Abstract
Objectives
Type 1 diabetes mellitus (T1DM), a chronic autoimmune disease characterized by insulin deficiency, is related to periodontal diseases in children and adolescents. Our aim was to profile salivary human beta-defensin (hBD)-2 and hBD-3 concentrations in relation to periodontal and T1DM status in children and adolescent populations.
Material and methods
Unstimulated saliva samples were collected from 66 participants including periodontally healthy T1DM patients (T1DM + C; n = 18), T1DM patients with gingivitis (T1DM + G; n = 20), systemically and periodontally healthy individuals (SH + C: n = 15), and systemically healthy gingivitis patients (SH + G; n = 13). Full mouth plaque index (PI), bleeding on probing (BOP), probing pocket depth (PPD), and clinical attachment level (CAL) were recorded. Salivary hBD-2 and hBD-3 concentrations were evaluated by sandwich ELISA method. A p value of < 0.05 was considered statistically significant.
Results
Salivary hBD-3 concentrations were lower in T1DM groups in comparison to systemically healthy counterparts (SH + G vs. T1DM + G; p < 0.001 and SH + C vs. T1DM + C; p < 0.001). Salivary hBD-2 levels did not differ between related groups. The difference in hBD-3 concentrations between T1DM and control groups was still significant (p = 0.008) after being adjusted for PI%, BOP%, and age.
Conclusion
In the limits of study, T1DM patients were found to have decreased salivary hBD-3 concentrations, regardless of their gingival inflammatory status.
Clinical relevance
Altered salivary hBD-3 concentration can partly explain why diabetic children are more prone to periodontal diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Periodontal diseases are chronic inflammatory disorders with infectious origin. Gingivitis, a subtype of periodontal disease, affects the soft tissues of periodontium and is the predominant form of the periodontal diseases in children and adolescents [1]. Type 1 diabetes mellitus (T1DM) is chronic autoimmune disease due to pancreatic beta-cell destruction. Genetic and environmental risk factors play role in its pathogenesis [2, 3]. The onset of the T1DM is generally diagnosed in childhood. Studies that have examined the interactions between T1DM and periodontal diseases suggested that patients with T1DM demonstrated more dental plaque and bleeding index as well as greater periodontal attachment loss than healthy controls, particularly in younger populations [4,5,6,7,8,9]. According to literature, it was concluded that patients with T1DM show increased susceptibility to periodontal disease, especially those with poorer metabolic control or with diabetic complications [10]. Proper periodontal treatment may have beneficial effects on glycemic control and diabetes complications [11]. The close relationship between T2DM and periodontitis is well-defined in terms of inflammatory burden and the modulation of local oral microbiome [12, 13]. However, there are still huge gaps in the relations between T1DM and periodontitis; eventually, underlying mechanisms remain to be elucidated.
Antimicrobial peptides are small cationic polypeptide molecules widely produced by organisms [14]. In the oral cavity, human beta-defensin (hBD) 1–3 are produced in gingival epithelium and are released to saliva and gingival crevicular fluid (GCF) [15, 16]. hBD 1–3 differ from each other regarding their localizations and secretion [14,15,16]. For instance, in periodontal tissues and saliva, secretion of hBD-1 considered is to be constitutive, whereas hBD-2 and -3 have demonstrated fluctuations in response to bacterial products or inflammatory conditions [17]. hBDs play an essential role in establishing homeostasis in the human body with their antimicrobial activity and bi-directional regulatory relations to the adaptive immune system, angiogenesis, and wound healing [17]. Despite their well-defined activities on immunity, controversial findings were presented regarding how periodontal disease and DM affected hBD levels in oral biologic fluids and tissues [18, 19]. In literature, studies regarding the relationship between T1DM and hBDs are scarce; according to one study, serum levels of hBD-1 were reduced in T1DM patients compared with healthy individuals, and it can be speculated that dysregulation of hBDs might influence the disease state [20].
Saliva is an important component of the oral defense system with its flow rate and protein composition. It is also known that T1DM can alter its content and antimicrobial properties [21, 22]. To the best of our knowledge, there is no study in the literature to investigate the salivary hBD-2 and hBD-3 concentrations in relation to T1DM and periodontal status. In the present study, the hypothesis was that periodontal status and T1DM impair salivary concentrations of hBD-2 and hBD-3. Therefore, the present study aims to profile salivary hBD-2 and hBD-3 concentrations in relation to periodontal and T1DM status in children and adolescent populations.
Material and methods
Study participants
This study was approved by the local ethics board of Sakarya University Faculty of Medicine (protocol number: E-71522473–050.01.04–15,422) and was performed in full accordance with the Helsinki Declaration of 1975, as revised in 2013. Overall, 66 participants including periodontally healthy T1DM patients (T1DM + C; n = 18), T1DM patients with gingivitis (T1DM + G; n = 20), systemically and periodontally healthy individuals (SH + C; n = 15), and systemically healthy gingivitis patients (SH + G; n = 13) were recruited in the study. The participant recruitment and sample collections were performed at the Department of the Pediatric Dentistry, Faculty of Dentistry, Sakarya University in collaboration with the Department of Pediatric Endocrinology, Faculty of Medicine, Sakarya University during November 2020 to January 2021. Study participants and their parents were informed about the study protocol verbally, and written informed consents were obtained. Demographic variables including age, sex, medical and dental treatment history, disease duration, and current medications if diagnosed with T1DM were obtained by interviews. Participants with diabetes-related systemic complications, existing or previous diagnosis of renal, hepatic disorders or HIV, having history of transplantation, receival of professional dental cleaning, intake of antibiotic therapy within the last 3 months, and history of orthodontic treatment were excluded from the study. The smoking status of the parents was obtained from self-reports of parents. The participants whose parents were smokers were defined as passive smokers.
Clinical Examination
The following clinical measurements were performed: plaque index [23] (PI), bleeding on probing [24] (BOP), probing pocket depth (PPD), and clinical attachment level (CAL). These periodontal indexes were recorded by using a manual periodontal probe (PW7, Hu-Friedy, IL, US) from four sites (buccal, lingual/palatal, mesial, and distal surfaces) per tooth, excluding deciduous teeth with any type of mobility. Dental caries status of participants was evaluated by the decayed, missing, and filled teeth (dmft/DMFT) (D = Decayed, M = missing, F = filled, T = tooth) index for permanent teeth (DMFT) and deciduous teeth (dmft). Oral and periodontal examination was performed by single calibrated (kappa: 0.89) pediatric dentist (NY). Gingivitis was diagnosed according to the 2017 Classification of Periodontal and Peri-implant Diseases and Conditions [25]. Briefly, participants were diagnosed having gingivitis in the presence of BOP ≥ 10% and PPD ≤ 3 mm. Moreover, BOP 10–30% was defined as localized gingivitis and BOP > 30% as generalized gingivitis, whereas BOP < 10% in the absence of attachment and bone loss was defined as periodontal health on an intact periodontium [25].
An expert pediatrician (RP) performed metabolic examinations. Data regarding the duration of diabetes, therapeutic regimen, daily insulin dose (unites/kg), and HbA1c (%) were obtained from medical records. T1DM diagnosis was performed according to American Diabetes Association’s 2018 guideline [26]; participants with fasting plasma glucose (FPG) ≥ 126 mg/dL (7.0 mmol/L, fasting is defined as no caloric intake for ≥ 8 h) and HbA1c ≥ 6.5% (48 mmol/mol) were diagnosed as having T1DM. Participants with HbA1c ≥ 7.5% (58 mmol/mol) were defined as uncontrolled T1DM (n = 24) [26].
Sample collection
Unstimulated saliva samples were obtained from all participants before the clinical and metabolic examination between 8 and 10 AM. Participants were required to avoid eating, drinking, and tooth brushing for at least 1 h before the sample collection [27]. Then, they were spat and filled the Eppendorf tubes (5 mL) for 5 min. Afterward, the saliva samples were centrifuged (6000 g, 5 min) following that they were immediately stored at − 80 °C until analyses.
Enzyme-linked immunosorbent assay for hBDs
Commercially available ELISA kits for hBD-2 and hBD-3 (Peprotech, London, UK) were used to determine analyte concentrations. In short, wells on a 96-well plate were coated in an overnight incubation with either 100 ng of hBD-3-specific primary antibody or 50 ng of hBD-2-specific antibody per well; free binding sites were blocked using 1% BSA in PBS. To each well, 100 µL of samples was added in duplicate. A total of 50 ng of biotin-conjugated secondary antibody was used for each well and washed away after an hour; avidin-conjugated horseradish peroxidase (avidin-HRP) was let to bind to biotin for half an hour at room temperature and the washed away. A total of 100 µL of ABTS was added and its HRP–catalyzed color reaction was monitored at 405 nm wavelength (Multiskan FC, Thermo Scientific) at 5-min intervals for a minimum of 20 min. The detection limits of ELISA kits were 16–2000 pg/ml for hBD-2 and 63–4000 pg/ml for hBD-3.
Statistical analyses
The sample size of this study could not be calculated before it started because there was no study to investigate salivary hBD-2 and hBD-3 levels in related study groups. Therefore, an achieved power analysis was applied. In post-hoc analysis, alpha error was accepted as 0.05 in order to control Type I error. The power ranged from 77.6 to 99.1%. Post-hoc power analysis was performed by G* Power 3.0.10 (Franz Faul, Universitat Kiel, Kiel, Germany). All data were checked for normal distribution with box-plot- and histogram-illustrations. Data distributions of age, PI, BOP, and dmft/DMFT were normal thus presented as means and standard deviations. All categorical variables (gender and passive smoking status) were presented as frequencies and proportions (percentages) and evaluated by chi-squared test. Data distributions of hBD-2 and -3 levels were found to be skewed, therefore presented as medians and minimum–maximum values. Intragroup comparisons were performed either using a parametric independent t-test (age, DMFT/dmft, PI%, BOP%, and PPD) or with the non-parametric Mann–Whitney U-test (hBD-2 and hBD-3), depending on the data distribution of the tested parameter. Univariate general linear model was used in adjusted comparisons of hBD-2 and hBD-3. A P value of < 0.05 was considered statistically significant. The Spearman’s test was performed for correlation analyses. Statistical analyses were run by a commercially available software (IBM SPSS Statistics for Windows, version 22.0, IBM Corp., Armonk, NY, USA).
Results
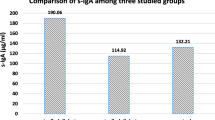
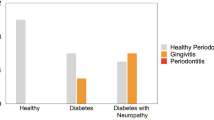
Demographic, oral/periodontal, and metabolic variables are presented in Table 1. Periodontal indexes were higher in gingivitis groups, as expected. Duration of T1DM, HbA1C, and daily insulin doses was not significantly different in participants with T1DM + gingivitis compared with T1DM + periodontally healthy individuals. Salivary hBD-2 and hBD-3 levels are presented in Table 2. Salivary hBD-3 concentrations were found to be decreased in T1DM patients with gingivitis in comparison to systemically healthy gingivitis patients (p < 0.001), and in periodontally healthy T1DM patients in comparison to systemically and periodontally healthy individuals (p < 0.001). No significant difference was observed in hBD-2 concentrations between the groups. Among the systemically healthy participants, there was no significant difference in salivary hBD-2 (p = 0.346) and hBD-3 (p = 0.393) levels between gingivitis patients in comparison to periodontally healthy individuals. In addition to these findings, no significant difference was observed in salivary hBD levels in gingivitis patients compared to periodontally healthy individuals among participants with T1DM (hBD-2 p = 0.856, hBD-3 p = 0.316). Age-, PI–, and BOP%–adjusted comparisons of hBD-2 and hBD-3 concentrations are presented in Fig. 1 (for hBD-2) and Fig. 2 (for hBD-3). According to the univariate general linear model, there was a significant difference in the adjusted (age, PI, and BOP%) hBD-3 concentrations between T1DM and control groups (p = 0.008). No significant correlation was detected between salivary hBDs, periodontal indexes, and metabolic variables (p > 0.05).
Discussion
To the best of the authors’ knowledge, this is the first study to demonstrate an association between decreased salivary hBD-3 concentrations and T1DM, regardless of individuals’ periodontal status.
In the present study, saliva was used as a biological sample. On the one hand, saliva collection is non-invasive and relatively easy, especially in the children and adolescents’ population, and it is also considered to reflect both periodontal and systemic status [28, 29]. On the other hand, the flow rate of saliva may affect the salivary peptide concentrations. To minimize this effect, salivary peptide concentrations could be presented in relation to the total amount of protein. However, we could not perform total protein determination due to a lack of sample material after several repetitions of the ELISA test, which may be considered a limitation of the present study. In our study, the current periodontal disease classification system with full mouth periodontal examination was applied to define participant periodontal status. This standardized, full mouth clinical examination is considered the gold standard for the assessment of the periodontal disease and treatment needs [30]. It also prevents the potential bias about the diagnosis and can be considered as a strength of present study. HbA1c is a demonstrative indicator to represent clinical status of DM. Participants with HbA1c ≥ 7.5% (58 mmol/mol) are defined as uncontrolled DM. In the present study, both well and uncontrolled participants were included. The metabolic status of participants may be related with our findings. Studies which include both well and uncontrolled patients separately would demonstrate the direct effect of metabolic control on salivary hBDs in T1DM, as our cross-sectional study design did not allow for the determination of fluctuations in hBD secretions in response to gingival and glycemic status and it also can be considered another limitation of the present study. Future studies including study groups with larger participants with prospective cohort design are warranted.
According to our findings, among the systemically healthy and T1DM patients, salivary hBD-2 and hBD-3 concentrations did not differ between gingivitis and periodontally healthy groups. In literature, there is no consensus regarding the relation between hBDs and gingival inflammation. Protein and RNA expression levels of hBDs in oral biological fluids and oral tissues have previously been found to be elevated, steady, or suppressed in participants diagnosed with either gingivitis or periodontitis [18, 31, 32]. These discrepancies may be explained differently: It is known that infection and pro-inflammatory mediators activate hBD-2 and -3 expression. However, bacteria, host-delivered proteases, and disrupted epithelium structure due to inflammation can limit the secretion and the levels of hBDs. For instance, our group demonstrated negative correlation between gingival tissue hBDs and total protease activity, indicating the degradation of related peptides in progressed inflammation [33]. A recent study from Dommisch et al. [31] also pointed out hBD-2 and hBD-3 can change their biological role during the development of gingival inflammation. It is important to keep in mind that the inflammatory mediators are weaker in children and inflammatory responses become stronger with age [34]. As children grow, systemic immune responses and local gingival conditions can change [1]. Future studies including different age groups in cohort study design would be helpful to understand this ambiguity. The inconsistencies in literature may also be related to studied biological samples. In saliva, the detection of hBDs can be challenging due to related peptides which can aggregate together or with salivary proteins. For instance, it has been demonstrated that salivary hBDs exhibit interaction with other antimicrobial peptides like mucins [35]. It was hypothesized that non-cationic peptides in saliva could mask hBD detection due to ionic interaction and significant size differences. Salivary concentrations do not necessarily correlate with those in GCF and gingival tissue since released hBDs in saliva may be diluted [29]. As an exudate, GCF components reflect the site-specific changes in periodontal tissues and valid source of locally derived biomarkers of periodontal disease. Yet, the collection of GCF in children is difficult because the gingival sulci in the primary teeth are shallower than in permanent teeth and the amount of this specific biological sample may be produced at low rate especially in case of periodontal health. Finally, the source oral of hBDs can be either exfoliation gingival epithelial cells, GCF, as an exudate or saliva, as a circulating fluid [36].
According to present findings, decreased salivary hBD-3 concentrations were observed in participants diagnosed with T1DM in comparison to systemically healthy individuals. The data related to hBD levels in patients with T1DM in literature are limited, yet our findings are in accordance with the existing studies. For instance, Brauner et al. [20] demonstrated reduced systemic levels of hBDs in participants with T1DM compared with healthy individuals. In another study performed in a systemically healthy children population, a positive correlation between hBD-2 and -3 in gingival tissue samples was indicated [37]. Besides, an in vitro study from Lan et al. [38] indicated the hyperglycemic conditions decreased the expression of hBD-3 in human keratinocytes at mRNA and protein levels. They demonstrated that this process involved inhibition of p38MAPK signaling which resulted from increased formation of advanced glycation end products [38]. Some other studies in the literature have demonstrated an increased level of hBD-2 in duodenal tissues and fecal samples in patients with T1DM [34, 35]. Related authors concluded that fungal and bacterial dysbiosis and intestinal inflammation are associated with beta-cell autoimmunity and development of T1DM [39, 40]. Discrepancies between the present and aforementioned studies may be related to the differences in sample material and the metabolic status of T1DM. In addition to biological sample differences, in our study, we included participants who had already been diagnosed with T1DM and most of the participants demonstrated poorly metabolic control according to their HbA1c values. Abovementioned studies, however, followed study participants during the development of T1DM. It can be speculated that the phase (onset vs. established) and metabolic control of T1DM may change the course and the severity of inflammatory responses. In present study, salivary hBD-2 concentrations did not significantly differ between study groups. hBD-2 and hBD-3 differ from each other in relation to localization in gingival epithelium and their functional characteristics [18]. It may be hypothesized that these differences of hBD-2 and hBD-3 may cause related biological interpretation which was demonstrated in our study. However, such a hypothesis is only speculative and requires further experiments.
In our study, patients diagnosed with T1DM and gingivitis demonstrated higher periodontal index scores than systemically healthy gingivitis patients. Several studies have indicated that diabetic children and adolescents have higher periodontal index scores than their systemically healthy counterparts, similar to our findings [4,5,6]. However, the underlying mechanism of this association is not clear. According to our results, it may be hypothesized that reduced levels of salivary hBD-3 can be one part of impaired immune response in diabetics and can make diabetic patients more prone to periodontal diseases. Underlying mechanisms need to be elucidated with future studies.
Conclusions
In the limits of this study, T1DM patients were found to have decreased salivary hBD-3 concentrations, regardless of the gingival inflammatory status. Impaired salivary hBD-3 concentration can partly explain why diabetic patients are more prone to periodontal diseases.
References
Moriya Y, Obama T, Aiuchi T, Sugiyama T, Endo Y, Koide Y, Noguchi E, Ishizuka M, Inoue M, Itabe H, Yamamoto M (2017) Quantitative proteomic analysis of gingival crevicular fluids from deciduous and permanent teeth. J Clin Periodontol 44:353–362. https://doi.org/10.1111/jcpe.12696
DiMeglio LA, Evans-Molina C, Oram RA (2018) Type 1 diabetes. Lancet 391:2449–2462. https://doi.org/10.1016/S0140-6736(18)31320-5
Katsarou A, Gudbjörnsdottir S, Rawshani A, Dabelea D, Bonifacio E, Anderson BJ, Jacobsen LM, Schatz DA, Lernmark Å (2017) Type 1 diabetes mellitus. Nat Rev Dis Primers 3:17016. https://doi.org/10.1038/nrdp.2017.16
Lifshitz F, Casavalle PL, Bordoni N, Rodriguez PN, Friedman SM (2016) Oral health in children with obesity or diabetes mellitus. Pediatr Endocrinol Rev 14:159–167. https://doi.org/10.17458/PER.2016.LCB.Oralhealth
Chakraborty P, Mukhopadhyay P, Bhattacharjee K, Chakraborty A, Chowdhury S, Ghosh S (2021) Periodontal disease in type 1 diabetes mellitus: Influence of pubertal stage and glycemic control. Endocr Pract 27:765–768. https://doi.org/10.1016/j.eprac.2021.01.010
Dicembrini I, Serni L, Monami M, Caliri M, Barbato L, Cairo F, Mannucci E (2020) Type 1 diabetes and periodontitis: prevalence and periodontal destruction-a systematic review. Acta Diabetol 57:1405–1412. https://doi.org/10.1007/s00592-020-01531-7
Keles S, Anik A, Cevik O, Abas BI, Anik A (2020) Gingival crevicular fluid levels of interleukin-18 and tumor necrosis factor-alpha in type 1 diabetic children with gingivitis. Clin Oral Investig 24:3623–3631. https://doi.org/10.1007/s00784-020-03238-z
Salvi GE, Franco LM, Braun TM, Lee A, Rutger Persson G, Lang NP, Giannobile WV (2010) Pro-inflammatory biomarkers during experimental gingivitis in patients with type 1 diabetes mellitus: a proof-of-concept study. J Clin Periodontol 37:9–16. https://doi.org/10.1111/j.1600-051X.2009.01500.x
Silvestre F-J, Miralles L, Liambes F, Bautista D, Sola-Izquierdo E, Hernandez-Mijares A (2009) Type 1 diabetes mellitus and periodontal disease: relationship to different clinical variables. Med Oral Patol Oral Cir Bucal 14:175–179
Genco RJ (2000) Borgnakke WS (2020) Diabetes as a potential risk for periodontitis: association studies. Periodontol 83:40–45. https://doi.org/10.1111/prd.12270
Genco RJ, Graziani F (2000) Hasturk H (2020) Effects of periodontal disease on glycemic control, complications, and incidence of diabetes mellitus. Periodontol 83:59–65. https://doi.org/10.1111/prd.12271
Pirih FQ, Monajemzadeh S, Singh N, Sinacola RS, Shin JM, Chen T et al (2000) (2021) Association between metabolic syndrome and periodontitis: The role of lipids, inflammatory cytokines, altered host response, and the microbiome. Periodontol 87:50–75. https://doi.org/10.1111/prd.12379
Teles F, Wang Y, Hajishengallis G, Hasturk H (2000) Marchesan JT (2021) Impact of systemic factors in shaping the periodontal microbiome. Periodontol 85:126–160. https://doi.org/10.1111/prd.12356
Gupta S, Bhatia G, Sharma A, Saxena S (2018) Host defense peptides: an insight into the antimicrobial world. J Oral Maxillofac Pathol 22:239–244. https://doi.org/10.4103/jomfp.JOMFP_113_16
Yilmaz D, Topcu AO, Akcay EU, Altındis M, Gursoy UK (2020) Salivary human beta-defensins and cathelicidin levels in relation to periodontitis and type 2 diabetes mellitus. Acta Odontol Scand 78:327–331. https://doi.org/10.1080/00016357.2020.1715471
Pereira AG, Costa LCM, Soldati KR, Guimarães de Abreu MHN, Costa FO, Zandim-Barcelos DL, Cota LOM (2020) Gingival crevicular fluid levels of human beta-defensin 2 and 3 in healthy and diseased sites of individuals with and without periodontitis. J Int Acad Periodontol 22:90–99
Suarez-Carmona M, Hubert P, Delvenne P, Herfs M (2015) Defensins: “simple” antimicrobial peptides or broad-spectrum molecules? Cytokine Growth Factor Rev 26:361–370. https://doi.org/10.1016/j.cytogfr.2014.12.005
Yılmaz D, Güncü GN, Könönen E, Barış E, Çağlayan F, Gursoy UK (2015) Overexpressions of hBD-2, hBD-3, and hCAP18/LL-37 in Gingiva of diabetics with periodontitis. Immunobiology 220:1219–1226. https://doi.org/10.1016/j.imbio.2015.06.013
Ertugrul AS, Dikilitas A, Sahin H, Alpaslan N, Bozoglan A, Tekin Y (2013) Gingival crevicular fluid levels of human beta-defensins 1 and 3 in subjects with periodontitis and/or type 2 diabetes mellitus: a cross-sectional study. J Periodontal Res 48:475–482. https://doi.org/10.1111/jre.12029
Brauner H, Lüthje P, Grünler J, Ekberg NR, Dallner G, Brismar K, Brauner A (2014) Markers of innate immune activity in patients with type 1 and type 2 diabetes mellitus and the effect of the anti-oxidant coenzyme Q10 on inflammatory activity. Clin Exp Immunol 177:478–482. https://doi.org/10.1111/cei.12316
Pappa E, Vougas K, Zoidakis J, Papaioannou W, Rahiotis C, Vastardis H (2021) Downregulation of salivary proteins, protective against dental caries, in type 1 diabetes. Proteomes 9:33. https://doi.org/10.3390/proteomes9030033
Cabras T, Pisano E, Mastinu A, Denotti G, Pusceddu PP, Inzitari R, Fanali C, Nemolato S, Castagnola M, Messana I (2010) Alterations of the salivary secretory peptidome profile in children affected by type 1 diabetes. Mol Cell Proteomics 9:2099–2108. https://doi.org/10.1074/mcp.M110.001057
Silness J, Loe H (1964) Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal condition. Acta Odontol Scand 22:121–135. https://doi.org/10.3109/00016356408993968
Ainamo J, Bay I (1975) Problems and proposals for recording gingivitis and plaque. Int Dent J 25:229–235
Chapple ILC, Mealey BL, Van Dyke TE et al (2018) Periodontal health and gingival diseases and conditions on an intact and a reduced periodontium: consensus report of workgroup 1 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Periodontol 89:74–84. https://doi.org/10.1111/jcpe.12940
American Diabetes Association (2018) 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2018. Diabetes Care 41:13–27. https://doi.org/10.2337/dc18-S002
Ebersole JL, Schuster JL, Stevens J, Dawson D 3rd, Kryscio RJ, Lin Y, Thomas MV, Miller CS (2013) Patterns of salivary analytes provide diagnostic capacity for distinguishing chronic adult periodontitis from health. J Clin Immunol 33:271–279. https://doi.org/10.1007/s10875-012-9771-3
Pappa E, Vastardis H, Rahiotis C (2020) Chair-side saliva diagnostic tests: an evaluation tool for xerostomia and caries risk assessment in children with type 1 diabetes. J Dent 93:103224. https://doi.org/10.1016/j.jdent.2019.103224
Güncü GN, Yilmaz D, Könönen E, Gürsoy UK (2015) Salivary antimicrobial peptides in early detection of periodontitis. Front Cell Infect Microbiol 24(5):99. https://doi.org/10.3389/fcimb.2015.00099
Ediani Machado M, Tomazoni F, Ruffo Ortiz F, Ardenghi TM, Zanatta FB (2017) Impact of partial-mouth periodontal examination protocols on the association between gingival bleeding and oral health-related quality of life in adolescents. J Periodontol 88:693–701. https://doi.org/10.1902/jop.2017.160622
Dommisch H, Skora P, Hirschfeld J, Olk G, Hildebrandt L, Jepsen S (2019) The guardians of the periodontium-sequential and differential expression of antimicrobial peptides during gingival inflammation. Results from in vivo and in vitro studies. J Clin Periodontol 46:276–285. https://doi.org/10.1111/jcpe.13084
Offenbacher S, Barros SP, Paquette DW, Winston JL, Biesbrock AR, Thomason RG, Gibb RD, Fulmer AW, Tiesman JP, Juhlin KD, Wang SL, Reichling TD, Chen KS, Ho B (2009) Gingival transcriptome patterns during induction and resolution of experimental gingivitis in humans. J Periodontol 80:1963–1982. https://doi.org/10.1902/jop.2009.080645
Özdemir M, Caglayan F, Bikker FJ, Pussinen P, Könönen E, Yamalik N, Gürsoy M, Fteita D, Nazmi K, Güncü GN, Pietiäinen M, Tolvanen M, Gürsoy UK (2020) Gingival tissue human beta-defensin levels in relation to infection and inflammation. J Clin Periodontol 47:309–318. https://doi.org/10.1111/jcpe.13227
Page RC, Offenbacher S, Schroeder HE, Seymour GJ (2000) Kornman KS (1997) Advances in the pathogenesis of periodontitis: summary of developments, clinical implications and future directions. Periodontol 14:216–248. https://doi.org/10.1111/j.1600-0757.1997.tb00199.x
Jourdain ML, Velard F, Pierrard L, Sergheraert J, Gangloff SC, Braux J (2019) Cationic antimicrobial peptides and periodontal physiopathology: a systematic review. J Periodontal Res 54:589–600. https://doi.org/10.1111/jre.12676
Güncü GN, Yilmaz D, Könönen E, Gürsoy UK (2015) Salivary antimicrobial peptides in early detection of periodontitis. Front Cell Infect Microbiol 5:99. https://doi.org/10.3389/fcimb.2015.00099
Saitoh M, Abiko Y, Shimabukuro S, Kusano K, Nishimura M, Arakawa T, Nakashima K, Takuma T, Kaku T, Igarashi S (2004) Correlated expression of human beta defensin-1, -2 and -3 mRNAs in gingival tissues of young children. Arch Oral Biol 49:799–803. https://doi.org/10.1016/j.archoralbio.2004.04.012
Lan CC, Wu CS, Huang SM, Kuo HY, Wu IH, Wen CH, Chai CY, Fang AH, Chen GS (2011) High-glucose environment inhibits p38MAPK signaling and reduces human beta-defensin-3 expression in keratinocytes. Mol Med 17:771–779. https://doi.org/10.2119/molmed.2010.00091
Graves CL, Li J, LaPato M, Shapiro MR, Glover SC, Wallet MA, Wallet SM (2017) Intestinal epithelial cell regulation of adaptive immune dysfunction in human type 1 diabetes. Front Immunol 7:679. https://doi.org/10.3389/fimmu.2016.00679
Honkanen J, Vuorela A, Muthas D, Orivuori L, Luopajärvi K, Tejesvi MVG, Lavrinienko A, Pirttilä AM, Fogarty CL, Härkönen T, Ilonen J, Ruohtula T, Knip M, Koskimäki JJ, Vaarala O (2020) Fungal dysbiosis and intestinal inflammation in children with beta-cell autoimmunity. Front Immunol 11:468. https://doi.org/10.3389/fimmu.2020.0046
Funding
This study is partly supported by Finnish Cultural foundation (JR) and by the Turku FINDOS doctoral program.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Dogukan Yilmaz, Neslihan Yilmaz, Elif Gül Aydın, Recep Polat, Verneri Nissilä, Jaana Rautava, Mervi Gürsoy, and Ulvi K. Gürsoy. The first draft of the manuscript was written by Dogukan Yilmaz, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yilmaz, D., Yilmaz, N., Polat, R. et al. Salivary levels of hBDs in children and adolescents with type 1 diabetes mellitus and gingivitis. Clin Oral Invest 26, 4897–4904 (2022). https://doi.org/10.1007/s00784-022-04457-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-022-04457-2