Abstract
Background
Galenic dural arteriovenous fistulas (DAVF) are rare; however, they are the most frequent type of DAVF to manifest aggressive clinical behavior and usually represent a diagnostic and therapeutic challenge for clinicians.
Methods
We retrospectively reviewed clinical and imaging data of patients managed with neuroendovascular techniques for the treatment of galenic DAVFs from 2000 to 2016. We searched the 2000–2016 English-language literature for papers discussing neuroendovascular management of galenic DAVFs, with or without companion surgical procedures.
Results
Five patients were treated for galenic DAVFs during the study period (four males; mean age, 61 years). Three presented with progressive neurological deterioration due to venous congestion, two with acute intracranial hemorrhage. Three were treated by staged transarterial embolization procedures (three procedures in two, four procedures in one); two underwent a single transvenous embolization procedure. Four out of five fistulas were completely occluded. All patients improved clinically; the patient whose fistula was partially occluded remains angiographically stable at 2-year follow-up. Six reports describing 17 patients are reviewed. Embolization was performed via transvenous approach in 1/17 and transarterial approach in 16/17 with additional open surgery in 9/16. The trend toward the use of transarterial approaches is based primarily on advances on embolization techniques that allow better and more controllable penetration of the embolizing agents with improved clinical and angiographic results, as well as the technical complexity of the transvenous approach.
Conclusions
Although transarterial embolization is the preferred endovascular route for the management of most galenic DAVFs, selected cases can be successfully treated by transvenous approach.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Galenic dural arteriovenous fistulas (DAVF) are, by definition, the most deeply and anteriorly located subtype of the relatively rare family of falco-tentorial fistulas [1, 8, 19, 26]. Although there are few descriptions of galenic DAVFs in the literature, they are the most frequent type of DAVF to manifest aggressive clinical behavior. This is likely the result of associated deep veno-occlusive disease and the recruitment of cortical venous drainage, which increases the risk of venous hypertension, interstitial edema, and hemorrhage [1, 8, 26]. Due to their rarity and their wide and varied clinical presentation, these fistulas represent a diagnostic and therapeutic challenge for clinicians. Based on recent reports, and mainly due to advances on microcatheter technology and embolizing agents, transarterial embolization is the preferred therapeutic modality to deal with this entity. Transvenous embolization, although frequently used in other types of DAVFs, has been a less explored alternative in galenic fistulas.
We report two cases of galenic DAVF with varying clinical presentations and angiographic features that were successfully managed by transvenous endovascular approaches, as well as three patients managed with transarterial approaches. Neuroimaging evaluation, endovascular therapy, and the relevant literature are discussed.
Material and methods
We retrospectively searched for patients with galenic DAVF admitted to our unit during the period 2002–2016. In that period, we diagnosed and treated five patients with galenic DAVFs. The diagnosis of DAVF was suspected based on computed tomography (CT) and magnetic resonance imaging (MRI) studies, and confirmed by cerebral angiography. Their clinical records and neuroradiological exams were retrospectively reviewed and relevant demographic and clinical data was extracted under Institutional Review Board approval with a waiver of informed consent. We correlate their clinical presentation, mainly venous congestion or hemorrhage, with specific angiographic features and physiopathological mechanisms, and describe their neuroendovascular management.
A search for the relevant English-language literature from 2000 to 2016 was performed using Medline and Google Scholar, with the search terms: “vein of Galen,” “vein of Rosenthal,” “deep venous system,” and “arteriovenous fistula.” Reports of patients with DAVFs involving the galenic system who were managed with neuroendovascular techniques alone or in combination with open surgical procedures were included.
Results
Patients
Details regarding the presentation, management, and outcomes of the five patients included in this report are shown in Table 1. There were four men and one woman, with ages ranging from 41 to 73 years (mean age, 61). Two of the patients (nos. 2 and 3) presented with acute subarachnoid and intraventricular hemorrhage, and three with progressive neurological deterioration (patients 1, 4, and 5). Both patients presenting with hemorrhage required insertion of external ventricular drainage upon admission. Patients with progressive neurological deterioration presented after protracted clinical deterioration over several years (patient 1, 2 years; patient 4, 2 years; patient 5, 3 years). All three had been misdiagnosed as presenting degenerative, vascular, and/or demyelinating processes. The five patients in this series all improved clinically following treatment. Those presenting with symptoms stemming from venous congestion (patients 1, 4, and 5) were stabilized first and then improved even at early stages following intervention when partial occlusion had been achieved. The two presenting with acute hemorrhage (patients 2 and 3) did not rebleed during clinical follow-up of 1 and 5 years, respectively.
Three patients (nos. 3, 4, and 5) were managed by staged transarterial embolization procedures, three procedures in patients 3 and 4, four procedures in patient 5. Two to three arterial pedicles were embolized in every procedure (median, 3); the preferred route for transarterial embolization was the middle meningeal artery in all the three cases. Onyx, the preferred embolizing agent in each case, was used in 22 out of a total of 28 embolized arterial pedicles and glue was used in six. In patients 1 and 4, the DAVF was completely occluded. In patient 5, the fistula was subtotally occluded with residual meningo-hypophyseal trunk feeders, but it remained angiographically stable with clinical and radiological improvement at 2-year follow-up.
Two patients (nos. 2 and 3) were managed using a single transvenous embolization procedure that was curative. These two are the primary focus of this report.
Transvenous neuroendovascular procedures
Patient 1
A 71-year-old man presented with a 2-year history of dizziness, double vision, hemifacial numbness, slow cognition, and gait imbalance. Over the last 6 months, paraparesis had evolved to progressive quadriparesis. On neurological examination, he presented neuropathies of cranial nerves V, VI, and VII, left hemi-hypoesthesia, right arm tremor, diadochokinesia, severe paraparesis, moderate left arm paresis, and mild right arm paresis (ascending quadriparesis).
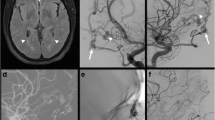
Based on a series of earlier neuroradiological examinations, he had been incorrectly diagnosed with extensive small vessel disease affecting the brainstem, and later with a probable demyelinating process. Reexamination of previous imaging studies and admission CT and MRI demonstrated brainstem swelling and an increased T2 signal in the pons, midbrain, and thalami (Fig. 1a-c). CT angiogram (CTA) showed pseudoaneurysmatic enlargement of the vein of Galen, raising the possible diagnosis of vascular malformation (Fig. 1d).
a–c T2-weighted MRI demonstrating diencephalic and brainstem swelling in a 71-year-old man (patient 1). Note hyperintense T2 signal in both thalami, mesencephalon, and pons. d Midsagittal CT angiogram (CTA) showing pseudoaneurysmatic enlargement of the vein of Galen, raising the possible diagnosis of vascular malformation. e–g Angiographic images of selective external carotid and left vertebral arteries showing that the DAVF is supplied through the middle meningeal, transdiploic-occipito-dural, posterior meningeal, and vermian branches. h Intraprocedural magnified angiographic view after retrograde microcatheterization of the thrombosed straight sinus. Microangiogram obtained at the superior cerebellar vein (thin arrow) after navigating through the vein of Galen (thick arrow) and superior cerebellar vein (bridging veins), demonstrates the arterialized flow patter of the vein of Galen, the inverted direction of flow in the basal vein of Rosenthal (curved arrow) and lateral mesencephalic vein (star). i Road map image shows occlusion of the pouch of the superior cerebellar vein by implant of detachable coils. j–k Immediate postembolization angiogram of the left common carotid and the left vertebral arteries confirm complete occlusion of the galenic fistula
After admission, the patient developed aspiration pneumonia and presented a complicated clinical course requiring intubation and mechanical ventilator assistance. When clinical stabilization was achieved, he underwent digital subtraction cerebral angiography, which demonstrated a galenic system DAVF supplied by petrosal branches of the middle meningeal arteries (MMA), mastoid branches of the occipital arteries, posterior meningeal branches of the posterior inferior cerebellar arteries (PICA), and vermian branches of both superior cerebellar arteries (Fig. 1e-g).
Under general anesthesia, femoral arterial and venous accesses were obtained. Angiograms of the left external carotid artery were used to obtain venous road maps. By means of the triaxial system and after retrograde microcatheterization of the thrombosed straight sinus, microangiogram obtained at the superior cerebellar vein demonstrated an arterialized flow pattern through the vein of Galen, as well as reversal of the direction of flow through the basal vein of Rosenthal, the lateral mesencephalic vein, and the petrosal veins (Fig. 1h). The superior cerebellar venous pouch and vermian vein, considered the site of the fistula, were occluded by means of detachable coils (Fig. 1i). Immediate postembolization angiogram confirmed complete occlusion of the DAVF (Fig. 1j-l).
On the day following intervention, the patient’s cranial neuropathies and motor functions showed marked improvement. He was discharged 1 week later to a rehabilitation facility after having regained his ability to stand and walk with the aid of a walker. At 1-month follow-up, he was able to walk independently. MRI obtained after 4 months confirmed complete resolution of brainstem and diencephalic edema (Fig. 1m). MR follow-up after 36 months showed no signs of edema.
Patient 2
This previously healthy 41-year-old woman was admitted through the emergency room after sudden onset of headache, followed by deterioration in consciousness. Admission CT showed massive intraventricular hemorrhage causing ventricular enlargement (Fig. 2a). CTA demonstrated a pseudoaneurysm of the vein of Galen associated with multiple abnormal vessels at the Galen-straight sinus junction (Fig. 2b). The patient was urgently intubated and external ventricular drainage was placed. Digital subtraction cerebral angiography demonstrated a galenic system DAVF supplied by the petrosal and tentorial branches of both middle meningeal arteries (MMA), the mastoid branches of the occipital arteries, the posterior meningeal branches of the posterior inferior cerebellar arteries (PICA), and the vermian branches of both superior cerebellar arteries (SCA) (Fig 2c-f). The vein of Galen presented an irregularly shaped pseudoaneurysmatic dilatation and clear small daughter sac anteriorly, which was considered the site of hemorrhage.
a Nonenhanced CT of a 41-year-old woman (patient 2) shows intraventricular hemorrhage and hydrocephalus. b CTA shows pseudoaneurysmatic enlargement of the vein of Galen. c–f Selective angiographic images of the right external carotid artery (lateral view), left external carotid artery (anteroposterior view), right internal carotid artery (oblique view), and left vertebral artery (anteroposterior view). The galenic DAVF is supplied by middle meningeal, occipital, and tentorial branches and confluent at the vein of Galen pseudoaneurysm, which drains caudally through the patent straight sinus. g Selective angiographic image of the right external carotid artery (oblique view) is used as road map for transvenous access. h Radioscopic image shows the intermediate catheter placed at the straight sinus and the microcatheter tip at the anterior aspect of the galenic pseudoaneurysm. i Microangiogram obtained at the galenian pouch shows cribriform filling defects caused by the afferent feeders. j Radioscopic image obtained after tight coiling of the pseudoaneurysm. k–l Immediate postembolization angiogram of the right external and internal carotid arteries confirming complete occlusion of the galenic fistula
Under general anesthesia, right femoral arterial and right cervical internal jugular venous accesses were obtained. Angiograms of the right external carotid artery were used to obtain procedural venous road maps (Fig. 2g). By means of a coaxial system (FARGO guiding catheter—Balt Extrusion, Montmorency, France; Excelsior SL-10 microcatheter—Stryker, Kalamazoo, MI, USA), retrograde microcatheterization of the straight sinus allowed microcatheterization and microangiographic evaluation of the lesion. The pseudoaneurysmatic pouch of the vein of Galen presented a cribriform appearance (feeder inflow) and demonstrated arterialized, high flow and rapid transit through the straight sinus (Fig. 2h-i). The galenic venous pouch, considered the site of the fistula, was then occluded by means of detachable coils (Fig.2j). Immediate postembolization angiogram confirmed complete occlusion of the DAVF (Fig. 2k-l).
The patient evolved satisfactorily and regained full consciousness without any focal neurological sequelae after 48 h. Ventriculostomy was converted to permanent ventriculoperitoneal shunt at day 12 and the patient was discharged to a rehabilitation facility on day 15. Follow-up angiogram after 3 months and CTA after 10 months confirmed occlusion of the DAVF.
Literature review
Six reports published between 2002 and 2016 were included in the current review [12, 17–19, 26, 27], with findings summarized in Table 1. A total of 17 patients are presented, including 12 men and five women with mean age 55 years (range, 29–73). Five presented with hemorrhage, three with hydrocephalus, and eight with neuropathies. Thalamic hyperintensities were seen in five of the 17. Overall, 7/17 were managed with transarterial embolization (six with onyx, one with glue); one patient underwent transvenous embolization with coils, and nine had a combination of transarterial embolization (three with onyx, six with other embolizing agents, including polyvinyl alcohol particles, coils, ethanol, glue, and combinations of these agents) and surgical treatment. Neuroendovascular procedures were thus performed via transarterial approaches in 16 patients with companion surgical procedures in nine, and through a transvenous approach in one patient. The DAVF was occluded in 16 patients (15 treated via transarterial approaches and one through a transvenous approach); one 54-year-old patient died after he hemorrhaged during the endovascular procedure.
Discussion
Galenic DAVFs are a heterogeneous group defined by drainage into the deep venous system at various sites and represent approximately 23% of all tentorial DAVFs [19]. They are located at the anterior falco-tentorial junction, and have been distinguished from straight sinus and torcular DAVFs that are based more posteriorly at the middle and posterior falco-tentorial junction. Lesions at these last two locations present a different angioarchitecture and clinical behavior, and require different surgical approaches [19].
We present two cases of galenic DAVFs with very different clinical presentation that were completely occluded in a single embolization procedure performed using a transvenous approach. The first patient had experienced a long, slowly progressing neurological deterioration, and the second presented with acute intraventricular and subarachnoid hemorrhage. Differences in clinical presentation may be attributed to different arterial feeding patterns or, more importantly, to differences in angioarchitectural venous features such as associated veno-occlusive disease (sinodural vein thrombosis), variations in venous collateral pattern, and venous outflow restriction. In general, tentorial DAVFs are classified as Borden type III/Cognard III–IV and present a high relative risk of hemorrhage [13].
In patient 1, we hypothesized that thrombosis of the straight sinus and associated compromise of the deep venous system, including the distal superior cerebellar vein, triggered development of a superior cerebellar-bridging vein DAVF. The superior cerebellar vein is a single trunk resulting from the union of the pre-central cerebellar vein and the superior vermian vein, which usually drains directly into the vein of Galen [9]. A DAVF at this vein should cause cerebellar venous hypertension and arterialization of the vein of Galen with flow inversion in its tributaries, thus leading to various degrees of venous hypertension of the basal, petrosal, pontine, precentral and mesencephalic veins [3, 9]. As a result, the venous drainage of the diencephalon, mesencephalum, striatum, and periventricular white matter was compromised in our patient, as evidenced by his clinical and neuroradiological data; however, the cerebellar vermis and tentorial cerebellar surface were not affected as expected. It seems that the vermis and tentorial cerebellar surface remained protected from the congestive hypertensive process due to coexistent distal thrombosis of the superior cerebellar vein. In cases of obstruction of the vein of Galen, or as in this case, hypertension with outflow occlusion (straight sinus thrombosis), anastomoses via the basal vein of Rosenthal and its most important venous outlet, the lateral mesencephalic vein, provide an important salvage outlet for venous drainage toward the petrosal sinus system. In this patient, collateralization proved to be insufficient to cope with the fistula debit, resulting in sustained venous congestion, and then mesencephalic and diencephalic interstitial edema.
Compromise of the deep venous system can cause different degrees of diencephalic edema, mental symptoms, coma, hyperpyrexia, tachycardia, tachypnea, myosis, limb rigidity, and exaggeration of deep tendon reflexes or eye movement disorders, closure of the aqueduct of the mesencephalon, and blindness and extraocular palsies [9, 22]. Anatomic variations of the mesencephalic veins may explain different clinical scenarios [7]. Holekamp et al. [17] recently presented their experience with a 71-year-old man who presented with cognitive decline and bilateral thalamic hyperintensities on MRI fluid-attenuated inversion recovery (FLAIR) examination. The patient had a partial improvement after undergoing two transarterial onyx embolizations with obliteration of the fistula, followed by surgery. The authors hypothesized that congestion of the patent draining veins may affect different territories, leading to unique clinical presentations such as thalamic dementia. Despite the clinical and radiological differences from our patient, in whom this congestion led also to myelopathy, the feeding vessels, flow, and site of the fistula were similar. Probst et al. [23], who described a non-galenic DAVF causing brainstem venous congestion, compared the pathophysiological mechanism of venous congestion in cerebral DAVFs, which cause reversible neurological symptoms of the brain stem, to the pathomechanism in the spinal dural fistula disease known as Foix-Alajouanine disease.
In patient 2, the DAVF developed at the vein of Galen itself, leading to pseudoaneurysmatic enlargement of the vein and rupture through an anteriorly located bleb. This type of venous aneurysm is exceptionally encountered with clinical symptoms. It develops as a direct result of the fistula, and represents its site. It is considered the source of hemorrhage, and its occlusion is thus considered mandatory. In contrast, venous aneurysms or ectasias are generally the result of longstanding venous hypertension or retrograde venous flow. They are to be seen as signs of focal structural decompensation of the cerebral venous system and markers of venous strain, as recently described by Baltsavias et al. [5]. In these cases, occlusion of the ectasias is not necessary and even detrimental. The fistula in our patient did not present leptomeningeal retrograde venous flow, a recognized feature of DAVFs presenting aggressive neurological behavior. Instead there was a bilateral arterial supply, high-flow shunting, and galenic venous drainage with this venous aneurysm, all characteristics associated with aggressive behavior [1, 5]. In addition, a Galen-straight sinus junction relative stenosis was identified as responsible for the venous outflow restriction that led to venous aneurysm rupture. This case exemplifies the exceptional but real hemorrhagic risks of an arterialized venous pouch and its treatment was analogous to the accepted approach for arterial aneurysms, i.e., embolization of the arterialized venous aneurysm.
De Vleeschouwer et al. [12] presented the first case of a ruptured galenic DAVF in a patient whose large central venous aneurysm was associated with the vein of Galen, which formed the key point of the fistula. The venous aneurysm was treated by surgical clipping and the DAVF was completely excluded. The case we present here confirms the rupture of a fistular venous aneurysm of the vein of Galen itself as the physiopathological mechanism for galenic DAVF hemorrhage, with the resulting need for aneurysm occlusion. It is noteworthy that, despite the fact that vein of Galen aneurysmal malformations may present venous aneurysms of giant dimensions, their rupture is considered exceptional.
It is generally accepted that the presentation of a DAVF is intrinsically linked to shunt topography, and that galenic lesions are the most frequent type of DAVF to manifest aggressive clinical behavior. Recently, Baltsavias et al. [4, 5] showed that topography is intrinsically linked to a specific venous anatomy that determines the angioarchitectural features of the dural shunts and dictates clinical presentation.
A review of the galenic DAVF subgroup is limited by the fact that many authors included their experience in the management of galenic DAVFs together with a broader undistinguished category of tentorial or falco-tentorial DAVFs [14, 20]. Our literature review shows these fistulas are more frequently managed by transarterial endovascular embolization techniques, primarily because of advances in embolization techniques that allow better and more controllable penetration of the embolizing agents with consequent improved clinical and angiographic results, as well as the technical complexity of the transvenous approach in this type of fistulas. The comparative advantages associated with the use of onyx for embolization of dural AV fistulas were discussed by Cognard et al. [11] and Nogueira et al. [21].
From the surgical point of view, Lawton et al. [19] considered galenic DAVFs to be the most complex of the tentorial fistulae. The galenic region is the deepest location, the confluence of falx and tentorium creates awkward barriers and surgical blind spots, arterial inflow arrives from all directions, and venous outflow can be difficult to decipher, particularly when veins are tortuous or variceal. Despite all these factors, some authors have reported complete and persistent obliteration of the fistula with good clinical results using embolization followed by surgery [12, 19]. Indeed, Halbach et al. [15] concluded that treatment of galenic DAVFs is challenging, often requiring combined transarterial-transvenous embolization and open surgery.
The transvenous approach and dural sinus therapeutic occlusion sacrifice has been an established and widely used method for the treatment of cranial DAVF for decades [15, 25]. Both dural sinus and emissary vein shunts are suitable for safe transvenous navigation and occlusion; however, navigation through leptomeningeal veins makes this approach more challenging in cases of bridging vein shunts [2, 3]. The two patients who are the primary focus of the current report illustrate the technical feasibility and efficacy of transvenous endovascular coiling in cases of bridging vein shunts in the management of this entity. However, venous anatomy is often extremely tortuous and thus inaccessible to this retrograde venous approach. Unfortunately, the transarterial route faces the dual problem of difficult access and multiplicity of feeder sources supplying the galenic DAVFs; thus, transarterial embolization has generally been considered palliative, and only rarely curative. Despite this limitation, with the advent of new embolizing agents such as onyx, there are a growing number of reports of complete galenic DAVF obliteration after transarterial embolization, with either preservation [10, 27] or occlusion of the vein of Galen [18, 27].
Our review of the recent literature on endovascular embolization of galenic DAVFs confirms that there is a relative shift towards transarterial embolization with onyx, and that the transvenous approach is used less often (Table 1). We also chose to treat three out of our five patients via transarterial routes, due to a relatively direct transarterial access and, more importantly, due to extreme tortuosity of the venous access in these cases. Nevertheless, despite the expected complexity with venous routes, straightforward venous access is feasible in selected cases, as shown in two patients who were successfully managed by transvenous coil embolization of a compromised superior cerebellar bridging vein and a galenic aneurysm.
The galenic system is a complex venous network, and embolization of the vein of Galen or its tributaries is dreaded by most neurointerventionalists, although the consequences of venous sacrifice have not been consistently reported in the literature [9]. However, as in other types of DAVFs, if the compromised vein, the target of embolization, no longer contributes to the drainage of normal tissue, the procedure can be carried out with acceptable safety. This has been shown previously in cases where the vein of Galen was intentionally occluded [18] and supports the embolization strategy used on patient 2. Based on experience in the management of pineal tumors, sacrificing the superior vermian, hemispheric, or vermian bridging veins has been considered relatively safe [16, 24], lending conceptual support to the embolization performed on patient 1. Nevertheless, every intended venous occlusion presents some degree of clinical unpredictability; thus, as a general rule, and especially in symptomatic cases where the clinical importance of the vein with retrograde filling cannot be adequately assessed, it is recommended that venous occlusion should be limited to the directly affected venous segment to reduce the risk of venous infarction, avoid distal occlusions, and reduce the probability of fistula progression.
The transvenous approach, performed through a thrombosed (patient 1) or a patent (patient 2) retrograde venous path, allowed complete occlusion of these DAVFs in a single embolization session. The efficacy and safety of retrograde navigation through thrombosed sinuses can be greatly aided by the gentle use of J-tipped, soft-tipped guidewires or by using the loop technique described by Benndorf et al. [6] for thrombosed inferior petrosal sinus access to the cavernous sinus.
Conclusions
The advent of new embolizing agents and advances in onyx-compatible microcatheter and microballoon technology have increased the efficiency and control of embolizing agent injection, leading to a trend toward transarterial embolization of dural fistulas. Moreover, results with this technique are considerable better in comparison to early reports, when curative transarterial procedures were not realistic. The procedures presented here exemplify the feasibility, safety, and efficacy of the transvenous approach in specific cases.
References
Awad IA, Little JR, Akarawi WP, Ahl J (1990) Intracranial dural arteriovenous malformations: factors predisposing to an aggressive neurological course. J Neurosurg 72:839–850
Baltsavias G, Kumar R, Avinash KM, Valavanis A (2015) Cranial dural arteriovenous shunts. Part 2. The shunts of the bridging veins and leptomeningeal venous drainage. Neurosurg Rev 38:265–271, discussion 272
Baltsavias G, Parthasarathi V, Aydin E, Al Schameri RA, Roth P, Valavanis A (2015) Cranial dural arteriovenous shunts. Part 1. Anatomy and embryology of the bridging and emissary veins. Neurosurg Rev 38:253–263, discussion 263–254
Baltsavias G, Roth P, Valavanis A (2015) Cranial dural arteriovenous shunts. Part 3. Classification based on the leptomeningeal venous drainage. Neurosurg Rev 38:273–281, discussion 281
Baltsavias G, Spiessberger A, Hothorn T, Valavanis A (2015) Cranial dural arteriovenous shunts. Part 4. Clinical presentation of the shunts with leptomeningeal venous drainage. Neurosurg Rev 38:283–291, discussion 291
Benndorf G, Bender A, Lehmann R, Lanksch W (2000) Transvenous occlusion of dural cavernous sinus fistulas through the thrombosed inferior petrosal sinus: report of four cases and review of the literature. Surg Neurol 54:42–54
Cannizzaro D, Rammos SK, Peschillo S, El-Nashar AM, Grande AW, Lanzino G (2016) The lateral mesencephalic vein: surgical anatomy and its role in the drainage of tentorial dural arteriovenous fistulae. World Neurosurg 85:163–168
Chaloupka JC (1994) Endovascular therapy of dural arteriovenous fistulae. Semin Interv Radiol 11:1–13
Chaynes P (2003) Microsurgical anatomy of the great cerebral vein of Galen and its tributaries. J Neurosurg 99:1028–1038
Choudhri O, Marks MP (2014) Endovascular treatment of a tentorial dural arteriovenous fistula. Neurosurg Focus 37:1
Cognard C, Januel AC, Silva NA Jr, Tall P (2008) Endovascular treatment of intracranial dural arteriovenous fistulas with cortical venous drainage: new management using Onyx. AJNR Am J Neuroradiol 29:235–241
De Vleeschouwer S, Smets CA, Wilms G (2011) Long-lasting, complete exclusion of a large galenic dural arteriovenous fistula after clipping of the central venous aneurysm of the vein of galen: case report. Neurosurgery 68:E571–574, discussion E574
Gross BA, Du R (2012) The natural history of cerebral dural arteriovenous fistulae. Neurosurgery 71:594–602, discussion 602–593
Gross BA, Du R (2013) Surgical treatment of high grade dural arteriovenous fistulae. J Clin Neurosci 20:1527–1532
Halbach VV, Higashida RT, Hieshima GB, Wilson CB, Hardin CW, Kwan E (1989) Treatment of dural fistulas involving the deep cerebral venous system. AJNR Am J Neuroradiol 10:393–399
Hart MG, Santarius T, Kirollos RW (2013) How I do it—pineal surgery: supracerebellar infratentorial versus occipital transtentorial. Acta Neurochir (Wien) 155:463–467
Holekamp TF, Mollman ME, Murphy RK, Kolar GR, Kramer NM, Derdeyn CP, Moran CJ, Perrin RJ, Rich KM, Lanzino G, Zipfel GJ (2016) Dural arteriovenous fistula-induced thalamic dementia: report of 4 cases. J Neurosurg 124:1752–1765
Laviv Y, Kasper E, Perlow E (2016) Single-session, transarterial complete embolization of Galenic dural AV fistula. Acta Neurochir (Wien) 158:255–259
Lawton MT, Sanchez-Mejia RO, Pham D, Tan J, Halbach VV (2008) Tentorial dural arteriovenous fistulae: operative strategies and microsurgical results for six types. Neurosurgery 62:110–124, discussion 124–115
Liu C, Xu B, Song D, Leng B, Mao Y, Gu Y, Liao Y (2014) Clinical approach of using Onyx via transarterial access in treating tentorial dural arteriovenous fistula. Neurol Res 36:983–991
Nogueira RG, Dabus G, Rabinov JD, Eskey CJ, Ogilvy CS, Hirsch JA, Pryor JC (2008) Preliminary experience with onyx embolization for the treatment of intracranial dural arteriovenous fistulas. AJNR Am J Neuroradiol 29:91–97
Ono M, Rhoton AL Jr, Peace D, Rodriguez RJ (1984) Microsurgical anatomy of the deep venous system of the brain. Neurosurgery 15:621–657
Probst EN, Christante L, Zeumer H (1994) Brain-stem venous congestion due to a dural arteriovenous fistula in the posterior fossa. J Neurol 241:175–177
Rey-Dios R, Cohen-Gadol AA (2013) A surgical technique to expand the operative corridor for supracerebellar infratentorial approaches: technical note. Acta Neurochir (Wien) 155:1895–1900
Uflacker R, Lima S, Ribas GC, Piske RL (1986) Carotid-cavernous fistulas: embolization through the superior ophthalmic vein approach. Radiology 159:175–179
Weigele JB, Chaloupka JC, Lesley WS (2002) Galenic dural arteriovenous fistula: unusual clinical presentation and successful endovascular therapy. Case report. J Neurosurg 97:467–470
Wu Q, Zhang XS, Wang HD, Zhang QR, Wen LL, Hang CH, Zhang X (2016) Onyx embolization for tentorial dural arteriovenous fistula with pial arterial supply: case series and analysis of complications. World Neurosurg 92:58-64
Acknowledgements
The authors wish to thank Shifra Fraifeld, Senior Medical Writer and Head of Research Support in the Departments of Neurosurgery and Radiology at the Hadassah—Hebrew University Medical Center, for her editorial assistance in the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research.
Conflict of interest
All authors certify that they have no affiliation with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) related to the subject matter or materials discussed in this manuscript.
Ethical approval
This study was completed in accordance with the ethical standards of the Institutional Research Board, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. All procedures discussed in the manuscript were performed as part of the routine medical care for these patients, and were not related in any way to a research or study protocol relating to this manuscript or other research. For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Cohen, J.E., Gomori, J.M., Rajz, G. et al. Clinical and angioarchitectural factors influencing the endovascular approach to galenic dural arteriovenous fistulas in adults: case series and review of the literature. Acta Neurochir 159, 845–853 (2017). https://doi.org/10.1007/s00701-017-3089-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-017-3089-0