Abstract
Objective
To describe the surgical application of anterior minimally invasive plating osteosynthesis (MIPO) using reversed proximal humerus internal locking system (PHILOS) plate for multifragmentary distal humeral shaft fractures.
Methods
Twelve patients with distal humeral shaft fractures (type 12B, n = 6 and type 12C, n = 6) were operated on by anterior MIPO and reversed PHILOS plate fixation. The amount of intact bone in the distal fragment was measured by fracture-to-coronoid distance (FCD). Data of the postoperative alignment, complications, union time, and clinical outcomes were collected.
Results
The mean time for fractures to unite in all patients was 14.8 weeks (range 12–22). There was no perioperative complication. The mean FCD was 4.8 cm (range 2.1–8.1). The mean coronal angulation was 3.4° (range 0–9), and the mean sagittal angulation was 1° (range 0–5). All patients had excellent UCLA shoulder score and MEP score results, and the mean range of elbow motion was 140° (range 130–145).
Conclusion
Anterior MIPO using reversed PHILOS plate is safe and effective for multifragmentary fractures of the distal humeral shaft even in a fracture with a length of intact bone above the coronoid fossa of only 2 cm.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The incidence of humeral shaft fracture is 3–5% of all fractures [1]. Optimal management of fractures located in the distal part is technically challenging and controversial. Despite nonoperative treatment providing high union rates and excellent functional outcomes, difficulty in controlling alignment by functional brace and a late angular deformity are still problems in distal humeral shaft fractures [2, 3].
In the literature, there are several options of surgical treatment. One option is conventional open reduction and plate fixation when operative treatment is indicated. Disadvantages of this method are devascularization of the fracture zone and complications, such as nonunion and radial nerve injury [4, 5]. Another option is closed intramedullary nailing that provides biological preservation and has a load-sharing property. There are two techniques of nailing: antegrade nailing and retrograde nailing. The disadvantages of antegrade nailing are shoulder problems from the approach to the nail entry point and its unsuitability for a small medullary canal and a short distal fragment [6, 7]. The drawback of retrograde nailing is higher risk of an iatrogenic supracondylar fracture [8, 9].
Minimally invasive plating osteosynthesis (MIPO) is an innovative alternative to these techniques. MIPO preserves the blood supply of the fracture zone and avoids complications from nailing. MIPO of the humeral shaft can be used via anterior [10,11,12,13,14,15,16], posterior [17,18,19], or lateral approaches [20]. Anterior MIPO has been reported to be safe and has provided excellent clinical outcomes. However, a limitation of this approach is when there is only a small amount of bone for fixation in a distal humeral shaft fracture. At least 6 cm of intact bone above coronoid fossa in distal fragment has been suggested to be a prerequisite for MIPO via the anterior approach [10, 13].
Proximal humerus internal locking system (PHILOS) plate is a commonly used implant for proximal humerus fixation (Fig. 1a, b). It has been used for other purposes, including fixation of the distal humeral metaphysis [21], the distal tibia [22], the proximal femur in children [23], and arthrodesis of the ankle and hindfoot [24]. Application of this implant could be alternative choice for fixing a humeral shaft fracture with a short distal fragment due to the matched contour of the plate to the metaphyseal flare of the distal humerus (Fig. 1c) and its multiple multi-directional locking screws (Fig. 1d).
Anterior MIPO using reversed PHILOS plate may be a safe and effective management for humeral shaft fractures with a short distal fragment. Thus, we describe a modification of the technique applied in 12 patients who underwent fixation of distal humeral shaft fractures. We report the outcomes focusing on the length of intact bone in distal fragment that is feasible for the applied implant, perioperative complications, as well as radiologic and clinical outcomes.
Materials and methods
A retrospective case series of anterior MIPO with reversed PHILOS plate fixation was performed on distal humeral shaft fractures in consecutively recruited 12 patients by one surgeon at trauma unit in a tertiary center between April 2016 and December 2018. No eligible patients declined to participate. The inclusion criteria were closed multifragmentary distal humeral shaft fracture and age ≥ 18 years. The exclusion criteria were an open fracture, pathological fracture, and age < 18 years. The demographic data, cause of injury, associated injury, fracture configuration by AO/OTA classification, and time-to-operate were recorded. The radiographs were reviewed, and the distance from fracture site to upper edge of coronoid fossa was measured and labeled as fracture-to-coronoid distance (FCD). This study has been approved by the ethical committees of Buddhachinaraj Hospital in accordance with the Declaration of Helsinki.
Surgical technique
All of the patients were performed operations under general anesthesia. For each patient, the affected arm was placed on a radiolucent table, and the surgeon positioned next to the lateral side of the arm. During the operation, the forearm was maintained in supination position to move the radial nerve away from the humeral shaft [10]. The operation started with a 4–6 cm distal skin incision that was 2.5 cm above the antecubital crease. After the lateral border of biceps muscle was identified (Fig. 2a), the biceps muscle was retracted medially to expose the brachialis muscle. The musculocutaneous nerve, which is located on the anteromedial surface of brachialis muscle, was identified. After that, the muscle was longitudinally divided 1.5–2 cm lateral to this nerve to expose the distal fragment of the humerus (Fig. 2b). A proximal skin incision between the medial border of the deltoid muscle and the lateral border of biceps muscle was made (Fig. 2c), and dissection was done directly to the anterior crest of the proximal fragment of humerus. A submuscular tunnel under the brachialis muscle connecting the proximal and the distal windows was created. A proper-length PHILOS plate (Synthes, Oberdorf, Switzerland) was chosen and was applied in a reversed position, namely proximal to distal, through the tunnel. The end of the plate was placed just above the coronoid fossa and parallel to the humeral shaft, and then a fluoroscope was used to check plate position. Two locking screws were inserted into the distal fragment. Shortening was corrected by longitudinal traction in elbow-flexion position, and then a plate reduction technique was performed by reducing the proximal portion of the plate to the proximal fragment. After alignment of the plate and the proximal fragment parallel, one screw was inserted in the proximal fragment. The plate position and fracture alignment were checked again by fluoroscopy, and then the remaining screws were applied. The length of the screws in the proximal fragment was carefully chosen so that the tip of the each screw just passed the posterior cortex to avoid injury to the radial nerve. At the final fixation, 3–4 screws were inserted in proximal fragment and at least 6 screws in distal fragment (Fig. 3). The wounds were closed over a vacuum drain.
a In the distal window, the lateral border of biceps muscle was identified before it was retracted medially to expose brachialis muscle. The medial border of deltoid muscle was identified in the proximal window. b After retracting the biceps muscle medially, the brachialis muscle was then divided longitudinally to expose distal fragment. c In proximal window, dissection was carried out between the medial border of the deltoid muscle and the lateral border of the biceps muscle to expose the anterior crest of humerus
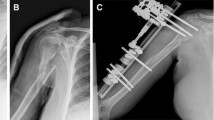
A 58-year-old male with a history of motorcycle accident was diagnosed with a closed distal humeral shaft fracture. a, b The initial plain radiograph showed a comminuted fracture (AO/OTA 12-C3) with an FCD of 3.7 cm. c, d At 1 year after anterior MIPO using reversed PHILOS, the fracture was united. e The surgical wounds were completely healed without any consequences. f, g The injured limb was fully functional
A 51-year-old female with a history of simple fall was diagnosed with a closed distal humeral shaft fracture. a The initial plain radiograph showed a wedge fracture (AO/ATO 12-B1) with an FCD of 2.1 cm. b–e At 1 year after anterior MIPO using reversed PHILOS, the fracture was united and the injured limb regained normal ROM
A 27-year-old male with a history of motorcycle accident was diagnosed with a closed distal humeral shaft fracture. a The initial plain radiograph showed a segmental fracture (AO/OTA 12-C3) with FCD of 2.8 cm. b, c Solid union was achieved with anterior MIPO using reversed PHILOS. d–g At 1 year postoperatively, the injured limb regained its normal ROM and strength
The drain was removed at 2 days after surgery, and then physical therapy was started for restoring motion of elbow and shoulder joints. No sling or any external immobilizers were required after the surgery. Weight bearing activities of the affected arms were allowed at 12 weeks after surgery or presentation of bridging callus. Radiographic assessment including fracture alignment and fracture union was recorded during immediate postoperative period and at every 6–8 weeks. After fracture union, the patients were counseled for implant removal only in particular circumstances, such as implant irritation and infection. Clinical assessment including postoperative complications, range of motion (ROM) of affected elbow, University of California at Los Angeles (UCLA) shoulder score and Mayo Elbow Performance (MEP) score was assessed and record.
Results
The present case series included 9 males and 3 females with a mean age of 34.2 years (range 19–58). Eleven patients were injured from motor vehicle accidents, and one from a simple fall. Floating knee was present in one patient and cerebral concussion in two patients. AO/OTA classification included 12B (n = 6) and 12C (n = 6). The mean of FCD was 4.8 cm (range 2.1–8.1). The mean time-to-surgery was 26.5 h (range 9–48) (Table 1).
There were no postoperative radial nerve palsies or any other complications. The mean follow-up time was 19.3 months (range 12–28). All fractures were united in a mean duration of 14.8 weeks (range 12–22). By physical examination, no apparent angular deformities were observed in any patients. By radiographic images, they had a mean coronal angulation of 3.4° (range 0–9) and a mean sagittal angulation of 1° (range 0–5). The mean ROM of the elbow was 140° (range 130–145). The mean MEP score was 98 (range 94–100), and the mean UCLA score was 34.4 (range 32–35). These were all considered to be excellent values (Table 2).
Discussion
The suitable technique and suitable implant for fixation of multifragmentary humeral shaft fracture with short distal fragment are currently still controversial. In the present study, fracture union and excellent clinical outcomes were achieved in all 12 cases of anterior MIPO using reversed PHILOS for distal humeral shaft fractures with short FCD.
MIPO of the distal humeral shaft can be used via anterior [10,11,12,13,14,15,16], posterior [17,18,19], or lateral approaches [20]. The posterior approach has advantage of more area for fixation because the implant can be placed distally to the end of posterior aspect of lateral column. However, drawbacks of this approach include technical difficulty to apply the implant under the radial nerve and to apply reduction devices for controlling proximal fragment. Gallucci et al. reported 21 cases of posterior MIPO for distal humeral shaft fractures, of which 16 cases had apparent varus deformities, and two cases had implant irritation needing to be removed [19]. The lateral approach is another choice for distal humeral fracture [20]. With this approach, the implant can be placed distally on the lateral humeral condyle, and this placement facilitates more screws for fixation in the distal fragment. However, the radial nerve could be injured because devices still need to pass under the nerve. MIPO via the anterior approach has been widely used and has the advantage that radial nerve is further away from the surgical field, thereby lessening the risk of damage. In the present study, anterior MIPO provided good fracture union without nerve injury and any perioperative complications.
For a standard 4.5-mm narrow dynamic compression plate, 6 cm of intact bone above the coronoid fossa is required for facilitating a 3-screw fixation in the distal fragment [10, 13]. PHILOS plate has been used widely for proximal humerus fracture. Park. et al. reported nine cases with distal metaphyseal fracture of the humerus using PHILOS plate in reversed position via an open anterolateral approach [21]. In the present study, at least 6 screws were inserted into the distal fragment in all cases to ensure stable distal fixation. All fractures were united with a mean FCD of 4.8 cm and the shortest FCD of 2.1 cm, demonstrating anterior MIPO with reversed PHILOS to be a feasible option even in a case with a short distal fragment.
Fracture verification is a technically demanding step in MIPO of the humerus. Lee. et al. reported MIPO for the humeral shaft with the assistance of an external fixator to maintain fracture reduction [16]. Lee and Yoon reported using flexible nails for temporary fixation before introducing the plate [25]. In the present study, because of the shorter time-to-surgery of not more than 2 days after injury, there was less soft tissue contracture and less fracture shortening. Thus, acceptable fracture alignment was established simply by manual traction and plate reduction technique.
There were some limitations to the present study. It was an uncontrolled retrospective case series, and the number of the enrolled patients was small. Furthermore, although the reversed PHILOS plate is well-contoured to anatomy of the distal humeral shaft, no biomechanical study demonstrating the strength of the construct with the applied implant has been reported to date.
Conclusion
Anterior MIPO using reversed PHILOS plate was safe and effective in a case series of 12 adult patients. It may be a feasible option for multifragmentary fracture of distal humeral shaft with a short distal fragment. However, if FCD is less than 2 cm, MIPO via other approaches and using other implants may be more suitable.
References
Volgas DA, Stannard JP, Alonso JE (2004) Nonunions of the humerus. Clin Orthop Relat Res 419:46–50
Sarmiento A, Zagorski JB, Zych GA, Latta LL, Capps CA (2000) Functional bracing for the treatment of fractures of the humeral diaphysis. J Bone Joint Surg Am 82(4):478–486
Ekholm R, Tidermark J, Törnkvist H, Adami J, Ponzer S (2006) Outcome after closed functional treatment of humeral shaft fractures. J Orthop Trauma 20(9):591–596
An Z, Zeng B, He X, Chen Q, Hu S (2010) Plating osteosynthesis of mid-distal humeral shaft fractures: minimally invasive versus conventional open reduction technique. Int Orthop 34(1):131–135
Jawa A, McCarty P, Doornberg J, Harris M, Ring D (2006) Extra-articular distal-third diaphyseal fractures of the humerus. a comparison of functional bracing and plate fixation. J Bone Joint Surg Am 88(11):2343–2347
Bhandari M, Devereaux PJ, McKee MD, Schemitsch EH (2006) Compression plating versus intramedullary nailing of humeral shaft fractures—a meta-analysis. Acta Orthop 77(2):279–284
Chapman JR, Henley MB, Agel J, Benca PJ (2000) Randomized prospective study of humeral shaft fracture fixation. J Orthop Trauma 14(3):162–166
Lin J, Shen PW, Hou SM (2003) Complications of locked nailing in humeral shaft fractures. J Trauma 52(5):943–949
Scheerlinck T, Handelberg F (2002) Functional outcome after intramedullary nailing of humeral shaft fractures: comparison between retrograde marchetti-vicenzi and unreamed ao antegrade nailing. J Trauma 52(1):60–71
Apivatthakakul T, Arpornchayanon O, Bavornratanavech S (2005) Minimally invasive plate osteosynthesis (MIPO) of the humeral shaft fracture: is it possible? A cadaveric study and preliminary report. Injury 36(4):530–538
Pospula W, Noor TA (2006) Percutaneous fixation of comminuted fractures of the humerus: initial experience at Al Razi Hospital, Kuwait. Med Princ Pract 15(6):423–426
Zhiquan A, Bingfang Z, Yeming W, Chi Z, Peiyan H (2007) Minimally invasive plating osteosynthesis (MIPO) of middle and distal third humeral shaft fractures. J Orthop Trauma 21(9):628–633
Kobayashi M, Watanabe Y, Matsushita T (2010) Early full range of shoulder and elbow motion is possible after minimally invasive plate osteosynthesis for humeral shaft fractures. J Orthop Trauma 24(4):212–216
Shin S-J, Sohn H-S, Do N-H (2012) Minimally invasive plate osteosynthesis of humeral shaft fractures. J Orthop Trauma 26(10):585–589
Oh CW, Byun YS, Oh JK, Kim JJ, Jeon IH, Lee JH et al (2012) Plating of humeral shaft fractures: comparison of standard conventional plating versus minimally invasive plating. Orthop Traumatol Surg Res 98(1):54–60
Lee HJ, Oh CW, Oh JK, Apivatthakakul T, Kim JW, Yoon JP et al (2013) Minimally invasive plate osteosynthesis for humeral shaft fracture: a reproducible technique with the assistance of an external fixator. Arch Orthop Trauma Surg 133(5):649–657
Gallucci G, Boretto J, Vujovich A, Alfie V, Donndorff A, De Carli P (2014) Posterior minimally invasive plate osteosynthesis for humeral shaft fractures. Tech Hand Up Extrem Surg 18(1):25–30
Balam KM, Zahrany AS (2014) Posterior percutaneous plating of the humerus. Eur J Orthop Surg Traumatol 24(5):763–768
Gallucci GL, Boretto JG, Alfie VA, Donndorff A, De Carli P (2015) Posterior minimally invasive plate osteosynthesis (MIPO) of distal third humeral shaft fractures with segmental isolation of the radial nerve. Chir Main 34(5):221–226
Ji F, Tong D, Tang H, Cai X, Zhang Q, Li J et al (2009) Minimally invasive percutaneous plate osteosynthesis (MIPPO) technique applied in the treatment of humeral shaft distal fractures through a lateral approach. Int Orthop 33(2):543–547
Park JH, Kim JW, Oh CH, Choi KS, Hong JY, Kim JG (2015) PHILOS plate osteosynthesis in metaphyseal fractures of the distal humerus through an anterolateral approach. Clin Shoulder Elb 18(3):128–132
Twaij H, Damany D (2013) PHILOS humerus plate for a distal tibial fracture. J Surg Case Rep 2013(1):rjs036
Cortes LE, Triana M, Vallejo F, Slongo TF, Streubel PN (2011) Adult proximal humerus locking plate for the treatment of a pediatric subtrochanteric femoral nonunion: a case report. J Orthop Trauma 25(7):e63–e67
Shearman AD, Eleftheriou KI, Patel A, Pradhan R, Rosenfeld PF (2016) Use of a proximal humeral locking plate for complex ankle and hindfoot fusion. J Foot Ankle Surg 55(3):612–618
Lee T, Yoon J (2016) Newly designed minimally invasive plating of a humerus shaft fracture; a different introduction of the plate. Int Orthop 40(12):2597–2602
Funding
There was no source of funding for this research.
Author information
Authors and Affiliations
Contributions
SJ was involved in drafting and revising the manuscript for content, including medical writing for content, study concept and design, analysis, and interpretation of data, as well as acquisition of the data. AG, NN, and WT were involved in revising the manuscript for content and analysis and interpretation of data.
Corresponding author
Ethics declarations
Conflict of interest
S. Jitprapaikulsarn, N. Neti, W. Thremthakanpon and A. Gromprasit declare that they have no conflict of interest.
Ethical approval
This study has been approved by the ethical committees of Buddhachinaraj Hospital in accordance with the Declaration of Helsinki.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jitprapaikulsarn, S., Neti, N., Thremthakanpon, W. et al. Anterior minimally invasive plating osteosynthesis using reversed proximal humeral internal locking system plate for distal humeral shaft fractures. Eur J Orthop Surg Traumatol 30, 1515–1521 (2020). https://doi.org/10.1007/s00590-020-02708-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-020-02708-0