrine 74, 270–280 (2021). https://doi.org/10.1007/s12020-021-02792-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-021-02792-0