Abstract
Purposes
The present study investigated the prognostic value of inflammation-based prognostic scores in patients with hepatocellular carcinoma (HCC) who underwent hepatectomy.
Methods
In total, 493 patients diagnosed HCC using the Milan criteria who underwent hepatic resection were retrospectively analyzed. Patients were evaluated according to several prognostic nutrition indices. Univariate and multivariate analyses were performed to identify clinicopathological variables associated with the overall survival (OS).
Results
According to a univariate analysis, higher values in the Glasgow Prognostic Score [GPS] (hazard ratio [HR] = 1.99, p = 0.002), modified GPS [mGPS] (HR = 2.26, p < 0.001), C-reactive protein [CRP]-to-albumin ratio [CAR] (HR = 1.86, p = 0.0012), and CONUT (HR = 1.65, p = 0.008) and a lower value of prognostic nutritional index [PNI] (HR = 2.36, p < 0.001) were significantly associated with a poor OS. A multivariate analysis showed that a CAR ≥ 0.037 (HR = 1.67, 95% CI 1.06–2.64, p = 0.03), FIB4-index > 3.25 (HR = 1.98, 95% confidence interval [CI] 1.25–3.14, p = 0.004) and PIVKA-II > 40 mAU/ml (HR = 1.72, 95% CI 1.14–2.61, p = 0.01) were independent prognostic factors.
Conclusions
This study demonstrated that the CAR was an independent prognostic score in patients with HCC and superior to other inflammation-based prognostic scores in terms of the prognosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary liver cancer is the sixth-most frequently diagnosed cancer worldwide and the fourth leading cancer-related death. An estimated 840,000 new liver cancer cases and 782,000 liver cancer-related deaths occurred in 2018. By region, it is relatively common in developing countries, mainly North and West Africa and East and Southeast Asia, and its incidence is expected to increase in the future.
Hepatocellular carcinoma [HCC] comprises 75–85% of primary liver cancer cases. The main risk factors for HCC are chronic infection with hepatitis B virus [HBV] or hepatitis C virus [HCV]. In some areas, although the number of infected patients is decreasing due to vaccination and treatment with antiviral drugs, the rates of liver cancer are increasing due to obesity [1,2,3,4,5]. Treatment of HCC is not limited to surgical resection but includes various treatment methods, such as transcatheter arterial radiofrequency ablation [RFA], transcatheter arterial chemoembolization [TACE], and systemic chemotherapy. Thanks to the development of such treatment modalities, the prognosis of patients with HCC is improving, but it is still unsatisfactory.
In recent years, it has been reported for various types of cancers that inflammation-based scores are associated with resistance to multidisciplinary treatments, complication rate, and the prognosis [6]. The GPS, mGPS, CAR, neutrophil-to-lymphocyte ratio [NLR], platelet-to-lymphocyte ratio [PLR], prognostic index [PI], and PNI have all been reported to be associated with the prognosis of patients with various types of cancers [7,8,9,10,11,12,13]. In addition to biomarkers, such as CRP and platelets that reflect the inflammatory response, neutrophils and lymphocytes that reflect immunity, and albumin that reflects protein metabolism, the CONUT score, which includes cholesterol levels that reflect lipid metabolism, has also been reported to be associated with the prognosis and risk of perioperative complications in various types of cancers [14,15,16,17].
Although there have been reports of collecting and comparing several inflammation-based scores, which inflammation-based prognostic scores are more suitable for predicting outcome in patients with HCC has not been fully elucidated. Therefore, in this study, we calculated eight preoperative inflammation-based prognostic scores (GPS, mGPS, CAR, NLR, PLR, PI, PNI, and CONUT) and examined the independent prognostic factors in patients with HCC according to the Milan criteria who underwent first liver resection.
Materials and methods
Study population
All consecutive patients who underwent first hepatic resection for HCC according to the Milan criteria at Kumamoto University Hospital (Kumamoto City, Japan) from January 2000 to December 2019 were enrolled. We excluded patients who underwent preoperative therapy, such as systemic chemotherapy, TACE, RFA, and R1 or R2 resection, from our study cohort.
The patients underwent imaging studies, such as ultrasonography, dynamic computed tomography [CT], and enhanced magnetic resonance imaging (MRI), for the primary liver cancer diagnosis and staging before surgery. All patients had pathologically confirmed diagnoses of HCC after surgery.
All patients gave their written informed consent, and the Ethics Committee of Kumamoto University approved this study's protocol. Our institutional ethical review board approved this study (IRB No.1291), and all procedures met the guidelines of the Declaration of Helsinki.
The diagnosis was to be based on the typical hallmarks of HCC, such as hypervascularity in the arterial phase with washout in the portal venous or delayed phase. Tumor-related variables, such as the maximal tumor diameter, tumor number, vascular invasion, and extrahepatic metastasis, were evaluated by the above-mentioned imaging techniques. Pathological findings were prospectively documented according to the pathological tumor (T), node (N), and metastasis (M) classifications and were relabeled according to the Union for International Cancer Control (UICC) reporting format for the HCC, eighth edition [18].
Inflammation-based prognostic scores and other variables
Blood samples were obtained before surgery to measure the values of CRP, albumin, aspartate aminotransferase [AST], alanine aminotransferase [ALT], total bilirubin, white blood cells, neutrophils, lymphocytes, platelets, prothrombin time [PT], α-fetoprotein [AFP], AFP-L3 fraction, protein induced by vitamin K absence or antagonist II [PIVKA-II], indocyanine green retention rate at 15 min [ICG-R15], and FIB-4, which combines standard biochemical values (platelets, ALT, AST) and age as a marker of fibrosis [19]. The type of resection (laparoscopic or not, anatomical or not), GPS, mGPS, NLR, PLR, CAR, PI, PNI, and CONUT were collected as described in Table 1.
Statistical analyses
Continuous variables were expressed as the mean ± standard deviation or the median (interquartile range) according to the data type (parametric or non-parametric, respectively); differences were assessed for significance using Student's t test or the Mann–Whitney test. Categorical variables were evaluated using the Chi-squared or Fisher’s exact tests, as appropriate. Survival analyses were performed using the Kaplan–Meier method, with comparisons using the Cox proportional hazards model. The overall survival [OS] was calculated from the date of surgery until death or last follow-up. p < 0.05 was considered to indicate statistical significance. Univariate and multivariate analyses were performed for the prognostic factors using the Cox proportional hazard model. Variables that proved to be significant in the univariate analysis were tested subsequently with the multivariate Cox proportional hazard model.
All statistical analyses were performed using JMP software program, version 14.3 (SAS Institute, Cary, NC, USA).
Results
Patient characteristics
The baseline characteristics of the patients are shown in Table 2. The median age was 69 (range 38–87) years-old. Three hundred and seventy-four (75.3%) patients were males, and 123 (24.7%) were females. The median body mass index [BMI] was 23.3 (11.6–39.6). Two hundred and fifty-three (50.9%) patients were positive for antibodies to HCV antibody (HCV-Ab), and 106 (21.3%) were positive for HBV surface antigen (HBs-Ag). Four hundred and sixty patients (92.6%) had Child–Pugh classification A grade. The median value of ICG-R15 was 12.0% (0.6–65.4%). One hundred and sixty-eight patients (33.8%) had laparoscopic resection. Two hundred and seventy-seven patients (55.7%) received anatomical resection. The median FIB4-index was 3.21 (0.15–27.9). Four hundred and twenty-seven (85.9%) patients had GPS 0, and 70 (14.1%) had GPS 1 or 2. Similarly, 412 (82.9%) patients had mGPS 0, and 85 (17.1%) had mGPS 1 or 2. The cutoff values of inflammation-based scores were set based on previous reports (NLR = 5, PLR = 150, CAR = 0.037, and PNI = 45) [9, 20]. Four hundred and sixty-two patients (93.0%) had NLR < 5, 425 (85.5%) had PLR < 150, and 381 (76.7%) had PNI ≥ 45. Four hundred and eighty-three patients (97.2%) had PI 0, and 14 (2.8%) had PI 1 or 2. Regarding CONUT scores, 260 patients (52.3%) had normal nutrition, 209 (42%) were in the light nutrition group, and 28 (5.7%) were in the moderate nutrition group.
Impact of inflammation-based scores on the prognosis
The median follow-up was 51.2 months. Three hundred and eighty-three patients (77.1%) were alive at the end of the follow-up period, while 104 patients (22.9%) had died. The 1-, 3-, and 5-year OS rates were 96.6%, 88.7%, and 81.1%, respectively.
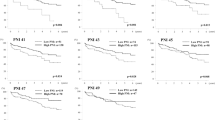
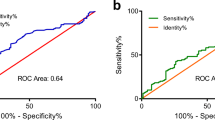
The relationships between the inflammation-based prognostic scores and OS are shown in Fig. 1a–h. Higher values for the GPS (5-year OS = 83.7%, hazard ratio [HR] = 1.99, p = 0.002), mGPS (5-year OS = 84.5%, HR = 2.26, p < 0.001), and CAR (5-year OS = 82.6%, HR = 1.86, p = 0.0012) and light + moderate + severe CONUT (5-year OS = 88.1%, HR = 1.65, p = 0.008) and lower PNI values (5-year OS = 86.5, HR = 2.36, p < 0.001) were associated with a significantly worse OS than other values, but the NLR (5-year OS = 81.6%, HR = 2.01, p = 0.09), PLR (5-year OS = 81.1%, HR = 1.36, p = 0.25), and PI (5-year OS = 81.6%, HR = 0.85, p = 0.78) showed no such association.
A univariate analysis showed that HBs-Ag status (HR = 0.59, p = 0.032), HCV-Ab status (HR = 1.55, p = 0.021), PIVKA-II (HR = 1.58, p = 0.019), ICG-R15 (HR = 1.84, p = 0.0063), Child–Pugh grade (HR = 1.93, p = 0.0479), maximal tumor diameter (HR = 1.51, p = 0.037), FIB4-index (HR = 2.22, p < 0.0001), GPS (HR = 1.99, p = 0.0025), mGPS (HR = 2.26, p < 0.0001), CAR (HR = 1.86, p = 0.0016), PNI (HR = 2.36, p < 0.0001), and CONUT (HR = 1.65, p = 0.0081) were significantly associated with the OS. The cutoff values of these variables ware set based on the median values for this cohort, except for the inflammation-based prognostic scores.
A multivariate analysis using these variables showed that high values for the FIB4-index (HR = 1.98, 95% CI 1.25–3.14, p = 0.004), CAR (HR = 1.67, 95% CI 1.06–2.64, p = 0.03), and PIVKA-II (HR = 1.72, 95% CI 1.14–2.61, p = 0.01) were independently associated with a poor OS (Table 3).
Discussion
This study investigated the prognostic value of various inflammation-based prognostic scores in patients with HCC who underwent hepatectomy. It demonstrated that the CAR was an independent poor prognosis marker in patients with HCC and was superior to the other inflammation-based scores examined (GPS, mGPS, NLR, PLR, PI, PNI, and CONUT) in terms of its prognostic predictive ability.
Host-tumor interaction between local and individual cancers is known to have a substantial effect on the general condition, such as the nutritional status and immunocompetence, of cancer patients [21]. Gullet et al. described nutritional disorders of cancer patients as cancer-related weight loss and cancer-induced weight loss [22]; the former is a reversible pathological condition caused by decreased nutrient intake/digestion and absorption due to physical gastrointestinal dysfunction, such as impaired gastrointestinal passage and diarrhea, or a prolonged fasting period, while the latter is an irreversible condition caused by host–tumor interaction. Although HCC rarely causes passage obstruction in the gastrointestinal tract, it can cause systemic metabolic disorders, and cancer-induced weight loss is considered a frequent cause of nutritional disorders. Thus, nutritional disorders are caused by cancer-induced weight loss in HCC and are associated with a poor prognosis.
The inflammation-based scores compared and examined in this study are roughly composed of three evaluation elements. The first is a value that reflects the inflammatory response, such as CRP, neutrophils, and platelets. CRP is an acute-phase reactant synthesized by hepatocytes and regulated by proinflammatory cytokines, especially interleukin-6 [23]. The CRP level is reportedly associated with tumor progression and a reduced liver function and is an independent poor prognostic marker in patients with HCC [24]. Neutrophils and platelets are typical blood cell components and are factors that closely link inflammation and tumor progression, as inflammation increases and induces the production of chemokines and cytokines that enhance tumor growth, infiltration, and angiogenesis [25,26,27,28,29,30]. The second element is a biomarker that reflects the immune capacity of lymphocytes. Total lymphocyte count is one of the classical nutritional evaluation indexes, and lymphocytes are a blood cell component that act as a tumor suppressor and have an influence on tumor immunity [31,32,33]. The third element is metabolic components, such as albumin and cholesterol. Serum albumin levels are commonly used as an indicator of the nutritional status and are also associated with the immune status and protein metabolism. Low serum albumin levels correlate with increased parameter measures of HCC aggressiveness, in addition to their role as a monitor of systemic inflammation [34]. The accumulation of cholesterol is a general feature of cancer tissue, and recent evidence suggests that cholesterol plays critical roles in the progression of cancers [35]. The dysregulation of metabolic pathways, including those involved in cholesterol biosynthesis, is implicated in tumor development and cancer progression [36]. Furthermore, CRP and albumin are correlated, and CRP levels in cancer patients reflect the amount of IL-6 in the circulating blood, but chronic CRP elevation is accompanied by persistently elevated IL-6 production, which is thought to indicate the amount of inflammation in the cancerous tissue. Furthermore, the increase in IL-6 is directly reflected in the dynamics of acute-phase proteins (APPs), and the representative factor for increasing APPs (positive APPs) is CRP, while conversely, the representative factor for decreasing APP (negative APPs) is albumin. Therefore, GPS, mGPS, and CAR are scoring systems that can reflect the APP dynamics [37].
However, there are some limitations associated with these systems. In addition, we considered other elements that may have been influenced by liver dysfunction such as liver cirrhosis and portal hypertension. We divided these factors roughly into three elements (inflammatory response, immune capacity, metabolic component), but the albumin level and platelet count are affected by the liver function reserve and degree of portal hypertension. In this regard, these inflammation-based scores are not simple indicators of systemic inflammation in patients with chronic liver dysfunction.
In the present study, our univariate analysis demonstrated that the GPS, mGPS, CAR, PNI, and CONUT values were significantly associated with the OS as inflammation-based scores. However, the multivariate analysis showed that only the CAR was independently associated with the OS. Kinoshita et al. [9] demonstrated that the CAR is an independent predictor of a poor OS in patients with HCC at various stages of diseases and with different liver functional statuses. They also showed that the CAR, GPS, and mGPS, which are CRP-based prognostic scores, were superior to the NLR which is a white blood cell-based score, in patients with HCC in terms of their prognostic ability. However, their study did not compare the CAR with the PLR, PI, PNI, or CONUT [9]. The present study is thus the first to have compared various representative inflammatory-based scores, revealing that the CAR is an independent prognostic score.
In our cohort, there were few cases such as a categorized score 2 having high CRP and low albumin, and most patients had scores of 0 or 1 in the GPS and mGPS. Furthermore, patients with low CRP and albumin values are included same score 1 with high CRP and high albumin cases in CAR. The CAR therefore enables a more detailed understanding of the patient status than the GPS or mGPS. The present study also included only cases with HCC that was untreated preoperatively, and all cases were diagnosed according to the Milan criteria. Therefore, the inflammation-based score directly reflected the patient’s condition, and our cohort is homogeneous with few biases. In HCC, scores that indicate the degree of the liver function and inflammation derived from the liver are more useful than scores that use blood cells, such as neutrophils and lymphocytes, or are more dependent on tumor-related factors according to the Milan criteria. Therefore, the usefulness of the CAR was highlighted by the reduced impact of tumor-related factors.
Surgical resection for HCC is the major treatment option, but other treatments for HCC have recently been developed, such as transcatheter arterial chemoembolization (TACE), radiofrequency ablation (RFA), and chemotherapy. CAR can be easily measured by a blood sampling test in the postoperative follow-up process, and it is easy to follow the course over time, so it can be used as a basis to judge the appropriateness of treatments other than surgical resection based on changes in the score.
One potential limitation of the present study is that it was a retrospective design, had a small sample size, and was conducted at a single center. Therefore, our findings need to be validated in a larger-scale prospective study.
In conclusion, we revealed that the CAR was an independent prognostic score in patients who underwent first liver resection for HCC according to the Milan criteria and was superior to other established inflammation-based prognostic scores in terms of its prognostic predictive ability.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
McGlynn KA, Petrick JL, London WT. Global epidemiology of hepatocellular carcinoma: an emphasis on demographic and regional variability. Clin Liver Dis. 2015;19(2):223–38.
Marengo A, Rosso C, Bugianesi E. Liver cancer: connections with obesity, fatty liver, and cirrhosis. Annu Rev Med. 2016;67:103–17.
Chang MH, Chen CJ, Lai MS, Hsu HM, Wu TC, Kong MS, et al. Universal hepatitis B vaccination in Taiwan and the incidence of hepatocellular carcinoma in children. Taiwan Childhood Hepatoma Study Group. N Engl J Med. 1997;336(26):1855–9.
Thursz M, Fontanet A. HCV transmission in industrialized countries and resource-constrained areas. Nat Rev Gastroenterol Hepatol. 2014;11(1):28–35.
Roxburgh CS, McMillan DC. Role of systemic inflammatory response in predicting survival in patients with primary operable cancer. Future Oncol. 2010;6(1):149–63.
Kinoshita A, Onoda H, Imai N, Iwaku A, Oishi M, Tanaka K, et al. The Glasgow Prognostic Score, an inflammation based prognostic score, predicts survival in patients with hepatocellular carcinoma. BMC Cancer. 2013;13:52.
Gomez D, Farid S, Malik HZ, Young AL, Toogood GJ, Lodge JP, et al. Preoperative neutrophil-to-lymphocyte ratio as a prognostic predictor after curative resection for hepatocellular carcinoma. World J Surg. 2008;32(8):1757–62.
Kinoshita A, Onoda H, Imai N, Iwaku A, Oishi M, Tanaka K, et al. The C-reactive protein/albumin ratio, a novel inflammation-based prognostic score, predicts outcomes in patients with hepatocellular carcinoma. Ann Surg Oncol. 2015;22(3):803–10.
Ishizuka M, Kubota K, Kita J, Shimoda M, Kato M, Sawada T. Impact of an inflammation-based prognostic system on patients undergoing surgery for hepatocellular carcinoma: a retrospective study of 398 Japanese patients. Am J Surg. 2012;203(1):101–6.
Pinato DJ, North BV, Sharma R. A novel, externally validated inflammation-based prognostic algorithm in hepatocellular carcinoma: the prognostic nutritional index (PNI). Br J Cancer. 2012;106(8):1439–45.
Smith RA, Bosonnet L, Raraty M, Sutton R, Neoptolemos JP, Campbell F, et al. Preoperative platelet-lymphocyte ratio is an independent significant prognostic marker in resected pancreatic ductal adenocarcinoma. Am J Surg. 2009;197(4):466–72.
Kasymjanova G, MacDonald N, Agulnik JS, Cohen V, Pepe C, Kreisman H, et al. The predictive value of pre-treatment inflammatory markers in advanced non-small-cell lung cancer. Curr Oncol. 2010;17(4):52–8.
Ignacio de Ulibarri J, Gonzalez-Madrono A, de Villar NG, Gonzalez P, Gonzalez B, Mancha A, et al. CONUT: a tool for controlling nutritional status. First validation in a hospital population. Nutr Hosp. 2005;20(1):38–45.
Yoshida N, Baba Y, Shigaki H, Harada K, Iwatsuki M, Kurashige J, et al. Preoperative nutritional assessment by controlling nutritional status (CONUT) is useful to estimate postoperative morbidity after esophagectomy for esophageal cancer. World J Surg. 2016;40(8):1910–7.
Tokunaga R, Sakamoto Y, Nakagawa S, Ohuchi M, Izumi D, Kosumi K, et al. CONUT: a novel independent predictive score for colorectal cancer patients undergoing potentially curative resection. Int J Colorectal Dis. 2017;32(1):99–106.
Miyata T, Yamashita YI, Higashi T, Taki K, Izumi D, Kosumi K, et al. The prognostic impact of controlling nutritional status (CONUT) in intrahepatic cholangiocarcinoma following curative hepatectomy: a retrospective single institution study. World J Surg. 2018;42(4):1085–91.
Kudo M, Kitano M, Sakurai T, Nishida N. General rules for the clinical and pathological study of primary liver cancer, nationwide follow-up survey and clinical practice guidelines: the outstanding achievements of the liver cancer study group of Japan. Dig Dis. 2015;33(6):765–70.
Vallet-Pichard A, Mallet V, Nalpas B, Verkarre V, Nalpas A, Dhalluin-Venier V, et al. FIB-4: an inexpensive and accurate marker of fibrosis in HCV infection comparison with liver biopsy and fibrotest. Hepatology. 2007;46(1):32–6.
Kinoshita A, Onoda H, Imai N, Iwaku A, Oishi M, Fushiya N, et al. Comparison of the prognostic value of inflammation-based prognostic scores in patients with hepatocellular carcinoma. Br J Cancer. 2012;107(6):988–93.
McMillan DC. An inflammation-based prognostic score and its role in the nutrition-based management of patients with cancer. Proc Nutr Soc. 2008;67(3):257–62.
Gullett N, Rossi P, Kucuk O, Johnstone PA. Cancer-induced cachexia: a guide for the oncologist. J Soc Integr Oncol. 2009;7(4):155–69.
Morris-Stiff G, Gomez D, Prasad KR. C-reactive protein in liver cancer surgery. Eur J Surg Oncol. 2008;34(7):727–9.
Kinoshita A, Onoda H, Takano K, Imai N, Saeki C, Fushiya N, et al. Pretreatment serum C-reactive protein level predicts poor prognosis in patients with hepatocellular carcinoma. Med Oncol. 2012;29(4):2800–8.
Tazzyman S, Lewis CE, Murdoch C. Neutrophils: key mediators of tumour angiogenesis. Int J Exp Pathol. 2009;90(3):222–31.
Gregory AD, Houghton AM. Tumor-associated neutrophils: new targets for cancer therapy. Cancer Res. 2011;71(7):2411–6.
Wagner DD. New links between inflammation and thrombosis. Arterioscler Thromb Vasc Biol. 2005;25(7):1321–4.
Stone RL, Nick AM, McNeish IA, Balkwill F, Han HD, Bottsford-Miller J, et al. Paraneoplastic thrombocytosis in ovarian cancer. N Engl J Med. 2012;366(7):610–8.
Jain S, Harris J, Ware J. Platelets: linking hemostasis and cancer. Arterioscler Thromb Vasc Biol. 2010;30(12):2362–7.
Nieswandt B, Hafner M, Echtenacher B, Mannel DN. Lysis of tumor cells by natural killer cells in mice is impeded by platelets. Cancer Res. 1999;59(6):1295–300.
Miller CL. Immunological assays as measurements of nutritional status: a review. JPEN J Parenter Enteral Nutr. 1978;2(4):554–66.
Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell. 2010;140(6):883–99.
Huber C, Bobek N, Kuball J, Thaler S, Hoffarth S, Huber C, et al. Inhibitors of apoptosis confer resistance to tumour suppression by adoptively transplanted cytotoxic T-lymphocytes in vitro and in vivo. Cell Death Differ. 2005;12(4):317–25.
Carr BI, Guerra V. Serum albumin levels in relation to tumor parameters in hepatocellular carcinoma patients. Int J Biol Markers. 2017;32(4):e391–6.
Silvente-Poirot S, Poirot M. Cancer. Cholesterol and cancer, in the balance. Science. 2014;343(6178):1445–6.
Kuzu OF, Noory MA, Robertson GP. The role of cholesterol in cancer. Cancer Res. 2016;76(8):2063–70.
Rossi JF, Lu ZY, Jourdan M, Klein B. Interleukin-6 as a therapeutic target. Clin Cancer Res. 2015;21(6):1248–57.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interest exists in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Matsumoto, T., Kitano, Y., Imai, K. et al. Clinical significance of preoperative inflammation-based score for the prognosis of patients with hepatocellular carcinoma who underwent hepatectomy. Surg Today 52, 1008–1015 (2022). https://doi.org/10.1007/s00595-021-02427-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-021-02427-x