Abstract
Species A rotaviruses are the leading viral cause of acute gastroenteritis in children under 5 years of age worldwide. Despite progress in the characterization of the pathogenesis and immunology of rotavirus-induced gastroenteritis, correlates of protection (CoPs) in the course of either natural infection or vaccine-induced immunity are not fully understood. There are numerous factors such as serological responses (IgA and IgG), the presence of maternal antibodies (Abs) in breast milk, changes in the intestinal microbiome, and rotavirus structural and non-structural proteins that contribute to the outcome of the CoP. Indeed, while an intestinal IgA response and its surrogate, the serum IgA level, are suggested as the principal CoPs for oral rotavirus vaccines, the IgG level is more likely to be a CoP for parenteral non-replicating rotavirus vaccines. Integrating clinical and immunological data will be instrumental in improving rotavirus vaccine efficacy, especially in low- and middle-income countries, where vaccine efficacy is significantly lower than in high-income countries. Further knowledge on CoPs against rotavirus disease will be helpful for next-generation vaccine development. Herein, available data and literature on interacting components and proposed CoPs against human rotavirus disease are reviewed, and limitations and gaps in our knowledge in this area are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Species A rotaviruses, members of the family Sedoreoviridae, are the leading viral cause of acute gastroenteritis and are responsible for 128,500–215,000 deaths of children under 5 years old worldwide [103, 120, 165, 170]. Rotavirus particles consist of a triple-layered capsid including the core shell formed by virus protein 2 (VP2), which encloses the 11 segments of the double-stranded RNA (dsRNA) genome [62], the intermediate capsid (VP6), and the outer capsid (VP7), which is decorated with VP4 spikes protruding from its surface [62]. Based on the RNA sequences of VP7 (a glycoprotein or G-type antigen) and VP4 (a protease-sensitive protein or P-type antigen), rotaviruses are classified into various G and P genotypes. Neutralizing antibodies (nAbs) are induced by both VP7 and VP4 proteins, while non-neutralizing antibodies are elicited by other structural proteins (VP6, VP2) and non-structural protein 4 (NSP4) [42, 145, 161, 162]. Proteolysis of VP4 results in its cleavage into two subunits, VP5* and VP8*, the head of the VP4 spike, which interacts with host cell receptors and is required for virion attachment and thus rotavirus infection [154]. Transmission occurs mainly by the fecal-oral route, although spread by person-to-person contact, contaminated water, or fomites is also possible [52]. The virus is highly contagious, and almost all unvaccinated children experience at least one rotavirus infection during their first two years of life [98, 175]. Accordingly, rotavirus infection is one of the main causes of childhood morbidity and mortality globally [165]. To date, no specific therapy for rotavirus-induced gastroenteritis is available, but the introduction of approved, safe, and effective live attenuated oral vaccines such as Rotarix and RotaTeq has had a great impact on the prevention and control of severe rotavirus-associated disease [13]. Moreover, Rotavac (Bharat Biotech) and Rotasiil (Hyderabad and Serum Institute of India) have exhibited an efficacy similar to that of RotaTeq and Rotarix in India [15] and have been prequalified by the World Health Organization (WHO). In 2009 [190], WHO recommended the inclusion of rotavirus vaccines in the national vaccination programs of all member countries. To date, 120 countries have included oral rotavirus vaccines (RotaTeq or Rotarix) in their national vaccination programs, and approximately 15 additional countries are planning to introduce them [1, 33]. Following the introduction of rotavirus vaccines, numerous high-income countries in the Americas, Europe, and Australia have reported a significant decline in hospitalizations and deaths of infants due to acute gastroenteritis [13, 23, 26]. However, this has not been the case in several low- and middle-income countries [56, 134, 165, 183], implying the need for improved next-generation vaccines [69] and/or a better understanding of the immune correlates of protection (CoPs) during the course of natural infection and vaccination. There are several reasons suggested for the observed lower efficacy/effectiveness of live attenuated rotavirus vaccines in low- and middle-income countries than in high-income countries. The most notable reasons include high titers of maternal antibodies (Abs) [56, 133, 174], impaired immune responses (due to malnutrition, environmental enteropathy, gut microbiota, and coinfections) [36, 56, 109, 135, 174], and differences in host receptor human histo-blood group antigens (HBGAs) [56, 121, 126].
By definition, a CoP is an immune response that is statistically correlated with protection against disease by vaccination (or natural infection) and might be either mechanistic (mCoP; which is causally responsible for the protection) or non-mechanistic (nCoP; which does not cause protection but correlates with other immune responses that are protective) [138]. In the case of rotavirus infection, CoPs are complex and can be affected by numerous factors. Currently, the rotavirus-specific immunoglobulin A (rotavirus-IgA) level is considered the standard for the assessment of vaccine/infection-induced immunity against rotavirus, while it is suggested to be a suboptimal nCoP marker in low- and middle-income countries [65, 142]. Indeed, maternal Abs, including IgG and IgA, which are thought to be responsible for the lower vaccine efficacy in low- and middle-income regions, might be factors that affect protection [104]. In addition, the presence of non-nAbs against VP2, VP6, NSP2, and NSP4, which are detected in most individual sera after rotavirus infection, are main antigenic targets other than VP4 and VP7 in immune responses and protection, but their clinical significance for protection is unclear [29, 44, 49, 131]. Moreover, the gut microbiome is also implicated in the pathogenesis of rotaviruses [57]. It has been shown that the microbiome diversity in rotavirus-infected children is lower than in healthy uninfected children [57]. The complexity and large number of factors contributing to protection against rotavirus infection present an important challenge, both for vaccination programs to control rotavirus infection in many (especially developing) countries and for next-generation vaccine development efforts. Herein, the clinical endpoints and the protective immune responses to natural infection or vaccination are reviewed, and limitations and gaps in our knowledge in this area are discussed.
Immune responses to natural rotavirus infection as potential CoPs
It has been suggested that immune responses to asymptomatic or symptomatic natural rotavirus infection do not provide sterilizing immunity but might protect the individual from moderate-to-severe disease and/or hospitalization for subsequent reinfections [64, 175]. Of note, the incidence of asymptomatic rotavirus infections in children between 6 and 24 months of age has been found to be 3-4 times higher than that of symptomatic infections. Interestingly however, both symptomatic and asymptomatic primary rotavirus infections confer a similar degree of protection against subsequent infections [175]. These observations highlight the crucial role of asymptomatic rotavirus infections in protection against disease and have implications for vaccine development.
The level of immunity generated by natural infection can be determined by observing a subsequent episode of rotavirus infection. One episode of rotavirus infection might provide > 70% protection against rotavirus-induced diarrhea, while after two subsequent infections (symptomatic or asymptomatic), complete protection for moderate-to-severe illness may be achieved [14, 18, 64, 93, 175, 186, 189]. In a cohort study of young children in India, the difference of the severity of diarrhea in the first and second infections was not found to be statistically significant, and protection against moderate or severe disease was only 79% after three subsequent infections [68]. Furthermore, a community cohort study of newborn children in Guinea-Bissau showed that a single infection conferred 66% protection against reinfection in the same epidemic, but only 34% protection against reinfection in subsequent epidemics [64]. The variability in protection after subsequent rotavirus infections could be attributed to differences in the subsequent inoculum size or differences in the level of immunity generated by natural infection in different population groups [44].
Numerous studies have shown that rotavirus-specific Abs can be used as immune markers following natural infection [40]. However, reports on Ab-based acquired homotypic and/or heterotypic immunity after natural rotavirus infection are complex and controversial. In this context, some studies have found homotypic Ab responses to be induced by initial exposure to a rotavirus and heterotypic Ab responses to be induced by subsequent exposures [38, 39, 55, 75, 129, 130, 147, 155, 163]. These findings suggest that homotypic immunity would be primed by Ab generation against homotypic epitopes on VP4 or VP7 proteins [74]. However, heterotypic protection might be boosted by generation of Abs against heterotypic (conserved) epitopes of VP4 or VP7 proteins [132] and also by non-nAbs directed against VP6, VP2, NSP2, and NSP4 [20, 125]. Accordingly, there are reports suggesting that serum titers of nAbs against rotavirus are correlated with either homotypic or heterotypic protection from viral disease [8]. However, due to the polyclonal nature and diversity of Abs raised against rotavirus proteins, the exact level (IU/mL) of serum Abs that can be considered protective is not known. In this context, the results of an early trial conducted in a Japanese orphanage indicated that nAb levels higher than 1:128 were protective against homotypic rotavirus gastroenteritis caused primarily by a G3 strain, while heterotypic responses against G1 and G4 strains were also produced [38]. Similarly, the results of a later study provided analogous data for homotypic protection, indicating that repeated infections with the same G type were less likely to occur [175], Accordingly, a case-control study in Bangladesh demonstrated that children with rotavirus-related diarrhea had considerably lower baseline homotypic and heterotypic nAb titers than age-matched controls, suggesting the importance of nAbs for protection against the disease [187]. Of note, results of similar studies on rotavirus-infected children with or without gastroenteritis indicated a correlation with pre-existing levels of IgA rather than IgG for protection against viral disease [84, 116]. In contrast, results of another study on Bangladeshi children suggested a correlation of IgG titers with protection against symptomatic and clinically significant rotavirus diarrhea [46]. Interestingly, the results of another study from Mexico [176] suggested the importance of both IgG and IgA as correlates of protection, showing that serum IgG titers of > 6400 and IgA titers of > 800 were associated with a lower risk of rotavirus infection. However, these titers were significantly higher than those reported in a study in the United States in which IgG titers of > 800 and IgA titers of > 200 were associated with a lower risk of rotavirus infection [130]. In parallel, results of a recent study on Indian children suggested the potential importance of sufficient pre-existing IgG and IgA Ab titers in serum for a reduced risk of rotavirus infection and found an increase in the titers of such Abs with age [141]. Therefore, ambiguous reports and controversial results pertaining to the type and titer of the Abs required for protection against rotavirus infection or disease indicate the need for better understanding of how they function as CoPs.
It has been shown that passive transmission of IgA and nAbs via breast milk can inhibit rotavirus infection [19, 32, 61, 123, 124, 152, 167]. Therefore, breastfeeding may protect against rotavirus infection not only by the nonspecific action of glycoproteins such as lactoferrin and lactadherin [160] but also by rotavirus-specific IgA that is produced via the gut-mammary gland axis [127]. Previous studies showed a rural/urban residency gradient of rotavirus-specific Abs [45, 127]. In this context, it has been shown that the level of IgA against rotavirus in breast milk from Bangladeshi mothers (whose exposure to rotaviruses is considerably higher) was higher than that from Swedish mothers. Considering the higher efficacy of rotavirus vaccination in Sweden than in Bangladesh, this observation might suggest a reverse relation of rotavirus-specific IgA in breast milk to rotavirus vaccination efficacy in breastfed children [127]. A similar study conducted in a rural community in Bangladesh showed that exclusive breastfeeding might temporarily protect infants and postpone severe rotavirus diarrhea, but there was no overall protection during the first two years of life [45]. In agreement with this, in a study in India, it was shown that IgA titers in the breast milk of mothers whose infants were infected with rotavirus within the first 5 days of life were significantly lower than in that of those whose infants were uninfected during the same time period [89]. However, contrary to the above reports, in a Mexican study, there was no difference in the titers of breast milk Abs between breastfed infants infected with rotavirus and those who remained unaffected during the first year of life [22]. Accordingly, a study undertaken in Vietnam showed that, while the level of total IgA was significantly higher in mothers living in a rural region than those in an urban region, urban mothers had significantly higher rotavirus-specific IgA Ab titers than rural mothers [168]. Although maternal anti-rotavirus Abs protect neonates and unvaccinated infants during the period of immune system maturation and can be protective during this time of high risk for experiencing severe rotavirus disease, further studies are required to determine its importance and contributing role in protection against rotavirus disease. Despite extensive investigations on the protective role of rotavirus-specific Abs [40], studies and data on the protective role of the T-cell immune responses in the course of natural rotavirus infection or vaccination are limited [101, 115]. Studies in animal models have indicated a crucial role of T cells in replication-inhibited clearance of infection and generation of protection-associated Abs [55, 118, 119]. Induction of both CD4+ and CD8+ T cell responses in rotavirus infection has been documented, albeit at much lower levels compared to other viral infections [88, 114]. A recent systemic review showed that although rotavirus-specific T cells are generally present at low frequency, their reactivity is broadened with increasing age in children [101]. In addition, CD4+ and CD8+ T cell responses in rotavirus infection are heterotypic and more transient, but they can occur in the absence of detectable antibody responses through repeated exposure [101]. Therefore, it is necessary to fully understand the protective role of rotavirus-specific T-cell responses in the course of natural infection or vaccination [111]. A summary of studies on potential CoPs against natural rotavirus infection is shown in Table 1.
Immune responses to rotavirus vaccination as potential CoPs
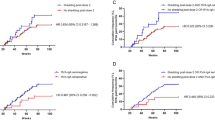
For most of the vaccines that have been approved for human use, such as those against hepatitis A and B, rabies, poliovirus, measles, anthrax, diphtheria, and tetanus, the humoral (antibody) response, which is usually measured by neutralization assay or ELISA, is the most important CoP [85, 139]. Of note, for many established enteric vaccines (such as those for hepatitis A, Vi typhoid, and poliovirus infections), humoral responses are considered CoPs, although they may not correlate well with protective efficacy or relevant gut immune responses [85, 139]. Likewise, in the case of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), strain-specific neutralizing Abs are the principal CoPs, and their titers correlate directly with protection against infection [58, 70]. However, it has also been shown that T cell responses and Fc effector Abs are also important players that can affect the efficacy of vaccines against SARS-CoV-2 infection [58, 67, 96]. It should be noted that vaccine-induced Abs might either act directly by neutralizing the infectious agent or be a marker for the presence of a robust T-cell response that protects against pathogenesis through distinct immunological mechanisms [21]. Therefore, despite the value of vaccine-induced neutralizing Abs as CoPs, for development of effective and durable vaccines against rotaviruses, other factors might need to be considered. Indeed, rotavirus vaccines represent one of the most complex challenges for the definition of CoPs. Vaccination has already impacted the global burden and epidemiology of rotavirus disease in a positive way, with great success in high-income countries, but the same is not true for low-income societies [24]. Infants typically receive two oral doses of Rotarix (GSK, UK) or three oral doses of RotaTeq (Merck, USA) in their first 6 months of life. In addition, two other live attenuated oral rotavirus vaccines, Rotavac (Bharat Biotech) and Rotasiil (Hyderabad and Serum Institute of India), have also been prequalified by WHO and licensed in several countries. Moreover, several monovalent rotavirus vaccines, such as Rotavin-M1 (PolyVac) [151, 166], Lanzhou lamb rotavirus (LLR) [192], and neonatal rotavirus vaccine (RV3-BB) [16], are licensed nationally in Vietnam, China, and Australia, respectively. Furthermore, several non-replicating rotavirus vaccines, including recombinant or inactivated vaccines, have shown promising results in preclinical or clinical studies. Identifying relevant CoPs for these vaccines would permit us to predict both the risk of clinical disease and vaccination efficacy [8]. Since the introduction of rotavirus vaccines, the intestinal IgA response and its surrogate, the serum IgA level, have been considered the principal CoPs. In this context, various human trials conducted in several countries around the world with different economic, cultural, sanitary, and nutritional conditions have used anti-rotavirus-IgA levels to examine the efficacy of rotavirus vaccines, especially for Rotarix and RotaTeq. Vaccine-induced anti-rotavirus IgA levels (> 20 U/mL) are an important predictor of protection against rotavirus infection and are associated with vaccine efficacy [11, 44, 65, 137, 169]. In some trials, type-specific neutralizing Ab titers have also been reported [9, 44, 156, 178]. A review of clinical trial data for the Rotarix and RotaTeq vaccines [137] showed that a geometric mean concentration (GMC) of anti-rotavirus IgA below 90 was associated with a decline in vaccine efficacy. Indeed, efficacy during first 2 years of life was significantly lower in countries with an IgA GMC < 90 than in countries with a GMC > 90. This suggests that IgA titers might be an important immune correlate protecting children from rotavirus diarrhea [137]. However, rotavirus-specific post-immunization serum IgA titers and seroconversion were more strongly associated with protection from rotavirus diarrhea in high-income (low child-mortality) countries than in low- and middle-income (high child-mortality) countries. In this context, it was shown that rotavirus-specific post-immunization serum IgA titers were not an optimal correlate of protection in many low- and middle-income (high child-mortality) countries such as Bangladesh [110]. Similar studies have shown that low serum rotavirus-specific IgA is associated with increased rotavirus load in vaccinated Malawian children with acute gastroenteritis and is also associated with an increased risk of clinical rotavirus vaccine failure [12, 140]. It has been shown that the kinetics of fecal Rotarix RNA shedding as well as the IgA responses in immunized twins after the first and second vaccine doses were similar, suggesting that rotavirus vaccine viral replication in the intestine and the host immune response are similar in twin siblings [60]. Generally, the documentation of factors that are related to protection will facilitate the improvement of rotavirus vaccines strategies. A summary of studies on potential CoPs related to vaccination is presented in Table 2.
Live attenuated rotavirus vaccines
WHO-prequalified rotavirus vaccines
The results of clinical trials and systemic reviews on all four licensed rotavirus vaccines [6, 9, 13, 82, 102, 197] have indicated low vaccine efficacy and effectiveness in low- and middle-income countries (29–77% within the first/second year after vaccination) compared to that of higher-income countries, where the efficacy was 85–98% for preventing severe rotavirus disease by immunization with RotaTeq or Rotarix [6, 15, 59, 95, 102, 108, 122, 144, 150, 159, 164, 177, 179, 180]. The results of the clinical trials in India and Niger for the Rotasiil vaccine demonstrated an efficacy of 36% and 67%, respectively, against severe rotavirus gastroenteritis [86, 99]. The results of a phase III efficacy trial of the Rotavac vaccine in India indicated an efficacy of 55% against severe rotavirus disease, with overall protection up to two years of age [15]. Similar results were reported for the same vaccine in infants in Zambia [41]. Reports on post-licensure vaccine effectiveness data indicated 84-86% (13 studies), 75-77% (8 studies), and 57-63% effectiveness for Rotarix in countries with low, medium, and high childhood mortality rates, respectively. For the RotaTeq vaccine, effectiveness was reported to be 84-90% (20 studies) and 45-66% in countries with low and high child mortality rates, respectively [25, 91]. Although efficacy data from clinical trials are available for Rotavac and Rotasiil, no post-licensure vaccine effectiveness data have been reported for these vaccines.
As discussed above, rotavirus-specific IgA Abs are used to monitor vaccine effectiveness at the population level. Studies relating rotavirus IgA seroconversion to protection have indicated that, in high-income countries, including Europe, Japan, Hong Kong, China, and Australia, high levels of vaccination effectiveness for both Rotarix and RotaTeq, with long-lasting (until two years of age) protection (both homotypic and heterotypic) have been documented. More recently, it was shown that for infants vaccinated with Rotarix in high-income countries, seroconversion might serve as a perfect CoP, correlating with 96% reduction in the risk of rotavirus gastroenteritis compared to infants showing no seroconversion [11]. However, lower and more variable levels of protection (about 30-60%) and reduction in the duration of protection have been reported in low- and middle-income countries, including South Africa, Malawi, Ghana, Kenya, and Mali, for the same vaccines [9, 15, 41, 53, 86, 99, 112]. In clinical studies, anti-rotavirus IgA is a valuable indicator of protection against rotavirus gastroenteritis. In particular, oral rotavirus vaccines replicate in the gut, and a mucosal IgA response (or its surrogate, serum IgA) can be considered an imperfect CoP. Although, it is not considered a true clinical endpoint and does not accurately predict specific levels of protective immunity, it is still a practical and informative measure of an infant’s risk of rotavirus gastroenteritis after vaccination.
Nationally licensed rotavirus vaccines
A study of vaccination with one dose of rhesus rotavirus-tetravalent vaccine (RRV-TV, licensed as RotaShield) showed that anti-rotavirus-IgA seroconversion was associated with protection from infection, but not from gastroenteritis. After three doses, the titer of anti-rotavirus IgA was found to have a significant association with protection against acute gastroenteritis, but no specific titer was reported as a CoP for this vaccine [43]. Another study compared serum anti-rotavirus IgA levels as a marker of protection in both RRV-TV (RotaShield)-vaccinated and naturally infected children. The results of that study indicated that a serum anti-rotavirus IgA level >1:800 correlated with 68% protection in children who had been infected previously, but this was not a reliable CoP for those immunized with the RRV-TV vaccine [73]. In parallel, results of a meta-analysis on the same vaccine indicated that levels of anti-rotavirus IgA ≥ 20 U/mL were moderately correlated with a lower risk of gastroenteritis in vaccinated children [37].
The effect of maternal Abs (either acquired transplacentally or from breast milk) were also studied extensively, but no inhibitory or beneficial effect on rotavirus vaccination efficacy (‘vaccine uptake’) could be documented [5, 77, 149]. It has been shown that, in the presence of maternal Abs and breast milk, neonatal P[6] strains such as RV3 (G3P[6]) replicate efficiently in the gut of the infected infant without causing any disease symptoms [30]. Based on this finding, this naturally attenuated human neonatal strain (G3P[6]) was used to develop the RV3-BB vaccine. The RV3-BB vaccine has been shown to be immunogenic and well tolerated when the first dose is given within 0–5 days after birth (neonatal schedule) or when the first dose is administered at 6-8 weeks of age (routine infant schedule) [16, 18]. The efficacy of RV3-BB when administered in three doses on a neonatal schedule (birth, 6 weeks, and 10 weeks) was shown to be 94% at 12 months and 75% at 18 months of age in a high-child-mortality setting in Indonesia [17, 153]. In a similar study in Malawi, 4 and 18 weeks after administration of three doses of RV3-BB on a neonatal schedule (birth, 6 weeks, and 10 weeks), cumulative serum IgA seroconversion was observed in 52% and 67% of participants, respectively, compared to 59% of these on an infant schedule (6, 10, and 14 weeks) [191]. Furthermore, recent studies in Indonesia and New Zealand [34, 54] have shown that maternal rotavirus Abs in breast milk appear to have a minimal impact on RV3-BB vaccine uptake when administered with a short delay in breast-feeding in settings with a high rotavirus disease burden. Anti-rotavirus IgA levels in colostrum or breast milk and levels of placental IgG and serum nAbs did not show any impact on the serum IgA response or stool excretion after three doses of RV3-BB vaccine using either a neonatal or infant schedule [34, 54]. Interestingly, immunization with three doses of RV3-BB vaccine in Indonesia resulted in an efficacy of 94% for neonates (0 to 5 days, 8, and 14 weeks of age) and 75% for infants (8 weeks, 14, and 18 weeks of age), suggesting that this vaccine is appropriate for use in a birth dose vaccination schedule [17]. Strategies including changes in vaccine scheduling, administration of probiotics, antibiotics, or immunomodulatory drugs, and development of novel vaccine formulations may further improve rotavirus vaccine performance [69]. However, it remains to be seen whether improved immune responses will translate into improved CoPs.
Non-replicating rotavirus vaccines
P2-VP8*-based recombinant rotavirus vaccines (RecVs)
It has been shown that protection against rotavirus infection can be mediated by nAbs that target epitopes on the VP7, VP5*, and VP8* proteins [125, 163]. Therefore, these proteins are candidate antigens for the development of improved, next-generation, broadly effective rotavirus vaccines [107, 125]. In this context, the results of a recent study showed that VP8* fused with the P2 epitope of tetanus toxin (so-called P2-VP8*; a non-replicating, parenteral vaccine) was capable of inducing anti-rotavirus nAbs with homotypic protection characteristics [66], i.e., they were protective only against the rotavirus genotypes included in the vaccine formulation. More recently, to cope with this shortcoming and to induce significant heterotypic immunity, a trivalent P2-VP8*-P[8]/P[6]/P[4] vaccine was developed (numbers in brackets indicate the included genotypes) [76, 117]. The results of human trials in South African adults, children, and infants showed that this vaccine induced high levels of anti-P2-VP8* IgG and nAbs against three different P-type antigens [78, 79]. However, the proportion of infants with an anti-P2-VP8 IgA seroresponse to each P-type antigen was only between 20% and 34% [79]. It remains to be seen whether Abs to the trivalent P2-VP8 subunit vaccine are capable of protecting children against infection and diarrhea from increasingly variable homologous and heterologous rotavirus strains. More recently, several mRNA-based P2-VP8 vaccines have been developed and evaluated in mice, guinea pigs, and gnotobiotic pigs [33]. Induction of high levels of anti-P[8] IgG and virus-neutralizing antibodies against both homotypic P[8] and heterotypic P[4] and P[6] rotavirus strains was observed in the vaccinated animals [33]. It should be noted that almost all human rotavirus G types have been detected in combination with P[8], P[4], or P[6] specificity. Therefore single or multivalent formulations with two or more of the P[8], P[4], and P[6] VP8* proteins (VP8*-P[8]/P[4]/P[6]) might provide pan-antigenic coverage of almost all G (VP7) types and confer cross-neutralizing protection against the most common rotavirus genotypes.
There are ongoing prime/boost vaccination studies using oral and parenteral non-replicating rotavirus vaccines. In this context, immunization with one dose of the oral Rotarix vaccine (prime) followed by one dose (boost) of the trivalent nanoparticle vaccine (S-VP8*P [8]/P[4]/P[6] nanoparticles consisting of the S domain of norovirus VP1 and rotavirus VP8*) was shown to be capable of eliciting high titers of virus-specific neutralizing IgG and IgA Abs [33, 83].
It should be noted that oral vaccines replicate in the gut and induce an intestinal mucosal IgA response. Therefore, it is logical to consider that non-replicating parenteral rotavirus vaccines might use other pathways of protection and thus have different CoPs than their live oral vaccine counterparts. Of particular note, it has been shown that some of the IgA Abs in serum contain a secretory component that might be derived from the intestine via “spillover”. This observation might account for the correlation of rotavirus-specific IgA levels in serum with protection from disease [7]. For parenteral vaccines, however, IgG rather than IgA might be a suitable marker of immunogenicity and a CoP. In this context, it has been shown that transplacental-derived IgG protects infants from rotavirus disease and interferes with live oral rotavirus vaccine uptake, while hyperimmune serum protects non-human primates against rotavirus challenge [133]. Serum IgG has also been shown to protect against viral infections in the lung and intestinal lumen due to its ability to cross epithelial barriers by receptor-mediated transcytosis [31, 143]. Future studies might clarify the role of neutralizing Abs and key immunogen(s) responsible for broad and durable protection.
VP6-based RecVs
It has been suggested that Abs targeting the VP6 protein of the middle capsid layer might play a significant role in protection from rotavirus infection by inhibiting virus replication [29, 162]. VP6-specific Abs (which are elicited at high titers in the course of natural infection/vaccination) are capable of protecting rotavirus-infected mice via passive transfer [27, 63], while immunization with VP6-based vaccines also induces or enhances protective immunity [71, 105]. Recently, parenteral and/or mucosal immunization of mice with a VP6 oligomeric subunit preparation was shown to provide partial protection against rotavirus challenge [172]. In addition to being highly immunogenic, VP6 has several other useful characteristics that could allow it to be used in adjuvants, immunological carriers, and drug-delivery vehicles and also as a scaffold for production of valuable nano-biomaterials [158]. Moreover, VP6-specific llama-derived nanobodies have been shown to have extensive cross-neutralizing activity that protects neonatal mice from rotavirus-associated diarrhea [28, 113]. Similarly, orally administered rotavirus VP6-specific nanobodies have been shown to be effective against rotavirus-induced diarrhea in neonatal pigs [172]. These findings highlight the potential value of broadly neutralizing VP6-specific nanobodies as a treatment that might complement or be used as an alternative to the current strain-specific rotavirus vaccines [172]. It has been shown that Abs elicited against VP6 during natural infection of mice and humans are of the IgA and IgG isotypes [94] and that natural infection and vaccination induce similar levels of serum IgA Abs [106]. However, results of a more recent study indicated that neutralization by VP6-specific IgG was far more effective than neutralization by VP6-specific IgA [29]. These results suggest that rotavirus VP6 Abs may play an important role as a potential CoP and suggest that VP6 might be useful as a vaccine antigen.
VP6-NSP4-based RecVs
The rotavirus nonstructural glycoprotein 4 (NSP4) is a viral enterotoxin that plays important roles in rotavirus pathogenesis. There is a high seroconversion rate for induction of anti-NSP4 Abs following natural rotavirus infection, with a heterotypic response detectable in 48% of people infected [181]. These observations suggest that anti-NSP4 Abs might be CoPs in rotavirus-induced diarrhea. Abs raised against NSP4 are broadly reactive and might prevent diarrhea caused by various rotavirus genotypes [145, 181, 193]. Therefore, despite being a relatively weak immunogen, NSP4 has been used in several studies as a target Ag for development of rotavirus vaccines [2, 193]. Recently, it was reported that a combination of recombinant rotavirus VP6 nanospheres (VP6S) and NSP4 proteins formulated in aluminum hydroxide adjuvant elicited higher levels of anti-NSP4 Abs in mice than NSP4 alone [4]. Thus, it appears that the immunogenicity of NSP4 can be enhanced by cost-effective strategies for the purpose of developing NAP4-based rotavirus subunit vaccines.
VLP-based vaccines
Virus-like particles (VLPs) have been investigated as rotavirus vaccine candidates in several studies [128, 157, 194]. Several VLP vaccine candidates based on the combination of VP2, VP4, VP6, and VP7, produced either in baculovirus-infected insect cells (Baylor College of Medicine) or using plant-based platforms (Mitsubishi Tanabe Pharma) have been developed [48, 50, 51, 90, 100]. In preclinical studies, these vaccine candidates induced production of a broad range of heterotypic and homotypic nAbs without any significant toxicity in animal models. Accordingly, a plant-based VLP vaccine (Ro-VLP) is currently being tested in a human clinical trial. The results show that intramuscular administration of this Ro-VLP vaccine to infants elicited a stronger IgG than IgA response in serum, and nAbs against rotavirus were elicited that protected vaccinated infants from disease [100]. Moreover, it has been shown that intramuscular administration of a live or inactivated rotavirus vaccine in an animal model (rabbits) is capable of inducing intestinal rotavirus-specific IgG and protecting rabbits from rotavirus infection [47]. In further support of a protective role of IgG, it has been shown that intravenous injection of sera with high rotavirus-specific IgG titers to non-human primates resulted in the transport of IgGs to the intestinal lumen to inhibit rotavirus infection [188]. These findings suggest that both parenteral immunization with rotavirus VLP vaccines and administration of oral rotavirus vaccines have the potential to contribute to protection against rotavirus infection through transudation or permeation of Abs (IgG) into the intestinal lumen.
Inactivated rotavirus vaccines
Although inactivated rotavirus vaccines (IRVs) can be safe and effective for prevention of rotavirus infection in children, no approved and licensed vaccines are available to date. The Centers for Disease Control and Prevention (CDC) of the United States recently developed a heat-inactivated whole-virus vaccine consisting of human rotavirus G1P[8] strain CDC-9. Pre-clinical studies showed that intramuscular administration of IRV CDC is able to induce IgG, IgA, and homotypic and heterotypic nAbs in serum and protection against rotavirus infection and acute gastroenteritis in animal models [173, 184, 185]. In addition, parenteral administration of this inactivated vaccine was also shown to induce mucosal immunity by promoting expression of the gut homing receptor LPAM-1 (integrin α4β7) on T and B cells in the spleen and intestinal mesenteric lymph nodes of vaccinated mice [146]. In support of this, it has also been shown that circulating T and B cells in children with rotavirus gastroenteritis express LPAM-1, while LPAM-1-expressing B cells secrete rotavirus-specific Abs [72, 87, 148]. However, no defined CoPs for LPAM-1 expression after either natural rotavirus infection or oral and parenteral rotavirus vaccination have been suggested.
Gut microbiome and CoPs against rotavirus infection
An antiviral effect of probiotics against rotavirus infection via mechanisms such as immune enhancement or modulation of intestinal microbiota (probiotic-related reductions in rotavirus gastroenteritis) has been proposed [3, 97]. Rotavirus-induced gastroenteritis has been shown to decrease the intestinal microbial diversity and composition, while recovery is associated with a return of the intestinal flora to that of the non-infected state [35, 171]. The significant role of the gut microbiome in immune responses that indirectly affect CoPs against rotavirus infection has mainly been demonstrated in rotavirus-infected/vaccinated animal models, such as gnotobiotic (Gn) piglets. Several clinical studies have suggested that the gut microbiota plays a role in the variation of rotavirus vaccine efficacy observed in different parts of the world. Although vaccine efficacy usually correlates with anti-rotavirus IgA levels, anti-rotavirus IgA is an imperfect CoP and may not necessarily reflect protection against clinically relevant disease. Furthermore, intestinal commensals such as Lactobacillus rhamnosus GG (LGG), L acidophilus, L. reuteri, and Bifidobacterium lactis Bb12 (Bb12), which regulate gut immunity, significantly enhance rotavirus vaccine immunogenicity and reduce the severity of gastroenteritis and the amount of viral shedding [10, 80, 92, 136, 182, 195, 196]. These observations support further exploration of microbiome manipulation as a way of improving rotavirus vaccine efficacy [81]. Since gut microbiota might indirectly affect the CoPs in rotavirus infection/vaccination, understanding the influence of the diversity and composition of the microbiome on gut immunity might lead to new treatments or vaccination approaches [97].
Conclusion
Although natural infection and rotavirus vaccination both induce anti-rotavirus immune responses, the mechanisms by which these immune responses contribute to long-term protection against rotavirus infection is not fully understood. In general, levels of rotavirus IgA and homotypic and heterotypic nAbs in serum, elicited by natural infection might protect children from later infections and thus might be considered CoPs in the context of natural infection. Since oral rotavirus vaccination failures seem to be correlated with lower anti-rotavirus IgA levels in serum, the level of IgA induced by vaccination might also be considered a CoP in the context of vaccination. Moreover, the significant role of IgGs that transudate into the intestinal lumen and inhibit virus infection has also been highlighted by studies of parenteral rotavirus vaccines. In the case of oral rotavirus vaccines, differences in the gut microbiota have been found to be associated with rotavirus immunogenicity, and specific taxa of bacteria have been associated with a boosted rotavirus vaccine response. Accordingly, total circulating Abs and homotypic and heterotypic nAbs are associated, but not completely correlated, with protection. This implies a potential role of other immune mechanisms such as cross-reactive T cells in protection against rotavirus infection. Some predictors of protection may not be directly involved in the control or clearance of infection. Therefore, further studies on the molecular immunology of rotavirus vaccination and infection are needed to understand the interactions between the arms of the immune system and viral antigens and to fill the knowledge gap regarding correlates of protection against rotavirus infection.
Data availability
The data used to support the findings of this study are included in the article.
References
International Vaccine Access Center. http://view-hub.org. Accessed 03 Jan 2023.
Afchangi A, Arashkia A, Shahosseini Z, Jalilvand S, Marashi SM, Roohvand F, Mohajel N, Shoja Z (2018) Immunization of mice by rotavirus NSP4-VP6 fusion protein elicited stronger responses compared to VP6 alone. Viral Immunol 31:233–241
Afchangi A, Latifi T, Jalilvand S, Marashi SM, Shoja Z (2021) Combined use of lactic-acid-producing bacteria as probiotics and rotavirus vaccine candidates expressing virus-specific proteins. Adv Virol 166:995–1006
Afchangi A, Jalilvand S, Arashkia A, Latifi T, Farahmand M, Shirazi MMA, Nasab SDM, Marashi SM, Roohvand F, Shoja Z (2022) Co-administration of rotavirus nanospheres VP6 and NSP4 proteins enhanced the anti-NSP4 humoral responses in immunized mice. Microb Pathog 163:105405
Ali A, Kazi AM, Cortese MM, Fleming JA, Moon S, Parashar UD, Jiang B, McNeal MM, Steele D, Bhutta Z (2015) Impact of withholding breastfeeding at the time of vaccination on the immunogenicity of oral rotavirus vaccine—a randomized trial. PLoS ONE 10:e0127622
Amin AB, Tate JE, Waller LA, Lash TL, Lopman BA (2023) Monovalent rotavirus vaccine efficacy against different rotavirus genotypes: a pooled analysis of phase II and III Trial data. Clin Infect Dis 76:e1150–e1156
Angel J, Franco MA, Greenberg HB (2007) Rotavirus vaccines: recent developments and future considerations. Nat Rev Microbiol 5:529–539
Angel J, Steele AD, Franco MA (2014) Correlates of protection for rotavirus vaccines: possible alternative trial endpoints, opportunities, and challenges. Hum Vaccin Immunother 10:3659–3671
Armah GE, Sow SO, Breiman RF, Dallas MJ, Tapia MD, Feikin DR, Binka FN, Steele AD, Laserson KF, Ansah NA (2010) Efficacy of pentavalent rotavirus vaccine against severe rotavirus gastroenteritis in infants in developing countries in sub-Saharan Africa: a randomised, double-blind, placebo-controlled trial. The Lancet 376:606–614
Azevedo MP, Vlasova AN, Saif LJ (2013) Human rotavirus virus-like particle vaccines evaluated in a neonatal gnotobiotic pig model of human rotavirus disease. Expert Rev Vaccines 12:169–181
Baker JM, Tate JE, Leon J, Haber MJ, Pitzer VE, Lopman BA (2020) Postvaccination serum antirotavirus immunoglobulin A as a correlate of protection against rotavirus gastroenteritis across settings. J Infect Dis 222:309–318
Bennett A, Pollock L, Jere KC, Pitzer VE, Lopman B, Bar-Zeev N, Iturriza-Gomara M, Cunliffe NA (2020) Duration and density of fecal rotavirus shedding in vaccinated Malawian children with rotavirus gastroenteritis. J Infect Dis 222:2035–2040
Bergman H, Henschke N, Hungerford D, Pitan F, Ndwandwe D, Cunliffe N, Soares-Weiser K (2021) Vaccines for preventing rotavirus diarrhoea: vaccines in use. Cochrane Database Syst Rev 2019:CD008521
Bernstein DI, Sander DS, Smith VE, Schiff GM, Ward RL (1991) Protection from rotavirus reinfection: 2-year prospective study. J Infect Dis 164:277–283
Bhandari N, Rongsen-Chandola T, Bavdekar A, John J, Antony K, Taneja S, Goyal N, Kawade A, Kang G, Rathore SS, Juvekar S, Muliyil J, Arya A, Shaikh H, Abraham V, Vrati S, Proschan M, Kohberger R, Thiry G, Glass R, Greenberg HB, Curlin G, Mohan K, Harshavardhan GV, Prasad S, Rao TS, Boslego J, Bhan MK, India Rotavirus Vaccine G (2014) Efficacy of a monovalent human-bovine (116E) rotavirus vaccine in Indian infants: a randomised, double-blind, placebo-controlled trial. Lancet 383:2136–2143
Bines JE, Danchin M, Jackson P, Handley A, Watts E, Lee KJ, West A, Cowley D, Chen MY, Barnes GL, Justice F, Buttery JP, Carlin JB, Bishop RF, Taylor B, Kirkwood CD (2015) Safety and immunogenicity of RV3-BB human neonatal rotavirus vaccine administered at birth or in infancy: a randomised, double-blind, placebo-controlled trial. Lancet Infect Dis 15:1389–1397
Bines JE, At Thobari J, Satria CD, Handley A, Watts E, Cowley D, Nirwati H, Ackland J, Standish J, Justice F, Byars G, Lee KJ, Barnes GL, Bachtiar NS, Viska Icanervilia A, Boniface K, Bogdanovic-Sakran N, Pavlic D, Bishop RF, Kirkwood CD, Buttery JP, Soenarto Y (2018) Human neonatal rotavirus vaccine (RV3-BB) to target rotavirus from birth. N Engl J Med 378:719–730
Bishop RF, Barnes GL, Cipriani E, Lund JS (1983) Clinical immunity after neonatal rotavirus infection: a prospective longitudinal study in young children. N Engl J Med 309:72–76
Bishop RF, Bugg HC, Masendyez PJ, Lund JS, Gorrell RJ, Barnes GL (1996) Serum, fecal, and breast milk rotavirus antibodies as indices of infection in mother-infant pairs. J Infect Dis 174:S22–S29
Blutt SE, Conner ME (2007) Rotavirus: to the gut and beyond! Curr Opin Gastroenterol 23:39–43
Britto C, Alter G (2022) The next frontier in vaccine design: blending immune correlates of protection into rational vaccine design. Curr Opin Immunol 78:102234
Brüssow H, Benitez O, Uribe F, Sidoti J, Rosa K, Cravioto A (1993) Rotavirus-inhibitory activity in serial milk samples from Mexican women and rotavirus infections in their children during their first year of life. J Clin Microbiol 31:593–597
Burke RM, Groom HC, Naleway AL, Katz EM, Salas B, Mattison CP, Donald J, Tsaknaridis L, Biggs C, Bowen MD, Tate JE, Parashar UD, Schmidt M, Hall AJ (2021) Rotavirus vaccine is effective against rotavirus gastroenteritis resulting in outpatient care: results from the medically attended acute gastroenteritis (MAAGE) study. Clin Infect Dis 72:2000–2005
Burnett E, Jonesteller CL, Tate JE, Yen C, Parashar UD (2017) Global impact of rotavirus vaccination on childhood hospitalizations and mortality from diarrhea. J Infect Dis 215:1666–1672
Burnett E, Parashar UD, Tate JE (2020) Real-world effectiveness of rotavirus vaccines, 2006–19: a literature review and meta-analysis. Lancet Glob Health 8:e1195–e1202
Burnett E, Parashar UD, Tate JE (2020) Global impact of rotavirus vaccination on diarrhea hospitalizations and deaths among children <5 years old: 2006–2019. J Infect Dis 222:1731–1739
Burns JW, Siadat-Pajouh M, Krishnaney AA, Greenberg HB (1996) Protective effect of rotavirus VP6-specific IgA monoclonal antibodies that lack neutralizing activity. Science 272:104–107
Caddy S, Papa G, Borodavka A, Desselberger U (2021) Rotavirus research: 2014–2020. Virus Res 304:198499
Caddy SL, Vaysburd M, Wing M, Foss S, Andersen JT, O’Connell K, Mayes K, Higginson K, Iturriza-Gómara M, Desselberger U, Leo CJ (2020) Intracellular neutralisation of rotavirus by VP6-specific IgG. PLoS Pathog 16:e1008732
Cameron D, Bishop R, Veenstra A, Barnes G, Holmes I, Ruck B (1978) Pattern of shedding of two noncultivable viruses in stools of newborn babies. J Med Virol 2:7–13
Castro-Dopico T, Clatworthy MR (2019) IgG and Fcγ receptors in intestinal immunity and inflammation. Front Immunol 10:805
Chan J, Nirwati H, Triasih R, Bogdanovic-Sakran N, Soenarto Y, Hakimi M, Duke T, Buttery JP, Bines JE, Bishop RF (2011) Maternal antibodies to rotavirus: could they interfere with live rotavirus vaccines in developing countries? Vaccine 29:1242–1247
Chen J, Grow S, Iturriza-Gómara M, Hausdorff WP, Fix A, Kirkwood CD (2022) The challenges and opportunities of next-generation rotavirus vaccines: summary of an expert meeting with vaccine developers. Viruses 14:2565
Chen MY, Kirkwood CD, Bines J, Cowley D, Pavlic D, Lee KJ, Orsini F, Watts E, Barnes G, Danchin M (2017) Rotavirus specific maternal antibodies and immune response to RV3-BB neonatal rotavirus vaccine in New Zealand. Hum Vaccin Immunother 13:1126–1135
Chen S-Y, Tsai C-N, Lee Y-S, Lin C-Y, Huang K-Y, Chao H-C, Lai M-W, Chiu C-H (2017) Intestinal microbiome in children with severe and complicated acute viral gastroenteritis. Sci Rep 7:1–7
Chepngeno J, Amimo JO, Michael H, Raev SA, Jung K, Lee MV, Damtie D, Omwando A, Vlasova AN, Saif LJ (2023) Vitamin A deficiency and vitamin A supplementation affect innate and T cell immune responses to rotavirus A infection in a conventional sow model. Front Immunol 14:1188757
Cheuvart B, Neuzil KM, Steele AD, Cunliffe N, Madhi SA, Karkada N, Han HH, Vinals C (2014) Association of serum anti-rotavirus immunoglobulin A antibody seropositivity and protection against severe rotavirus gastroenteritis: analysis of clinical trials of human rotavirus vaccine. Hum Vaccin Immunother 10:505–511
Chiba S, Nakata S, Urasawa T, Urasawa S, Yokoyama T, Morita Y, Taniguchi K, Nakao T (1986) Protective effect of naturally acquired homotypic and heterotypic rotavirus antibodies. Lancet 328:417–421
Chiba S, Nakata S, Ukae S, Adachi N (1993) Virological and serological aspects of immune resistance to rotavirus gastroenteritis. Clin Infect Dis 16:S117–S121
Chilengi R, Simuyandi M, Beach L, Mwila K, Becker-Dreps S, Emperador DM, Velasquez DE, Bosomprah S, Jiang B (2016) Association of maternal immunity with rotavirus vaccine immunogenicity in Zambian infants. PLoS ONE 11:e0150100
Chilengi R, Mwila-Kazimbaya K, Chirwa M, Sukwa N, Chipeta C, Velu RM, Katanekwa N, Babji S, Kang G, McNeal MM, Meyer N, Gompana G, Hazra S, Tang Y, Flores J, Bhat N, Rathi N (2021) Immunogenicity and safety of two monovalent rotavirus vaccines, ROTAVAC® and ROTAVAC 5D® in Zambian infants. Vaccine 39:3633–3640
Choi AH, McNeal MM, Basu M, Flint JA, Stone SC, Clements JD, Bean JA, Poe SA, VanCott JL, Ward RL (2002) Intranasal or oral immunization of inbred and outbred mice with murine or human rotavirus VP6 proteins protects against viral shedding after challenge with murine rotaviruses. Vaccine 20:3310–3321
Clark HF, Bernstein DI, Dennehy PH, Offit P, Pichichero M, Treanor J, Ward RL, Krah DL, Shaw A, Dallas MJ (2004) Safety, efficacy, and immunogenicity of a live, quadrivalent human-bovine reassortant rotavirus vaccine in healthy infants. J Pediatr 144:184–190
Clarke E, Desselberger U (2015) Correlates of protection against human rotavirus disease and the factors influencing protection in low-income settings. Mucosal Immunol 8:1–17
Clemens J, Rao M, Ahmed F, Ward R, Huda S, Chakraborty J, Yunus M, Khan M, Ali M, Kay B (1993) Breast-feeding and the risk of life-threatening rotavirus diarrhea: prevention or postponement? Pediatrics 92:680–685
Clemens JD, Ward RL, Rao MR, Sack DA, Knowlton DR, van Loon FP, Huda S, McNeal M, Ahmed F, Schiff G (1992) Seroepidemiologic evaluation of antibodies to rotavirus as correlates of the risk of clinically significant rotavirus diarrhea in rural Bangladesh. J Infect Dis 165:161–165
Conner ME, Crawford SE, Barone C, Estes MK (1993) Rotavirus vaccine administered parenterally induces protective immunity. J Virol 67:6633–6641
Conner ME, Crawford S, Barone C, O’Neal C, Zhou Y-J, Fernandez F, Parwani A, Saif L, Cohen J, Estes M (1996) Rotavirus subunit vaccines. Viral gastroenteritis. Springer, Vienna, pp 199–206
Cowley D, Pavlic D, Bogdanovic-Sakran N, Boniface K, Kirkwood CD, Bines JE (2018) Serological responses to rotavirus NSP2 following administration of RV3-BB human neonatal rotavirus vaccine. Hum Vaccin Immunother 14:2082–2087
Crawford SE, Labbe M, Cohen J, Burroughs MH, Zhou Y-J, Estes MK (1994) Characterization of virus-like particles produced by the expression of rotavirus capsid proteins in insect cells. J Virol 68:5945–5952
Crawford SE, Estes MK, Ciarlet M, Barone C, O’Neal CM, Cohen J, Conner ME (1999) Heterotypic protection and induction of a broad heterotypic neutralization response by rotavirus-like particles. J Virol 73:4813–4822
Crawford SE, Ramani S, Tate JE, Parashar UD, Svensson L, Hagbom M, Franco MA, Greenberg HB, O’Ryan M, Kang G (2017) Rotavirus infection. Nat Rev Dis Prim 3:1–16
Cunliffe NA, Witte D, Ngwira BM, Todd S, Bostock NJ, Turner AM, Chimpeni P, Victor JC, Steele AD, Bouckenooghe A (2012) Efficacy of human rotavirus vaccine against severe gastroenteritis in Malawian children in the first two years of life: a randomized, double-blind, placebo controlled trial. Vaccine 30:A36–A43
Danchin MH, Bines JE, Watts E, Cowley D, Pavlic D, Lee KJ, Huque H, Kirkwood C, Nirwati H, At thobari J, Dewi Satria C, Soenarto Y, Oktaria V (2020) Rotavirus specific maternal antibodies and immune response to RV3-BB rotavirus vaccine in central java and yogyakarta, Indonesia. Vaccine 38:3235–3242
Desselberger U, Huppertz H-I (2011) Immune responses to rotavirus infection and vaccination and associated correlates of protection. J Infect Dis 203:188–195
Desselberger U (2017) Differences of rotavirus vaccine effectiveness by country: likely causes and contributing factors. Pathogens 6:65
Desselberger U (2018) The mammalian intestinal microbiome: composition, interaction with the immune system, significance for vaccine efficacy, and potential for disease therapy. Pathogens 7:57
Earle KA, Ambrosino DM, Fiore-Gartland A, Goldblatt D, Gilbert PB, Siber GR, Dull P, Plotkin SA (2021) Evidence for antibody as a protective correlate for COVID-19 vaccines. Vaccine 39:4423–4428
Ella R, Babji S, Ciarlet M, Blackwelder WC, Vadrevu KM (2019) A randomized, open-labelled, non-inferiority phase 4 clinical trial to evaluate the immunogenicity and safety of the live, attenuated, oral rotavirus vaccine, ROTAVAC® in comparison with a licensed rotavirus vaccine in healthy infants. Vaccine 37:4407–4413
Enya Y, Hiramatsu H, Ihira M, Suzuki R, Higashimoto Y, Funato Y, Kozawa K, Miura H, Miyata M, Kawamura Y (2023) Similarities in rotavirus vaccine viral shedding and immune responses in pairs of twins. Fujita Med J 9:253–258
Espinoza F, Paniagua M, Hallander H, Svensson L, Strannegård Ö (1997) Rotavirus infections in young Nicaraguan children. Pediatr Infect Dis J 16:564–571
Estes MK, Cohen J (1989) Rotavirus gene structure and function. Microbiol Rev 53:410–449
Feng N, Lawton JA, Gilbert J, Kuklin N, Vo P, Prasad BV, Greenberg HB (2002) Inhibition of rotavirus replication by a non-neutralizing, rotavirus VP6-specific IgA mAb. J Clin Investig 109:1203–1213
Fischer TK, Valentiner-Branth P, Steinsland H, Perch M, Santos G, Aaby P, Mølbak K, Sommerfelt H (2002) Protective immunity after natural rotavirus infection: a community cohort study of newborn children in Guinea-Bissau, west Africa. J Infect Dis 186:593–597
Franco MA, Angel J, Greenberg HB (2006) Immunity and correlates of protection for rotavirus vaccines. Vaccine 24:2718–2731
Gil MT, de Souza CO, Asensi M, Buesa J (2000) Homotypic protection against rotavirus-induced diarrhea in infant mice breast-fed by dams immunized with the recombinant VP8* subunit of the VP4 capsid protein. Viral Immunol 13:187–200
Gilbert PB, Montefiori DC, McDermott AB, Fong Y, Benkeser D, Deng W, Zhou H, Houchens CR, Martins K, Jayashankar L (2022) Immune correlates analysis of the mRNA-1273 COVID-19 vaccine efficacy clinical trial. Science 375:43–50
Gladstone BP, Ramani S, Mukhopadhya I, Muliyil J, Sarkar R, Rehman AM, Jaffar S, Gomara MI, Gray JJ, Brown DW (2011) Protective effect of natural rotavirus infection in an Indian birth cohort. N Engl J Med 365:337–346
Glass RI, Tate JE, Jiang B, Parashar U (2021) The rotavirus vaccine story: from discovery to the eventual control of rotavirus disease. J Infect Dis 224:S331–S342
Goldblatt D, Alter G, Crotty S, Plotkin SA (2022) Correlates of protection against SARS-CoV-2 infection and COVID-19 disease. Immunol Rev 310:6–26
Gonzalez A, Nguyen T, Azevedo M, Jeong K, Agarib F, Iosef C, Chang K, Lovgren-Bengtsson K, Morein B, Saif LJ (2004) Antibody responses to human rotavirus (HRV) in gnotobiotic pigs following a new prime/boost vaccine strategy using oral attenuated HRV priming and intranasal VP2/6 rotavirus-like particle (VLP) boosting with ISCOM. Clin Exp Immunol 135:361–372
Gonzalez AM, Jaimes MC, Cajiao I, Rojas OL, Cohen J, Pothier P, Kohli E, Butcher EC, Greenberg HB, Angel J (2003) Rotavirus-specific B cells induced by recent infection in adults and children predominantly express the intestinal homing receptor α4β7. Virology 305:93–105
González R, Franco M, Sarmiento L, Romero M, Schael IP (2005) Serum IgA levels induced by rotavirus natural infection, but not following immunization with the RRV-TV vaccine (Rotashield), correlate with protection. J Med Virol 76:608–612
Green K, Kapikian AZ (1992) Identification of VP7 epitopes associated with protection against human rotavirus illness or shedding in volunteers. J Virol 66:548–553
Green KY, Taniguchi K, Mackow ER, Kapikian AZ (1990) Homotypic and heterotypic epitope-specific antibody responses in adult and infant rotavirus vaccinees: implications for vaccine development. J Infect Dis 161:667–679
Groome M, Fairlie L, Morrison J, Fix A, Koen A, Masenya M, Page N, Jose L, Madhi S, McNeal M (2018) Safety and immunogenicity of a parenteral P2-VP8 subunit rotavirus vaccine. In: International rotavirus symposium Minsk, Belarus
Groome MJ, Moon S-S, Velasquez D, Jones S, Koen A, Nv N, Jiang B, Parashar UD, Madhi SA (2014) Effect of breastfeeding on immunogenicity of oral live-attenuated human rotavirus vaccine: a randomized trial in HIV-uninfected infants in Soweto, South Africa. Bull World Health Organ 92:238–245
Groome MJ, Koen A, Fix A, Page N, Jose L, Madhi SA, McNeal M, Dally L, Cho I, Power M (2017) Safety and immunogenicity of a parenteral P2-VP8-P [8] subunit rotavirus vaccine in toddlers and infants in South Africa: a randomised, double-blind, placebo-controlled trial. Lancet Infect Dis 17:843–853
Groome MJ, Fairlie L, Morrison J, Fix A, Koen A, Masenya M, Jose L, Madhi SA, Page N, McNeal M (2020) Safety and immunogenicity of a parenteral trivalent P2-VP8 subunit rotavirus vaccine: a multisite, randomised, double-blind, placebo-controlled trial. Lancet Infect Dis 20:851–863
Harris VC (2018) The significance of the intestinal microbiome for vaccinology: from correlations to therapeutic applications. Drugs 78:1063–1072
Harris VC, Haak BW, Handley SA, Jiang B, Velasquez DE, Hykes BL, Droit L, Berbers GAM, Kemper EM, van Leeuwen EMM, Boele van Hensbroek M, Wiersinga WJ (2018) Effect of antibiotic-mediated microbiome modulation on rotavirus vaccine immunogenicity: a human, randomized-control proof-of-concept trial. Cell Host Microbe 24:197-207.e194
Henschke N, Bergman H, Hungerford D, Cunliffe N, Grais R, Kang G, Parashar U, Wang S, Neuzil K (2022) The efficacy and safety of rotavirus vaccines in countries in Africa and Asia with high child mortality. Vaccine 40:1707–1711
Hensley C, Nyblade C, Zhou P, Parreño V, Ramesh A, Frazier A, Frazier M, Garrison S, Fantasia-Davis A, Cai R (2023) Combined live oral priming and intramuscular boosting regimen with Rotarix® and a nanoparticle-based trivalent rotavirus vaccine evaluated in gnotobiotic pig models of G4P [6] and G1P [8] human rotavirus infection. Vaccines 11:927
Hjelt K, Paerregaard A, Nielsen OH, Krasilnikoff PA, Grauballe PC (1987) Protective effect of preexisting rotavirus-specific immunoglobulin A against naturally acquired rotavirus infection in children. J Med Virol 21:39–47
Holmgren J, Parashar UD, Plotkin S, Louis J, Ng S-P, Desauziers E, Picot V, Saadatian-Elahi M (2017) Correlates of protection for enteric vaccines. Vaccine 35:3355–3363
Isanaka S, Langendorf C, McNeal MM, Meyer N, Plikaytis B, Garba S, Sayinzoga-Makombe N, Soumana I, Guindo O, Makarimi R (2021) Rotavirus vaccine efficacy up to 2 years of age and against diverse circulating rotavirus strains in Niger: extended follow-up of a randomized controlled trial. PLoS Med 18:e1003655
MaC J, Rojas OL, Kunkel EJ, Lazarus NH, Soler D, Butcher EC, Bass D, Angel J, Franco MA, Greenberg HB (2004) Maturation and trafficking markers on rotavirus-specific B cells during acute infection and convalescence in children. J Virol 78:10967–10976
Jaimes MC, Rojas OL, González AM, Cajiao I, Charpilienne A, Pothier P, Kohli E, Greenberg HB, Franco MA, Angel J (2002) Frequencies of virus-specific CD4+ and CD8+ T lymphocytes secreting gamma interferon after acute natural rotavirus infection in children and adults. J Virol 76:4741–4749
Jayashree S, Bhan M, Kumar R, Bhandari N, Sazawal S (1988) Protection against neonatal rotavirus infection by breast milk antibodies and trypsin inhibitors. J Med Virol 26:333–338
Jiang B, Estes MK, Barone C, Barniak V, O’Neal CM, Ottaiano A, Madore HP, Conner ME (1999) Heterotypic protection from rotavirus infection in mice vaccinated with virus-like particles. Vaccine 17:1005–1013
Jonesteller CL, Burnett E, Yen C, Tate JE, Parashar UD (2017) Effectiveness of rotavirus vaccination: a systematic review of the first decade of global postlicensure data, 2006–2016. Clin Infect Dis 65:840–850
Kandasamy S, Chattha KS, Vlasova AN, Rajashekara G, Saif LJ (2014) Lactobacilli and Bifidobacteria enhance mucosal B cell responses and differentially modulate systemic antibody responses to an oral human rotavirus vaccine in a neonatal gnotobiotic pig disease model. Gut microbes 5:639–651
Kapikian A, Wyatt R, Levine M, Yolken R, VanKirk D, Dolin R, Greenberg H, Chanock R (1983) Oral administration of human rotavirus to volunteers: induction of illness and correlates of resistance. J Infect Dis 147:95–106
Kavanagh O, Zeng X-L, Ramani S, Mukhopadhya I, Crawford SE, Kang G, Estes MK (2013) A time-resolved immunoassay to measure serum antibodies to the rotavirus VP6 capsid protein. J Virol Methods 189:228–231
Kawamura N, Tokoeda Y, Oshima M, Okahata H, Tsutsumi H, Van Doorn LJ, Muto H, Smolenov I, Suryakiran P, Han HH (2011) Efficacy, safety and immunogenicity of RIX4414 in Japanese infants during the first two years of life. Vaccine 29:6335–6341
Khoury DS, Cromer D, Reynaldi A, Schlub TE, Wheatley AK, Juno JA, Subbarao K, Kent SJ, Triccas JA, Davenport MP (2021) Neutralizing antibody levels are highly predictive of immune protection from symptomatic SARS-CoV-2 infection. Nat Med 27:1205–1211
Kim AH, Hogarty MP, Harris VC, Baldridge MT (2021) The complex interactions between rotavirus and the gut microbiota. Front Cell Infect Microbiol 10:586751
Kotloff KL (2017) The burden and etiology of diarrheal illness in developing countries. Pediatr Clin N Am 64:799–814
Kulkarni PS, Desai S, Tewari T, Kawade A, Goyal N, Garg BS, Kumar D, Kanungo S, Kamat V, Kang G (2017) A randomized Phase III clinical trial to assess the efficacy of a bovine-human reassortant pentavalent rotavirus vaccine in Indian infants. Vaccine 35:6228–6237
Kurokawa N, Robinson MK, Bernard C, Kawaguchi Y, Koujin Y, Koen A, Madhi S, Polasek TM, McNeal M, Dargis M (2021) Safety and immunogenicity of a plant-derived rotavirus-like particle vaccine in adults, toddlers and infants. Vaccine 39:5513–5523
Laban NM, Goodier MR, Bosomprah S, Simuyandi M, Chisenga C, Chilyabanyama ON, Chilengi R (2022) T-cell responses after rotavirus infection or vaccination in children: a systematic review. Viruses 14:459
Lamberti LM, Ashraf S, Walker CLF, Black RE (2016) A systematic review of the effect of rotavirus vaccination on diarrhea outcomes among children younger than 5 years. Pediatr Infect Dis J 35:992–998
Lanata CF, Fischer-Walker CL, Olascoaga AC, Torres CX, Aryee MJ, Black RE, Organization CHERGotWH, UNICEF (2013) Global causes of diarrheal disease mortality in children< 5 years of age: a systematic review. PLoS ONE 8:e72788
Langel S, Steppe J, Chang J, Travieso T, Webster H, Otero C, Williamson L, Crowe J, Greenberg H, Wu H, Hornik C, Mansouri K, Edwards R, Stalls V, Acharya P, Blasi M, Permar S (2021) Protective transfer: maternal passive immunization with a rotavirus-neutralizing dimeric IgA protects against rotavirus disease in suckling neonates. bioRxiv: 2021.2009.2021.461116
Lappalainen S, Pastor AR, Tamminen K, López-Guerrero V, Esquivel-Guadarrama F, Palomares LA, Vesikari T, Blazevic V (2014) Immune responses elicited against rotavirus middle layer protein VP6 inhibit viral replication in vitro and in vivo. Hum Vaccin Immunother 10:2039–2047
Lappalainen S, Blazevic V, Malm M, Vesikari T (2017) Rotavirus vaccination and infection induce VP6-specific IgA responses. J Med Virol 89:239–245
Latifi T, Jalilvand S, Golsaz-Shirazi F, Arashkia A, Kachooei A, Afchangi A, Zafarian S, Roohvand F, Shoja Z (2023) Characterization and immunogenicity of a novel chimeric hepatitis B core-virus like particles (cVLPs) carrying rotavirus VP8* protein in mice model. Virology 588:109903
Lau Y-L, Nelson EAS, Poon K-H, Chan PK, Chiu S, Sung R, Leung CW, Ng D, Ma YM, Chan D (2013) Efficacy, safety and immunogenicity of a human rotavirus vaccine (RIX4414) in Hong Kong children up to three years of age: a randomized, controlled trial. Vaccine 31:2253–2259
Lazarus RP, John J, Shanmugasundaram E, Rajan AK, Thiagarajan S, Giri S, Babji S, Sarkar R, Kaliappan PS, Venugopal S (2018) The effect of probiotics and zinc supplementation on the immune response to oral rotavirus vaccine: a randomized, factorial design, placebo-controlled study among Indian infants. Vaccine 36:273–279
Lee B, Carmolli M, Dickson DM, Colgate ER, Diehl SA, Uddin MI, Islam S, Hossain M, Rafique TA, Bhuiyan TR, Alam M, Nayak U, Mychaleckyj JC, McNeal MM, Petri WA, Qadri F, Haque R, Kirkpatrick BD (2018) Rotavirus-specific immunoglobulin A responses are impaired and serve as a suboptimal correlate of protection among infants in Bangladesh. Clin Infect Dis 67:186–192
Lee B (2021) Update on rotavirus vaccine underperformance in low-to middle-income countries and next-generation vaccines. Hum Vaccin Immunother 17:1787–1802
Madhi SA, Kirsten M, Louw C, Bos P, Aspinall S, Bouckenooghe A, Neuzil KM, Steele AD (2012) Efficacy and immunogenicity of two or three dose rotavirus-vaccine regimen in South African children over two consecutive rotavirus-seasons: a randomized, double-blind, placebo-controlled trial. Vaccine 30:A44–A51
Maffey L, Vega CG, Miño S, Garaicoechea L, Parreño V (2016) Anti-VP6 VHH: an experimental treatment for rotavirus A-associated disease. PLoS ONE 11:e0162351
Malamba-Banda C, Mhango C, Benedicto-Matambo P, Mandolo JJ, Chinyama E, Kumwenda O, Barnes KG, Cunliffe NA, Iturriza-Gomara M, Jambo KC (2023) Acute rotavirus infection is associated with the induction of circulating memory CD4+ T cell subsets. Sci Rep 13:9001
Malm M, Hyöty H, Knip M, Vesikari T, Blazevic V (2019) Development of T cell immunity to norovirus and rotavirus in children under five years of age. Sci Rep 9:1–9
Matson DO, O’Ryan ML, Herrera I, Pickering LK, Estes MK (1993) Fecal antibody responses to symptomatic and asymptomatic rotavirus infections. J Infect Dis 167:577–583
McAdams D, Estrada M, Holland D, Singh J, Sawant N, Hickey JM, Kumar P, Plikaytis B, Joshi SB, Volkin DB (2022) Concordance of in vitro and in vivo measures of non-replicating rotavirus vaccine potency. Vaccine 40:5069–5078
McNeal MM, Rae MN, Ward RL (1997) Evidence that resolution of rotavirus infection in mice is due to both CD4 and CD8 cell-dependent activities. J Virol 71:8735–8742
McNeal MM, VanCott JL, Choi AH, Basu M, Flint JA, Stone SC, Clements JD, Ward RL (2002) CD4 T cells are the only lymphocytes needed to protect mice against rotavirus shedding after intranasal immunization with a chimeric VP6 protein and the adjuvant LT(R192G). J Virol 76:560–568
Metrics IfH, Evaluation (2017) Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2016 (GBD 2016) results. Institute for Health Metrics and Evaluation, Seattle
Middleton BF, Danchin M, Cunliffe NA, Jones MA, Boniface K, Kirkwood CD, Gallagher S, Kirkham L-A, Granland C, McNeal M (2023) Histo-blood group antigen profile of Australian Aboriginal children and seropositivity following oral rotavirus vaccination. Vaccine 41:3579–3583
Mo Z, Ma X, Luo P, Mo Y, Kaplan SS, Shou Q, Zheng M, Hille DA, Arnold BA, Liao X (2019) Immunogenicity of pentavalent rotavirus vaccine in Chinese infants. Vaccine 37:1836–1843
Moon S-S, Wang Y, Shane AL, Nguyen T, Ray P, Dennehy P, Baek LJ, Parashar U, Glass RI, Jiang B (2010) Inhibitory effect of breast milk on infectivity of live oral rotavirus vaccines. Pediatr Infect Dis J 29:919
Moon S-S, Tate JE, Ray P, Dennehy PH, Archary D, Coutsoudis A, Bland R, Newell M-L, Glass RI, Parashar U (2013) Differential profiles and inhibitory effect on rotavirus vaccines of nonantibody components in breast milk from mothers in developing and developed countries. Pediatr Infect Dis J 32:863
Nair N, Feng N, Blum LK, Sanyal M, Ding S, Jiang B, Sen A, Morton JM, He X-S, Robinson WH, Greenberg HB (2017) VP4- and VP7-specific antibodies mediate heterotypic immunity to rotavirus in humans. Sci Transl Med 9:eaam5434
Nordgren J, Sharma S, Bucardo F, Nasir W, Gunaydin G, Ouermi D, Nitiema LW, Becker-Dreps S, Simpore J, Hammarstrom L, Larson G, Svensson L (2014) Both Lewis and secretor status mediate susceptibility to rotavirus infections in a rotavirus genotype-dependent manner. Clin Infect Dis 59:1567–1573
Novak D, Svennerholm AM (2015) A comparison of seasonal variations in rotavirus antibodies in the breast milk of Swedish and Bangladeshi mothers. Acta Paediatr 104:247–251
O’Neal CM, Crawford SE, Estes MK, Conner ME (1997) Rotavirus virus-like particles administered mucosally induce protective immunity. J Virol 71:8707–8717
O’Ryan ML, Matson DO, Estes MK, Pickering LK (1994) Anti-rotavirus G type-specific and isotype-specific antibodies in children with natural rotavirus infections. J Infect Dis 169:504–511
O’Ryan ML, Matson DO, Estes MK, Pickering LK (1994) Acquisition of serum isotype-specific and G type-specific antirotavirus antibodies among children in day care centers. Pediatr Infect Dis J 13:890–895
Offit P (1994) Immunologic determinants of protection against rotavirus disease. Curr Top Microbiol Immunol 185:229–254
Offit PA, Blavat G (1986) Identification of the two rotavirus genes determining neutralization specificities. J Virol 57:376–378
Otero CE, Langel SN, Blasi M, Permar SR (2020) Maternal antibody interference contributes to reduced rotavirus vaccine efficacy in developing countries. PLoS Pathog 16:e1009010
Parker EP, Ramani S, Lopman BA, Church JA, Iturriza-Gomara M, Prendergast AJ, Grassly NC (2018) Causes of impaired oral vaccine efficacy in developing countries. Future Microbiol 13:97–118
Parker EPK, Praharaj I, Zekavati A, Lazarus RP, Giri S, Operario DJ, Liu J, Houpt E, Iturriza-Gomara M, Kampmann B, John J, Kang G, Grassly NC (2018) Influence of the intestinal microbiota on the immunogenicity of oral rotavirus vaccine given to infants in south India. Vaccine 36:264–272
Parreno V, Bai M, Liu F, Jing J, Olney E, Li G, Wen K, Yang X, Castellucc TB, Kocher JF (2022) Probiotic as adjuvant significantly improves protection of the Lanzhou trivalent rotavirus vaccine against heterologous challenge in a gnotobiotic pig model of human rotavirus infection and disease. Vaccines 10:1529
Patel M, Glass RI, Jiang B, Santosham M, Lopman B, Parashar U (2013) A systematic review of anti-rotavirus serum IgA antibody titer as a potential correlate of rotavirus vaccine efficacy. J Infect Dis 208:284–294
Plotkin SA, Gilbert PB (2012) Nomenclature for immune correlates of protection after vaccination. Clin Infect Dis 54:1615–1617
Plotkin SA (2023) Recent updates on correlates of vaccine-induced protection. Front Immunol 13:1081107
Pollock L, Bennett A, Jere KC, Mandolo J, Dube Q, Bar-Zeev N, Heyderman RS, Cunliffe NA, Iturriza-Gomara M (2022) Plasma rotavirus-specific IgA and risk of rotavirus vaccine failure in infants in Malawi. Clin Infect Dis 75:41–46
Premkumar P, Lopman B, Ramani S, Paul A, Gladstone B, Muliyil J, Mukhopadhya I, Parashar U, Kang G (2014) Association of serum antibodies with protection against rotavirus infection and disease in South Indian children. Vaccine 32:A55–A61
Qin L, Gilbert PB, Corey L, McElrath MJ, Self SG (2007) A framework for assessing immunological correlates of protection in vaccine trials. J Infect Dis 196:1304–1312
Rath T, Kuo TT, Baker K, Qiao S-W, Kobayashi K, Yoshida M, Roopenian D, Fiebiger E, Lencer WI, Blumberg RS (2013) The immunologic functions of the neonatal Fc receptor for IgG. J Clin Immunol 33:9–17
Rathi N, Desai S, Kawade A, Venkatramanan P, Kundu R, Lalwani SK, Dubey A, Rao JV, Narayanappa D, Ghildiyal R (2018) A Phase III open-label, randomized, active controlled clinical study to assess safety, immunogenicity and lot-to-lot consistency of a bovine-human reassortant pentavalent rotavirus vaccine in Indian infants. Vaccine 36:7943–7949
Ray P, Malik J, Singh RK, Bhatnagar S, Bahl R, Kumar R, Bhan MK (2003) Rotavirus nonstructural protein NSP4 induces heterotypic antibody responses during natural infection in children. J Infect Dis 187:1786–1793
Resch TK, Wang Y, Moon S-S, Joyce J, Li S, Prausnitz M, Jiang B (2018) Inactivated rotavirus vaccine by parenteral administration induces mucosal immunity in mice. Sci Rep 8:561
Rojas A, Boher Y, Guntinas M, Perez-Schael I (1995) Homotypic immune response to primary infection with rotavirus serotype G1. J Med Virol 47:404–409
Rojas OL, González AM, González R, Pérez-Schael I, Greenberg HB, Franco MA, Angel J (2003) Human rotavirus specific T cells: quantification by ELISPOT and expression of homing receptors on CD4+ T cells. Virology 314:671–679
Rongsen-Chandola T, Strand TA, Goyal N, Flem E, Rathore SS, Arya A, Winje BA, Lazarus R, Shanmugasundaram E, Babji S (2014) Effect of withholding breastfeeding on the immune response to a live oral rotavirus vaccine in North Indian infants. Vaccine 32:A134–A139
Ruiz-Palacios GM, Perez-Schael I, Velazquez FR, Abate H, Breuer T, Clemens SC, Cheuvart B, Espinoza F, Gillard P, Innis BL, Cervantes Y, Linhares AC, Lopez P, Macias-Parra M, Ortega-Barria E, Richardson V, Rivera-Medina DM, Rivera L, Salinas B, Pavia-Ruz N, Salmeron J, Ruttimann R, Tinoco JC, Rubio P, Nunez E, Guerrero ML, Yarzabal JP, Damaso S, Tornieporth N, Saez-Llorens X, Vergara RF, Vesikari T, Bouckenooghe A, Clemens R, De Vos B, O’Ryan M, Human Rotavirus Vaccine Study G (2006) Safety and efficacy of an attenuated vaccine against severe rotavirus gastroenteritis. N Engl J Med 354:11–22
Saluja T, Palkar S, Misra P, Gupta M, Venugopal P, Sood AK, Dhati RM, Shetty A, Dhaded SM, Agarkhedkar S (2017) Live attenuated tetravalent (G1–G4) bovine-human reassortant rotavirus vaccine (BRV-TV): randomized, controlled phase III study in Indian infants. Vaccine 35:3575–3581
Santos SM, Ferreira TL, Quintal VS, Carbonare SB, Tino-De-Franco M (2013) Milk from Brazilian women presents secretory IgA antibodies and neutralizes rotavirus G9P [5]. Jornal de pediatria 89:510–513
Segovia MG (2018) Human neonatal rotavirus vaccine (RV3-BB) to target rotavirus from birth. Acta Pediatrica Espanola 76:62–63
Settembre EC, Chen JZ, Dormitzer PR, Grigorieff N, Harrison SC (2011) Atomic model of an infectious rotavirus particle. EMBO J 30:408–416
Shaw RD, Fong KJ, Losonsky GA, Levine MM, Maldonado Y, Yolken R, Flores J, Kapikian AZ, Vo PT, Greenberg HB (1987) Epitope-specific immune responses to rotavirus vaccination. Gastroenterology 93:941–950
Shin S, Anh DD, Zaman K, Yunus M, Thiem VD, Azim T, Victor JC, Dallas MJ, Steele AD, Neuzil KM (2012) Immunogenicity of the pentavalent rotavirus vaccine among infants in two developing countries in Asia, Bangladesh and Vietnam. Vaccine 30:A106–A113
Shoja Z, Tagliamonte M, Jalilvand S, Mollaei-Kandelous Y, De Stradis A, Tornesello ML, Buonaguro FM, Buonaguro L (2015) Formation of self-assembled triple-layered rotavirus-like particles (tlRLPs) by constitutive co-expression of VP2, VP6, and VP7 in stably transfected high-five insect cell lines. J Med Virol 87:102–111
Shoja Z, Jalilvand S, Latifi T, Roohvand F (2022) Rotavirus VP6: involvement in immunogenicity, adjuvant activity, and use as a vector for heterologous peptides, drug delivery, and production of nano-biomaterials. Arch Virol 167:1013–1023
Sow SO, Tapia M, Haidara FC, Ciarlet M, Diallo F, Kodio M, Doumbia M, Dembélé RD, Traoré O, Onwuchekwa UU (2012) Efficacy of the oral pentavalent rotavirus vaccine in Mali. Vaccine 30:A71–A78
Superti F, Ammendolia M, Valenti P, Seganti L (1997) Antirotaviral activity of milk proteins: lactoferrin prevents rotavirus infection in the enterocyte-like cell line HT-29. Med Microbiol Immunol 186:83–91
Svensson L, Sheshberadaran H, Vene S, Norrby E, Grandien M, Wadell G (1987) Serum antibody responses to individual viral polypeptides in human rotavirus infections. J Gen Virol 68:643–651
Svensson L, Sheshberadaran H, Vesikari T, Norrby E, Wadell G (1987) Immune response to rotavirus polypeptides after vaccination with heterologous rotavirus vaccines (RIT 4237, RRV-1). J Gen Virol 68:1993–1999
Taniguchi K, Urasawa T, Kobayashi N, Ahmed M, Adachi N, Chiba S, Urasawa S (1991) Antibody response to serotype-specific and cross-reactive neutralization epitopes on VP4 and VP7 after rotavirus infection or vaccination. J Clin Microbiol 29:483–487
Tapia MD, Armah G, Breiman RF, Dallas MJ, Lewis KD, Sow SO, Rivers SB, Levine MM, Laserson KF, Feikin DR (2012) Secondary efficacy endpoints of the pentavalent rotavirus vaccine against gastroenteritis in sub-Saharan Africa. Vaccine 30:A79–A85
Tate JE, Burton AH, Boschi-Pinto C, Parashar UD, Network WHOCGRS, Agocs M, Serhan F, de Oliveira L, Mwenda JM, Mihigo R (2016) Global, regional, and national estimates of rotavirus mortality in children< 5 years of age, 2000–2013. Clin Infect Dis 62:S96–S105
Thiem VD, Anh DD, Ha VH, Hien ND, Huong NT, Nga NT, Thang TC, McNeal MM, Meyer N, Pham HL, Huong NM, Gompana G, Cassels F, Tang Y, Flores J, Rathi N (2021) Safety and immunogenicity of two formulations of rotavirus vaccine in Vietnamese infants. Vaccine 39:4463–4470
Tino De Franco M, Vieira P, Santos S, Ferreira T, Araújo E, Quintal V, Carbonare SB (2013) Neutralizing activity and secretory IgA antibodies reactive with rotavirus SA-11 (serotype G3) in colostrum and milk from Brazilian women. Paediatr Int Child Health 33:102–107
Trang NV, Braeckman T, Lernout T, Hau VT, Anh LT, Luan LT, Van Damme P, Anh DD (2014) Prevalence of rotavirus antibodies in breast milk and inhibitory effects to rotavirus vaccines. Hum Vaccin Immunother 10:3681–3687
Tregnaghi MW, Abate HJ, Valencia A, Lopez P, Da Silveira TR, Rivera L, Medina DMR, Saez-Llorens X, Ayala SEG, De León T (2011) Human rotavirus vaccine is highly efficacious when coadministered with routine expanded program of immunization vaccines including oral poliovirus vaccine in Latin America. Pediatr Infect Dis J 30:e103–e108
Troeger C, Khalil IA, Rao PC, Cao S, Blacker BF, Ahmed T, Armah G, Bines JE, Brewer TG, Colombara DV (2018) Rotavirus vaccination and the global burden of rotavirus diarrhea among children younger than 5 years. JAMA Pediatr 172:958–965
Twitchell EL, Tin C, Wen K, Zhang H, Becker-Dreps S, Azcarate-Peril MA, Vilchez S, Li G, Ramesh A, Weiss M (2016) Modeling human enteric dysbiosis and rotavirus immunity in gnotobiotic pigs. Gut Pathog 8:1–18
Vega CG, Bok M, Vlasova AN, Chattha KS, Gómez-Sebastián S, Nuñez C, Alvarado C, Lasa R, Escribano JM, Garaicoechea LL (2013) Recombinant monovalent llama-derived antibody fragments (VHH) to rotavirus VP6 protect neonatal gnotobiotic piglets against human rotavirus-induced diarrhea. PLoS Pathog 9:e1003334
Velasquez DE, Wang Y, Jiang B (2015) Inactivated human rotavirus vaccine induces heterotypic antibody response: correction and development of IgG avidity assay. Hum Vaccin Immunother 11:531–533
Velasquez DE, Parashar U, Jiang B (2018) Decreased performance of live attenuated, oral rotavirus vaccines in low-income settings: causes and contributing factors. Expert Rev Vaccines 17:145–161
Velázquez FR, Matson DO, Calva JJ, Guerrero ML, Morrow AL, Carter-Campbell S, Glass RI, Estes MK, Pickering LK, Ruiz-Palacios GM (1996) Rotavirus infection in infants as protection against subsequent infections. N Engl J Med 335:1022–1028
Velázquez FR, Matson DO, Guerrero ML, Shults J, Calva JJ, Morrow AL, Glass RI, Pickering LK, Ruiz-Palacios GM (2000) Serum antibody as a marker of protection against natural rotavirus infection and disease. J Infect Dis 182:1602–1609
Vesikari T, Clark HF, Offit PA, Dallas MJ, DiStefano DJ, Goveia MG, Ward RL, Schodel F, Karvonen A, Drummond JE, DiNubile MJ, Heaton PM (2006) Effects of the potency and composition of the multivalent human-bovine (WC3) reassortant rotavirus vaccine on efficacy, safety and immunogenicity in healthy infants. Vaccine 24:4821–4829
Vesikari T, Matson DO, Dennehy P, Van Damme P, Santosham M, Rodriguez Z, Dallas MJ, Heyse JF, Goveia MG, Black SB (2006) Safety and efficacy of a pentavalent human–bovine (WC3) reassortant rotavirus vaccine. N Engl J Med 354:23–33
Vesikari T, Itzler R, Matson DO, Santosham M, Christie CD, Coia M, Cook JR, Koch G, Heaton P (2007) Efficacy of a pentavalent rotavirus vaccine in reducing rotavirus-associated health care utilization across three regions (11 countries). Int J Infect Dis 11:S29–S35
Vesikari T, Karvonen A, Prymula R, Schuster V, Tejedor J, Cohen R, Meurice F, Han H, Damaso S, Bouckenooghe A (2007) Efficacy of human rotavirus vaccine against rotavirus gastroenteritis during the first 2 years of life in European infants: randomised, double-blind controlled study. Lancet 370:1757–1763
Vizzi E, Calvino E, Gonzalez R, Perez-Schael I, Ciarlet M, Kang G, Estes MK, Liprandi F, Ludert JE (2005) Evaluation of serum antibody responses against the rotavirus nonstructural protein NSP4 in children after rhesus rotavirus tetravalent vaccination or natural infection. Clin Diagn Lab Immunol 12:1157–1163
Vlasova AN, Rajashekara G, Saif LJ (2018) Interactions between human microbiome, diet, enteric viruses and immune system: Novel insights from gnotobiotic pig research. Drug Discov Today Dis Models 28:95–103
Wandera EA, Mohammad S, Komoto S, Maeno Y, Nyangao J, Ide T, Kathiiko C, Odoyo E, Tsuji T, Taniguchi K, Ichinose Y (2017) Molecular epidemiology of rotavirus gastroenteritis in Central Kenya before vaccine introduction, 2009–2014. J Med Virol 89:809–817
Wang Y, Azevedo M, Saif LJ, Gentsch JR, Glass RI, Jiang B (2010) Inactivated rotavirus vaccine induces protective immunity in gnotobiotic piglets. Vaccine 28:5432–5436
Wang Y, Vlasova A, Velasquez DE, Saif LJ, Kandasamy S, Kochba E, Levin Y, Jiang B (2016) Skin vaccination against rotavirus using microneedles: proof of concept in gnotobiotic piglets. PLoS ONE 11:e0166038
Ward RL, Bernstein DI, Shukla R, Young EC, Sherwood JR, McNeal MM, Walker MC, Schiff GM (1989) Effects of antibody to rotavirus on protection of adults challenged with a human rotavirus. J Infect Dis 159:79–88
Ward RL, Clemens JD, Knowlton DR, Rao MR, Van Loon FP, Huda N, Ahmed F, Schiff GM, Sack DA (1992) Evidence that protection against rotavirus diarrhea after natural infection is not dependent on serotype-specific neutralizing antibody. J Infect Dis 166:1251–1257
Westerman LE, McClure HM, Jiang B, Almond JW, Glass RI (2005) Serum IgG mediates mucosal immunity against rotavirus infection. Proc Natl Acad Sci 102:7268–7273
White LJ, Buttery J, Cooper B, Nokes DJ, Medley G (2008) Rotavirus within day care centres in Oxfordshire, UK: characterization of partial immunity. J R Soc Interface 5:1481–1490
WHO (2009) Rotavirus vaccines: an update. Wkly Epidemiol Rec Relevé épidémiologique hebdomadaire 84:533–540
Witte D, Handley A, Jere KC, Bogandovic-Sakran N, Mpakiza A, Turner A, Pavlic D, Boniface K, Mandolo J, Ong DS (2022) Neonatal rotavirus vaccine (RV3-BB) immunogenicity and safety in a neonatal and infant administration schedule in Malawi: a randomised, double-blind, four-arm parallel group dose-ranging study. Lancet Infect Dis 22:668–678
Xia S, Du J, Su J, Liu Y, Huang L, Yu Q, Xie Z, Gao J, Xu B, Gao X (2020) Efficacy, immunogenicity and safety of a trivalent live human-lamb reassortant rotavirus vaccine (LLR3) in healthy Chinese infants: a randomized, double-blind, placebo-controlled trial. Vaccine 38:7393–7400
Xie L, Yan M, Wang X, Ye J, Mi K, Yan S, Niu X, Li H, Sun M (2015) Immunogenicity and efficacy in mice of an adenovirus-based bicistronic rotavirus vaccine expressing NSP4 and VP7. Virus Res 210:298–307
Yuan L, Geyer A, Hodgins DC, Fan Z, Qian Y, Chang K-O, Crawford SE, Parreño V, Ward LA, Estes MK (2000) Intranasal administration of 2/6-rotavirus-like particles with mutant Escherichia coli heat-labile toxin (LT-R192G) induces antibody-secreting cell responses but not protective immunity in gnotobiotic pigs. J Virol 74:8843–8853
Yuan L, Saif LJ (2002) Induction of mucosal immune responses and protection against enteric viruses: rotavirus infection of gnotobiotic pigs as a model. Vet Immunol Immunopathol 87:147–160
Yuan L, Azevedo MS, Gonzalez AM, Jeong K-i, Van Nguyen T, Lewis P, Iosef C, Herrmann JE, Saif LJ (2005) Mucosal and systemic antibody responses and protection induced by a prime/boost rotavirus-DNA vaccine in a gnotobiotic pig model. Vaccine 23:3925–3936
Zaman K, Anh DD, Victor JC, Shin S, Yunus M, Dallas MJ, Podder G, Thiem VD, Mai LTP, Luby SP, Tho LH, Coia ML, Lewis K, Rivers SB, Sack DA, Schödel F, Steele AD, Neuzil KM, Ciarlet M (2010) Efficacy of pentavalent rotavirus vaccine against severe rotavirus gastroenteritis in infants in developing countries in Asia: a randomised, double-blind, placebo-controlled trial. Lancet 376:615–623
Acknowledgments
The authors are grateful to Professor Ulrich Desselberger for assistance in reviewing language and helpful comments relevant to this manuscript.
Funding
The present study was funded and supported by the Pasteur Institute of Iran (grant no. 1316) and Tehran University of Medical Sciences (grant no. 1401-3-340-58739 and grant no. 240/150).
Author information
Authors and Affiliations
Contributions
All authors contributed to the writing of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interests.
Additional information
Handling Editor: Hester G O'Neill.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Latifi, T., Kachooei, A., Jalilvand, S. et al. Correlates of immune protection against human rotaviruses: natural infection and vaccination. Arch Virol 169, 72 (2024). https://doi.org/10.1007/s00705-024-05975-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00705-024-05975-y