Abstract
Cranial dural arteriovenous fistulae have been classified into high- and low-risk lesions mainly based on the pattern of venous drainage. Those with leptomeningeal venous drainage carry a higher risk of an aggressive clinical presentation. Recently, it has been proposed that the clinical presentation should be considered as an additional independent factor determining the clinical course of these lesions. However, dural shunts with leptomeningeal venous drainage include a very wide spectrum of inhomogeneous lesions. In the current study, we correlated the clinical presentation of 107 consecutive patients harboring cranial dural arteriovenous shunts with leptomeningeal venous drainage, with their distinct anatomic and angiographic features categorized into eight groups based on the “DES” (Directness and Exclusivity of leptomeningeal venous drainage and features of venous Strain) concept. We found that among these groups, there are significant angioarchitectural differences, which are reflected by considerable differences in clinical presentation. Leptomeningeal venous drainage of dural sinus shunts that is neither direct nor exclusive and without venous strain manifested only benign symptoms (aggressive presentation 0 %). On the other end of the spectrum, the bridging vein shunts with direct and exclusive leptomeningeal venous drainage and venous strain are expected to present aggressive symptoms almost always and most likely with bleeding (aggressive presentation 91.5 %). Important aspects of the above correlations are discussed. Therefore, the consideration of leptomeningeal venous drainage alone, for prediction of the clinical presentation of these shunts appears insufficient. Angiographic analysis based on the above concept, offers the possibility to distinguish the higher- from the lower-risk types of leptomeningeal venous drainage. In this context, consideration of the clinical presentation as an additional independent factor for the prediction of their clinical course seems superfluous and possibly misleading. Topography is connected to the clinical presentation of the dural shunts inasmuch as the former determines the venous anatomy and the angioarchitectural features of the lesions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cranial dural arteriovenous fistulae (CDAVF) with leptomeningeal venous drainage (LVD) are complex vascular lesions, which carry a significant risk of an aggressive clinical presentation and have a poor natural history [11, 4, 25, 24, 6, 26, 1]. Recent reports have proposed that lesions with a benign presentation have a better clinical course in comparison to those with an aggressive clinical presentation [4, 11, 25, 24]. However, lesions with LVD constitute a very heterogeneous group since they include shunts with different angioarchitectural features. Analyses, which do not take into consideration the spectrum of these features and the corresponding subgroups of lesions with LVD, may lead to erroneous conclusions. Assuming that presentation may be closely related to the above features, being presumably their clinical expression, we examined the relation between the distinct anatomic and angiographic features of CDAVF with LVD, based on the “DES” (Directness and Exclusivity of leptomeningeal venous drainage and features of venous Strain) scheme, and their clinical presentation. In parallel, we examined the relation of the above features with the topography of the lesions. Whether clinical presentation constitutes an additional independent determining factor of poor natural history [28] is an important related issue, addressed indirectly in this study. A critical review of recent related publications is also presented.
Materials and methods
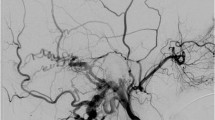
From a series of 211 consecutive patients with CDAVF treated in our department during the last 19 years, 107 patients demonstrating a lesion with LVD had complete angiographic images [2]. Among them, 36 patients had lesions with mixed leptomeningeal and dural drainage (Borden [3] grade 2 and Cognard [5] grades IIb, IIa + b) and 71 cases had lesions with LVD only (Borden grade 3 and Cognard grades III, IV, V). Cases of pediatric and/or congenital CDAVFs were excluded. The angiographic images of all cases were analyzed by two specialists blinded to the clinical presentation data. They recorded data on the base of the DES (Directness, Exclusivity of leptomeningeal venous drainage and venous Strain) concept. A direct LVD is characterized by a venous drainage through the bridging vein(s) (BV) to the leptomeningeal venous system without interposition of a sinus. Therefore, the directness of the LVD is the expression of the exact location of the shunt on a bridging vein. An exclusive LVD was defined as venous drainage by only the leptomeningeal veins. Therefore, the exclusivity of the LVD is mostly the expression of venous outflow restrictions (VOR) as complete or partial sinus thrombosis or stenosis. The characteristics of venous strain included congestion with pseudophlebitic appearance [27, 16, 8] of the leptomeningeal veins as well as venous ectasia. In our descriptions, ectasia and varix were deemed as synonymous terms and, together with venous aneurysms, were considered as signs of focal structural decompensation of the cerebral venous system, likely linked to hemorrhagic presentation. Uniformly dilated veins along their entire course, without signs of ectasia or aneurysm, although they certainly express some degree of venous hypertension, were not deemed signs of venous decompensation, and therefore, were not recorded as venous strain. The so-called pseudophlebitic pattern of the venous system was considered as another sign of venous decompensation with congestion and stagnation, heralding venous infarction, and likely linked to progressive neurological deficit. Interobserver agreement for the recorded data was evaluated between the two readers and cases of disagreement were settled by consensus.
In this way, the three main aspects D, E, S of the CDAVF angioarchitecture were compared to the clinical presentation of the lesions. Although hemorrhage (H) is usually recorded together with other aggressive presentations, we opted to record it also separately taking into account that hemorrhage is always a sudden and irreversible event, very often with significant impact on the brain. Progressive neurological deficit (PND) due to regional venous congestion or mass-effect of a venous varix or dementia, which have a more gradual and possibly reversible course were also recorded as aggressive presentations. TIA and epilepsy, which are mostly episodic and rather warning neurological manifestations (NM) were not included in the aggressive presentation group because from a purely clinical point of view, they were deemed as intermediate clinical presentation. Therefore, the sum of hemorrhages and PND was referred to as aggressive presentation (AP). Benign was defined as the clinical presentation when symptoms including tinnitus, atypical headaches, and/or dizziness and those related to orbital venous congestion, were described. Cases that presented with cranial nerve deficits and diplopia, facial nerve palsy, or glaucoma with decreased visual acuity, were not included in the benign group [19, 9], because from a purely clinical point of view, they were considered to have an intermediate severity. These symptoms, together with the NM, were defined as intermediate presentation (IP). An incidental discovery was not considered a benign presentation and was not counted in the calculation of percentages. In patients with multiple lesions, only the higher-grade shunt with LVD was considered.
Accordingly, the patients were grouped into the following eight groups: the nD-nE-nS group with non-direct, non-exclusive LVD, without cortical venous strain; the nD-nE-S group with non-direct, non-exclusive LVD, with cortical venous strain; the nD-E-nS group with non-direct, exclusive LVD, without cortical venous strain; the nD-E-S group with non-direct, exclusive LVD, with cortical venous strain; the D-nE-nS group with direct, non-exclusive LVD, without cortical venous strain; the D-nE-S group with direct, non-exclusive LVD, with cortical venous strain; the D-E-nS group with direct and exclusive LVD, without cortical venous strain; and the D-E-S group with direct and exclusive LVD, with cortical venous strain.
We hypothesized that each group should show varying degrees of aggressive clinical presentation. An exact conditional chi-squared test for small samples was used to access statistical significance of aggressive clinical presentation among the groups by testing independence of group and AP [13]. The effect of each angioarchitectural characteristic of the DES system, namely directness (D), exclusivity (E), and venous strain (S) on the clinical presentation, possible association of venous strain pattern (pseudophlebitic congestion and venous ectasia) with distinct aggressive clinical presentations and association of anatomic locations with a specific type of shunt were also investigated.
Interobserver agreement for each of the three angioarchitectural main features (D, E, and S) was calculated using Cohen kappa coefficient.
Results
Patient data and group assignment are shown in Table 1. All 50 patients with non-direct (nD) LVD carried by definition a shunt based in the sinus, called “dural sinus shunt” (DSS). Among them, the groups with exclusive LVD correspond to the so-called isolated sinus shunt (ISS). The rest of the 57 patients with direct (D) LVD correspond to shunts based in BVs, thus called BV shunts (BVS), with the vast majority having an exclusive LVD at the time of presentation; only 4 (7 %) of these shunts had a non-exclusive LVD.
Shunts with non-direct LVD
None of the shunts of the nD-nE-nS group had an aggressive presentation (0 %). From the nD-nE-S group, three patients presented with bleeding (33 %); two with venous hypertension-dementia, therefore, an overall aggressive presentation in 55.5 %; one with epileptic attack, whereas, three patients with tinnitus. Most of the nD-E-nS group presented with benign symptoms. Two patients presented with a small hemorrhage in the hemisphere contralateral to the lesion; none had a draining vein near. One had a known coagulopathy, which was considered the cause of bleeding since the contralateral occurrence was difficult to be attributed to the shunt; thus, it was deemed as an incidental finding. The second patient had no other apparent cause for the bleeding and it was deemed his clinical presentation. From the nD-E-S group, two patients presented with bleeding (20 %), four patients with progressive neurological deficit due to regional venous congestion, one patient with dementia, two with epilepsy, one with headaches, and one with small co-incidental stroke of the pons; therefore, an aggressive presentation was recorded in 70 % of cases.
Shunts with direct LVD
One case from D-nE-nS group was an incidental finding, whereas the second case presented with tinnitus and suspicion of epileptic attack. The D-nE-S group also included two cases: one presenting with epilepsy and the second with strong headaches and dizziness. Among the 16 cases of the D-E-nS group, 3 patients presented with bleeding (23 %), 4 patients with progressive neurological deficit (31 %), 1 with epilepsy, 2 with TIA, 3 with atypical symptoms, including headaches, balance disturbances, dizziness, amaurosis, prominent frontal veins, leg tremor, and lip numbness, which were considered manifestations of the benign spectrum, plus 3 patients with their lesion incidentally discovered. Therefore, the aggressive presentation rate of this group was 54 %. Among the 37 patients of the D-E-S group, 27 presented with bleeding (75 %), 6 with progressive neurological deficit (16.5 %), 1 with TIA, 1 with epilepsy, 1 with atypical symptoms as headaches, dizziness, fall attacks with and without loss of consciousness, and 1 patient with a lesion incidentally discovered. Therefore, the aggressive presentation rate of this group reached the 91.5 %.
Overall, the distribution of AP differed significantly between the groups (p value < 0.001). The presence of each angioarchitectural feature (D, E, and S) significantly more often led to AP as compared to lesions with absence of these features (nD, nE, and nS) (Table 2).
A collective diagrammatic representation of the distribution of clinical presentations among the groups is presented in Fig. 1.
Diagrammatic representation of the distribution of clinical presentations among the groups, displayed according to the AP risk, from lowest (left) to highest (right). Their angioarchitecture, described in DES terms, appears at the bottom of the columns. At the top of the columns, the alternative description (DSS, ISS, BVS) is shown. The dural sinus shunt (DSS) groups correspond to the Borden type 2 lesions, the ISS groups correspond to the isolated sinus shunts variety of DSS (Borden type 3), and the BVS groups, to the bridging vein shunts (Borden type 3). The D-nE-nS and D-nE-S groups are not shown due to rarity. The benign presentations appear in green color. The gray colors symbolize an intermediate clinical presentation. The light gray color under the name “CND” represents the cases presenting with cranial nerve deficits. The dark gray color represents the cases presented with episodic neurological manifestations (NM). The dark red “aggressive-H” presentation stands for hemorrhage, whereas the red “aggressive-PND” for progressive neurological deficit. This chart summarizes the main results of the study. Overall, on the left side, the three groups with lower AP have no venous strain (nS), whereas the three groups on the right side have venous strain (S). The sequence of types according to AP remains the same on both sides: DSS, ISS, BVS. Sinus-based shunts (DSS) with non-exclusive LVD and without venous strain had 0 % AP. On the other end of the spectrum, the bridging vein shunts (BVS) with venous strain were the most aggressive with 91.5 % AP. In the middle, the bridging vein shunts without venous strain and the sinus shunts with venous strain, have a moderate frequency of AP (54 and 55.5 %, respectively). The ISSs and BVSs with venous strain differ significantly in the percentage of hemorrhage (20 vs. 75 %, respectively)
The ISSs (nD-E-nS + nD-E-S) in comparison to BVSs (D-E-nS + D-E-S), both with exclusive LVD, had significantly less aggressive presentation, overall 50 vs. 81.5 % (p value 0.007). The ISS with venous strain (group nD-E-S) in comparison with the corresponding BVS with venous strain (group D-E-S), despite that they both showed a high rate of overall aggressive presentation, the hemorrhages, were significantly lower in the sinus-based shunts, 20 vs. 75 % (p value 0.002).
Among the “S” groups (with venous strain), the presence of ectasia was significantly associated with hemorrhage (p value <0.001) whereas the presence of congestion was significantly associated with PND (p value 0.04) (Table 3).
Among the four dural sinus shunt groups (all the nD ones) the transverse and/or sigmoid sinuses were the most common locations (76 %), with the cavernous sinus being the second most common site (Table 4). As seen in Table 5, the tentorial BVs together with petrosal BVs were, by far, the most frequent locations of the BV shunts. In addition, tentorial shunts, being BV-based shunts, all had a direct and nearly all-exclusive CVD. All ethmoidal shunts had also a direct and exclusive CVD.
The four ethmoidal dural shunts of the D-E-S group showed an overall aggressive presentation 50 % (both bleedings) and one NM. From the five ethmoidal cases of the D-E-nS group, none presented with bleeding, one was incidentally discovered, three presented with benign symptoms, and one with epilepsy. The rate of aggressive presentation of the ethmoidal dural shunts was markedly lower in comparison to the general rate of the corresponding groups, namely 0 vs. 54 % (p value 0.12) and 50 vs. 91.5 % (p value 0.09) for the nS and S varieties, respectively. The distribution of the two subtypes of anterior cranial fossa shunts (ethmoidal BV shunts and cribrosal shunts) among the S and nS groups and their presentation were not studied, since their small numbers did not allow further analysis.
There was no significant difference between sex distribution comparing sinus vs. BV lesions (72 % with BVS and 60 % with DSS were men; p value 0.28).
The interobserver agreements on the three main angioarchitectural features were per definition perfect for directness and exclusivity, with Cohen kappa coefficients 0.96 and 0.91, respectively, and substantial for venous strain patterns, with kappa coefficient of 0.69.
Discussion
In many CDAVF studies, hemorrhages, focal or global neurological deficit, and neurological manifestations including TIA and epilepsy, are deemed as an aggressive presentation, whereas cranial nerve palsy and visual impairment due to glaucoma are grouped together with headache, tinnitus, and orbital phenomena in the benign spectrum of symptoms [19, 26, 9]. This consideration about the benign or aggressive nature of symptoms is mostly based on the relation of the symptoms to the central (CNS) vs. peripheral nervous system (PNS), which certainly has a value. However, from a purely clinical point of view (as we are dealing with clinical presentation), we should notice that an epileptic attack in terms of severity and impact is very dissimilar from an intracerebral bleeding, although both are related to the CNS. On the other hand, the clinical impact of diplopia and glaucoma with impaired vision is certainly different than the impact of tinnitus, with the former always receiving urgent medical attention. Hence, we decided to abandon the dipole benign-aggressive, evocative of a black-white approach and consider epileptic attacks and TIAs as episodic neurological manifestations having an intermediate severity and mostly representing warning features. We found this standpoint more close to a balanced and realistic clinical approach. We also think that categorizing cranial nerve deficits as benign symptoms, although widely accepted, cannot be really justified. These symptoms, although related to the PNS, should rather be grouped in a gray zone with the intermediate symptoms from the central nervous system rather than in the benign spectrum, due to their disabling nature. A view of the clinical presentation distribution among the groups based on the above consideration appears in Fig. 1. Additionally and contrary to previous studies [9, 25], we did not count incidental discovery in the benign presentation because we deemed that it does not amount to presentation; we considered that incidental discovery happens before the lesion develops symptoms, which can be either aggressive or benign, regardless.
Our results demonstrated that among CDAVFs with LVD, there are significant angioarchitectural differences, which are reflected by considerable differences in clinical presentation. LVD of sinus-based shunts that is neither direct nor exclusive and without venous strain is not expected to present aggressive symptoms. On the other end of the spectrum, the BV-based shunts with direct and exclusive LVD and venous strain will present aggressively almost always and most likely with bleeding.
The most aggressive of the sinus shunts, those with exclusive LVD and venous strain (corresponding to an ISS with cortical venous strain), despite the fact that they showed a high rate of overall aggressive presentation, the hemorrhage rate, in comparison to a BV shunt with cortical venous strain, was significantly lower. This shows that the most aggressive BVSs present more frequently with hemorrhage, whereas the most aggressive DSSs present more frequently with PND.
Another interesting point to mention was the fact that nearly all BVSs had an exclusive LVD at the time of diagnosis. Only four patients had non-exclusive LVD, and none of them presented with bleeding. The first case was discovered incidentally; the flow to the transverse sinus was distinguishable only during a superselective injection, which speaks for a rather low flow. The second lesion, similar to the first, was a temporal BV shunt with some residual drainage to the transverse sinus, presented with tinnitus (and suspicion of focal epileptic attack). The third case was a shunt of a superior convexial parietal BV. Although the exit of the BV to the sinus was still patent, there was a medullary venous reflux due to lack of superficial collaterals of that particular vein. This explains why the patient presented with epilepsy, while flow still existed to the sinus at the time of presentation. The fourth case was a shunt of the superior petrosal vein with its exit to the superior petrosal sinus and cavernous sinus not completely occluded. Despite the ectatic changes of the draining vein, the presentation was still benign with headache and dizziness. Most likely, when the BV-exit to the sinus is still available, the existing leptomeningeal venous hypertension is far from its zenith, which matches for the incidental discovery of the first and the still benign presentation of the second and fourth cases. The D-nE shunts (S and nS included) could be considered a transitional phase in the development of BVSs, presumably towards exclusive and aggressively symptomatic LVD. Accordingly, the small number of these groups (D-nE-nS and D-nE-S) should not be considered a particularity of our series or weakness of the DES concept. On the contrary, it should be deemed as a merit of the concept since it captures a relatively silent phase of otherwise aggressive shunts, reflecting thus the dynamic nature of these lesions.
The distribution of intermediate presentation (IP) among the groups showed that (1) BVSs did not present with cranial nerve deficits. The fact that these symptoms were recorded only in patients with DSS without venous strain seems primarily location-specific (all CS shunts belonged to the nD-nE-nS and nD-E-nS groups) and not grade-specific. (2) Among the nS shunts, only the BVSs presented with NM and indeed in a remarkable proportion of 23 %. In other words, BVSs even without venous strain showed a high rate (77 %) of non-benign (AP + IP) presentation. (3) The ISSs with venous strain can manifest themselves with warning symptoms (IP 20 %). (4) The BVSs with venous strain rarely showed warning symptoms (IP only 5.5 %).
All cases with non-exclusive LVD correspond to Borden type 2 lesions and the cases with exclusive LVD belong to Borden type 3. If we exclude the ISS from the Cognard types III and IV, then our D-E-nS group corresponds to the Cognard type III and the D-E-S group with the type IV. We see that within the Borden type 2 lesions, as a consequence of significant differences in angioarchitecture, there are considerably divergent clinical expressions; both nD-nE-nS and nD-nE-S groups belong to the Borden type 2 with 0 and 55.5 % aggressive presentation, respectively. Therefore, the fact that some lesions with LVD have a benign presentation, in contrast to other lesions with LVD, is absolutely tenable since LVD alone does not appear to be the determining factor of the clinical presentation. Directness and exclusivity of the LVD and their impact on the venous system, expressed by concrete signs of failure (ectasia and/or congestion) seem to play the protagonist roles. The cause of this failure may be primarily dependent on the collateralization [7] of the affected individual venous system as other authors have hypothesized [26, 25, 4, 23]. Additionally, the factor of time should be always considered in both directions [15]. Other factors and comorbidities such as coagulopathies should also be considered as relevant in some cases [21]. The causative relation of the bleeding contralateral to the lesion in one patient of the nD-E-nS group remains unclear although it was included in the analysis. The other patient of the same group was considered as an incidental discovery since the bleeding at presentation could be better attributed to the underlined coagulopathy.
In the literature, it is often mentioned that the mode of presentation is intrinsically linked to the shunt topography; with classic examples, the anterior cranial fossa and tentorium, both locations linked to an aggressive presentation [1, 19, 20, 12, 14, 22, 28]. Our study shows that topography, being intrinsically linked to a specific venous anatomy, determines the angioarchitectural features of the dural shunts, which ultimately dictate the clinical presentation (Tables 4 and 5).
The groups without venous strain (nS) showed the lowest AP rate in comparison with the groups with venous strain (S). Among the three nS and three S groups, the DSSs showed the lowest AP rates and the BVSs the highest AP rates (see Fig. 1). It seems that venous strain is a strong determinant of an aggressive clinical behavior, reasonably enough, since venous strain signifies the disarrangement of the venous system. This disarrangement can be focal and structural, expressed by ectatic lesions, or more regional and functional, expressed by venous congestion and stagnation. The importance of venous ectasia and its correlation with risk of bleeding has been previously demonstrated [4, 5]. Bulters et al. have actually expressed their thoughts about a potential simple classification of CDAVFs based only on the presence of venous ectasia. Our results advocate a way of analysis and concretely, the DES concept, which takes venous strain very seriously into consideration but not as the only criterion and the ectasia not as the only expression of venous strain. According to our study, the directness of the LVD correlates with the ectatic version of the venous strain, which is linked to hemorrhagic presentation; which makes absolute sense. On the other hand, a non-direct shunt, as in the case of ISS, appears more related to the congestive, regional version of venous strain, which is linked mostly with non-hemorrhagic neurological deficits; which also makes sense because a shunt of an isolated sinus segment empties indirectly and often into more than one BV.
Interestingly, the rate of aggressive presentation of the ethmoidal dural shunts, although by definition they belong to the D-E groups, was considerably lower in comparison to the general rate of the groups, for the nS and S varieties, respectively. We found no apparent reason explaining this. The peculiar venous anatomy with spinal cord-like bridging-emissary vein [17] configuration and bidirectional flow in the area of the lamina cribriformis may play a role. Also, the ethmoidal BVS subtype of this group may show a tendency for aggressive presentation in comparison to the cribrosal subtype of the same group, but the numbers were too small for further analysis.
Recently, Shin et al. [23] analyzed the angioarchitectural venous features of a series of 41 CDAVFs and found that ISS had an aggressive presentation in all cases (100 %) and a hemorrhagic presentation in 20 % of cases, although they did not correlate these percentages with presence or absence of ectasias and congestion in the above cases. Their results are in accordance with ours regarding the hemorrhagic presentation (ours 23.5 %), but contradict with our overall aggressive presentation of 65 % for both ISS groups. For the lesions with direct CVD, they found an overall aggressive presentation similar to ours (89 vs. 92 % if we sum our aggressive presentations with NM, as they did) but significantly lower hemorrhagic presentation, i.e., 33 vs. 61 % (the average for our two groups with direct LVD). These discrepancies may reflect population bias or differences in angiographic analysis of the cases. They also found that “brisk drainage” reported in 14/41 cases, was correlated with benign presentation, in contrary to the pseudophlebitic appearance of the draining veins reported in 30/41, which was correlated with aggressive presentation. The above implies that three patients had both brisk drainage and pseudophlebitic draining veins, which was not specifically analyzed. Regarding the involvement of a long network of cortical veins in the drainage of a CDAVF, they concurred with previous observations [10] that patients with aggressive presentation were significantly associated with a longer length of LVD. An exact definition of “length” and reliable way of measurement were not provided. Although similar data were not collected in the current study, the above observation can be warranted since it reflects the collateralization capacity of the regional venous system and more concretely, the availability of a short-course collateral venous exit to the nearest sinus.
The assumption that different clinical presentations of CDAVFs with LVD may signify a different clinical course was based on the observation that some CDAVFs with LVD had an aggressive presentation and others, not [25, 24]. A reasonable question is whether this observation is well supported and if, in fact, the shunts with aggressive presentation are the same lesions with those presenting with a benign mode. As our results showed and other authors noted, LVD as the only criterion for prediction of clinical presentation is not enough [25], since, e.g., nD-nE-nS lesions in comparison with D-E-S lesions have a huge difference in terms of architecture and clinical presentation.
Strom et al. [25] reported that CDAVFs with LVD presented with benign symptoms or incidentally, may have a less aggressive clinical course than those that presented with bleeding and neurological deficit. However, their study had some weaknesses. Their conclusions were based on 17 cases of the benign presentation group and 11 cases of the aggressive presentation group. Regarding the former group, a methodological weakness was the inclusion of seven incidentally discovered lesions (41 %), despite the fact that one of the incidentally discovered shunts presented later with bleeding, after refusing treatment. Six of these seven incidental lesions were Borden type 3; in total, eight lesions were Borden type 3. No data about ISS were provided. The above would mean that 6/8 shunts (75 %), which had the higher potential of an aggressive presentation, at the time of diagnosis had not expressed it yet since they were discovered incidentally. Looking at the locations of Borden type 3 lesions, three shunts (“transverse,” “sigmoid,” “torcular”) appeared to be likely sinus-based lesions (ISS), two were likely BV shunts (“clivus” and “petrous”) whereas the location of three shunts was non-specifically recorded (“occipital area,” “frontal region,” and “cranial base”). If we accept the above assumption correlating the described location with the nature of the lesion (sinus vs. BV shunt), then the BV shunts, which have a direct and mostly exclusive LVD and are expected to have a more aggressive presentation than a sinus shunt, counted only up to 25 % of the Borden 3 lesions and 12 % of the entire group of benign presentation. Moreover, only 1 shunt of the 17 had signs of venous strain and was described as Cognard type IV. Venous strain phenomena were recorded for none of the nine Borden type 2 lesions, unknown if because none of the used classifications anticipate such phenomena for type 2 lesions or because none had one. According to our findings, lesions without venous strain are expected to have relatively benign presentation. Such lesions may be expected to continue having a benign clinical behavior as long as their architecture, which mostly determines their presentation, does not change. In the same report by Strom et al., the group of aggressive presentation comprised five Borden type 2 shunts and six Borden type 3 shunts, of those one Cognard type IV and one type V. Looking at the locations of the Borden type 3 lesions, four shunts (two “tentorium”, two petrous) appear most likely as BV lesions and two (transverse) likely as ISS. Again, if we accept the above assumption correlating the described location with the nature of the lesion as presumably true, then the BV lesions, with the higher potential to present aggressively, made up 66.5 % of the Borden 3 lesions (vs. 25 % of the benign presentation group) and 36 % of the entire group of aggressive presentation (vs. 12 % of the benign presentation group). Therefore, the inhomogeneity of the groups, defined only on the base of presence of LVD, and the above-presumed difference in the percentage of BV shunts between the benign and aggressive presentation group, might be the reason for this distinct clinical expression. Apart from the above-analyzed weaknesses, Strom et al. did note that LVD might not be a reliable indicator of cortical venous hypertension, an observation supported by our study. Further, they suggested that less flow through the fistula, more efficient collateral pathways, or other factors at a microvascular level, may explain why lesions with LVD have a non- or less aggressive presentation, but failed to refer to the heterogeneity of the “LVD group” itself as a confounding factor.
Söderman et al. [24], in their study on natural history of dural shunts, similarly, analyzed their population by mixing together lesions with exclusive and non-exclusive LVD. Of the eight Borden type 2 shunts presented with hemorrhage, no data were provided about venous ectasia or pseudophlebitic venous congestion. Of the 29 Borden type 3 shunts having a non-hemorrhagic presentation, no data were provided about number of lesions belonging to the ISS group.
The clinical presentation, as an additional criterion of a classification system [28], linked to treatment recommendations, implies that presentation should be considered a determining factor of the clinical course, independent from the anatomic background of the lesion. We consider clinical presentation as inherently linked to the anatomic background [19, 18]. If we contemplate a cause-effect scheme for the analysis and prediction of behavior of these lesions, and we accept that anatomy and angiographic features of a shunt belong to the cause-side and the clinical presentation and course to the effect-side, then the above attempt [28] is equivalent to a partial displacement of the effect- into the cause-side, just to make our predictions about future effect more successful instead of analyzing the cause-side further. Moreover, the predictive value of such an analysis and classification for incidentally discovered lesions would be, by definition, void. Furthermore, if we accept that incidental discovery should be counted as benign presentation, then a classification taking into account a thus defined clinical presentation, would be misleading. Our study shows that angioarchitectural features, previously ignored as distinct factors, can further explain the different clinical expressions within the largely inhomogeneous group of lesions with LVD. Failure to identify these factors in angiographic analyses and to recognize them as determinants of the clinical presentation and (most likely) course, may in fact make the use of the clinical presentation criterion “necessary” although conceptually inconsequent.
The substantial (but non-perfect) interobserver agreement concerning the description of venous strain features reflects the relative subjectivity in the comprehension and application of defined criteria in complex cases. The analysis of data by two readers aimed to diminish this limitation. We consider the factor of angiographic analysis of images as the major limitation of the current, as well as every study of this kind.
Conclusions
CDAVFs with LVD constitute a wide and inhomogeneous group of lesions with significant angioarchitectural differences reflected by considerable differences in clinical presentation. Instead of trying to elaborate the clinical course of CDAVFs by considering their initial clinical expression, which is rather a tautology, the DES scheme allows a more concrete analysis of their angioanatomic features based on the factors of directness and exclusivity of LVD in combination with signs of significant cortical venous strain. This way of analysis, in contrary to the currently used classifications, enables the recording of differences among the subgroups and may sufficiently provide the necessary criteria for prediction of the clinical presentation and course of these lesions, and furthermore the indications for treatment.
References
Awad IA, Little JR, Akarawi WP, Ahl J (1990) Intracranial dural arteriovenous malformations: factors predisposing to an aggressive neurological course. J Neurosurg 72(6):839–850. doi:10.3171/jns.1990.72.6.0839
Baltsavias G, Valavanis A (2014) Endovascular treatment of 170 consecutive cranial dural arteriovenous fistulae: results and complications. Neurosurg Rev 37(1):63–71. doi:10.1007/s10143-013-0498-2
Borden JA, Wu JK, Shucart WA (1995) A proposed classification for spinal and cranial dural arteriovenous fistulous malformations and implications for treatment. J Neurosurg 82(2):166–179. doi:10.3171/jns.1995.82.2.0166
Bulters DO, Mathad N, Culliford D, Millar J, Sparrow OC (2012) The natural history of cranial dural arteriovenous fistulae with cortical venous reflux—the significance of venous ectasia. Neurosurgery 70(2):312–318. doi:10.1227/NEU.0b013e318230966f, discussion 318–319
Cognard C, Gobin YP, Pierot L, Bailly AL, Houdart E, Casasco A, Chiras J, Merland JJ (1995) Cerebral dural arteriovenous fistulas: clinical and angiographic correlation with a revised classification of venous drainage. Radiology 194(3):671–680
Duffau H, Lopes M, Janosevic V, Sichez JP, Faillot T, Capelle L, Ismail M, Bitar A, Arthuis F, Fohanno D (1999) Early rebleeding from intracranial dural arteriovenous fistulas: report of 20 cases and review of the literature. J Neurosurg 90(1):78–84. doi:10.3171/jns.1999.90.1.0078
Duvernoy HM, Delon S, Vannson JL (1981) Cortical blood vessels of the human brain. Brain Res Bull 7(5):519–579
Gaston A, Chiras J, Bourbotte G, Leger JM, Guibert-Tranier F, Merland JJ (1984) Meningeal arteriovenous fistulae draining into cortical veins. 31 cases. J Neuroradiol J Neuroradiol 11(3):161–177
Geibprasert S, Pereira V, Krings T, Jiarakongmun P, Toulgoat F, Pongpech S, Lasjaunias P (2008) Dural arteriovenous shunts: a new classification of craniospinal epidural venous anatomical bases and clinical correlations. Stroke 39(10):2783–2794. doi:10.1161/strokeaha.108.516757
Geibprasert S, Pongpech S, Jiarakongmun P, Shroff MM, Armstrong DC, Krings T (2010) Radiologic assessment of brain arteriovenous malformations: what clinicians need to know. Radiograph: Rev Publ Radiol Soc N Am Inc 30(2):483–501. doi:10.1148/rg.302095728
Gross BA, Du R (2012) The natural history of cerebral dural arteriovenous fistulae. Neurosurgery 71(3):594–602. doi:10.1227/NEU.0b013e31825eabdb, discussion 602–593
Halbach VV, Higashida RT, Hieshima GB, Wilson CB, Barnwell SL, Dowd CF (1990) Dural arteriovenous fistulas supplied by ethmoidal arteries. Neurosurgery 26(5):816–823
Hothorn T, Hornik K, van de Wiel MA, Zeileis A (2006) A lego system for conditional inference. Am Stat 60(3):257–263. doi:10.1198/000313006X118430
King WA, Martin NA (1992) Intracerebral hemorrhage due to dural arteriovenous malformations and fistulae. Neurosurg Clin N Am 3(3):577–590
Lasjaunias P (1997) Editorial comment on Davies' papers. Angioarchitecture and natural history of dural arteriovenous shunts. Interv Neuroradiol 3(4):313–317
Lasjaunias P (1997) Vascular diseases in neonates, infants and children: interventional neuroradiology management. Springer, Berlin
Lasjaunias P, Berenstein A, ter Brugge K (2001) Surgical neuroangiography: clinical vascular anatomy and variations, vol 1, 2nd edn. Springer, Berlin
Lasjaunias P, Berenstein A, ter Brugge K (2001) Surgical neuroangiography: dural arteriovenous shunts, vol 2.2, Springer
Lasjaunias P, Chiu M, ter Brugge K, Tolia A, Hurth M, Bernstein M (1986) Neurological manifestations of intracranial dural arteriovenous malformations. J Neurosurg 64(5):724–730. doi:10.3171/jns.1986.64.5.0724
Malik GM, Pearce JE, Ausman JI, Mehta B (1984) Dural arteriovenous malformations and intracranial hemorrhage. Neurosurgery 15(3):332–339
Peng T, Liu A, Jia J, Jiang C, Li Y, Wu Z, Yang X (2014) Risk factors for dural arteriovenous fistula intracranial hemorrhage. J Clin Neurosci : Off J Neurosurg Soc Australas 21(5):769–772. doi:10.1016/j.jocn.2013.07.024
Pierot L, Chiras J, Meder JF, Rose M, Rivierez M, Marsault C (1992) Dural arteriovenous fistulas of the posterior fossa draining into subarachnoid veins. AJNR Am J Neuroradiol 13(1):315–323
Shin NY, Kwon YS, Ha SY, Kim BM, Kim DI, Kim DJ (2013) Venous angioarchitectural features of intracranial dural arteriovenous shunt and its relation to the clinical course. Neuroradiology 55(9):1119–1127. doi:10.1007/s00234-013-1222-1
Soderman M, Pavic L, Edner G, Holmin S, Andersson T (2008) Natural history of dural arteriovenous shunts. Stroke 39(6):1735–1739. doi:10.1161/strokeaha.107.506485
Strom RG, Botros JA, Refai D, Moran CJ, Cross DT 3rd, Chicoine MR, Grubb RL Jr, Rich KM, Dacey RG Jr, Derdeyn CP, Zipfel GJ (2009) Cranial dural arteriovenous fistulae: asymptomatic cortical venous drainage portends less aggressive clinical course. Neurosurgery 64(2):241–247. doi:10.1227/01.neu.0000338066.30665.b2, discussion 247–248
van Dijk JM, terBrugge KG, Willinsky RA, Wallace MC (2002) Clinical course of cranial dural arteriovenous fistulas with long-term persistent cortical venous reflux. Stroke 33(5):1233–1236
Willinsky R, Goyal M, terBrugge K, Montanera W (1999) Tortuous, engorged pial veins in intracranial dural arteriovenous fistulas: correlations with presentation, location, and MR findings in 122 patients. AJNR Am J Neuroradiol 20(6):1031–1036
Zipfel GJ, Shah MN, Refai D, Dacey RG Jr, Derdeyn CP (2009) Cranial dural arteriovenous fistulas: modification of angiographic classification scales based on new natural history data. Neurosurg Focus 26(5):E14. doi:10.3171/2009.2.focus0928
Acknowledgments
We wish to thank Professor V. Runge for his valuable comments on the manuscript and knowledgeable suggestions.
Conflict of interest
We declare that we have no conflict of interest.
Financial support
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Michihiro Tanaka, Kamogawa City, Japan
Directness and exclusivity of leptomeningeal venous drainage and signs of venous strain were well described in corresponding to each angiographic feature in terms of clinical manifestation of CDAVFs. The discussion of clinical appearance and the existing of parenchymal venous congestion or incidence of intracerebral hemorrhage is well appreciated. Tentorial and petrosal BVs, as well as ethmoidal location, are highly associated with the category of D-E-S. These locations are characterized as the lateral epidural space group in the classification of Geibprasert, and the malignancy of this group has been already discussed.
Karel terBrugge, Toronto, Canada
Dr. Baltsavias and the Zurich team are to be complemented on the in-depth analysis of their extensive experience with DAVS and using it to modify to interpret more accurately the to-be-expected risks of those DAVS that are associated with so called “cortical venous reflux.” In their analysis, it became clear that additional factors influenced expected clinical risk and they included the presence of direct (D) and exclusive (E) retrograde leptomeningeal reflux (LVR) as well as evidence of venous strain (S). By analyzing each of the factors individually and in combination, it became clear that further stratification of the clinical risks in the natural history of DAVS with LVR could be accomplished. This, in turn, should be helpful to understand and manage patients with DAVS with LVR including those that are incidentally discovered.
Rights and permissions
About this article
Cite this article
Baltsavias, G., Spiessberger, A., Hothorn, T. et al. Cranial dural arteriovenous shunts. Part 4. Clinical presentation of the shunts with leptomeningeal venous drainage. Neurosurg Rev 38, 283–291 (2015). https://doi.org/10.1007/s10143-014-0595-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-014-0595-x