Abstract
Purpose
The aim of this study was to compare the clinical outcomes between laparoscopic partial liver resection and open partial hepatectomy for tumors in the posterosuperior segments.
Methods
The clinical outcomes of patients who underwent either laparoscopic (n = 20) or open (n = 44) resection in segments 7/8 of the liver were initially evaluated. Because of disparities in the background characteristics, a case-matched study (1:1) was conducted. In addition, a comparative study of the patients who met the institutional criteria for laparoscopic partial hepatectomy was performed.
Results
In the case-matched study, the laparoscopic technique required a longer operation time (p = 0.001), but was associated with less intraoperative blood loss (p = 0.021), a lower incidence of major complications (p = 0.014), higher levels of serum albumin on postoperative days 3 and 7 (p = 0.031 and p = 0.035), and earlier discharge (p = 0.001) than open resection. The results of the latter study were similar to those of the case-matched analysis.
Conclusions
Laparoscopic partial hepatectomy was a feasible procedure for treating tumors in the posterosuperior segments without compromising oncological safety and yielded better short-term outcomes than open techniques. In addition, this study provides concrete selection criteria for laparoscopic partial hepatectomy for difficult lesions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nowadays, laparoscopic liver resection (LLR) is applied for tumors located in the entire area of the liver and has become one of the standard treatments for liver resection of the antero-lateral segments and left lateral sectionectomy [1,2,3]. However, laparoscopic resection of tumors located in the posterosuperior (PS) segments of the liver (segments 7 and 8 according to Couinaud’s classification) is still considered technically challenging due to difficulty in establishing a sufficiently clear operative field to identify safe resection margins and secure hemostasis [4, 5], although some reports of laparoscopic hepatectomy for PS lesions have emerged from centers specialized in performing laparoscopic liver resection [2, 3, 6,7,8,9,10,11,12].
For resection of tumors located in the PS segments, conventional open liver resection (OLR) requires a large incision to facilitate mobilization of the right hepatic lobe and to gain access to the target area, even when the tumor size is small. In contrast, LLR for the PS segments of the liver does not require a large skin incision for mobilization and extraction of the specimen. In addition, laparoscopic partial liver resection, i.e., laparoscopic wedge resection or non-anatomical resection, has been advocated as one of the most appropriate approaches for colorectal liver metastasis, due to its ability to preserve the remnant liver function and volume thus making it possible to perform repeat liver resection [13]. Therefore, we suspected that laparoscopic partial hepatectomy in segment 7 or 8 would be strongly associated with better intraoperative and postoperative outcomes than an open approach without compromising oncological results.
This retrospective analysis was designed to compare the perioperative outcomes of laparoscopic partial hepatectomy with open partial hepatectomy in the PS part of the liver. To minimize the influence of potential confounders, we conducted a case-matched analysis based on preoperative variables. In addition, a comparative analysis using our institutional indications for laparoscopic partial liver resection as selection criteria was performed.
Methods
Patients and study design
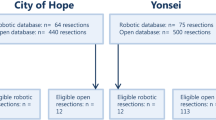
Patients were identified from a prospectively maintained database at the Department of Surgery, Tohoku University Hospital. From January 2010, when LLR was introduced at our institution, to July 2016, a total of 479 liver resection surgeries were performed (Fig. 1). The Japanese health insurance system covered laparoscopic partial hepatectomy and laparoscopic left lateral sectionectomy from April 2010, and before that we had performed LLR as an advanced medical treatment. From the cohort of 479 patients, 217 patients who underwent hepatectomy for bile duct carcinoma or hepatolithiasis were excluded. The charts of the remaining 262 patients were reviewed, and 122 and 76 cases were excluded because the patients underwent anatomical liver resection and partial liver resection not involving segments 7 or 8, respectively. Following this screening process, the perioperative and postoperative outcomes of 64 patients (20 patients in the LLR group and 44 patients in the OLR group) were retrospectively examined.
During this study period, we performed 68 laparoscopic partial hepatectomies and all of the patients who underwent LLR for the PS segments were included in this study. Two cases that converted to open surgery due to severe adhesion identified intraoperatively and unmanageable bleeding from the right hepatic vein (one each) were also included in the LLR group. Indications for LLR were determined at a hepatobiliary surgeons’ meeting preoperatively, but were inconsistent because this period included a learning curve. All laparoscopic procedures were performed by the same surgical team (TM, MI, and TT).
As there were some discrepancies in the background factors, 20 patients in the LLR group were matched with 20 patients in the OLR group based on the following perioperative variables: age, sex, number of resected tumors, and maximum tumor diameter. In addition, to validate our recent criteria for laparoscopic partial liver resection, we also performed a further analysis of patients who met our recent institutional criteria (16 LLR patients and 19 OLR patients). The indication for laparoscopic partial liver resection in our institution at present is as follows: tumor diameter ≤ 5 cm, tumor location ≤ 3 cm from the surface of the liver, and ≤ 3 tumors; our exclusion criteria are location in proximity to the hepatic hilum or inferior vena cava, the need for bile duct resection and lymph node dissection, and severe peritoneal adhesions identified on a preoperative ultrasound examination. The preoperative liver function was not used as a specific indicator when selecting the surgical approach.
The following variables were used in our analysis: relevant descriptive characteristics of patients, including age, sex, body mass index (BMI), history of laparotomy and liver resection, and preoperative physical status score by the American Society of Anesthesiologists (ASA) classification; clinicopathological information, including the diagnosis and diameter and number of tumors, as well as the preoperative laboratory test results for viral hepatitis, total bilirubin, aspartate aminotransferase (AST), alanine aminotransferase (ALT), albumin, platelet count, prothrombin time, and indocyanine green retention rate at 15 min; intraoperative data, including concurrent surgical procedures, operation time, volume of blood loss, blood transfusion rate, and negative surgical margin; postoperative course, including the time to ambulation, restoration of oral ingestion, length of hospital stay, morbidity, major complications, mortality, and readmission rate; and postoperative laboratory data, including total bilirubin, AST, ALT, albumin, and platelet counts on postoperative days 1, 3, and 7. Complications were defined as any events that occurred in the hospital or within 90 days after surgery, and major complications were defined as those scored ≥ IIIa under the Clavien–Dindo (CD) classification [14]. The surgical margin was defined as microscopically negative (R0) if tumor cells were not identified along the periphery of the resected specimen.
The present study was approved by the Institutional Review Board of Tohoku University (2016-1-748), and informed consent for this study was waived because of the retrospective nature.
Operative technique for OLR and LLR
Open and laparoscopic partial hepatectomy was performed under general and epidural anesthesia. For OLR, a right subcostal J-shaped incision was made with the patient in a supine position. For LLR, the patient was placed on the left, semi-lateral side in a reverse Trendelenburg position. After creating an initial 12-mm port at the umbilicus or right upper quadrants, pneumoperitoneum was established and maintained at a pressure ≤ 12 mmHg. The abdominal cavity was thoroughly examined and four additional 12-mm ports were placed into the subcostal area. Accessing the PS segments required transection of the ligaments around the liver, such as the falciform ligament and the right triangular ligament, and mobilization of the right hepatic lobe from the diaphragm to allow us to pull down and rotate the liver. Frequently, the right adrenal gland was also exposed. The mobilization of the right lobe of the liver in OLR was identical to that in LLR.
An intraoperative ultrasound examination was routinely performed for both OLR and LLR to identify the location and surgical characteristics of the tumors and to confirm the surgical boundaries. Parenchymal transection for OLR was performed using an ultrasonic surgical aspirator (CUSA Excel; Integra Lifescience, Plainsboro, NJ, USA), and for LLR, the surface of the liver was dissected using laparoscopic coagulating shears, with deeper parenchymal dissection being performed using a laparoscopic ultrasonic surgical aspirator. As a precaution in case of abrupt hemorrhaging during the parenchymal transection, inflow occlusion, known as the Pringle’s maneuver, was performed for both. Bleeding from small branches of the hepatic veins was controlled by sutures and ligature for OLR and clipping for LLR, and monopolar soft-mode coagulation with hemostatic forceps was used for both procedures. In the laparoscopic approach, after resection of the targeted liver tissue was performed, one of the trocar sites was extended for extraction of a retrieval bag into which the specimen was inserted. A closed drain was placed, as necessary, and the wound was approximated in layers and closed with sutures.
Statistical analyses
For descriptive purposes, the mean ± standard deviation was calculated for normally distributed continuous variables and the median (range) for non-normally distributed continuous variables, while categorical variables were expressed as proportions. Between-group differences were evaluated using the Chi-square test or Fisher’s exact test for categorical variables, as appropriate for the distribution of values, and Student’s t test or Mann–Whitney U test, again as appropriate for the distribution of values, for continuous variables. The survival was calculated from the date of hepatectomy, estimated using the Kaplan–Meier method, and compared between the groups using the log-rank test. All analyses were performed using the JMP pro 13 software program (SAS Institute Inc., Cary, NC, USA), with the level of significance for all tests set at p < 0.05.
Results
Analyses of all 64 patients
Descriptive information of all of the patients in this study is shown in Table 1. This cohort had 44 males with a median age of 64 years and a median maximum tumor diameter of 20 mm. The median number of tumors was 1, and partial liver resection was performed most frequently for metastatic liver tumors in each group. In between-group comparisons of descriptive variables, basic descriptive variables (age, sex, BMI), the pathological diagnosis, and laboratory data were comparable. A history of liver resection was more frequent for patients in the OLR group than in the LLR group, although this difference did not reach statistical significance. The number of tumors in the OLR group was significantly higher than that in the LLR group (p = 0.033). The intra- and postoperative outcomes are shown in Table 2. The average operation time was 330 ± 115 min, and the operation time of the LLR group was significantly longer than that of the OLR group (p < 0.001). In contrast, the median intraoperative blood loss was 512.5 g, and the laparoscopic approach was associated with less blood loss than open resection (p = 0.024). However, there was no marked difference in the blood transfusion rate or R0 resection rate between the groups.
Regarding the postoperative course, the median time to restarting ambulation, restored oral ingestion, and discharge from the hospital was 2, 2, and 12 days, respectively, and the use of the laparoscopic technique was associated with earlier ambulation (p = 0.013) and earlier postoperative discharge (p = 0.002) than open resection.
Twenty-one patients experienced postoperative complications, and 7 developed major complications. The incidence of complications was comparable between the groups, but the rate of major complications in the OLR group was significantly higher than that in the LLR group. These major complications were managed conservatively in six patients, and one patient with intra-abdominal hemorrhaging required reoperation for peritoneal drainage. The rate of hospital readmission was not a significant factor for either group, and two patients were readmitted to the hospital five and eight days after discharge due to an intra-abdominal abscess and pleural effusion, respectively.
Regarding the long-term outcomes, the 5-year overall survival (OS) was 81.7%, and the 5-year recurrence-free survival (RFS) was 52.8% with a median follow-up period of 39.0 (0.4–85.7) months. There were no significant differences in the 5-year OS (OLR vs. LLR: 85.6% vs. 80.8%, p = 0.839) or RFS (OLR vs. LLR: 66.1% vs. 46.8%, p = 0.267) between the groups (Figs. 2, 3).
Analyses of the matched patients
The basic descriptive variables, pathological diagnoses, and laboratory examinations of 40 patients were well matched (Table 3). In particular, the number of resected tumors, which was significantly different between the two groups in the full analysis set, was comparable between the LLR and OLR groups in this analysis. The intra- and postoperative outcomes of this cohort are shown in Table 4. The operation time was significantly longer and the intraoperative blood loss significantly lower in the LLR group than in the OLR group (p = 0.001, and p = 0.021, respectively), consistent with the results of the overall analysis. Open partial hepatectomy was associated with significantly more major complications than the laparoscopic approach, although there was no significant difference in the overall morbidity between the groups. Regarding the postoperative course, the postoperative hospital stay in the LLR group was significantly shorter than that in the OLR group, and the median between-group difference in the hospital stay was 4.5 days. Table 5 summarizes the postoperative changes in the results of biochemical examinations. There were no significant differences between groups in the total bilirubin, AST, ALT, and platelet counts at any time point. However, the serum albumin levels on postoperative days 3 and 7 in the LLR group were significantly higher than those in the OLR group.
Analyses of the patients consistent with institutional criteria
Thirty-five patients (16 LLR patients and 19 OLR patients) have so far met the indications for laparoscopic partial liver resection at our institution and comparative analyses were performed of this cohort. No significant differences were observed between the groups regarding the basic descriptive variables, pathological diagnoses, and laboratory examinations (data not shown). The operation time was significantly longer and the intraoperative blood loss significantly less in the LLR group than the OLR group, consistent with the results of the case-matched analysis (Table 6). In addition, the blood transfusion rate was significantly higher in the OLR group than in the LLR group. LLR was associated with a lower rate of major complications and a shorter hospital stay, and the serum albumin levels on postoperative days 3 and 7 in the LLR group were also significantly higher than those in the OLR group (3.2 ± 0.36 vs. 2.8 ± 0.41, p = 0.005, and 3.4 ± 0.14 vs. 3.0 ± 0.13, p = 0.023), respectively. These results also resembled those in the case-matched analysis.
Discussion
Laparoscopic hepatectomy has emerged as a treatment of choice in liver surgery, and while its spread was initially slow [5], the number of procedures performed has increased exponentially with advances in laparoscopic devices and surgical experience, making LLR now one of the standard approaches to liver surgery [1]. Many studies have found that laparoscopic hepatectomy was associated with less intraoperative blood loss, a shorter hospital stay, and comparable oncological and financial outcomes compared with open hepatectomy [2, 5, 13, 15,16,17]. In addition, some comparative studies have reported that LLR of tumors in the PS segments is superior to OLR in terms of intraoperative blood loss [6, 8, 9], complication rate [8, 11], and postoperative hospital stay [6, 8, 10, 11]. Laparoscopic partial liver resection for the PS segments poses some difficulties in making a curvilinear resection surface and in controlling bleeding, as the costal margin and right hepatic lobe hinder the establishment of a safe operative field and the movement of laparoscopic instruments [11, 18]. For this reason, LLR tends to be adopted for major or anatomical liver resection in the PS segments, even if the tumor size is equivalent to that in the anterolateral segment [2, 7, 8, 12]. However, at our institution, partial liver resection has mainly been adopted according to a parenchyma-preserving policy for liver neoplastic lesions [9, 13], especially for liver metastases of colorectal cancer, and this policy has also been applied to laparoscopic hepatectomy for difficult lesions. We therefore investigated the clinical results of laparoscopic partial hepatectomy in the PS segments compared with the open approach.
In our case-matched study, we demonstrated that some clinical outcomes of LLR, such as intraoperative blood loss, major complication rate, and hospital stay, were superior to those with OLR for tumors located in the PS segments. However, few studies have compared laparoscopic partial liver resection with the conventional open approach in the PS segments. Bueno et al. [6] reported that laparoscopic partial liver resection of the PS segments was associated with a smaller number of total complications, a hemoglobin decrease of < 2 g/dL, and a length of stay < 5 days; however, they did not describe in detail the perioperative outcomes of these patients. Sruderi et al. [11] performed a propensity score-matched analysis between laparoscopic and open resection of the PS segments of the liver and found that LLR was associated with a lower complication rate, shorter duration of analgesia, and shorter hospital stay than OLR, results that were similar to our own.
The operation time was significantly longer for the laparoscopic procedure than the open procedure in the present study, although several studies have reported equivalent operation times between open and laparoscopic liver surgery [8, 13, 17]. One possible reason for the longer operation time in the LLR group was that the data used in this analysis were obtained when LLR was first introduced at our institution. Alternatively, the aforementioned technical problems associated with LLR in the PS segments may be involved. It was also reported that laparoscopic partial liver resection in segments 7 and 8 is sometimes more difficult than laparoscopic anatomical resection [11]. Solutions for shortening the operation time for laparoscopic resection of tumors located in the PS segments include the use of intercostal trocars and placing the patient in a semi-prone position [18,19,20]. The surgical outcome will likely be improved further when these solutions are implemented in our institution. Regardless, we were able to perform LLR with less blood loss than that with OLR, reflecting the technical and surgical advantages of the laparoscopic approach, such as improved visualization and magnification followed by meticulous dissection and decreased venous oozing under pneumoperitoneum pressure [5, 8, 17]. In addition, the blood transfusion rate in the LLR group tended to be lower than that in the OLR group in the case-matched study and was significantly lower in the comparative study limited to the patients compatible with current indications. Blood transfusion has been reported to be associated with a poor prognosis in hepatocellular carcinoma patients [21] and infectious complications after hepatectomy [22], and a decrease in blood transfusion leads to the conservation of blood resources. Therefore, the benefits of a reduced blood loss outweigh the longer operation time associated with LLR.
The rate of major complications was also significantly lower in the LLR group than in the OLR group, which likely reflects the more precise resection of the target area with LLR. In addition, the overall analysis showed that ambulation was achieved earlier in the LLR group than in the OLR group, undoubtedly due to the reduced surgery-related trauma to the abdominal wall. We also demonstrated higher postoperative serum concentrations of albumin using the laparoscopic approach. Xiang et al. reported that the postoperative levels of serum albumin in patients who underwent LLR in the PS segments were comparable to those in the anterolateral segments, although the operation time was significantly longer and the intraoperative blood loss significantly greater in the PS group than in the anterolateral segment group [12]. Therefore, the improvement in the nutritional status after LLR is assumed to result from the decreased surgical trauma and earlier return of the physical function. Reduced blood loss, a decreased risk for postoperative complications, and an improved nutritional status eventually lead to a significantly shortened hospitalization for patients in the LLR group compared to the OLR group.
A major concern with LLR for malignant liver tumors is the risk of inadequate oncologic resection. In this study, the R0 resection rates for the LLR and OLR groups were comparable, confirming the findings of a comparable tumor margin status and long-term survival rate for the two procedures in other studies [2, 5, 8, 9, 17]. Furthermore, although various types of tumors were included, the OS and RFS were comparable between the LLR and OLR groups in the full analysis set. Laparoscopic surgery also provides specific benefits for cancer patients, including improved tolerance for repeated hepatectomy and earlier access to adjuvant chemotherapy due to the earlier postoperative recovery [3, 5, 10, 23]. Multi-institutional trials are required to confirm whether or not LLR for malignant tumors results in a better prognosis than OLR.
We also conducted an analysis using our institution’s current indications for laparoscopic partial liver resection as selection criteria. In this analysis, LLR resulted in better clinical outcomes than OLR, showing that these indications capitalized on the advantages of LLR over OLR. We have added tumor depth from the liver surface to these criteria, although most studies have used surgical adaptation criteria of tumor size, number, and location. Okuno et al. [10] reported that surgeons tended to perform OLR for tumors located at a depth of ≥ 3 cm in the PS segments. Therefore, our criteria, including a tumor depth of ≤ 3 cm from the liver surface, appear reasonable for determining patients suitable for laparoscopic partial liver resection and may be used as the criteria for future studies to further clarify the superiority of laparoscopic partial liver resection over OLR.
There are several limitations that must be considered when applying our outcomes to practice, including the fact that this study was retrospective and not randomized. Furthermore, this is an analysis of a small number of patients from a single institution, and all LLR procedures were performed by a single surgical team. Moreover, some selection bias will exist because the selection criteria for LLR have broadened over time, although we performed a case-matched analysis to minimize potential confounders. While we were unable to reach robust conclusions, we were still able to demonstrate the feasibility of laparoscopic partial liver resection in the PS segments with technical and oncological safety under a parenchyma-preserving policy.
Conclusions
The present findings indicate that, for well-selected patients, laparoscopic partial hepatectomy is a safe and feasible procedure for resecting liver tumors in the PS segments without jeopardizing the oncological integrity. Compared to an open procedure, laparoscopic techniques yielded better short-term outcomes, including less intraoperative blood loss, a lower rate of major complications, higher postoperative levels of serum albumin, and an earlier discharge. Furthermore, our study provides concrete selection criteria for laparoscopic partial liver resection to treat difficult lesions.
References
Wakabayashi G, Cherqui D, Geller DA, Buell JF, Kaneko H, Han HS, et al. Recommendations for laparoscopic liver resection: A report from the second international consensus conference held in Morioka. Ann Surg. 2015; 261:619–29.
Yoon YS, Han HS, Cho JY, Ahn KS. Total laparoscopic liver resection for hepatocellular carcinoma located in all segments of the liver. Surg Endosc. 2010;24:1630–7.
Ishizawa T, Gunbs AA, Kokudo N, Gayet B. Laparoscopic segmentectomy of the liver: From segment I to VIII. Ann Surg. 2012;256:959–64.
Kaneko H, Takagi S, Shiba T. Laparoscopic partial hepatectomy and left lateral segmentectomy: technique and results of a clinical series. Surgery. 1996;120:468–75.
Simillis C, Constantinides VA, Tekkis PP, Darzi A, Lovegrove R, Jiao L, et al. Laparoscopic versus open hepatic resections for benign and malignant neoplasms–a meta-analysis. Surgery. 2007;141:203–11.
Bueno A, Rotellar F, Benito A, Marti-Cruchaga P, Zozaya G, Hermida J, et al. Laparoscopic limited liver resection decrease morbidity irrespective of the hepatic segment resected. HPB. 2014;16:320–26.
Cho JY, Han HS, Yoon YS, Shin SH. Experiences of laparoscopic liver resection including lesions in the posterosuperior segments of the liver. Surg Endosc. 2008;22:2344–9.
Xiao L, Xiang LJ, Li JW, Chen J, Fan YD, Zheng SG. Laparoscopic versus open liver resection for hepatocellular carcinoma in posterosuperior segments. Surg Endosc. 2015;29:2994–3001.
D’Hondt M, Tamby E, Boscart I, Turcotte S, Parmentier I, Pottel H, et al. Laparoscopic versus open parenchymal preserving liver resections in the posterosuperior segments: a case-matched study. Surg Endosc. 2018;32:1478–85.
Okuno M, Goumard C, Mizuno T, Omichi K, Tzeng CWD, Chun YS, et al. Operative and short-term oncologic outcomes of laparoscopic versus open liver resection for colorectal liver metastases located in the posterosuperior liver: a propensity score matching analysis. Surg Endosc. 2018;32:1776–86.
Scuderi V, Barkhatov L, Montalti R, Ratti F, Cipriani F, Pardo F, et al. Outcome after laparoscopic and open resections of posterosuperior segments of the liver. Br J Surg. 2016;22:2344–9.
Xiang L, Xiao L, Li J, Chen J, Fan Y, Zheng S. Safety and feasibility of laparoscopic hepatectomy for hepatocellular carcinoma in the posterosuperior liver segments. World J Surg. 2015;39:1202–9.
Montalti R, Berardi G, Laurent S, Sebastiani S, Ferdinande L, Libbrecht LJ, et al. Laparoscopic liver resection compared to open approach in patients with colorectal liver metastasis improves further resectability: Oncological outcomes of a case-control matched-pairs analysis. Eur J Surg Oncol. 2014;40:536–44.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Kawaguchi Y, Otsuka Y, Kaneko N, Nagai M, Nomura Y, Yamamoto M, et al. Comparisons of financial and short-term outcomes between laparoscopic and open hepatectomy: benefits for patients and hospitals. Surg Today. 2016;46:535–42.
Guerron AD, Aliyev S, Agcaoglu O, Aksoy E, Taskin HE, Aucejo F, et al. Laparoscopic versus open resection of colorectal liver metastasis. Surg Endosc. 2013;27:1138–43.
Nguyen KT, Marsh JW, Tsung A, Steel JJL, Gamblin TC, Geller DA. Comparative benefits of laparoscopic vs open hepatic resection: a critical appraisal. Arch Surg. 2011;146:348–56.
Araki K, Kubo M, Watanabe A, Kuwano H, Shirabe K. Systematic review of the feasibility and future of laparoscopic liver resection for difficult lesions. Surg Today. 2018. https://doi.org/10.1007/s00595-017-1607-6.
Lee W, Han HS, Yoon YS, Cho JY, Choi YR, Shin HK. Role of intercostal trocars on laparoscopic liver resection for tumors in segments 7 and 8. J Hepatobiliary Pancreat Sci. 2014;21:E65–8.
Ikeda T, Yonemura Y, Ueda N, Kabashima A, Shirabe K, Taketomi A, et al. Pure laparoscopic right hepatectomy in the semi-prone position using the intrahepatic Glissonian approach and a modified hanging maneuver to minimize intraoperative bleeding. Surg Today. 2011;41:1592–8.
Wada H, Eguchi H, Nagao H, Kubo S, Nakai T, Kaibori M, et al. Perioperative allogenic blood transfusion is a poor prognostic factor after hepatocellular carcinoma surgery: a multi-center analysis. Surg Today. 2018;48:73–9.
Pessaux P, van den Broek MAJ, Wu T, Olde Damink SWM, Piardi T, Dejong CHC, et al. Identification and validation of risk factors for postoperative infectious complication following hepatectomy. J Gastorointest Surg. 2013;17:1907–16.
Shafaee Z, Kazaryan AM, Marvin MR, Cannon R, Buell JF, Edwin B, et al. Is laparoscopic repeat hepatectomy feasible? A tri-institutional analysis. J Am Coll Surg. 2011;212:171–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Takanori Morikawa and the co-authors have no conflicts of interest or financial ties to disclose in association with this study.
Rights and permissions
About this article
Cite this article
Morikawa, T., Ishida, M., Takadate, T. et al. Laparoscopic partial liver resection improves the short-term outcomes compared to open surgery for liver tumors in the posterosuperior segments. Surg Today 49, 214–223 (2019). https://doi.org/10.1007/s00595-018-1719-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-018-1719-7