Abstract
Purpose
Periprosthetic joint infection (PJI) is a devastating complication following total knee or total hip arthroplasty (TKA/THA). Appropriate empiric antibiotic treatment, initiated directly after debridement and implant retention (DAIR), is suggested to contribute to treatment success. The aim of this study was to describe the microbiology and the antibiotic susceptibility in early PJI to guide future empiric treatment in a region with a low incidence of methicillin-resistant Staphylococcus aureus (MRSA).
Methods
Consecutive patients who underwent DAIR within 3 months after primary unilateral TKA or THA between January 2011 and December 2018 were retrospectively identified from the hospital electronic health records. Data on causative pathogens, antimicrobial susceptibility and the number of post-operative days until cultures demonstrated bacterial growth were collected.
Results
One hundred and eleven early PJIs were identified of which 65 (59%) were monomicrobial and 46 (41%) polymicrobial. Among all isolated pathogens, Staphylococcus aureus (n = 53; 29%) was the most commonly identified pathogen in early PJI without any involvement of MRSA. 72% of PJIs were susceptible to vancomycin which could be increased to around 90% by adding gram-negative coverage. On the 5th postoperative day, bacterial growth was observed in 98% of cases. All gram-negative bacteria demonstrated positive tissue cultures on the 4th postoperative day.
Conclusion
Vancomycin combined with ciprofloxacin or a third generation cephalosporin provided the highest antimicrobial coverage of all responsible pathogens identified in early PJI. Empiric treatment of gram-negative treatment can be safely terminated in the absence of gram-negative pathogens after 4 days of culturing in cases without preoperative antibiotic treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Periprosthetic joint infection (PJI) is one of the most serious complications following total knee or hip arthroplasty (TKA/THA) and accounts for up to 25% of failed TKA and 15% of failed THA [1, 2]. The annual number of THAs and TKAs are projected to increase substantially [3] which will eventually also lead to an increase in PJI cases.
PJI can be subdivided into early (< 3 months after surgery), delayed (3–12 months after surgery) and late (> 1 year after surgery) infections [4]. Early PJI is the most frequently encountered subtype and is generally treated by means of debridement, antibiotics and implant retention (DAIR) with varying success rates (23–100%) [5, 6].
Several studies have suggested factors associated with an improved treatment outcome of DAIR. These factors include absence of renal- and/or liver failure, uncemented arthroplasty, failure in timely initiation of DAIR (< 3 weeks of onset of symptoms), absence of MRSA among the pathogens, and exchange of mobile parts [7,8,9]. Despite ongoing efforts to elucidate the effectiveness of DAIR, empiric antibiotic treatment remains an understudied aspect even though several scientific associations between ineffective empiric therapy and treatment failure have been suggested [10, 11].
Following DAIR, empiric antibiotic therapy should be commenced directly after surgery. Since the results of the intra-operative tissue cultures are only available a few days after surgery, the post-surgery choice of antibiotics is usually aimed at the organisms most likely to cause the PJI [12]. Because biofilm formation in PJI starts directly after exposure to the pathogen [13], rapid exposure of the causative pathogen to an adequate antibiotic agent is believed to contribute to treatment success [10, 11].
In the past few years, concerns have been raised about the increase in antibiotic resistance among pathogens causing PJI. For example, research has suggested that methicillin resistance among coagulase-negative staphylococci (CNS) strains in PJI has increased from 2 [14] to 75% in more recent years [15, 16]. Current (American) guidelines advocate the empiric use of a broad spectrum β-lactam combined with vancomycin [6] and in the past, a British study recommended the use of vancomycin combined with a carbapenem [17]. Unfortunately, the spectrum of causative pathogens differs between countries and regions [18]. Considering the latter, these previous recommendations may not be applicable to regions associated with a low incidence of methicillin-resistant Staphylococcus aureus (MRSA) where vancomycin is used as a second resort in case of proven resistance to, or contraindications for other (less toxic or more effective) antibiotics. Therefore, the aim of this study was to describe the spectrum of causative pathogens and the corresponding antibiotic resistance patterns in a large general teaching hospital in the Netherlands. Using this information, we aim to provide guidance on the optimization of the empiric treatment of early PJI in this region associated with a low incidence of MRSA.
Materials and methods
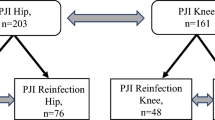
All consecutive patients who underwent debridement, antibiotics and implant retention (DAIR) surgery within 3 months after primary unilateral TKA or THA between January 2011 and December 2018 were retrospectively identified from hospital electronic health records of a large Dutch teaching hospital.
Cases with eventual negative tissue cultures or patients that had received preoperative antibiotic treatment were excluded. Cases were also excluded if patients underwent early revision surgery preceding DAIR for aseptic failure or in the presence of positive tissue cultures obtained during primary implantation.
Patient records were reviewed to retrieve gender, age, the American Society of Anesthesiologists (ASA) classification at the time of THA or TKA implantation, cement use during index implantation as well as up to 6 tissue culture results along with the corresponding antibiotic resistance patterns obtained during DAIR. Furthermore, the number of postoperative days until tissue cultures demonstrated bacterial growth and the time until the determination of the corresponding antibiotic susceptibilities was retrieved. Antibiotic susceptibility was compared for 9 potential empiric treatment strategies: flucloxacillin, amoxicillin–clavulanic acid, cefazolin, cefuroxime, ciprofloxacin, ceftriaxone, or vancomycin monotherapy, and for vancomycin plus either ceftriaxone or ciprofloxacin combination therapy.
Data related to subsequent DAIR procedures were excluded. PJI was diagnosed according to the major Musculoskeletal Infection Society (MSIS) criteria by means of 2 or more tissue cultures demonstrating growth of an identical pathogen [19].
Furthermore, the Dutch national joint registry was consulted to verify that no cases were missed that underwent revision surgery elsewhere.
The study received approval of the Rijnstate Committee for Research Involving Human Subjects that granted a waiver of informed consent (study number: 2018–1333). Statistical analysis was performed using IBM SPSS Statistics (version 25).
Surgery protocol
All patients were screened for nasal carriage of S. aureus through nasal swab cultures. Confirmed carriers were instructed to apply mupirocin ointment (20 mg/g) in the nares three times a day and to use chlorhexidine soap (40 mg/mL) once daily to wash their body and hair. This eradication treatment was started three days before surgery and continued for five days.
Within an hour before the index arthroplasty surgery patients received prophylactic administration of cefazolin. Antibiotic prophylaxis was discontinued 24 h postoperatively. All patients underwent THA by posterolateral approach. Poor bone quality, bone loss or age > 75 years were indications for cemented (Exeter®; Stryker Howmedica) THA. Otherwise, uncemented implants (Zweymuller®; Zimmer up to 2014 and from then on CLS Spotorno®/Allofit; Zimmer) were used. All TKAs were performed using cemented implants (LCS®, DePuy Synthes) through a medial parapatellar arthrotomy. Bone cement (Palacos G®; Heraeus) in both TKA and THA contained gentamicin. All patients were subjected to prospective surveillance of PJI for at least 3 months after surgery. In case of a suspected early infection (persistent wound leakage 10 days after primary THA/TKA, fever, rising levels of C-reactive protein) DAIR with exchange of mobile parts was performed and six intra-articular tissue cultures were obtained. Awaiting culture results, empiric treatment with intravenous antibiotics (flucloxacillin 8 g every 24 h through continuous infusion) was initiated according to the hospital protocol.
Microbiological methods
The obtained tissue biopsies were homogenized and inoculated onto sheep blood, chocolate, MacConkey, fastidious anaerobe, and neomycin anaerobic blood agars (Oxoid Ltd., Basingstoke, UK) and incubated at 35 °C for 10 days. Sheep blood and chocolate agars were incubated at 5% CO2; MacConkey at 5% O2; and the anaerobic agars were incubated anaerobically. In addition, 0.2 mL of the homogenized substance was inoculated into brain heart infusion broth (Brewer, Oxoid Ltd., Basingstoke, UK) and incubated at 35 °C. At day 4 of the 7-day (until mid-2016) or day 6 of the 10-day incubation period, or earlier if cloudy, 0.1 mL of broth was subcultured on chocolate agar, fastidious anaerobe, and neomycin anaerobic blood agars for 3 (until 2016) or 4 days. Microorganisms were identified with the use of a Bruker Biotyper MALDI-TOF MS (Bruker, Bremen, Germany). Antibiotic resistance patterns were registered per patient.
Statistical methods
The coverage of nine potential empiric treatment strategies (flucloxacillin, amoxicillin–clavulanic acid, cefazolin, cefuroxime, ceftriaxone, or vancomycin monotherapy, and vancomycin plus ceftriaxone or ciprofloxacin combination therapy) was studied. In the presence of polymicrobial infections, a cumulative sensitivity pattern was formulated (e.g., if one or more pathogens of a polymicrobial infection were resistant to an antibiotic, the case would be registered as resistant to this antibiotic regimen). Percentages were compared to reveal the antibiotic regimen that yielded the highest sensitivity rate.
Results
A total of 160 cases were identified from the electronic health records. Forty-nine (31%) patients were excluded since tissue cultures remained negative, leaving 111 cases for analysis. Patient demographics are presented in Table 1. Through consultation of the Dutch national joint registry, no cases were identified that underwent early revision surgery elsewhere related to infection.
Among these 111 cases, 65 (59%) were monomicrobial and 46 (41%) were polymicrobial infections. Eighty-one (73%) cases were infected with gram-positive pathogens only and 11 (10%) cases with gram-negative pathogens (Table 2). All isolated pathogens and their frequency of involvement are displayed in supplementary file. Staphylococcus aureus was the most commonly identified species (29%, Table 2). The cumulative susceptibilities of nine potential empiric antibiotic regimens are displayed in Fig. 1, identifying vancomycin as the superior antibiotic agent regarding in vitro antibiotic coverage. Combination therapy of vancomycin and ciprofloxacin or a third-generation cephalosporin yielded the highest coverage (88–92%).
Bar chart illustrating the percentage of cases susceptible to the different empiric antibiotic regimens. Green bars represent monotherapy and red bars represent combination therapy. FLX: flucloxacillin, AMC: amoxicillin–clavulanic acid, CFZ: cefazolin, CXM: cefuroxime, CRO: ceftriaxone, CIP: ciprofloxacin, VAN: vancomycin
The mean number of days until bacterial growth was 2.5 ± 1.2 days (range 1–9 days). In 108 (98%) cases, the first positive tissue culture results were obtained within five postoperative days (Fig. 2). Two cultures (1.8%) showed growth later, respectively, after 6 days (Corynebacterium species) and 9 days (Cutibacterium acnes). In a single case, data on the time to culture results were missing. Gram-negative pathogens grew after a maximum of 4 days, whereas gram-positive pathogens took up to 10 days to grow (Fig. 3). Antibiotic susceptibilities were available after a mean of 3.7 ± 1.6 days (range 2–13 days).
Discussion
Staphylococcus aureus was the most commonly identified pathogen in early PJI in this study, notably without any involvement of MRSA. Despite the absence of MRSA, cumulative antimicrobial susceptibility demonstrated vancomycin as the empiric agent that yielded the highest coverage due. Furthermore, 41% of PJIs were polymicrobial in nature which underlines the importance of broad-spectrum empiric antibiotic treatment.
The identification of Staphylococcus aureus and CNS as the most prevalent pathogens and the spectrum of other isolated pathogens in this study are in line with the results of several previous studies from different topographic regions describing the microbiology of PJI [16, 17, 20,21,22,23]. However, this is the first study to specifically address causative pathogens in early PJI and the corresponding spectrum of antimicrobial susceptibility. Only a few previous studies have provided specific recommendations on the optimal empiric antibiotic treatment while taking this antimicrobial susceptibility into account. For example, Moran et al. recommended the use of vancomycin combined with a carbapenem, whereas Fulkerson et al. had previously recommended the specific use of either vancomycin or a 3rd or 4th generation cephalosporin [16, 17]. Two more recent studies also recommended vancomycin as the designated empiric agent; however the common denominator regarding these studies is a relatively high incidence of MRSA [24, 25]. The generalizability of these recommendations to regions with low incidences of MRSA is therefore questionable [26]. Recently, a Dutch study recommended the use of cefazolin for the empiric treatment of PJI [21]. However, only 3 different potential empiric antibiotic agents were incorporated in their analysis and vancomycin was not investigated. Taken together, there is no consensus on the optimal choice of empiric antibiotic treatment. From the studies presented there appears a tendency toward advocating vancomycin as the empiric treatment of choice in particular for regions with MRSA. In our study, no infections with MRSA occurred and still vancomycin had the highest coverage of all monotherapeutic antibiotic regimens that were analyzed. The coverage could be further increased by adding ceftriaxone or ciprofloxacin to cover gram-negative pathogens.
Still, one should consider vancomycin’s important disadvantages such as increased toxicity compared to beta-lactam antibiotics, necessity for blood level measurements, its decreased effectiveness against methicillin-sensitive Staphylococcus aureus, and its suboptimal activity in biofilms [27,28,29].
It is important to note that a high coverage does not necessarily imply high efficacy. Reaction with the components of the biofilm matrix reduces the ability of several antibiotics to penetrate the biofilm which results in a reduced exposure of bacteria to the antibiotics and a subsequent decrease in antibiotic action [30].
Timely termination of empiric antibiotics when cultures remain negative could reduce the costs associated with unnecessary administration of antibiotics, reduce the in-hospital stay, decrease the emergence of resistant organisms, and reduce the risk of potential side effects related to antibiotic toxicity. The proposition to reduce the duration of the post-operative antibiotic therapy is not new and it has recently been proposed to reduce the coverage of gram-negative bacilli to not more than 3 days [31]. These results match our findings with gram-negative pathogens growing before day 4 (Fig. 3). These combined findings suggest that empiric treatment of gram-negative pathogens can be safely terminated on day 4 in case of no growth of gram-negative pathogens by that timepoint.
Among all included cases, 98% of all cultures demonstrated bacterial (gram-positive or gram-negative) growth by the fifth day. Based on this result and considering that 30% of primary DAIR procedures were excluded because PJI was ruled out, termination of empiric antibiotics in certain cases might be considered in cases with a low suspicion of infection. Obviously, the decision to terminate antibiotics in patients with preoperatively administered antibiotics should be considered with care.
Limitations
The major limitation of this study is its retrospective design. Furthermore, the present study is a single-center study and therefore may yield institute-specific results since the spectrum of isolated pathogens in early PJI may be dependent on pre- and peri-operative anti-septic measures including the designated prophylactic antibiotics. Also, antibiotic-loaded cemented or cementless THA may influence the spectrum of isolated pathogens.
Conclusion
Effective empiric treatment has been associated with improved treatment outcomes in the treatment of PJI. A combination of vancomycin and ciprofloxacin or a third-generation cephalosporin had the highest antibiotic coverage in early PJI, even in the setting of a low incidence of MRSA. The American recommendation of vancomycin as part of an empiric treatment regime for early PJI therefore also seems applicable for regions with a low incidence of MRSA. However, this knowledge has to be balanced against other factors such as potential side effects and biofilm penetration. Empiric treatment of gram-negative pathogens can be safely terminated in the absence of gram-negative pathogens in the tissue cultures on the 4th postoperative day. In addition, if cultures remain sterile up to day 5 early PJI becomes highly unlikely and complete termination of empiric treatment could be considered. However, great care should be undertaken in the decision to terminate treatment in patients that received preoperative antibiotics.
Availability of data and material
Data are included within the manuscript and the associated supplementary data. Additional data can be made available upon special request.
References
Bozic KJ, Kurtz SM, Lau E, Ong K, Chiu V, Vail TP, Rubash HE, Berry DJ (2010) The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop Relat Res 468(1):45–51. https://doi.org/10.1007/s11999-009-0945-0
Bozic KJ, Kurtz SM, Lau E, Ong K, Vail TP, Berry DJ (2009) The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am 91(1):128–133. https://doi.org/10.2106/jbjs.H.00155
Kurtz S, Ong K, Lau E, Mowat F, Halpern M (2007) Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 89(4):780–785. https://doi.org/10.2106/jbjs.F.00222
Zimmerli W, Trampuz A, Ochsner PE (2004) Prosthetic-joint infections. N Engl J Med 351(16):1645–1654. https://doi.org/10.1056/NEJMra040181
Fernández-Sampedro M, Fariñas-Alvarez C, Garces-Zarzalejo C, Alonso-Aguirre MA, Salas-Venero C, Martínez-Martínez L, Fariñas MC (2017) Accuracy of different diagnostic tests for early, delayed and late prosthetic joint infection. BMC Infect Dis 17(1):592. https://doi.org/10.1186/s12879-017-2693-1
Osmon DR, Berbari EF, Berendt AR, Lew D, Zimmerli W, Steckelberg JM, Rao N, Hanssen A, Wilson WR (2013) Diagnosis and management of prosthetic joint infection: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis 56(1):e1–e25. https://doi.org/10.1093/cid/cis803
Wouthuyzen-Bakker M, Sebillotte M, Lomas J, Taylor A, Palomares EB, Murillo O, Parvizi J, Shohat N, Reinoso JC, Sánchez RE, Fernandez-Sampedro M, Senneville E, Huotari K, Barbero JM, Garcia-Cañete J, Lora-Tamayo J, Ferrari MC, Vaznaisiene D, Yusuf E, Aboltins C, Trebse R, Salles MJ, Benito N, Vila A, Toro MDD, Kramer TS, Petersdorf S, Diaz-Brito V, Tufan ZK, Sanchez M, Arvieux C, Soriano A (2019) Clinical outcome and risk factors for failure in late acute prosthetic joint infections treated with debridement and implant retention. J Infect 78(1):40–47. https://doi.org/10.1016/j.jinf.2018.07.014
Qu GX, Zhang CH, Yan SG, Cai XZ (2019) Debridement, antibiotics, and implant retention for periprosthetic knee infections: a pooling analysis of 1266 cases. J Orthop Surg Res 14(1):358. https://doi.org/10.1186/s13018-019-1378-4
Tornero E, Morata L, Martínez-Pastor JC, Bori G, Climent C, García-Velez DM, García-Ramiro S, Bosch J, Mensa J, Soriano A (2015) KLIC-score for predicting early failure in prosthetic joint infections treated with debridement, implant retention and antibiotics. Clin Microbiol Infect 21(8):786.e789-786.e717. https://doi.org/10.1016/j.cmi.2015.04.012
Peel TN, Cheng AC, Choong PF, Buising KL (2012) Early onset prosthetic hip and knee joint infection: treatment and outcomes in Victoria, Australia. J Hosp Infect 82(4):248–253. https://doi.org/10.1016/j.jhin.2012.09.005
Puhto AP, Puhto T, Niinimäki T, Ohtonen P, Leppilahti J, Syrjälä H (2015) Predictors of treatment outcome in prosthetic joint infections treated with prosthesis retention. Int Orthop 39(9):1785–1791. https://doi.org/10.1007/s00264-015-2819-2
Burke JF (1961) The effective period of preventive antibiotic action in experimental incisions and dermal lesions. Surgery 50:161–168
Gbejuade HO, Lovering AM, Webb JC (2015) The role of microbial biofilms in prosthetic joint infections. Acta Orthop 86(2):147–158. https://doi.org/10.3109/17453674.2014.966290
Møller JK (1988) Drug resistance and plasmid profiles in Staphylococcus epidermidis in 1964 and 1986. J Hosp Infect 12(1):19–27. https://doi.org/10.1016/0195-6701(88)90118-1
Nickinson RS, Board TN, Gambhir AK, Porter ML, Kay PR (2010) The microbiology of the infected knee arthroplasty. Int Orthop 34(4):505–510. https://doi.org/10.1007/s00264-009-0797-y
Fulkerson E, Valle CJ, Wise B, Walsh M, Preston C, Di Cesare PE (2006) Antibiotic susceptibility of bacteria infecting total joint arthroplasty sites. J Bone Joint Surg Am 88(6):1231–1237. https://doi.org/10.2106/jbjs.E.00004
Moran E, Masters S, Berendt AR, McLardy-Smith P, Byren I, Atkins BL (2007) Guiding empirical antibiotic therapy in orthopaedics: The microbiology of prosthetic joint infection managed by debridement, irrigation and prosthesis retention. J Infect 55(1):1–7. https://doi.org/10.1016/j.jinf.2007.01.007
Kuiper JW, Vos S, Burger TJ, Colen S (2016) Variety in diagnosis and treatment of periprosthetic joint infections in Belgium and the Netherlands. Acta Orthop Belg 82(2):149–160
Parvizi J, Gehrke T (2014) Definition of periprosthetic joint infection. J Arthroplasty 29(7):1331. https://doi.org/10.1016/j.arth.2014.03.009
Gundtoft PH, Pedersen AB, Schønheyder HC, Møller JK, Overgaard S (2017) One-year incidence of prosthetic joint infection in total hip arthroplasty: a cohort study with linkage of the Danish Hip Arthroplasty Register and Danish Microbiology Databases. Osteoarthritis Cartilage 25(5):685–693. https://doi.org/10.1016/j.joca.2016.12.010
Van Erp JHJ, Heineken AC, Van Wensen RJA, Van Kempen R, Hendriks JGE, Wegdam-Blans M, Fonville JM, Van Der Steen MCM (2019) Optimization of the empirical antibiotic choice during the treatment of acute prosthetic joint infections: a retrospective analysis of 91 patients. Acta Orthop 90(5):455–459. https://doi.org/10.1080/17453674.2019.1621595
Duque AF, Post ZD, Lutz RW, Orozco FR, Pulido SH, Ong AC (2017) Is there still a role for irrigation and debridement with liner exchange in acute periprosthetic total knee infection? J Arthroplasty 32(4):1280–1284. https://doi.org/10.1016/j.arth.2016.10.029
Koh IJ, Han SB, In Y, Oh KJ, Lee DH, Kim TK (2015) Open debridement and prosthesis retention is a viable treatment option for acute periprosthetic joint infection after total knee arthroplasty. Arch Orthop Trauma Surg 135(6):847–855. https://doi.org/10.1007/s00402-015-2237-3
Ravi S, Zhu M, Luey C, Young SW (2016) Antibiotic resistance in early periprosthetic joint infection. ANZ J Surg 86(12):1014–1018. https://doi.org/10.1111/ans.13720
Sousa R, Pereira A, Massada M, da Silva MV, Lemos R, Costa e Castro J, (2010) Empirical antibiotic therapy in prosthetic joint infections. Acta Orthop Belg 76(2):254–259
Lee AS, de Lencastre H, Garau J, Kluytmans J, Malhotra-Kumar S, Peschel A, Harbarth S (2018) Methicillin-resistant Staphylococcus aureus. Nat Rev Dis Primers 4:18033. https://doi.org/10.1038/nrdp.2018.33
Farber BF, Kaplan MH, Clogston AG (1990) Staphylococcus epidermidis extracted slime inhibits the antimicrobial action of glycopeptide antibiotics. J Infect Dis 161(1):37–40. https://doi.org/10.1093/infdis/161.1.37
Souli M, Giamarellou H (1998) Effects of slime produced by clinical isolates of coagulase-negative staphylococci on activities of various antimicrobial agents. Antimicrob Agents Chemother 42(4):939–941. https://doi.org/10.1128/aac.42.4.939
König C, Schwank S, Blaser J (2001) Factors compromising antibiotic activity against biofilms of Staphylococcus epidermidis. Eur J Clin Microbiol Infect Dis 20(1):20–26. https://doi.org/10.1007/pl00011232
Fux CA, Costerton JW, Stewart PS, Stoodley P (2005) Survival strategies of infectious biofilms. Trends Microbiol 13(1):34–40. https://doi.org/10.1016/j.tim.2004.11.010
Duployez C, Wallet F, Migaud H, Senneville E, Loiez C (2020) Culturing periprosthetic tissues in BacT/Alert® Virtuo blood culture bottles for a short duration of post-operative empirical antibiotic therapy. J Bone Jt Infect 5(3):145–150. https://doi.org/10.7150/jbji.44621
Funding
All authors, their immediate families, and any research foundation with which they are affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article.
Author information
Authors and Affiliations
Contributions
RS was involved in literature research and data collection. RS, PK, JG, MS and JvS were involved in data interpretation and writing of the manuscript. JvS and MS were involved in study supervision. RS, PK, JG and MS were involved in study design. RS and MS were involved in study set up.
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Consent to publish
All authors hereby consent to publication of the work.
Ethical approval
The study received approval of the Rijnstate Committee for Research Involving Human Subjects that granted a waiver of informed consent (study number: 2018–1333).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Scholten, R., Klein Klouwenberg, P.M.C., Gisolf, J.E.H. et al. Empiric antibiotic therapy in early periprosthetic joint infection: a retrospective cohort study. Eur J Orthop Surg Traumatol 33, 29–35 (2023). https://doi.org/10.1007/s00590-021-03156-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-021-03156-0