Abstract
Aims
A bidirectional relationship has been reported between diabetes mellitus and periodontitis. The present study aimed to estimate salivary fructosamine in diabetic and non-diabetic individuals with healthy and diseased periodontium and to measure its changes after non-surgical periodontal therapy. Another aim was to identify the cut-off value of salivary fructosamine to diagnose diabetes mellitus and to correlate it with glycated hemoglobin.
Methods
Salivary fructosamine and HbA1c were assessed in periodontally healthy individuals and periodontitis patients (n = 60 in each group). Both groups comprised of equal number of patients with and without diabetes mellitus. Salivary fructosamine estimation was repeated 4 weeks after non-surgical periodontal therapy in periodontitis patients.
Results
HbA1c and Salivary fructosamine were significantly higher in the periodontally diseased compared to the healthy group. Significantly higher values of these biomarkers were noticed in diabetic patients with periodontitis compared to the non-diabetic group. Periodontal therapy significantly reduced salivary fructosamine in both diabetic and nondiabetic periodontitis patients. A significant positive high correlation was noticed between salivary fructosamine and HbA1c (r = 0.76). The cut-off value of salivary fructosamine was found to be 68 µg/mL with 95% sensitivity, 81.67% specificity, 83.82% positive predictive value, and 94.23% negative predictive value.
Conclusion
Periodontitis can contribute to glycemic control and periodontal therapy can bring about improvement in glycemic status. Salivary fructosamine could be used as an alternate glycemic biomarker and its advantages over HbA1c include simple and non-invasive collection of saliva and it can provide intermediate glycemic status.
Clinical Trial Registry of India:
2020/11/038496
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Periodontitis is a non-communicable disease with a high prevalence, affecting 11.2% of the world’s population, and is the sixth most common human disease [1]. It is a chronic, multifactorial disease like type 2 diabetes mellitus (T2DM) and is considered the 6th complication of T2DM [2]. In addition, periodontitis may worsen glycaemic control, and periodontal therapy is reported to bring about improvement in glycemic status [3].
T2DM is usually diagnosed by assessing either Random Blood Glucose level, Fasting Blood glucose level, or 2-h postprandial blood glucose levels as per American Diabetes Association Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2021 [4]. Glycated haemoglobin (HbA1c) is another reliable biomarker that is the currently available best method to assess long-term glycaemic control over the past 3 months in diabetic patients [5]. Lowering HbA1c levels is the main strategy to reduce the risk of long-term macrovascular and microvascular complications of T2DM [6]. But HbA1c can only be detected in blood with limited diagnostic accuracy in many conditions including alcoholism, lead poisoning, elevated triglycerides, chronic aspirin therapy, hemoglobinopathy, pregnancy, or other complicating illnesses affecting the erythrocyte lifespan, such as hemolytic anemia [7]. So, there is a demand for an alternative biomarker to assess glycemic control that provides additional or substitute information about the progression of hyperglycemia especially when metabolic alterations are far more dynamic than the 2–3 months prior period as assessed by HbA1c [8].
Protein comprises major components of blood and other tissue fluids like saliva. Glycosylation of proteins leads to the formation of fructosamine (FA) which is predominantly comprised of glycated albumin. Due to increased protein turnover, FA reflects average glucose levels during the preceding 2–3 weeks, providing an intermediate index for glycemic control [8].
Unlike HbA1c, fructosamine can be detected in saliva which offers a distinctive advantage over serum in the estimation of FA levels as it is non-invasive, easy to collect without much expertise, and is cost-effective [9]. Saliva glucose is rapidly decomposed by bacteria and enzymes in the mouth, so it is very difficult to measure it without using ultrafiltration [10]. However salivary glycated proteins, i.e., proteins combined with glucose, are relatively stable against bacteria, and a correlation has already been made between salivary glycated proteins and blood glucose as well as glycated hemoglobin in diabetic patients [9, 10]. A recent systematic review reported the correlation of salivary FA measurements with established blood glycemic biomarkers such as serum FA, blood glucose, and HbA1c [11]. They could identify the overall level of evidence as low, and the risk of bias was determined to be high due to the heterogeneity of the included studies and limitations in sample size. They recommended future well-controlled studies before making a definitive conclusion.
Hitherto no studies are available regarding the levels of salivary FA in periodontitis patients. The impact of periodontal treatment on salivary and serum FA is another unexplored area. We hypothesize that salivary FA in periodontally healthy individuals differs from periodontitis patients and periodontal therapy can bring about a change in salivary FA values. So, the aim of the present study was to compare the salivary FA level in diabetic and non-diabetic individuals with healthy and diseased periodontium. Another objective was to assess the impact of nonsurgical periodontal therapy (NSPT) on glycaemic control using salivary FA in periodontitis patients. In addition, salivary FA is correlated with HbA1c, and the cut-off value of the assay for diagnosing diabetes mellitus is also determined.
Materials and methods
The present study was conducted in the Department of Periodontics, PMS College of Dental Science and Research, Trivandrum from January 2022 to December 2022 after obtaining clearance from the institutional ethical committee (IEC NO: PMS/IEC/2020–21/15). The study was conducted in accordance with Helsinki Declaration 1975, as revised in 2000, and was registered in the clinical trial registry of India (2020/11/038496).
The prevalence of severe periodontitis was 19% and that of type II diabetes mellitus was 9% as per published literature [12, 13]. The sample size was calculated using the formula n = 2 σ2 (Zα + Zβ) 2 ÷ δ. Type 1 error was kept as 0.05 and type 2 error as 0.20. σ (standard deviation) and effect size δ were taken from the pilot study. Pooled σ is 4 and clinically significant effect size δ is chosen to be 2.5. Substituting the values and considering the chance of 10% dropouts during the study the minimum sample size required was calculated as 60 in each group (severe periodontitis patients and periodontally healthy individuals).
The study was conducted in two phases. The first phase of the study was an observational comparative study comparing the clinical and biochemical parameters between the groups. The second phase of the study was a pre-post quasi-experimental study that compared the clinical and biochemical parameters of the periodontitis patients before and 4 weeks after NSPT.
Periodontally healthy and Stage III -IV generalized periodontitis patients were diagnosed according to criteria given by the World Workshop on the Classification of Periodontal and Peri‐implant Diseases and Conditions in 2017 [14]. Patients diagnosed with T2DM according to criteria given by American Diabetes Association: Standards of Medical Care, 2020 [15]. Undiagnosed individuals who have HbA1c > 6.5 were also included in the diabetic group. Pregnant and lactating females, smokers, Immunocompromised patients, patients with conditions that interfere with the hemoglobin metabolism or protein metabolism like renal, hepatic and thyroid diseases, and diabetic patients on insulin therapy were excluded.
A quota sampling technique was used to select study participants until the required sample size was reached in each group. An equal number of diabetic and nondiabetic individuals were included in both groups. So, there were 4 subgroups of 30 samples each based on their diabetic and periodontitis status.
1. Group A: Periodontally healthy, without T2DM.
2. Group B: Stage III -IV generalized Periodontitis, without T2DM.
3. Group C: Periodontally healthy, with T2DM.
4. Group D: Stage III -IV generalized Periodontitis, with T2DM.
The STROBE checklist is provided as supplementary Table 1.All participants were informed about the study protocol and written consent was obtained. Following blood and saliva sample collection, full mouth periodontal status evaluation on four sites per tooth was carried out that included full mouth plaque score (FMPS) [16], Full mouth bleeding score (FMBS) [17], probing pocket depth (PPD) and clinical attachment loss/level (CAL), using a manual periodontal probeFootnote 1 by a single calibrated examiner. The initial step of NSPT was professional mechanical plaque control using an ultrasonic scaler in a single visit by the same investigator. All the participants were provided oral hygiene instructions, and they were motivated to maintain good plaque control. All the periodontitis patients were recalled after 1 week for subgingival instrumentation in indicated sites under topical anaesthesia using a combination of ultrasonic scalerFootnote 2 and Gracey curettesFootnote 3. The procedure was completed in a single visit by the same examiner. Salivary FA and clinical parameters were re-assessed 4 weeks following subgingival instrumentation.
Blood sample collection
2.5 ml of blood sample was collected from the antecubital fossa by venipuncture using a 20-gauge needle with a 5 ml syringe, before periodontal examination at baseline for the estimation of HbA1c. The blood sample was transferred to a clean container with an anticoagulant (EDTA) and was immediately transported at room temperature to the laboratory for analysis. The ion exchange high-performance liquid chromatography method was used for HbA1c estimation.
Saliva collection
Unstimulated whole expectorated saliva (2 ml) was collected from each subject after two hours of fasting, between 9:00 and 11:30 a.m., to avoid circadian variations as described previously [18]. The patients were asked to swallow first and then allow the unstimulated saliva to pool at the bottom of the mouth. It was collected using a syringe and transferred to a sterile capped tube. Collected saliva was immediately placed on ice prior to freezing at − 20° C immediately after collection. The sample was transported to the laboratory in liquid nitrogen. Samples were defrosted and analyzed within 6 months of collection. Each saliva sample was pipetted into a clean microcap tube and centrifugation was done at 4,000 rpm for 10 min at 40° C. The supernatant was transferred to clean microcap tubes.
FA content of saliva was estimated by the nitro blue tetrazolium (NBT) method described previously with slight modifications [19]. Concentrations of FA were determined using a colorimetric test that is based on the ability of FAs to act as reducing agents in an alkaline solution and convert NBT to a purple dye that can be monitored by absorbance at 530 nm. 1 ml of saliva was mixed with 3 ml of NBT reagent (0.75 mmol/L) and incubated at 37° C. The absorbance was measured at 530 nm in time intervals (10 min and 60 min). The change in absorbance at 530 nm is a measure of FA values. FA values were calculated by using a standard graph. The results of the FA assay were expressed as micrograms per milliliter for concentrations.
Statistical analysis
Data were statistically described in terms of mean ± standard deviation. A comparison of salivary FA levels in 2 groups (periodontally healthy individuals and periodontitis patients) was done using an unpaired t-test. Comparison between levels of FA in subgroups A, B, C, and D was done using analysis of variance with a post hoc test (Tukey’s HSD test). Comparison of salivary FA levels in periodontitis patients before and after NSPT was done using paired t-test. Correlation between HbA1c and salivary FA was done using the Pearson correlation coefficient. Sensitivity and specificity were used to describe the diagnostic accuracy. Receiver operator characteristic (ROC) analysis was carried out and the optimum cut-off value for salivary FA in diagnosing T2DM was determined from the receiver operator characteristics curve (ROC) by the method of Index of Union (IU) [20]. p < 0.05 was considered statistically significant in all the comparisons. All were done using computer programFootnote 4.
Results
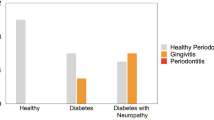
59 females and 61 males with a mean age of 42.35 ± 7.13 were recruited for the study. Screening and categorization of study participants are provided in Figure S1. The first phase of the study was completed in the initial 6 months and the remaining time was taken to complete the second phase. No significant difference was noticed among the groups for age or gender. The baseline clinical characteristics of the study population such as FMBS, FMPS, PPD, and CAL were statistically higher in cases compared with the control (p < 0.00001), and data are provided in Table 1. HbA1c and Salivary FA were also significantly different in the periodontally healthy compared to the diseased group. However, in subgroup analysis, salivary FA was not significantly different between periodontally healthy individuals and periodontitis patients when diabetic and non-diabetic groups were analyzed separately (Table 2). FMBS, HbA1c, and salivary FA were significantly higher in diabetic patients with periodontitis compared to the nondiabetic group. Salivary FA was significantly higher in diabetic patients compared to non-diabetic individuals (79.27 ± 15.06 and 52.326 ± 22.2 respectively, < 0.00001).
The mean frequency of moderate and deep pockets in groups B and D before and after NSPT are given in Supplementary Table 2. NSPT significantly reduced all the clinical parameters as well as salivary FA in both diabetic and nondiabetic periodontitis patients (Table 3). A highly significant (p < 0.01) reduction in the mean percent of salivary fructosamine was noticed in group D as compared to group B as per the intergroup analysis. The data is provided in supplementary Table 3. Patients who were lost to follow-up in groups B and D were not included in the analysis.
A significant positive high correlation was noticed between salivary FA and HbA1c when diabetic (r = 0.6) and non-diabetic groups (r = 0.68) were analysed separately and together (r = 0.76) (Table 4), (Fig. 1).
Salivary FA could significantly differentiate diabetic patients from nondiabetic controls with a p-value of 0.000. The area under the ROC curve was 0.869 ± 0.038 (confidence interval − 0.794 to 0.944). The cut-off value of salivary FA is 68 µg/mL with 95% sensitivity, 81.67% specificity, 83.82% positive predictive value, and 94.23% negative predictive value (Fig. 2). 23.3% of the patients in the non-diabetic group were above the cut-off point before non-surgical therapy which was reduced to 20% in re-evaluation. Correspondingly in the diabetic group, a 30% reduction was noticed (from 100 to 70%).
Discussion
A substantial body of evidence shows that the onset of diabetes can be prevented or delayed greatly in individuals at high risk by adopting a comprehensive preventive approach, which includes a healthy lifestyle. Early diagnosis and glycemic control are essential to prevent various complications of T2DM [21]. Periodontitis and diabetes are reported to share a bidirectional relationship and periodontitis may influence the blood sugar values. The most commonly available test for monitoring long-term glycemic control is the estimation of HbA1c. In the present study, HbA1c was significantly higher in periodontitis patients as reported previously in the literature [22]. However, HbA1c may not be useful for many conditions like hemoglobinopathies, and it can be detected only in blood. So, we selected salivary FA as a non-invasive alternate biomarker and we could find significantly higher values of salivary FA in periodontitis patients compared to periodontally healthy individuals (70.27 ± 16.67 vs 61.33 ± 65, p = 0.017). The increase in salivary FA noticed in periodontitis patients could be considered an alarming sign predisposing them to develop T2DM in the future.
Glycemic control is worsened with advanced destruction of periodontal tissues and periodontal therapy helps in improving glycemic control. A 0.56% reduction in HbA1c following non-surgical periodontal therapy in diabetic periodontitis patients was reported in a recent meta-analysis [23]. However, the HbA1c assay indicates the plasma glucose range over 3–4 months. Since we are evaluating the results of nonsurgical periodontal therapy after 4–6 weeks HbA1c may not be the ideal biomarker. FA is an excellent choice in this regard which provides average glycemic control of the preceding 2–3 weeks (because the half-life of an albumin molecule is 14–20 days) [24]. In the present study, we could notice a significant reduction in salivary FA levels after non-surgical periodontal therapy in both diabetic and non-diabetic periodontitis patients indicating the beneficial effects of periodontal therapy in improving glycemic control. The reduction was more pronounced in the diabetic group.
To the best of our knowledge, we could not identify any studies evaluating salivary FA in periodontitis patients. However, few studies have estimated serum FA in periodontally healthy and diseased individuals [24, 25]. Similarly, we could find few studies reporting salivary FA estimation in diabetic and non-diabetic patients. Nakamoto et al. 2003 reported the mean Salivary FA among healthy controls (n = 31), patients with Impaired Glucose Tolerance tests (n = 10), and diabetic patients (n = 10) as 25.2 ± 11.6 μmol/g protein [9]. They measured salivary FA per 1 gm of protein in saliva unlike the total FA estimation done in our study. So, we cannot do a comparison of their results with ours. However they correlated HbA1c with salivary FA in each group and obtained a positive correlation of r = 0.64 in the diabetic group which is comparable to our results (r = 0.6; p < 0.00001).
Morenkova et al. in 2004, reported that there was an increase in Salivary FA concentration with an increase in Plasma Glucose levels [26]. The levels of Salivary FA in healthy controls and T2DM patients were 3.7 ± 0 mmol/L and 7.3 ± 2.0 mmol/L respectively compared to our results of 79.27 ± 15.06 µmol/L in diabetics and 52.32 ± 22.2 µmol/L in nondiabetics. The inconsistency in the values could be due to the presence of unaccountable confounding factors and differences in the ethnicity of the population.
Our results are consistent with the findings of Manjrekar et al. 2012 who observed significantly higher levels of Salivary FA (113.17 ± 57.9 µmol/L) in individuals in the diabetic group compared to individuals in the non-diabetic group (55.88 ± 28.05 µmol/L) [27].
Kandavel et al. in 2019 reported the mean levels of salivary FA in diabetic male (n = 30) and female (n = 20) participants as 158.80 ± 97.736 µmol/L and 208.10 ± 72.480 µmol/L, respectively [28]. For comparison purposes, we have calculated our results separately for male and female participants and we got 78.7 ± 15.81 µmol/L and 80.3 ± 13.5 µmol/L respectively for males (n = 35) and females (n = 25). Among non-diabetic male (n = 21) and female (n = 29) participants, the mean levels of salivary FA were observed to be 80.90 ± 29.348 and 85.07 ± 25.209 µmol/L, respectively compared to 49.65 ± 17.8 µmol/L (n = 26) &54.37 ± 24.85 µmol/L (n = 34) in our study. Even though we got a similar trend in levels of salivary FA in both diabetic and non-diabetic groups, the inconsistency in value may be due to differences in sample size and mean age of the study population taken. The correlation coefficient between salivary FA and HbAlc in diabetic (r = 0.83) and non-diabetic (r = 0.3) groups are in line with our values (r = 0.6 & 0.68 respectively).
In none of the above-mentioned articles, cut-off value of salivary FA was determined. So, ours is a novel approach to determine the cut-off value which will be beneficial for the development of future chairside diagnostic kits. FA assay has many advantages, such as low cost and simplicity of the clinical laboratory procedure when compared to HbAlc assay [25]. Additionally, FA has clinical utility in conditions where information regarding short-term glucose control is important in the management of the patient such as in pregnancy, recent medication adjustment as well as for monitoring people with fluctuating blood sugar values or poorly controlled diabetes [29].
Salivary FA evaluation remains a futile criterion in cases of protein-losing disorders like nephropathy or liver disease. Likewise, any type of oral or salivary disease may influence the results. In the present study, we haven’t checked for the effect of major confounders like smoking, nutritional deficiencies, or hormonal variations. The reference method for measuring HbA1c is a standardized unit ie, millimoles of HbA1c per mole of Hb which avoid fluctuation in blood hemoglobin levels. There is uncertainty regarding FA measurements and controversy exists whether measurements should be corrected for total albumin, total protein, or neither. In our study, we have calculated uncorrected values of salivary FA. Future studies may be conducted to evaluate the variation concerning corrected FA values in periodontitis patients. We have conducted the study mostly in controlled T2DM patients in a limited population. To generalize the results, we must conduct future studies in larger samples, at different timings, using different methods of saliva collection, on different populations, especially uncontrolled diabetic patients.
The present study highlights the chances of utilizing salivary FA for monitoring T2DM and its possibility of being used as a method for easy identification of intermediate glycemic control in diabetic patients especially in response to periodontal treatment. Since FA can be assessed easily from saliva, various chairside diagnostic equipment can be developed in the future for the rapid and easy assessment of glycemic status in diabetic patients. The strong correlation between HbA1c and salivary FA obtained in the present study increases the generalisability and the predictability of salivary FA to be used as an alternate biomarker for T2DM. In large-scale epidemiological studies, saliva can be used as a non-invasive tool for screening purposes. Moreover, saliva also offers the possibility of developing a home test kit that may be used by the patients themselves.
Conclusion
Periodontitis can contribute to glycemic control and periodontal therapy can bring about improvement in glycemic status. The conventional methods of monitoring glycemic control, which includes Plasma glucose, HbA1c, and serum FA are invasive as they require venous puncture. In the present study, salivary FA is suggested as an alternative glycemic marker since the collection of saliva is simple and non-invasive. Positive strong correlation of salivary FA to HbA1c points to the possibility that it could be used as an alternate intermediate glycemic biomarker.
Notes
PW7, Hu- Friedy, IL, US
Aceton Satelec-p5-booster-ultrasonic-scaler
Hu-Friedy, Chicago, IL, USA
IBM SPSS (Statistical Package for the Social Science; IBM Corp, Armonk, NY, USA) release 22 for Microsoft Windows was the software used for statistical analysis
References
Kassebaum NJ, Bernabé E, Dahiya M et al (2014) Global burden of severe periodontitis in 1990–2010: a systematic review and meta-regression. J Dent Res 93(11):1045–1053. https://doi.org/10.1177/0022034514552491
Löe H (1993) Periodontal disease. The Sixth Complicat Diabetes Mellitus Diabetes Care 16(1):329–334
Di Domenico GL, Minoli M, Discepoli N, Ambrosi A, de Sanctis M (2023) Effectiveness of periodontal treatment to improve glycemic control: an umbrella review. Acta Diabetol 60(1):101–113. https://doi.org/10.1007/s00592-022-01991-z
American Diabetes Association (2021). Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2021 [published correction appears in Diabetes Care. 2021 Sep; 44(9):2182] Diabetes Care 44(Suppl 1): S15-S33 https://doi.org/10.2337/dc21-S002
Syed IA (2011) Glycated hemoglobin; past present and future are we ready for the change. J Pak Med Assoc 61(4):383–388
Stratton IM, Adler AI, Neil HA et al (2000) Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ 321(7258):405–412. https://doi.org/10.1136/bmj.321.7258.405
Rodríguez-Segade S, Rodríguez J, Camiña F (2017) Corrected fructosamine improves both correlation with HbA1C and diagnostic performance. Clin Biochem 50(3):110–115. https://doi.org/10.1016/j.clinbiochem.2016.10.014
Ribeiro RT, Macedo MP, Raposo JF (2016) HbA1c, Fructosamine, and glycated albumin in the detection of dysglycaemic conditions. Curr Diabetes Rev 12(1):14–19. https://doi.org/10.2174/1573399811666150701143112
Nakamoto I, Morimoto K, Takeshita T, Toda M (2003) Correlation between saliva glycated and blood glycated proteins. Environ Health Prev Med 8(3):95–99. https://doi.org/10.1007/BF02897922
Reena CS, Indira AP, David MP (2017) Evaluation of salivary albumin in type II diabetes mellitus. Inter J Contemp Med Research 4(6):1364–1366
Khoury ZH, Illesca P, Sultan AS (2021) Salivary Fructosamine as a noninvasive glycemic biomarker: a systematic review. JDR Clin Trans Res 6(4):382–389. https://doi.org/10.1177/2380084420954354
Janakiram C, Mehta A, Venkitachalam R (2020) Prevalence of periodontal disease among adults in India: a systematic review and meta-analysis. J Oral Biol Craniofac Res 10(4):800–806. https://doi.org/10.1016/j.jobcr.2020.10.016
Menon VU, Kumar KV, Gilchrist A et al (2006) Prevalence of known and undetected diabetes and associated risk factors in central Kerala—ADEPS. Diabetes Res Clin Pract 74(3):289–294
Papapanou PN, Sanz M, Buduneli N et al (2018) Periodontitis: consensus report of workgroup 2 of the 2017 world workshop on the classification of periodontal and peri-implant diseases and conditions. J Periodontol 89(Suppl 1):S173–S182. https://doi.org/10.1002/JPER.17-0721
American Diabetes Association (2020) 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2020. Diabetes Care 43(Suppl 1): S14-S31. https://doi.org/10.2337/dc20-S002
O’Leary TJ, Drake RB, Naylor JE (1972) The plaque control record. J Periodontol 43(1):38. https://doi.org/10.1902/jop.1972.43.1.38
Mühlemann HR, Son S (1971) Gingival sulcus bleeding–a leading symptom in initial gingivitis. Helv Odontol Acta 15(2):107–113
Nisha KJ, Janam P, Harshakumar K (2019) Identification of a novel salivary biomarker miR-143-3p for periodontal diagnosis: a proof of concept study. J Periodontol 90(10):1149–1159. https://doi.org/10.1002/JPER.18-0729
Johnson RN, Metcalf PA, Baker JR (1983) Fructosamine: a new approach to the estimation of serum glycosylprotein. An Index Diabetic Control Clin Chim Acta 127(1):87–95. https://doi.org/10.1016/0009-8981(83)90078-5
Unal I (2017) Defining an optimal cut-point value in ROC analysis: an alternative approach. Comput Math Methods Med 2017:3762651
Kuzuya T (2000) Early diagnosis, early treatment and the new diagnostic criteria of diabetes mellitus. Br J Nutr 84(Suppl 2):S177–S181
Teeuw WJ, Kosho MX, Poland DC, Gerdes VE, Loos BG (2017) Periodontitis as a possible early sign of diabetes mellitus. BMJ Open Diabetes Res Care 5(1):e000326
Baeza M, Morales A, Cisterna C et al (2020) Effect of periodontal treatment in patients with periodontitis and diabetes: systematic review and meta-analysis. J Appl Oral Sci 28:e20190248
Panezai J, Altamash M, Engstrӧm PE, Larsson A (2020) Association of glycated proteins with inflammatory proteins and periodontal disease parameters. J Diabetes Res 2020:6450742
Unal T, Firatli E, Sivas A, Meric H, Oz H (1993) Fructosamine as a possible monitoring parameter in non-insulin dependent diabetes mellitus patients with periodontal disease. J Periodontol 64(3):191–194. https://doi.org/10.1902/jop.1993.64.3.191
Morenkova SA (2004) Sravnitel’nyĭ analiz zavisimosti soderzhaniia sorbitola i fruktozamina v sliune ot kontsentratsii gliukosy krovi u bol’nykh diabetom [comparative analysis of dependence of saliva sorbitol and fructosamine levels on blood glucose level in patients with diabetes]. Biomed Khim 50(6):612–614
Manjrekar PA, Hegde A, D’souza F et al (2012) Fructosamine in non-diabetic first-degree relatives of type 2 diabetes patients: risk assessor. J Clin Diagn Res 6(5):770–773
Kandavel S, Kumar PDM (2019) Association between salivary fructosamine, plasma glycated hemoglobin, and plasma glucose levels among type II diabetes mellitus and nondiabetic individuals-a cross-sectional study. Eur J Dent 13(3):310–317
John J, Sakarde A, Chafle J et al (2023) An assessment of the utility of serum fructosamine in the diagnosis and monitoring of diabetes mellitus. Cureus 15(1):e33549
Funding
The work was self-funded by the authors.
Author information
Authors and Affiliations
Contributions
Conceptualization and design: Ambili R, Aathira Vijayakumar; Acquisition and analysis of data—Ambili R, Ashni Ann Reju and Baiju KV, Interpretation of data—Ambili R, Baiju KV, Original draft preparation—Aathira Vijayakumar, Ashni Ann Reju, Review and editing—Ambili R, Baiju KV.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Clearance was obtained from the institutional ethics committee (IEC NO: PMS/IEC/2020–21/15). The study was conducted in accordance with the Helsinki Declaration of 1975, as revised in 2013 and it was registered under Clinical Trial Registry of India (CTRI no. – CTRI/2020/11/038496).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Managed by Massimo Federici.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ambili, R., Aathira, V., Ashni, A. et al. Salivary fructosamine in diabetic and non-diabetic individuals with healthy and diseased periodontium and its changes after non-surgical periodontal therapy. Acta Diabetol (2024). https://doi.org/10.1007/s00592-024-02334-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00592-024-02334-w