Abstract
Curcumin is assumed to be a plant-derived therapeutic drug that triggers apoptotic cell death in vitro and in vivo by affecting different molecular targets such as NF-κB. Phase I/II trial of curcumin alone or with chemotherapeutic drugs has been accomplished in pancreatic, colon, prostate and breast cancer cases. Recently, autocrine growth hormone (GH) signaling-induced cell growth, metastasis and drug resistance have been demonstrated in breast cancer. In this study, our aim was to investigate the potential therapeutic effect of curcumin by evaluating the molecular machinery of curcumin-triggered apoptotic cell death via focusing on NF-κB signaling and polyamine (PA) metabolism in autocrine GH-expressing MCF-7, MDA-MB-453 and MDA-MB-231 breast cancer cells. For this purpose, a pcDNA3.1 (+) vector with a GH gene insert was transfected by a liposomal agent in all breast cancer cells and then selection was conducted in neomycin (G418) included media. Autocrine GH-induced curcumin resistance was overcome in a dose-dependent manner and curcumin inhibited cell proliferation, invasion–metastasis and phosphorylation of p65 (Ser536), and thereby partly prevented its DNA binding activity in breast cancer cells. Moreover, curcumin induced caspase-mediated apoptotic cell death by activating the PA catabolic enzyme expressions, which led to generation of toxic by-products such as H2O2 in MCF-7, MDA-MB-453 and MDA-MB-231 GH+ breast cancer cells. In addition, transient silencing of SSAT prevented curcumin-induced cell viability loss and apoptotic cell death in each breast cancer cells. In conclusion, curcumin could overcome the GH-mediated resistant phenotype via modulating cell survival, death-related signaling routes and activating PA catabolic pathway.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is one of the leading types of cancer among women and the fifth most common cause of cancer death worldwide (Siegel et al. 2012). The molecular mechanism of breast cancer is controlled by various growth factors, including hormones such as HER2/Neu, estrogen and prolactin (Sternlicht 2006). Recently, besides prolactin, growth hormone (GH) has also been shown to be related to mammary gland development and takes a major role in ductal epithelial differentiation during puberty (Sternlicht 2006). Positive expression levels of both GH and its receptor (GHR) were determined in breast cancer samples (Wu et al. 2011). Although active GH signaling affects muscle and bone development through insulin-like growth factor-I (IGF-I), active autocrine GH signaling was demonstrated in mammary carcinoma (Kaulsay et al. 2001). GH expression was remarkable in aggressive breast cancer cases compared to healthy breast tissues (Mol et al. 1995) and these findings were supported by the high occurrence of breast cancer cases among acromegaly patients, who have excess serum GH levels after puberty (Raccurt et al. 2002).
A number of studies have shown that the signaling of autocrine GH led to epithelial to mesenchymal transition (EMT) and triggered a metastatic profile by increasing occludin and fibronectin expression levels in MCF-7 breast cancer cells (Mukhina et al. 2004). Similar to this finding, forced GH expression-mediated tumorigenesis and metastasis was reported in estrogen receptor (ER)-negative MDA-MB-453 and SK-BR-3 breast cancer cells (Chen et al. 2015). In addition, autocrine GH signaling-triggered oncogenic transformation as a result of increased expression of c-myc, cyclin-D1 and Bcl-2 in MCF-10 breast epithelial cells was reported (Zhu et al. 2005a). A high expression rate of GH-mediated chemoresistance against various drugs such as doxorubicin, mitomycin C and tamoxifen has been determined in breast cancer cells (Bougen et al. 2011; Minoia et al. 2012; Mojarrad et al. 2010; Zatelli et al. 2009). However, GH might also produce a sensitive phenotype against arsenic trioxide, a Chinese patented-drug in MCF-7 breast cancer cells (Zekri et al. 2013). Clinically approved chemotherapeutic drugs, commonly used in the treatment of metastatic breast cancer cases, may promote the chemoresistance phenotype. For this reason, new drug candidates are needed for the treatment of metastatic breast cancer cases.
One of the promising functional food derivative is curcumin isolated from Curcuma longa, which has been shown to be an anti-inflammatory, and antioxidant, and has an anti-tumorigenic effect on colon, cervical, prostate and breast cancer cells (Chauhan 2002; Duvoix et al. 2005; Guo et al. 2013; Liao et al. 2008). A number of reports have shown that curcumin possesses an anti-carcinogenic effect that suppresses cell proliferation, invasion and metastasis. In addition, curcumin-induced caspase-dependent apoptotic cell death by modulating different molecular targets including nuclear factor kappa B (NF-κB), signal transducer and activator of transcription (STAT), cyclin-D and matrix metalloproteinase-1 (MMP-1) was demonstrated (Liu et al. 2009). Supporting these observations, it was reported that curcumin triggered reactive oxygen species (ROS) generation through downregulation of ornithine decarboxylase (ODC) gene expression in HL-60 leukemia cells (Liao et al. 2008).
The natural PAs, putrescine (Put), spermidine (Spd) and spermine (Spm), are amine-derived organic cations, which have essential roles in cell proliferation, growth, differentiation and cancer progression (Cohen 1978; Igarashi and Kashiwagi 2000). Since high intracellular PA levels are associated with cancer development and progression, PA catabolic pathway-targeting chemotherapeutics have gained importance as new anticancer therapy models (Pegg 1988). Curcumin induced apoptotic cell death by depletion of intracellular PA level, downregulation of ODC gene expression and also upregulation of PA catabolic enzyme (SSAT and PAO) gene expressions in MCF-7 wt and Bcl-2+ breast cancer cells (Berrak et al. 2016). Although curcumin has been evaluated as a powerful apoptotic agent in pre-clinical cancer studies, phase I/II trials on curcumin are contradictory because of the stability problems of curcumin in human studies. However, combinational therapy of curcumin with chemotherapeutic drugs (docetaxel, gemcitabine) increased the potential therapeutic effect of curcumin due to its inhibitory effect on carcinogenic molecules, especially NF-κB (Bayet-Robert et al. 2010; Kanai et al. 2011). Therefore, to evaluate the therapeutic efficiency of curcumin in clinical trials, previous in vitro studies should be conducted to demonstrate the molecular targets in curcumin-mediated apoptotic cell death in breast cancer cells, especially with high metastatic profile. In this study, our aim was to investigate the potential molecular targets of curcumin-triggered apoptotic cell death in GH-mediated aggressive breast cancer cells regarding the NF-κB and EMT pathway and also to demonstrate the role of PA metabolism as a final consequence of curcumin-mediated apoptotic cell death.
Materials and methods
Drugs, chemical and antibodies
Curcumin was purchased from Sigma (St. Louis, MO, USA) and dissolved in DMSO to prepare a 10 mM stock solution of which aliquots were kept at − 20 °C. N-Acetylcysteine (NAC) and wedelolactone were purchased from Sigma (St. Louis, MO, USA). Rabbit anti-GH, anti-Src, anti-STAT5, anti-pSTAT5, anti-STAT1, anti-pSTAT1, anti-STAT3, anti-pSTAT3, anti-SOCS-1, anti-SOCS-2, anti-PIAS-3, anti-PI3K, anti-Akt, anti-pAkt, anti-pFOXO3a, anti-p38, anti-pp38, anti-p44/42, anti-pp44/42, anti-Ras, anti-c-Raf, anti-c-fos, anti-c-jun, anti-c-myc, anti-N-cadherin, anti-snail, anti-vimentin, anti-β-catenin, anti-IKK-α, anti-IKK-β, anti-IκBα, anti-pIκB α, anti-NF-κB, anti-pNF-κB, anti-NIK, anti-TRAF2, anti-TRAF3, anti-RelB, anti-Histon-3, anti-p53, anti-p21, anti-Rb, anti-pRb, anti-Fas, anti-FADD, anti-TRADD, anti-pro-caspase-2, anti-pro-caspase-8, anti-Bax, anti-Bak, anti-Bad, anti-Puma, anti-Bcl-2, anti-Bcl-xL, anti-Mcl-1, anti-PARP, anti-β-actin, anti-pro-caspase-9 and anti-pro-caspase-7 antibodies (each 1:1000 dilution) were purchased from Cell Signaling Technology (CST, Danvers, MA, USA), whereas rabbit anti-JAK-2, anti-pJAK-2, anti-SSAT and anti-PAO antibodies (each 1:1000 dilution) were purchased from Santa Cruz (Santa Cruz, CA, USA). Mouse anti-MMP-2, anti-MMP-9, anti-TIMP-1 and anti-TIMP-2 antibodies were purchased from CalBioChem (San Diego, CA, United States). ODC, AZ and AZI primary antibodies (each 1:1000 dilution) were gifted by Prof. Chaim Kahana from Weizmann Institute of Science, Israel. HRP-conjugated secondary anti-rabbit and anti-mouse antibodies (1:5000) were purchased from CST (Danvers, MA, USA).
pcDNA3.1-GH plasmid generation
Total DNA was isolated from venous blood by the salting out method (Miller et al. 1988). Genomic GH gene was amplified by PCR according to the 5′-TCTAAGCTTAGGATCCCAAGGCCCAACTC-3′ and 5′-AAGAATTCCTAGAAGCCACAGCTGCCCTCCAC-3′ primers (IDT, Iowa, USA). The PCR protocol included an initial denaturation step at 94 °C for 3 min, followed by 30 cycles with 30 s of denaturation at 94 °C, 30 s of annealing at 65 °C and 45 s of elongation at 72 °C, followed by a final elongation step at 72 °C for 10 min. PCR results were electrophoresed at 1% agarose gel and visualized by gel detection system (Bio-Rad, California, USA). Both GH PCR product and pcDNA3.1 (+) (Invitrogen, Waltham, MA, USA) plasmid were double digested by EcoRI and HindIII restriction enzymes (Thermo Scientific, Waltham, MA, USA). Digestion products were purified from agarose gel electrophoresis using Gel extraction kit (Qiagene, Valencia, CA, USA) and ligated by T4 ligase (Thermo Scientific, Waltham, MA, USA). The GH gene-inserted pcDNA3.1 (+) plasmids were transformed to E. coli HB101 competent cells and selected by ampicillin. Positive clones were determined by both colony PCR and DNA sequencing.
Cell lines and culture conditions
MCF-7 (ATCC-HTB-22), MDA-MB-453 (ATCC-HTB-131) and MDA-MB-231 (ATCC-HTB-26) breast cancer cells were purchased from the American Type Culture Collection (ATCC, Manassas, USA). Stable GH-expressing MCF-7, MDA-MB-453 and MDA-MB-231 breast cancer cells were generated by transfection of GH-inserted pcDNA3.1 (+) plasmid by Lipofectamine 2000 (Thermo Fisher Scientific, Waltham, MA, USA). Following transfection, neomycin selection was performed and the highest GH-expressing positive clone was selected by immunoblotting and GH ELISA results. The selected GH-expressing clones for MCF-7, MDA-MB-453 and MDA-MB-231 breast cancer cells were used in all experiments in this study. MCF-7, MDA-MB-453 and MDA-MB-231 wild-type (wt) and GH+ breast cancer cells were maintained in DMEM medium (PAN Biotech, Aidenbach, Germany) supplemented with 2 mM l-glutamine, 10% fetal calf serum (PAN Biotech, Aidenbach, Germany), 1% non-essential amino acids (Biological Industries, Kibbutz Beit-Haemek, Israel) and 100 U/100 mg/ml penicillin/streptomycin (Biological Industries, Kibbutz Beit-Haemek, Israel) in the presence of 5% CO2 in a humidified atmosphere at 37 °C.
Determination of GH expression by GH ELISA
1 × 106 MCF-7, MDA-MB-453 and MDA-MB-231 wt and GH+ breast cancer cells were incubated 24 h without FBS serum, the cell-free media were filtered by Amicon Ultra-15 Centrifugal Filter (Millipore Darmstadt, Germany) and the concentration of the secreted GH was determined by GH ELISA Assay (Abcam, Cambridge, MA, USA) according to manufacturer’s instructions.
MTT cell viability assay
The dose-dependent effect of curcumin alone and/or siRNA transfection (SSAT siRNA) on cell viability was determined using a colorimetric 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl-tetrazolium bromide (MTT) assay (Roche, Indianapolis, IN, USA) in each wt and GH + breast cancer cells. Cells were seeded at a density of 4 × 103 cells per well in a 96-well plate. 20 pmol SSAT siRNA (Santa Cruz Biotechnology, CA, USA) transfection was performed for 48 h and following transfection selected doses of curcumin were applied to cells for 24 h.
Trypan blue dye exclusion assay
Each cell line was seeded at a density of 5 × 104 cells/well in a six-well plate and treated with selected curcumin concentration for 72 h. Every 24 h, cells were trypsinized and stained with trypan blue; viable and death cells were counted under light microscopy. The obtained data were placed on a graph for the number of cells (y-axis) and time (x-axis).
Soft agar assay
The base agar was prepared creating a mixture with equal amounts of 2× DMEM medium (20% FBS and 2% penicillin/streptomycin) and 0.5% agarose in PBS and the mixture was dispersed 1 ml into each well in six-well plates. After solidification of gel, 2.5 × 105 cells/ml in a 1:1 mix of 2× DMEM medium and 0.3% agarose were added on top of the base gel. After solidification, 500 µl media in the presence or absence of drugs was added on the gel and incubated at 37 °C for 15 days and cells were stained with 0.05% crystal violet for 30 min.
In vitro cell migration and invasion assays
Assays were performed in BioCoat Matrigel invasion chambers (BD Biosciences, Bedford, MA, USA) according to the manufacturer’s instructions, with uncoated porous filters (8 μm pore size) for estimation of cell migration and filters pre-coated with Matrigel to examine cell invasion. Cells were serum deprived for 24 h before the experiment. Values for cell migration or invasion were denoted as the average number of cells per microscopic field over four fields per one filter for triplicate experiments, as described previously (Hazan et al. 2000).
siRNA-mediated SSAT silencing
Each breast cancer cell was seeded at a density of 4 × 105 in 60 mm Petri dishes and allowed to adhere overnight at 37 °C. Next, 80 pmol SSAT siRNA (Santa Cruz Biotechnology, CA, USA) in 1:3 siRNA transfection reagent (Santa Cruz Biotechnology, CA, USA) was prepared in 200 μl serum-free culture medium and incubated for 30 min at room temperature. The mixture was gently added dropwise to the cells in 800 μl culture medium with 10% FBS and incubated for 0–48 h at 37 °C in a CO2 incubator. Following transient silencing for 48 h, the cells were treated with determined doses of curcumin for 24 h after which total proteins were extracted.
RNA isolation, cDNA synthesis, RT-PCR and qRT-PCR
Total RNA was isolated from each cell line using TRIPure (Roche, Indianapolis, IN, USA) according to the manufacturer’s indications. First-strand cDNA was transcribed using iScript cDNA Synthesis Kit (Bio-Rad, Hercules, CA, USA). MMP-2, MMP-9, TIMP-1 and 18S genes were amplified using synthesized cDNAs by RT-PCR, electrophoresed at 2% agarose gel and visualized by Gel Detection System (Bio-Rad, Hercules, CA, USA). Following 24 h of selected doses of curcumin treatment in each breast cancer cells, total RNA was isolated by using TRIPure (Roche, Indianapolis, IN, USA) according to the manufacturer’s indications. First-strand cDNA was transcribed by using iScript cDNA Synthesis Kit (Bio-Rad, Hercules, CA, USA). ODC, PAO and SSAT primers (Santa Cruz Biotechnology, CA, USA) were used to amplify the ODC, PAO and SSAT gene expression profile by using Bio-Rad CFX Connect (Bio-Rad, Hercules, CA, USA). The mean of the Ct levels was analyzed using the 2ΔΔCt method and the 18S primer was used as a reference gene.
Protein extraction and immunoblotting
Total proteins were isolated from each sample, which was treated with the appropriate concentrations of curcumin for 24 h by using ProteoJET Mammalian cell lysis buffer (Fermentas, St. Leon-Rot, Germany). Following curcumin treatment, nuclear and cytoplasmic proteins were isolated from MCF-7, MDA-MB-453 and MDA-MB-231 GH+ breast cancer cells using NE-PER Nuclear and Cytoplasmic Extraction Reagent kit and following the detailed instructions provided (Pierce Biotechnology, Rockford, IL, USA). Protein concentrations were determined using a Bradford protein assay (Bio-Rad, Hercules, CA, USA) and total protein lysates (50 μg) were separated by 12% SDS-PAGE and transferred to PVDF membranes (Roche, Indianapolis, USA). After this, the membranes were blocked with 5% milk blocking solution in Tris-buffered saline (TBS)–Tween 20 (Sigma Ultra, St. Louis, MO, USA) and incubated with the appropriate primary and horseradish peroxidase (HRP)-conjugated secondary antibodies (CST, Danvers, MA, USA) in antibody buffer containing 5% (v/v) milk blocking solution. Following a gentle washing step with 1× TBS–Tween20, protein bands were analyzed using an enhanced chemiluminescence reagent (ECL, PierceTM, Thermo Scientific, Waltham, MA, USA) and signals from the HRP-conjugated antibodies were detected using ChemiDoc MP Imaging System (Bio-Rad, Hercules, CA, USA). All results were replicated at least two times and representative blots given.
Electrophoretic mobility shift assay (EMSA) for NF-κB
The 3′- end biotin-labeled probe containing the NF-κB anti-sense: 5′-AGTTGAGGGGACTTTCCCAGGC-3′, wt sense 5′-GCCTGGGAAAGTCCCCTCAACT-3′ STAT5 anti-sense: 5′-AGATTTCTAGGAATTCAATCC-3′ and wt sense: 5′-GGATTGAATTCCTAGAAATCT-3′ was purchased from Integrated DNA Technologies (IDT, Iowa, USA). The biotinylated oligonucleotides were annealed via denaturing at 90 C for 1 min, followed by cooling to room temperature for 1 h. The EMSA binding reactions were performed by using LightShift Chemiluminescent EMSA Kit (Pierce, Biotechnology, Rockford, IL, USA) according to the manufacturer’s instructions. 3 µg nuclear protein extracts was incubated in 1× binding buffer containing 2.5% glycerol, 0.05% NP-40, 50 mM KCl, 5 mM MgCl2, 50 ng Poly (dI-dC) and biotinylated probe with or without protein extracts for 30 min at room temperature. The complex was separated on a 6% polyacrylamide–0.5 × Tris–borate–EDTA gel and transferred to positively charged nylon membrane. Following the transfer procedure, the membrane was cross-linked and then biotin-labeled DNA was detected using ChemiDoc MP Imaging System (Bio-Rad Laboratories, Hercules, CA, USA).
FACS flow analysis
DCFH-DA staining
Each cell line was seeded at a density of 1.25 × 105 cells/well in a six-well plate. Next, 80 pmol SSAT siRNA (Santa Cruz Biotechnology, CA, USA) in 1:3 siRNA transfection reagent (Santa Cruz Biotechnology, CA, USA) was prepared in 100 μl serum-free culture medium and incubated for 30 min at room temperature. The mixture was gently added dropwise to the cells in 900 μl culture medium with 10% FBS and incubated for 0–48 h at 37 °C in a CO2 incubator. Following transient silencing, the cells were treated with determined doses of curcumin for 24 h and harvested by trypsinization. The pellets were re-suspended in 1 × PBS with 1 µM of DCFH-DA and the cells were incubated in a cell incubator [(37°C), high relative humidity (95%) and controlled CO2 level (5%)] in the dark for 45 min. 5000 events were analyzed in FACS flow cytometry [Accuri C6 Flow Cytometer (BD Biosciences, Bedford, MA, USA)]. Fluorescence intensity of DCF staining was analyzed on FL-1 (525 nm).
Annexin V/PI double staining
Cells were seeded at a density of 3 × 105 cells/well in a six-well plate and treated with selected dose of curcumin for 24 h following with/without siRNA transfection (SSAT siRNA; 80 pmol each) for 48 h. Both floating and adherent cells were collected; after centrifugation, the cell pellets were re-suspended in 1 × PBS, RNase (100 µg/ml) and Annexin V (10 µg/ml), incubated for 10 min, followed by the addition of PI (40 µg/ml), kept in the dark for 5 min and analyzed using an Accuri C6 (BD Biosciences, Bedford, MA, USA) Flow Cytometer. Fluorescence emissions were collected through 530 and 570-nm band-pass filters for FITC and PI, respectively. Data were evaluated using BD Accuri C6 software and presented as dot plots (Annexin fluorescence on the x-axis; PI fluorescence on the y-axis).
Cell cycle analysis by PI staining
Each cell line was seeded at a density of 2 × 105 cells/well in a six-well plate and then treated with an appropriate curcumin dose for 24 h. Both floating and adherent cells were collected and fixed with 70% ethanol. Following incubation on ice for 30 min, the samples were centrifuged at 1200 rpm for 5 min, after which the pellets were re-suspended in 1 × PBS containing RNase (100 μg/ml) and PI solution (40 μg/ml). The resulting samples were kept for 30 min at 37 °C in the dark and analyzed using Accuri C6 (BD Biosciences, Bedford, MA, USA) equipped with a 15 mW, 488-nm air-cooled argon ion laser. Fluorescence emission was collected through a 570 nm band-pass filter. Cell cycle distribution analyses were performed using the C6 software (BD Biosciences, Bedford, MA, USA).
PA analysis by HPLC
Intracellular PA levels were determined by HPLC analysis following a benzoylation procedure (Berrak et al. 2016). MCF-7, MDA-MB-231 and MDA-MB-453 wt and GH+ breast cells were seeded at a density of 1.2 × 106 in 100 mm Petri dishes and allowed to adhere overnight. Next, the cells were treated with curcumin for 24 h. Following washing in 1 × PBS the cells were collected by scraping and transferred to a new microfuge tube, after which 50% trichloroacetic acid was added to each sample (1:10, v/v). The samples were kept at − 20 °C until benzoylation. Following benzoylation, the samples were immediately run on an HPLC system (Agilent, Santa Clara, CA, USA) using a UV detector set at 226 mV. The results obtained were evaluated against the internal standard 1,7-diaminoheptane, and Put, Spd and Spm standard curves (each 10 mM stock concentration).
Statistical analysis
All the experiments were analyzed statistically by two-way ANOVA using GraphPad Prism 6 (GraphPad Software, La Jolla, CA, USA). Statistically significant results by ANOVA were further analyzed by Bonferroni post hoc analysis (where indicated). p values considered as statistically significant were **p < 0.05, **p < 0.01 and ***p < 0.001, respectively. Error bars in the graphs were generated using ± standard deviation (SD) values. The mean ± SD of the data representing ELISA assay, MTT cell viability, growth assay and qRT-PCR analysis were achieved from at least three experiments with four replicates. All the immunoblotting results were repeated at least twice and Image J was applied to calculate the band intensities.
Results
Curcumin decreased cell viability in a dose- and time-dependent manner
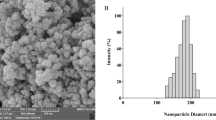
To determine the dose-dependent effect of curcumin on GH-expressing MCF-7, MDA-MB-453 and MDA-MB-231 breast cancer cells, we generated stable cell lines expressing GH by pcDNA3.1 (+) vector with the GH gene inserted. Selected clones, which were secreting and expressing GH, were analyzed using GH ELISA assay and the immunoblotting method, respectively. According to the ELISA assay results, selected clones from each cell line, which exerted a higher expression profile of GH when compared to wt cells, also had positive results for GH secretion in all breast cancer cells (Fig. 1a). Increasing concentrations (0–30 µM) of curcumin caused the downregulation of GH expression in all the breast cancer cell lines. For further experiments, we selected an effective anti-hormonal concentration of curcumin 20 µM for GH+ MCF-7 and MDA-MB-453 cells and 25 µM for MDA-MB-231 cells (Fig. 1b). Although autocrine GH expression caused resistant phenotype against curcumin-induced cell viability loss compared to parental cells, dose-dependent curcumin treatment overcame this effect in GH+ breast cancer cells. According to the MTT cell viability assay, exposure of 20 µM curcumin decreased cell viability by 49% in MCF-7 wt and 48% in MDA-MB-453 wt breast cancer cells for 24 h. However, curcumin decreased cell viability loss by 74% in MCF-7 GH+ and 60% in MDA-MB-453 GH + cells for 24 h (Fig. 2a). Similarly, 25 µM curcumin induced 47 and 24% cell viability loss in MDA-MB-231 wt and GH+ breast cancer cells, respectively (Fig. 2a). Although GH overexpression induced cell growth in each cell line as compared to parental breast cancer cells, 20 µM (MCF-7, and MDA-MB-453) or 25 µM (MDA-MB-231) curcumin suppressed growth inhibition in a time-dependent manner (Fig. 2b).
Curcumin suppressed the autocrine GH expression in MCF-7, MDA-MB-453 and MDA-MB-231 breast cancer cells. a The extracellular expression of GH in each breast cancer after GH-inserted pcDNA3.1 (+) vector transfection and neomycin selection was determined by GH ELISA and immunoblotting in MCF-7 (left), MDA-MB-453 (middle) and MDA-MB-231 (right) breast cancer cells. b Dose-dependent curcumin effect on GH expression was determined by immunoblotting in MCF-7 GH+, MDA-MB-453 and MDA-MB-231 GH+ breast cancer cells. P pellet, M medium. β-actin was used as a loading control
The cytotoxic effect of curcumin in autocrine GH-expressing MCF-7, MDA-MB-453 and MDA-MB-231 breast cancer cells. a The effect of curcumin on cell viability was determined by MTT cell viability assay after curcumin (0–100 μM) treatments for 24 h in MCF-7 (left), MDA-MB-453 (middle) and MDA-MB-231 (right) wt and GH + breast cancer cells. b The effect of curcumin on cell growth inhibition effect was determined in MCF-7 (left), MDA-MB-453 (middle) and MDA-MB-231 (right) wt and GH+ cells by trypan blue growth assay. The data shown represent the mean ± S.D. from three experiments with four replicates. Statistical difference was analyzed using a two-way ANOVA; **p < 0.05, * p < 0.01, ***p < 0.001
GH-induced JAK/STAT and PI3K/Akt/MAPK activation prevented by curcumin treatment
The major effect of forced GH expression was upregulation of STAT-1, STAT-3 and pSTAT-3 protein expressions in GH+ MCF-7, MDA-MB-453 and MDA-MB-231 breast cancer cells. Autocrine GH-mediated JAK2, STAT-5 phosphorylation and STAT-5 gene upregulation were observed in MCF-7 and MDA-MB-231 breast cancer cells. In addition, increased phosphorylation status of STAT-1 was determined in MDA-MB-231 and MDA-MB-453 breast cancer cell during biologically active GH signaling. When the cells were exposed to the selected curcumin concentration, we found that the expression levels of STAT-5, STAT-1 and STAT-3 protein expressions were diminished, and curcumin triggered downregulation of pSTAT-1 (Tyr701), pSTAT-3 (Ser727) and pSTAT-5 (Tyr694) protein levels in each GH+ breast cancer cell. Downregulation of JAK-2 and pJAK-2 protein expressions were observed in both MCF-7 and MDA-MB-231 GH+ cells following curcumin treatment. Although curcumin treatment upregulated PIAS-3 expression in MCF-7 and MDA-MB-453 breast cancer cells, downregulation in SOCS-1 and SOCS-3 expression levels was observed in MCF-7 and MDA-MB-453 GH+ breast cancer cells (Fig. 3a). To determine the STAT-5 activation in GH + breast cells, and the potential effect of curcumin on STAT-5 activity, we performed EMSA assay (Fig. 3b). According to the EMSA assay, nuclear translocation of GH-induced STAT-5 prevented by curcumin treatment was established. Forced GH expression triggered Ras, c-raf, c-fos, c-jun and c-myc expression and altered the phosphorylation of Akt, p44/42 in breast cancer cells. While curcumin treatment led to downregulation of Ras and c-raf in all GH+ breast cancer cells, GH-mediated c-fos, c-jun and c-myc protein expressions were suppressed by curcumin treatment especially in MDA-MB-453 breast cancer cells (Fig. 3c).
Autocrine GH induced JAK/STAT and PI3K/Akt/MAPK signaling suppressed by curcumin treatment in breast cancer cells. a The effect of autocrine GH expression and curcumin treatment on JAK-2, pJAK-2 (Tyr1007/1008), Src, STAT5, pSTAT5 (Tyr694), STAT1, pSTAT1 (Tyr701), STAT3, pSTAT3 (Ser727), SOCS-1, SOCS-3 and PIAS-3 protein expression profiles was determined by immunoblotting in MCF-7 (left), MDA-MB-453 (Middle), MD-MB-231 (right) wt and GH+ breast cancer cells. Autocrine GH expression-induced STAT-5 activation and potential effect of curcumin on STAT-5 activity was determined by EMSA assay in b MCF-7 (left), MDA-MB-453 (Middle), MDA-MB-231 (right) wt and GH+ breast cancer cells. c PI3K, Akt, pAkt (Ser473), pFOXO (Ser318/321), p38, pp38 (Thr180/Ty182), p44/42, pp44/42 (Thr202/Tyr204), Ras, c-raf, c-fos, c-jun and c-myc expression alteration due to GH overexpression and the curcumin effect was determined by immunobloting. β-actin was used as a loading control
Curcumin prevented active GH signaling-mediated invasion and metastasis
Although autocrine GH signaling increased colony formation as compared to wt cells, exposure of cells to curcumin was effective to decrease colony formation in all cell lines regardless of the GH expression profile (Fig. 4a). Concomitantly, the increased colony formation due to active GH signaling triggered metastatic and invasive cell phenotype. Similar to previous results, curcumin acted as a negative modulator on metastasis and invasion. In all breast cancer cells, although GH expression caused an increase in the invasive and metastatic cell populations compared to wt cells, curcumin prevented the GH-mediated aggressive cell phenotype (Fig. 4b). Although forced GH expression elevated mRNA levels of MMP-2 and TIMP-1 in each breast cancer cell, curcumin treatment suppressed MMP-2 expression levels in MCF-7 and TIMP-1 expression levels in MDA-MB-453 GH+ breast cancer cells (Fig. 4c). While a distinct increase was observed for MMP-9 and TIMP-2 protein expressions in GH+ breast cancer cells as compared to wt cells, curcumin treatment effectively prevented this effect only in MDA-MB-453 cells. Moreover, forced GH expression induced vimentin, snail and ß-catenin protein expression as compared to wt cells. However, curcumin treatment decreased vimentin and snail, and ß-catenin expressions in each cell line (Fig. 4d).
Forced GH expression-induced colony formation and invasion–metastasis prevented by curcumin treatment via acting on EMT marker expression profiles in breast cancer cells. a Curcumin treatment prevents the autocrine GH-induced colony formation in MCF-7 (left), MDA-MB-453 (middle) and MDA-MB-231 (right) breast cancer cells. The effect of curcumin on the diameter of colonies was calculated and given as a bar graph. b 0.5 × 104 MCF-7 (left), MDA-MB-453 (middle) and MDA-MB-231 (right) wt and GH+ breast cancer cells with or without curcumin seeded on invasion plate with pore size 8 µm, and following 24 h curcumin treatment, invasive cell number (Upper chamber) and metastatic cell number (lower chamber) were counted and given as a bar graph. The data shown represent the mean ± S.D. from three experiments with four replicates. Statistical difference was analyzed using a two-way ANOVA; **p < 0.05, **p < 0.01, ***p < 0.001. c The transcriptional expression profiles of MMP-2, MMP-9 and TIMP-1 were determined by RT-PCR in MCF-7 (left), MDA-MB-453 (Middle), MD-MB-231 (right) wt and GH+ breast cancer cells. 18S RNA was used as loading control in RT-PCR. d The translational expression profiles of MMP-2, MMP-9, TIMP-1, TIMP-2, N-cadherin, vimentin, snail and β-catenin gene expressions were determined by immunoblotting in MCF-7 (left), MDA-MB-453 (Middle), MD-MB-231 (right) wt and GH+ breast cancer cells. β-actin was used as a loading control
GH-induced NF-κB signaling prevented by curcumin in breast cancer cells
Autocrine GH signaling triggered the upregulation of NF-κB p65 and RelB protein levels through increasing phosphorylation of NF-κB p65 (Ser536) compared to parental cells, but curcumin treatment decreased the GH-induced NF-κB p65 and RelB expression levels in all breast cancer cells (Fig. 5a). Although autocrine GH signaling upregulated the expression levels of p100 and p52 in MCF-7 and MDA-MB-453 breast cancer cells, respectively, curcumin induced downregulation of these protein expression levels. GH overexpression induced translocation of pNF-κB and RelB from the cytoplasm to the nucleus in all breast cancer cells, but curcumin treatment prevented their translocation in each GH+ breast cancer cell line (Fig. 5b–d). Moreover, the transcriptional activity of NF-κB was determined by EMSA assay in curcumin-treated and -untreated MCF-7, MDA-MB-231 wt and GH+ breast cancer cells. According to the NF-κB EMSA assay, while NF-κB p65 nuclear DNA binding was noticeably higher in GH-expressing MCF-7, MDA-MB-453 and MDA-MB-231 breast cancer cells, curcumin treatment sharply decreased the GH-triggered biological activity of NF-κB in MDA-MB-453 breast cancer cells (Fig. 5e).
Curcumin prevented autocrine GH-induced classical and alternative NFκB signaling and nuclear localization of NF-κB in MCF-7, MDA-MB-453 and MDA-MB-231 breast cancer cells. a The effect of curcumin on IκKα, IκKβ, pIκKα/β (Ser176/180), Iκ-B, pIκ-B (Ser32), NF-κB, pNF-κB (Ser536), NIK, TRAF2, TRAF3, p100, pp100 (Ser866/870) and RelB gene expression profiles were determined by immunoblotting in MCF-7 (left), MDA-MB-453 (middle), MDA-MB-231 (right) wt and GH+ breast cancer cells. NF-κB and ReblB translocation due to autocrine GH expression and the curcumin treatment-induced suppression were determined in nuclear and cytoplasmic extracts by immunoblotting. Wedelolactone (10 µM) was used as a positive control for nuclear NF-κB and RelB translocation in b MCF-7, c MDA-MB-453, d MDA-MB-231 GH+ breast cancer cells. β-actin was used as a cytoplasmic loading control, Histon-3 was used as a nuclear loading control. e Biological activity of nuclear translocated NF-κB was determined by EMSA Assay in MCF-7 (left), MDA-MB-453 (middle) and MDA-MB-231 (right) breast cancer cells
Curcumin treatment depletes intracellular PA levels via modulating PA metabolism
Forced GH expression triggered the expression of ODC gene in GH+ cells as compared to wt breast cancer cells, but curcumin treatment suppressed ODC gene expression in both wt and GH+ breast cancer cells. However, this effect was clear in wt breast cancer cells as compared to GH+ breast cancer cells in transcriptional and translational level (Fig. 6a–d). Similarly, curcumin decreased the expressions of AZ and AZI in MDA-MB-231 wt and GH+ breast cancer cells. When we checked the expression levels of the PA catabolic enzymes, PAO and SSAT, upregulation in PAO and SSAT gene expressions was determined following curcumin treatment in each breast cancer cell. According to HPLC results, autocrine GH expression induced intracellular Put and Spd levels, but curcumin distinctly depleted autocrine GH-mediated PA level in MCF-7 breast cancer cells. However, in MDA-MB-453 breast cancer cells, active GH signaling was not effective in altering PA levels as compared to parental cells. When we compared the effect of curcumin on intracellular PA levels, we observed that curcumin significantly depleted the Spd and Spm levels in MDA-MB-453 breast cancer cells (Fig. 6e, f). Although curcumin treatment depleted intracellular Put, Spd and Spm levels in MDA-MB-231 wt cells, curcumin clearly depleted only Put and Spm levels in forced GH-expressing MDA-MB-231 breast cancer cells (Fig. 6g). To modulate the curcumin-induced ROS generation in GH+ MCF-7, MDA-MB-453 and MDA-MB-231 breast cancer cells, we performed DCFH-DA staining. According to the fluorescence microscopy of DCFH-DA staining, curcumin induced ROS generation in wt and GH+ MCF-7, MDA-MB-453 and MDA-MB-231 breast cancer cells. Flow cytometry analysis of DCFH-DA staining also confirmed these results. To demonstrate the reversible effect of curcumin-induced ROS generation, we performed N-acetylcysteine (NAC) pre-treatment with curcumin in MCF-7, MDA-MB-453 and MDA-MDA-MB-231 wt and GH+ breast cancer cells by DCFDH-DA staining (Fig. 6h).
Curcumin induced PA depletion by preventing ODC expression and triggering SSAT expression in autocrine GH-expressing breast cancer cells. a PA metabolic enzymes, ODC, AZ, AZI, SSAT and PAO, expression profiles following curcumin treatment were investigated in MCF-7 (left), MDA-MB-453 (middle), MDA-MB-231 (right) wt and GH+ breast cancer cells by immunoblotting. β-actin was used as a loading control. The transcriptional expression levels of b ODC, c SSAT and d PAO were determined by qRT-PCR in MCF-7, MDA-MB-453 and MDA-MB-231 breast cancer cells. 18S was used as a housekeeping and fold of alteration in expression profile calculated by the ΔΔCt method. The effect of curcumin on intracellular PA pool was determined by HPLC analysis in e MCF-7, f MDA-MB-453 and g MDA-MB-231 wt and GH+ breast cells. The data shown represent the mean ± S.D. from three experiments with four replicates. Statistical difference was analyzed using a two-way ANOVA; **p < 0.05, **p < 0.01, ***p < 0.001. h Curcumin and curcumin with NAC (5 mM) pre-treatment-induced ROS generation was determined by fluorescence microscopy and FACS flow cytometer after DCFD-HA staining in MCF-7, MDA-MB-453, MDA-MB-231 wt and GH+ breast cancer cells. Statistical difference was analyzed using two-way ANOVA; **p < 0.05, **p < 0.01, ***p < 0.001
Transient silencing of SSAT expression prevented curcumin-mediated cell viability loss, apoptotic cell death and ROS generation in GH+ breast cancer cells
Following SSAT transient silencing for 48 h, each cell line were treated with selected curcumin doses for 24 h. Using an MTT assay, we observed a significant decrease in the curcumin-mediated cell viability loss following SSAT silencing when we compared with only curcumin exposure in MCF-7, MDA-MB-453 and MDA-MB-231 breast cancer cells (***p < 0.001) (Fig. 7a–c). Subsequent Annexin V/PI staining performed to assess apoptotic cell death under SSAT silencing conditions revealed that curcumin-induced apoptotic cell death was overcome by SSAT silencing in each breast cancer cell. The curcumin-induced apoptotic cell death rate decreased from 6.7 to 0.8% in MCF-7 wt, and from 2.2 to 0.6% in MCF-7 GH+ breast cancer cells. Similarly, curcumin-triggered apoptotic cell death was prevented by SSAT silencing conditions in MDA-MB-453 wt and GH+ breast cancer cells. Moreover, transient silencing of SSAT declined the apoptotic cell death population from 11.8 to 4.6% in MDA-MB-231 wt and from 7.3 to 3.8% in MDA-MB-231 GH+ cells (Fig. 7d). To demonstrate the inhibition of curcumin-induced ROS generation under SSAT silencing condition, DCFDH-DA FACS flow analysis was performed for each breast cancer cell (Fig. 7e). MTT cell viability assay and Annexin V/PI analysis results were confirmed by DCFDH-DA FACS flow analysis.
Silencing of SSAT prevented curcumin-triggered cell viability loss, apoptotic cell death and ROS generation. The effect of curcumin on cell viability was assessed by MTT assay after SSAT silencing in a MCF-7, b MDA-MB-453, c MDA-MB-231 wt and GH+ breast cancer cells. d The apoptotic cell death after SSAT silencing of MCF-7, MDA-MB-453, MDA-MB-231 wt and GH+ breast cancer cells determined by PI and Annexin V/PI staining and flow cytometry, respectively. e Curcumin alone and with SSAT siRNA transfection induced ROS generation was determined by FACS flow cytometer after DCFDH-DA staining in MCF-7, MDA-MB-453, MDA-MB-231 wt and GH+ breast cancer cells
Curcumin induced cell cycle arrest at the G2/M phase in autocrine GH expressing breast cancer cells
Curcumin treatment led to a significant increase in the percentage of G2/M population compared to untreated cells in both MCF-7 wt and MCF-7 GH+ breast cancer cells (Fig. 8a). In MDA-MB-453 cells, curcumin triggered significant accumulation of the subG1 population in both wt and GH+ breast cancer cells. When we checked the potential effect of curcumin on wt and GH+ MDA-MB-231 breast cancer cells by PI FACS flow cytometer analysis, curcumin triggered the accumulation of the subG1 population in wt and GH+ MDA-MB-231 breast cancer cells. Moreover, exposure of curcumin not only induced subG1 population accumulation, but also triggered G2/M arrest in both wt and GH+ breast cancer cells. Curcumin treatment induced p53 and p21 expression, and downregulated the expression of Rb and pRb (Ser780) in autocrine GH-expressing MCF-7, MDA-MB-453, and MDA-MB-231 breast cancer cells (Fig. 8b).
Effects of curcumin on cell cycle progression induced apoptotic cell death via activating the extrinsic and intrinsic pathway and modulating Bcl-2 family members in autocrine breast cancer cells. a MCF-7, MDA-MB-453 and MDA-MB-231 wt and GH+ breast cancer cells were treated with curcumin for 24 h and then cells were harvested, fixed with ethanol and stained with PI. The cellular DNA contents were determined by flow cytometry analysis to detect the cell cycle distribution. Results shown were representative of three independent experiments. The bar graph presents the percentage of subG1, G1, S and G2/M phases in each cell line given below the PI FACS flow cytometer analysis. Results are shown as the means ±S.D. of two independent experiments. Statistical difference was analyzed using two-way ANOVA; **p < 0.05, **p < 0.01, ***p < 0.001. b The expression profiles of p53, p21, Rb and pRb (Ser 780) proteins were determined following curcumin treatment in MCF-7 (Left), MDA-MB-453 (Middle), MDA-MB-231 (Right) wt and GH+ breast cancer cells by immunoblotting. c The effect of curcumin on Fas, FADD, TRADD, caspase-2, -8,-3, -9, PARP expressions in MCF-7 (left), MDA-MB-453 (middle) and MDA-MB-231 (right) wt and GH+ breast cancer cells by immunoblotting. d The expression profiles of Bad, Bak, Bax, Bcl-2, Bcl-xL, Mcl-1 and Puma gene were determined by immunoblotting in MCF-7 (left), MDA-MB-453 (middle) and MDA-MB-231 (right) wt and GH+ breast cancer cells following 24 h curcumin treatment. β-actin was used as a loading control
Curcumin is a strong apoptotic agent by modulating Bcl-2 family members
Similar to Annexin V/PI staining, curcumin treatment triggered PARP cleavage in GH+ MCF-7, MDA-MB-453 and MDA-MB-231 breast cancer cells. While curcumin upregulated Fas expression, on the contrary FADD downregulation was observed in GH+ MCF-7 and MDA-MB-231 breast cancer cells. Although TRADD expression was downregulated in GH+ MCF-7 and MDA-MB-453 breast cancer cells, upregulation of TRADD expression was demonstrated following curcumin treatment in MDA-MB-231 GH+ cells. In addition, curcumin activated caspase-2, -8, -7 and -9 in each autocrine GH-expressing breast cancer cell (Fig. 8c). Moreover, curcumin treatment induced Bax expression and downregulated Bcl-XL expression in autocrine GH-expressing MCF-7, MDA-MB-453 and MDA-MB-231 breast cancer cells. However, in MCF-7 GH+ cells, curcumin treatment upregulated Bak and Puma expression, and downregulated Mcl-1 protein expression. However, no distinctive effect on Bad and Bcl-2 expression was detected as compared to MCF-7 wt breast cancer cells. In MDA-MB-453 GH+ breast cancer cells, curcumin-induced downregulation of Bak, Bcl-2 and Mcl-1 protein expression was established. Although curcumin had no obvious effect on Bak expression, upregulation in Bad, Puma expression, Bcl-2 and Mcl-1 downregulation were determined in MDA-MB-231 GH+ breast cancer cells (Fig. 8d). As a result, curcumin modulated the key players of the extrinsic and intrinsic apoptotic pathways, which led to increased apoptotic cell death in GH-expressing MCF-7, MDA-MB-453 and MDA-MB-231 breast cancer cells.
Discussion
Curcumin is a pleiotropic plant-derived molecule that exhibits anti-inflammatory, antioxidant and anticarcinogenic activity by targeting various signaling pathway such as PI3K/Akt, mTOR, NF-κB and JAK/STAT signaling. As a potential chemotherapeutic agent, curcumin induces cell death in various cancer cells such as prostate, melanoma, pancreatic, colon and breast cancer (Chauhan 2002; Guo et al. 2013; Liao et al. 2008). Due to in vivo studies demonstrating the effective antitumorigenic and antimetastatic potential of curcumin in colon, prostate and breast cancer, curcumin has been assumed o be a promising plant-derived therapeutic drug in cancer therapy. Although pre-clinical studies increase the potential of curcumin as a chemotherapeutic drug, the results from phase I/II trials of curcumin are contradictory and frustrating for the treatment potential of curcumin in cancer cases (Nelson et al. 2017). According to phase I trials of curcumin in colon cancer cells, poor detection of curcumin and its metabolite levels in urine attenuated the benefit of curcumin in gastrointestinal tract cancer therapy (Sharma et al. 2004). However, phase II trials of curcumin in advanced pancreatic cancer is promising because of its inhibitory effect on inflammatory cytokine levels such as IL-6, IL-10, IL-8 and IL-1 receptor antagonist (Dhillon et al. 2008). Although the therapeutic potential of curcumin was demonstrated to be a failure because of curcumin instability, and the low half-life in cancer patient’s circulation, a number of biological evidences obtained from in vitro and in vivo studies have gained attention for the evaluation of the apoptotic efficiency of curcumin, especially in drug-resistant in vitro cancer models to improve the effective chemotherapeutic strategy of curcumin (Bahadori and Demiray 2017; Nelson et al. 2017).
Recently, autocrine GH signaling-triggered invasion and metastatic profile has been demonstrated in MCF-10 mammary epithelial cells (Zhu et al. 2005a) and in MDA-MB453-GH+ xenograft mice models (Chen et al. 2015). Moreover, resistance against well-known chemotherapeutics such as tamoxifen (Mojarrad et al. 2010), doxorubicin (Minoia et al. 2012; Zatelli et al. 2009), daunorubicin (Zhu et al. 2005b), mitomycin C (Bougen et al. 2011) and its radioresistance potential (Bougen et al. 2012) have been reported for MCF-7, T47D and BT474 breast cancer cells. In this study, we demonstrated that although autocrine GH signaling revealed a resistance phenotype against low curcumin doses, increased doses of curcumin overcame the autocrine GH expression-mediated drug resistance in MCF-7, MDA-MB-453 and MDA-MB-231 breast cancer cells. Similar to our results, it was reported that an active autocrine GH-signaling mechanism in MDA-MB-231 and T47D breast cancer cells provided resistance to mitomycin C treatment (Bougen et al. 2011). However, contrary to all these data, it was established that GH expression might also cause a dose-dependent sensitivity for arsenic oxide treatment in MCF-7 breast cancer cells (Zekri et al. 2013). Thus, autocrine GH signaling has been assumed to be an obstacle for the therapeutic effect of drugs by triggering cancer drug resistance profile. However, curcumin managed to overcome GH-induced aggressiveness in a dose-dependent manner in breast cancer cells.
GH demonstrates its biological activity by activating JAK2-dependent STAT phosphorylation and nuclear translocation of STAT-5 dimers through the GH-targeting genes following binding its receptor, GHR (Birzniece et al. 2009). Autocrine GH signaling triggered cell proliferation through increasing the expression of JAK-2 and STAT-5 without acting on STAT-1 and STAT-3 expressions in MCF-7 breast cancer cells (Kaulsay et al. 1999). In a previous study, it was shown that JAK-2 was dependent on the increased GH expression, which led to invasive and metastatic mammary cell carcinoma (Kaulsay et al. 2000). Similar to previous data, we also demonstrated the forced GH expression increased the expression of STAT-1, -3, -5 and their phosphorylated forms in each GH+ breast cancer cell. However, we demonstrated curcumin prevented GH-mediated active JAK2 signaling due to phosphorylation at Tyr1007/1008 residues. Concomitantly, curcumin prevented STAT activation by inhibiting pSTAT5 (Tyr694) and pSTAT1 (Tyr701) expression in each GH+ breast cancer cell for the first time in this study. Therefore, we concluded that curcumin strongly inhibited the autocrine GH-mediated JAK2/STAT activation in breast cancer cells and might be used as STAT-3 and STAT-5 inhibitor in breast cancer therapy.
Besides STAT activation, it was reported that JAK-2 phosphorylation modulated p44/42 (Winston and Bertics 1992), c-jun N-terminal kinase (JNK) (Zhu et al. 1998) and p38 MAPK (Lanning and Carter-Su 2006). Exogenous GH was also demonstrated to activate both the p44/42 and p38 pathways (Hodge et al. 1998; Moller et al. 1992). p38 and p44/42 signaling was dependent on GH-mediated cell proliferation in MCF-7 cells, using the p38 and p44/42 pathway inhibitors SB203580 and PD98059, respectively (Kaulsay et al. 1999). Moreover, GH-expressing MCF-10A cells demonstrated oncogenic transformation via c-myc-induced cell growth and colony formation (Zhu et al. 2005a). Although GH overexpression-triggered cell growth and colony formation in breast cancer cells have been reported, the potential preventive effect of curcumin on autocrine GH-mediated growth induction in breast cancer cells has not yet been investigated. In accordance with previous results, autocrine GH-signaling breast cancer cells that exert higher expression profiles for key cascade molecules such as pAkt (Ser473), p38, pp38, p44/42, pp44/42 and their downstream targets c-raf, c-fos, c-jun and c-myc have been demonstrated in this study. Therefore, in this study, we evaluated that curcumin inhibited the GH-mediated activation of Akt/MAPK signaling axis to limit the cell survival machinery in MCF-7, MDA-MB-453 and MDA-MB-231 breast cancer cells.
Forced GH expression induced cell proliferation, invasion and metastasis in MDA-MB-453 and SKBR-3 breast cancer cells when compared with wt parental cells and triggered increased tumor volume in vivo (Chen et al. 2015). Moreover, GH expression was evaluated to increase cell proliferation and colony formation by triggering the expression of cyclin-D1, Bcl-2 and c-Myc in MCF-7 and NIH-3T3 as well as in vivo tumor growth in forced GH-expressing MCF-10 subcutaneously injected mouse models (Zhu et al. 2005a). Furthermore, one of the major regulators of angiogenesis promoting endothelial cell proliferation, survival, migration and invasion is vascular endothelial growth factor (VEGF-A), which has shown increased expression in autocrine GH-expressing MCF-7 cells as compared to mutant GH-expressing MCF-7 breast cancer cells (Brunet-Dunand et al. 2009). In addition, the GH-induced invasion and metastatic profile was reported in MCF-7 breast cancer cell by triggering the expression of EMT markers such as vimentin and fibronectin (Mukhina et al. 2004). Besides abnormal EMT marker expressions, loss of E-cadherin was also demonstrated to develop a cancer-invasive and metastatic profile (Nollet et al. 1999). Snail and slug transcription factors have been reported to act as repressors on E-cadherin expression in breast cancer cells (Hajra et al. 2002). Loss of E-cadherin activity through snail-induced metastasis via MMP activations was reported (Hajra et al. 2002). Similarly, autocrine GH-expressing MCF-7 cells showed sensitivity against arsenic trioxide via downregulation in MMP-2, -9 and E-cadherin compared to wt MCF-7 cells (Zekri et al. 2013). Similar to all these findings, autocrine GH expression triggers colony formation, invasion and metastasis in MCF-7, MDA-MB-231 and MDA-MB-453 breast cancer cells by inducing the EMT pathway, but curcumin suppressed the autocrine GH-induced invasive and metastatic profile by acting on MMP-2, vimentin and snail expression in breast cancer cells.
The expressions of snail and slug are under the control of NF-κB, a transcription factor, which acts on various intracellular cell processes such as cell proliferation, invasion, metastasis and angiogenesis. Binding of NF-κB with IκB initiates ubiquitin-dependent NF-κB degradation and prevents the NF-κB nuclear localization. However, activation of NF-κB is due to release of IκB from NF-κB through phosphorylation of IκB by Iκκ (Perkins 2007). Curcumin exposure suppresses nuclear translocation of NF-κB, which is one of the key molecules that triggers inflammation and carcinogenesis in cancer cells such as melanoma and breast cancer (Berrak et al. 2016; Marin et al. 2007). Curcumin triggered cell cycle arrest and invasion–metastasis via inhibiting the NF-κB-dependent inhibition of MMP-1 and -2 expressions in BT-483 and MDA-MB-231 breast cancer cells (Liu et al. 2009). Curcumin prevented the NF-κB translocation by blocking the IKK activation and triggering the IκBα induction agent, leading to the degradation of NF-κB (Shishodia et al. 2003). Therefore, one of the major obstacles in the failure of chemotherapy and radiotherapy is the insufficient NF-κB inhibition within the carcinogenic cells during cancer therapy. Since curcumin is an effective NF-κB inhibitor, the apoptotic induction potential of curcumin supported the application of curcumin as a chemotherapeutic agent in advanced pancreatic cancer cells and breast cancer (Bahadori and Demiray 2017; Nelson et al. 2017). In our in vitro autocrine GH-signaling breast cancer cell line models, GH overexpression induced classical and alternative NF-κB signaling, but the NF-κB inhibition potential of curcumin through suppressing the nuclear translocation of p65 and RelB in autocrine GH-expressing MCF-7, MDA-MB-453 and MDA-MB-231 breast cancer cells has been evaluated by our study. Therefore, this is the first report demonstrating that GH expression induced both classical and alternative NF-κB signaling, but curcumin was negatively effective on EMT by acting on NF-κB p65 and RelB in autocrine GH-signaling breast cancer cells.
As multiple genes targeting transcription factor, NF-κB inactivation through curcumin treatment induced apoptotic cell death via upregulating the PA catabolic enzyme SSAT gene expression in MCF-7 cells (Berrak et al. 2016). Since increased intracellular PA levels and accelerated ODC expression were reported in cancer cells when compared with healthy cells, chemotherapeutic drugs have been suggested with high therapeutic potential due to activation of PA catabolic enzymes: PAO, SMO, and SSAT (Battaglia et al. 2014). Curcumin-induced cell viability loss and apoptotic cell death due to inhibition of ODC activity were reported in HeLa cells (Liao et al. 2008). Similarly, chemotherapeutic drug-induced apoptotic cell death was evaluated due to PA depletion and ROS generation as a by-product of induced SSAT activity (Battaglia et al. 2014). Curcumin-induced ROS generation and intrinsic apoptotic cell death were reported in MCF-7 and BT-474 breast cancer cells (Berrak et al. 2016; Somasundaram et al. 2002). Moreover, drug-induced PA catabolic pathway key enzymes, SSAT and PAO, expression upregulation caused ROS generation-mediated apoptotic cell death in the colon (HCT 116 and HT-29) (Coskun et al. 2015) and prostate cancer cells (LNCaP and DU145) (Obakan et al. 2014). In addition, silencing of SSAT or PAO gene expression prevented drug-triggered apoptotic cell death in LNCaP and DU145 prostate colon cancer (Arisan et al. 2014). Besides, transient silencing of PAO prevented drug-mediated cell viability loss and PARP cleavage in HCT 116 colon cancer cells (Gurkan et al. 2013). As drugs induced the generation of H2O2 by upregulating PA catabolic enzymes in cancer cells, silencing of SSAT expression may be used to evaluate the role of PA catabolic pathway in the drug-induced apoptotic cell death in cancer cells. Thus, this study has evaluated the potential therapeutic effect of curcumin due to SSAT activation-induced ROS generation and PA depletion in autocrine GH expression-induced metastatic profile in breast cancer cells. Moreover, this study demonstrates that curcumin induced cell viability loss due to ROS generation in both wt and GH-expressing MCF-7, MDA-MB-453 and MDA-MB-231 breast cancer cells, but SSAT silencing prevented the curcumin-induced ROS generation and apoptotic cell death in autocrine GH+ breast cancer cells.
Curcumin exhibited a therapeutic effect via inducing S and G2/M phase arrest in cancer cells (Ke et al. 2014). Additional GH prevented doxorubicin-induced apoptotic cell death in both ER+ (MCF-7) and ER− (MDA-MB-231) breast cancer cells without activating or reverting to the doxorubicin-induced G2/M arrest (Minoia et al. 2012). Moreover, autocrine GH-expressing MDA-MB-231, and T47D breast cancer cells resistant to mitomycin C treatment were reported (Bougen et al. 2011). Doxorubicin-induced apoptotic cell death was reported to occur via blocking GHR in both ER− and ER+ breast cancer cells (Minoia et al. 2012). In addition, curcumin-induced apoptotic cell death occurred via activating both intrinsic and extrinsic pathway through modulating Bcl-2 family members in breast cancer cells (Reuter et al. 2008). Similar to all these previous data, although autocrine GH induced a resistant profile via upregulating snail and slug, due to NF-κB activation it triggered an aggressive breast cancer in vitro model. Concomitantly, curcumin triggered the activation of caspases to trigger extrinsic and intrinsic apoptotic cell death through causing G2/M cell cycle arrest. In addition, by this study, we evaluated the curcumin-induced apoptotic cell death in autocrine GH+ MCF-7, MDA-MB-453 and MDA-MB-231 breast cancer cells by upregulation of Bax and Bad and downregulation of Bcl-xL and Bcl-2 expression. Contrary to this result, autocrine GH-expressing MCF-7 cells sensitivity against arsenic trioxide via Bcl-2, c-myc and Bax expression prominently accelerated in GH+ MCF-7 cells compared to MCF-7 wt cells (Zekri et al. 2013). Thus, this is the first report that demonstrates autocrine GH-induced drug resistance phenotype can be overcome by dose-dependent curcumin treatment as a final consequence of NF-κB inactivation, ROS generation and PA depletion in MCF-7, MDA-MB-453 and MDA-MB-231 breast cancer cells. As curcumin acts as a potential NF-κB inhibitor and PA catabolic pathway activator, it might be used as a chemotherapeutic agent alone or in combination with other drugs to increase the apoptotic response in metastatic and/or drug-resistant breast cancer cases due to autocrine GH expression.
In accordance with previous reports, we found that autocrine GH signaling triggered aggressive cell phenotype via promoting cell growth, proliferation, invasion and metastasis under the control of the JAK/STAT and Akt/MAPK signaling pathway in in vitro forced GH-expressing breast cancer cells. As a novel finding, apoptotic dose of curcumin prevented autocrine GH-mediated invasion and metastasis through acting on both classical and alternative NF-κB signaling in ER− and ER+ breast cancer cells. In addition, the findings from this study revealed that curcumin induced extrinsic and intrinsic apoptotic cell death via SSAT activation-mediated ROS generation in autocrine GH-expressing MCF-7, MDA-MB-453 and MDA-MB-231 breast cancer cells. In this study, silencing of SSAT prevented curcumin-induced apoptotic cell death, and ROS generation in autocrine GH-expressing breast cancer cells was evaluated. In conclusion, we determined the therapeutic potential of curcumin in GH-mediated aggressive breast cancer cells. Further studies are required to illustrate the molecular machinary of curcumin-mediated apoptotic cell death in drug-resistant breast cancer cells and also evaluate the therapeutic potential of curcumin in autocrine GH triggered aggressive breast cancer in vivo models.
References
Arisan ED, Obakan P, Coker-Gurkan A, Calcabrini A, Agostinelli E, Unsal NP (2014) CDK inhibitors induce mitochondria-mediated apoptosis through the activation of polyamine catabolic pathway in LNCaP, DU145 and PC3 prostate cancer cells. Curr Pharm Des 20:180–188
Bahadori F, Demiray M (2017) A realistic view on “The essential medicinal chemistry of curcumin”. ACS Med Chem Lett 8:893–896. https://doi.org/10.1021/acsmedchemlett.7b00284
Battaglia V, Shields CD, Murray-Stewart T, Casero RA Jr (2014) Polyamine catabolism in carcinogenesis: potential targets for chemotherapy and chemoprevention. Amino Acids 46:511–519. https://doi.org/10.1007/s00726-013-1529-6
Bayet-Robert M et al (2010) Phase I dose escalation trial of docetaxel plus curcumin in patients with advanced and metastatic breast cancer. Cancer Biol Ther 9:8–14
Berrak O, Akkoc Y, Arisan ED, Coker-Gurkan A, Obakan-Yerlikaya P, Palavan-Unsal N (2016) The inhibition of PI3K and NF-κB promoted curcumin-induced cell cycle arrest at G2/M via altering polyamine metabolism in Bcl-2 overexpressing MCF-7 breast cancer cells. Biomed Pharmacother 77:150–160. https://doi.org/10.1016/j.biopha.2015.12.007
Birzniece V, Sata A, Ho KK (2009) Growth hormone receptor modulators. Rev Endocr Metab Disord 10:145–156. https://doi.org/10.1007/s11154-008-9089-x
Bougen NM, Yang T, Chen H, Lobie PE, Perry JK (2011) Autocrine human growth hormone reduces mammary and endometrial carcinoma cell sensitivity to mitomycin C. Oncol Rep 26:487–493. https://doi.org/10.3892/or.2011.1305
Bougen NM et al (2012) Autocrine human GH promotes radioresistance in mammary and endometrial carcinoma cells. Endocr Relat Cancer 19:625–644. https://doi.org/10.1530/ERC-12-0042
Brunet-Dunand SE et al (2009) Autocrine human growth hormone promotes tumor angiogenesis in mammary carcinoma. Endocrinology 150:1341–1352. https://doi.org/10.1210/en.2008-0608
Chauhan DP (2002) Chemotherapeutic potential of curcumin for colorectal cancer. Curr Pharm Des 8:1695–1706
Chen YJ, Zhang X, Wu ZS, Wang JJ, Lau AY, Zhu T, Lobie PE (2015) Autocrine human growth hormone stimulates the tumor initiating capacity and metastasis of estrogen receptor-negative mammary carcinoma cells. Cancer Lett 365:182–189. https://doi.org/10.1016/j.canlet.2015.05.031
Cohen SS (1978) What do the polyamines do? Nature 274:209–210
Coskun D, Obakan P, Arisan ED, Coker-Gurkan A, Palavan-Unsal N (2015) Epibrassinolide alters PI3K/MAPK signaling axis via activating Foxo3a-induced mitochondria-mediated apoptosis in colon cancer cells. Exp Cell Res 338:10–21. https://doi.org/10.1016/j.yexcr.2015.08.015
Dhillon N et al (2008) Phase II trial of curcumin in patients with advanced pancreatic cancer. Clin Cancer Res 14:4491–4499. https://doi.org/10.1158/1078-0432.CCR-08-0024
Duvoix A et al (2005) Chemopreventive and therapeutic effects of curcumin. Cancer Lett 223:181–190. https://doi.org/10.1016/j.canlet.2004.09.041
Guo H, Xu YM, Ye ZQ, Yu JH, Hu XY (2013) Curcumin induces cell cycle arrest and apoptosis of prostate cancer cells by regulating the expression of IkappaBalpha, c-Jun and androgen receptor. Pharmazie 68:431–434
Gurkan AC, Arisan ED, Obakan P, Palavan-Unsal N (2013) Inhibition of polyamine oxidase prevented cyclin-dependent kinase inhibitor-induced apoptosis in HCT 116 colon carcinoma cells. Apoptosis 18:1536–1547. https://doi.org/10.1007/s10495-013-0885-8
Hajra KM, Chen DY, Fearon ER (2002) The SLUG zinc-finger protein represses E-cadherin in breast cancer. Cancer Res 62:1613–1618
Hazan RB, Phillips GR, Qiao RF, Norton L, Aaronson SA (2000) Exogenous expression of N-cadherin in breast cancer cells induces cell migration, invasion, and metastasis. J Cell Biol 148:779–790
Hodge C, Liao J, Stofega M, Guan K, Carter-Su C, Schwartz J (1998) Growth hormone stimulates phosphorylation and activation of elk-1 and expression of c-fos, egr-1, and junB through activation of extracellular signal-regulated kinases 1 and 2. J Biol Chem 273:31327–31336
Igarashi K, Kashiwagi K (2000) Polyamines: mysterious modulators of cellular functions. Biochem Biophys Res Commun 271:559–564. https://doi.org/10.1006/bbrc.2000.2601
Kanai M et al (2011) A phase I/II study of gemcitabine-based chemotherapy plus curcumin for patients with gemcitabine-resistant pancreatic cancer. Cancer Chemother Pharmacol 68:157–164. https://doi.org/10.1007/s00280-010-1470-2
Kaulsay KK, Mertani HC, Tornell J, Morel G, Lee KO, Lobie PE (1999) Autocrine stimulation of human mammary carcinoma cell proliferation by human growth hormone. Exp Cell Res 250:35–50. https://doi.org/10.1006/excr.1999.4492
Kaulsay KK, Mertani HC, Lee KO, Lobie PE (2000) Autocrine human growth hormone enhancement of human mammary carcinoma cell spreading is Jak2 dependent. Endocrinology 141:1571–1584. https://doi.org/10.1210/endo.141.4.7426
Kaulsay KK, Zhu T, Bennett W, Lee KO, Lobie PE (2001) The effects of autocrine human growth hormone (hGH) on human mammary carcinoma cell behavior are mediated via the hGH receptor. Endocrinology 142:767–777. https://doi.org/10.1210/endo.142.2.7936
Ke CS, Liu HS, Yen CH, Huang GC, Cheng HC, Huang CY, Su CL (2014) Curcumin-induced Aurora-A suppression not only causes mitotic defect and cell cycle arrest but also alters chemosensitivity to anticancer drugs. J Nutr Biochem 25:526–539. https://doi.org/10.1016/j.jnutbio.2014.01.003
Lanning NJ, Carter-Su C (2006) Recent advances in growth hormone signaling. Rev Endocr Metab Disord 7:225–235. https://doi.org/10.1007/s11154-007-9025-5
Liao YF, Hung HC, Hour TC, Hsu PC, Kao MC, Tsay GJ, Liu GY (2008) Curcumin induces apoptosis through an ornithine decarboxylase-dependent pathway in human promyelocytic leukemia HL-60 cells. Life Sci 82:367–375. https://doi.org/10.1016/j.lfs.2007.11.022
Liu Q, Loo WT, Sze SC, Tong Y (2009) Curcumin inhibits cell proliferation of MDA-MB-231 and BT-483 breast cancer cells mediated by down-regulation of NFkappaB, cyclinD and MMP-1 transcription. Phytomedicine 16:916–922. https://doi.org/10.1016/j.phymed.2009.04.008
Marin YE et al (2007) Curcumin downregulates the constitutive activity of NF-kappaB and induces apoptosis in novel mouse melanoma cells. Melanoma Res 17:274–283. https://doi.org/10.1097/CMR.0b013e3282ed3d0e
Miller SA, Dykes DD, Polesky HF (1988) A simple salting out procedure for extracting DNA from human nucleated cells. Nucleic Acids Res 16:1215
Minoia M et al (2012) Growth hormone receptor blockade inhibits growth hormone-induced chemoresistance by restoring cytotoxic-induced apoptosis in breast cancer cells independently of estrogen receptor expression. J Clin Endocrinol Metab 97:E907–E916. https://doi.org/10.1210/jc.2011-3340
Mojarrad M et al (2010) Autocrine human growth hormone expression leads to resistance of MCF-7 cells to tamoxifen. Med Oncol 27:474–480. https://doi.org/10.1007/s12032-009-9237-5
Mol JA, Henzen-Logmans SC, Hageman P, Misdorp W, Blankenstein MA, Rijnberk A (1995) Expression of the gene encoding growth hormone in the human mammary gland. J Clin Endocrinol Metab 80:3094–3096. https://doi.org/10.1210/jcem.80.10.7559904
Moller C, Hansson A, Enberg B, Lobie PE, Norstedt G (1992) Growth hormone (GH) induction of tyrosine phosphorylation and activation of mitogen-activated protein kinases in cells transfected with rat GH receptor cDNA. J Biol Chem 267:23403–23408
Mukhina S, Mertani HC, Guo K, Lee KO, Gluckman PD, Lobie PE (2004) Phenotypic conversion of human mammary carcinoma cells by autocrine human growth hormone. Proc Natl Acad Sci USA 101:15166–15171. https://doi.org/10.1073/pnas.0405881101
Nelson KM, Dahlin JL, Bisson J, Graham J, Pauli GF, Walters MA (2017) The essential medicinal chemistry of curcumin. J Med Chem 60:1620–1637. https://doi.org/10.1021/acs.jmedchem.6b00975
Nollet F, Berx G, van Roy F (1999) The role of the E-cadherin/catenin adhesion complex in the development and progression of cancer. Mol Cell Biol Res Commun 2:77–85. https://doi.org/10.1006/mcbr.1999.0155
Obakan P, Arisan ED, Calcabrini A, Agostinelli E, Bolkent S, Palavan-Unsal N (2014) Activation of polyamine catabolic enzymes involved in diverse responses against epibrassinolide-induced apoptosis in LNCaP and DU145 prostate cancer cell lines. Amino Acids 46:553–564. https://doi.org/10.1007/s00726-013-1574-1
Pegg AE (1988) Polyamine metabolism and its importance in neoplastic growth and a target for chemotherapy. Cancer Res 48:759–774
Perkins ND (2007) Integrating cell-signaling pathways with NF-kappaB and IKK function. Nat Rev Mol Cell Biol 8:49–62. https://doi.org/10.1038/nrm2083
Raccurt M, Lobie PE, Moudilou E, Garcia-Caballero T, Frappart L, Morel G, Mertani HC (2002) High stromal and epithelial human gh gene expression is associated with proliferative disorders of the mammary gland. J Endocrinol 175:307–318
Reuter S, Eifes S, Dicato M, Aggarwal BB, Diederich M (2008) Modulation of anti-apoptotic and survival pathways by curcumin as a strategy to induce apoptosis in cancer cells. Biochem Pharmacol 76:1340–1351. https://doi.org/10.1016/j.bcp.2008.07.031
Sharma RA et al (2004) Phase I clinical trial of oral curcumin: biomarkers of systemic activity and compliance. Clin Cancer Res 10:6847–6854. https://doi.org/10.1158/1078-0432.CCR-04-0744
Shishodia S, Potdar P, Gairola CG, Aggarwal BB (2003) Curcumin (diferuloylmethane) down-regulates cigarette smoke-induced NF-kappaB activation through inhibition of IkappaBalpha kinase in human lung epithelial cells: correlation with suppression of COX-2, MMP-9 and cyclin D1. Carcinogenesis 24:1269–1279. https://doi.org/10.1093/carcin/bgg078
Siegel R et al (2012) Cancer treatment and survivorship statistics. CA Cancer J Clin 62:220–241. https://doi.org/10.3322/caac.21149
Somasundaram S, Edmund NA, Moore DT, Small GW, Shi YY, Orlowski RZ (2002) Dietary curcumin inhibits chemotherapy-induced apoptosis in models of human breast cancer. Cancer Res 62:3868–3875
Sternlicht MD (2006) Key stages in mammary gland development: the cues that regulate ductal branching morphogenesis. Breast Cancer Res 8:201. https://doi.org/10.1186/bcr1368
Winston LA, Bertics PJ (1992) Growth hormone stimulates the tyrosine phosphorylation of 42- and 45-kDa ERK-related proteins. J Biol Chem 267:4747–4751
Wu ZS et al (2011) Tumor expression of human growth hormone and human prolactin predict a worse survival outcome in patients with mammary or endometrial carcinoma. J Clin Endocrinol Metab 96:E1619–E1629. https://doi.org/10.1210/jc.2011-1245
Zatelli MC et al (2009) Growth hormone excess promotes breast cancer chemoresistance. J Clin Endocrinol Metab 94:3931–3938. https://doi.org/10.1210/jc.2009-1026
Zekri A, Ghaffari SH, Yousefi M, Ghanizadeh-Vesali S, Mojarrad M, Alimoghaddam K, Ghavamzadeh A (2013) Autocrine human growth hormone increases sensitivity of mammary carcinoma cell to arsenic trioxide-induced apoptosis. Mol Cell Endocrinol 377:84–92. https://doi.org/10.1016/j.mce.2013.07.002
Zhu T, Goh EL, Lobie PE (1998) Growth hormone stimulates the tyrosine phosphorylation and association of p125 focal adhesion kinase (FAK) with JAK2. Fak is not required for stat-mediated transcription. J Biol Chem 273:10682–10689
Zhu T, Starling-Emerald B, Zhang X, Lee KO, Gluckman PD, Mertani HC, Lobie PE (2005a) Oncogenic transformation of human mammary epithelial cells by autocrine human growth hormone. Cancer Res 65:317–324
Zhu Z, Mukhina S, Zhu T, Mertani HC, Lee KO, Lobie PE (2005b) p44/42 MAP kinase-dependent regulation of catalase by autocrine human growth hormone protects human mammary carcinoma cells from oxidative stress-induced apoptosis. Oncogene 24:3774–3785. https://doi.org/10.1038/sj.onc.1208541
Acknowledgements
The authors wish to thank Furkan Kaysın and Derya Bulut for their technical support.
Funding
This work was supported by the TUBITAK Scientific Projects Support Center (TUBITAK-1001 Program; Grant Number: 113Z791, 2014-2017).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical statement
This article does not involve any studies with animals performed by any of the authors. The research has been performed on commercially available cell lines. Ethical approval for GH cloning experiment was obtained from the Marmara University Medical Faculty and Research Ethics Committee.
Additional information
Handling Editor: E. Agostinelli.
Rights and permissions
About this article
Cite this article
Coker-Gurkan, A., Celik, M., Ugur, M. et al. Curcumin inhibits autocrine growth hormone-mediated invasion and metastasis by targeting NF-κB signaling and polyamine metabolism in breast cancer cells. Amino Acids 50, 1045–1069 (2018). https://doi.org/10.1007/s00726-018-2581-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00726-018-2581-z