Abstract
Objective
To report the functional and radiological results of unusual comminuted fractures of the proximal humerus, treated with ‘closed reduction and external fixation’ (CREF) using hybrid-type unilateral external fixators (EFs).
Patients and methods
Between January 2012 and June 2013, eight patients (mean age 62.6; range 48–84 years) with comminuted proximal humeral fractures extending to the humeral head and one-third proximal diaphysis were treated with CREF using hybrid-type EFs. Functional results were evaluated in terms of shoulder ranges of movement, Constant, DASH, and VAS scores, and radiological results were evaluated using antero-posterior and lateral radiograms of the treated humerus.
Results
The mean follow-up was 16.6 (range 12–28) months. The mean fixator time was 84 (range 63–118) days. The mean range of forward flexion, internal rotation, external rotation, and abduction were 145°, 61.2°, 65°, and 115°, respectively. The mean Constant, DASH, and VAS scores were 79.8, 10, and 1.75, respectively. Seven of the eight patients (87.5 %) healed radiologically. Two complications were observed in two patients: non-union and superficial pin site infection.
Conclusions
In the treatment of unusual, comminuted proximal diaphyseal humeral fractures, CREF using a hybrid-type EF is a minimally invasive, advantageous procedure with acceptable rates of healing, low risk of surgical site infection, and early range of motion.
Level of evidence
Level IV, case series.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Proximal humeral fractures include 3 % of all fractures and 20 % of upper extremity fractures [1]. One-third of the patients are females, and the incidence is higher in elderly and osteoporotic patients [2]. Currently, conservative treatment of humeral shaft fractures remains the gold standard. Although 85–90 % of patients are treated conservatively successfully, reduction loss, mal-union, and disability of the extremity can be seen [1, 3, 4]. Comminuted proximal diaphyseal humeral fractures are rare and may include head, neck, and one-third of the proximal and middle part of the diaphysis [4–8]. Most of these fractures are seen in osteoporotic, elderly patients after a minor, torsional trauma and, rarely, in younger adults after a high-energy trauma. The treatment is typically surgical because of the fracture line geometry and its tendency to be displaced by the attached muscles [2, 4, 8–12].
Humeral head and neck fractures are usually classified according to Neer, and shaft fractures are usually classified according to the AO/OTA classification system [13, 14]. Although the AO classification system gives detailed information about the fracture line geometry, in comminuted proximal humeral shaft fractures, the fracture may extend more proximally and distally; thus, they cannot be classified fully according to the AO/OTA or the Neer classification systems. Consequently, we defined them as unusual proximal humeral fractures. Stedtfeld et al. divided the humerus into five zones: the head, one-third proximal diaphysis, one-third mid-diaphysis, one-third distal diaphysis, and the condylar area. They then developed a classification system concerning zones of fracture lines and muscle insertions affecting the fractured fragments [11]. They stated that one-third proximal humeral diaphyseal fractures typically extended more proximally and more distally; thus, care should be taken that implants for internal fixation are sufficiently long [8, 11, 15]. Although a few minimally invasive techniques have been described, longer implants can cause more soft tissue damage, increasing the rate of failure and complications [8].
The aim of this retrospective case series study was to evaluate the functional and radiological results of closed reduction and external fixation (CREF) in unusual, comminuted, proximal humeral shaft fractures, using hybrid-type external fixators (EFs).
Patients and methods
This study was conducted in accordance with the Helsinki Declaration. Between February 2012 and June 2013, eight patients (six females, two males), with a mean age of 62.6 (range 42–84) years, were diagnosed with comminuted, proximal humeral diaphyseal fractures and treated with CREF (Tasarimmed Ltd Sti, Eyup, Istanbul, Turkey). These patients were evaluated retrospectively. All patients were injured after simple falls. An olecranon fracture in one patient, an ipsilateral distal radius fracture in one, and a cranial trauma in one patient were also diagnosed. The mean number of comorbidities was two: hypertension in five patients, diabetes mellitus in four, anemia in two, tongue carcinoma in one, and scoliosis in one patient.
All patients with diaphyseal humeral fractures underwent closed reductions and coaptation U-splints in the emergency department on the day after the injury, and control antero-posterior and trans-thoracic lateral X-rays were taken to evaluate the reduction. Patients with >20° angulation in the sagittal plane, >30° angulation in the coronal plane, >2 cm shortening or distraction were selected for CREF and included in the study. Patients with open fractures, neurovascular injuries, non-union, simple fractures, and fractures that extended to the glenohumeral joint were excluded from the study.
According to the Stedtfeld classification, fractures were in the one-third proximal diaphysis and extending to the greater tuberculum in all patients, and an additional one-third mid-diaphyseal extension was detected in three patients. The mean time to surgery was 6 (1–11) days. CREF using a hybrid-type EF was achieved in all patients with fluoroscopy. Passive exercises were started on the first day postoperatively and active assisted exercises 10 days after surgery.
Fixators were dynamized when callus formation was seen at two cortices on the control radiographs, and they were removed if three cortices callus formation was observed, which was defined as ‘union’. Functional results were evaluated using shoulder range of motion (ROM) and Constant, DASH, and VAS scores.
Surgical technique
Fixation of the fracture was achieved with a hybrid-type EF, which has a half-ring at its proximal end for multidirectional fixation of the humeral head. Because the axillary nerve passes within 5 cm distal from the lateral edge of the acromion, half-pins (5 mm) were inserted into the humeral head between the insertion of the supraspinatus tendon and the axillary nerve. Three or four hydroxyapatite (HA)-coated half-pins were inserted into the humeral head; one from the anterolateral to the posteromedial direction for fixation of the lesser tuberculum and one from the posterolateral to the anteromedial direction for fixation of the greater tuberculum and the head. After fixation of the proximal part of the fracture to the half-ring, two or three half-pins were inserted into the distal fragment through the 3–5 cm incision for radial nerve exploration, from the lateral to the medial direction and perpendicular to the longitudinal axis of the shaft. After fluoroscopic control of the reduction and fixation, the ROMs of the shoulder and elbow were evaluated.
Results
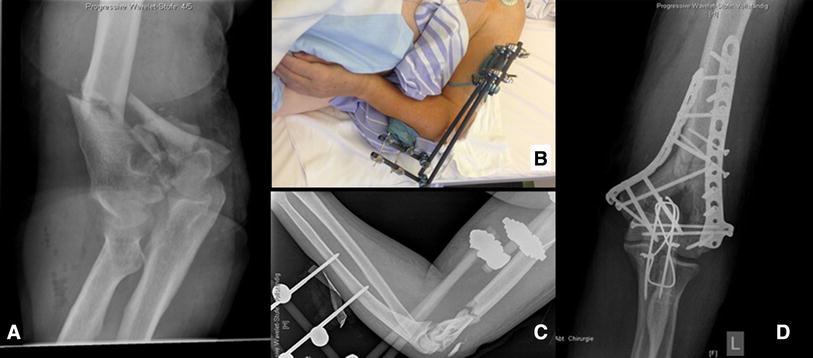
Union was achieved in seven of eight patients who were treated using CREF method (Fig. 1). The mean follow-up was 16.6 (12–28) months. The mean time to fixator dynamization was 72 (50–100) days, and the mean fixator time (FT) was 84 (63–118) days. At the 1-year follow-up, the mean Constant, DASH, and VAS scores were 78.8 (45–98), 10 (2.3–30), and 1.85 (1–3), respectively (Table 1). The mean range of forward flexion (FF), abduction, internal rotation (IR), and external rotation (ER) were 145° (100°–170°), 115° (80°–140°), 61.2° (30°–70°), and 65° (20°–70°), respectively.
Two complications were observed: superficial pin tract infection in one patient who was treated with oral antibiotic therapy and non-union in one patient who was offered pseudoarthrosis surgery, but refused because she was pain-free and satisfied. During follow-up, no humeral head avascular necrosis was observed in the control radiographs. Preoperative radial nerve palsy was seen in the patient with non-union; nerve exploration was performed during the surgery, and the nerve was intact. The palsy had resolved at the 6-month follow-up.
Discussion
Although most humeral fractures heal with conservative treatment methods, proximal diaphyseal comminuted fractures should be treated surgically because they tend to be displaced, due to the divergent effects of the deltoid and pectoralis major muscles [11, 15]. Open reduction and internal fixation (ORIF) in this type of fracture usually require an extended approaches and wide soft tissue dissections, which may result in surgical site infection, avascular necrosis, pseudoarthrosis, pericapsular fibrosis, and iatrogenic vessel or nerve injuries [16].
Lambotte first used EFs in the treatment of humeral shaft fractures [17]. It is a preferred method in open fractures with or without bone loss, comminuted fractures, concomitant vascular injury, infected non-union, and in patients with multiple trauma. Half-pins with hybrid-type EF have been suggested instead of Kirshner wires in circular EF, due to the high risk of neurovascular injury [18].
Several studies support the superiority of HA-coated over non-coated screws in osteoporotic bones. HA-coated lag screws with a DHS plate in osteoporotic intertrochanteric femur fractures showed better results and fewer complications [19]. In another study, the pullout strength of HA-coated pedicle screws was 1.6-fold higher than that of titanium-coated screws [12]. HA-coated Schanz screws were used in our series for the proximal fixation of the fractures, into possibly osteoporotic humeral heads. However, no loosening or pullout of the half-pins was observed.
In the treatment of humeral shaft fractures, some reports have proposed plate-screw osteosynthesis after open reduction or intramedullary nailing (IMN) [8, 20]. Wound problems in open reduction and shoulder problems in antegrade nailing are the main disadvantages of those techniques [8, 21].
In comminuted diaphyseal proximal humeral fractures, IMN could be considered a ‘standard’ technique but is prone to many complications. The rate of shoulder dysfunction after antegrade IMN is reported to be 6–100 %, mostly resulting from proximal migration of the nail, impingement, or rotator cuff lesions [4, 22]. Garnavos and Lasaianos [8] observed moderate shoulder pain in 8 of 15 patients, but none of the nails required removal. Our patients did not have shoulder complaints because the fixator allows early ROM exercises; indeed, they rapidly regained almost their preoperative ROMs in the shoulder and elbow.
Non-union rates in closed reduction and IMN in humeral shaft fractures have been reported to be 0–29 % [4, 23]. ORIF has a 92–96 % union rate and a 5–25 % rate of complications, including infection, non-union, mal-union, and neurovascular injury [4, 24]. We experienced only one minor complication (superficial pin site infection, treated with oral antibiotics) and one case of non-union.
Castella et al. investigated 30 humeral non-unions after ORIF; 9 patients had spiral fractures in the proximal humerus. The authors concluded that fractures in the proximal region of the humerus were prone to non-union [25]. In the study by Yang [26], 10 humeral fractures were treated with ORIF using helical plates and 3 by autologous tricortical iliac crest bone grafting; they reported that all patients healed. Brunner et al. [1] treated 15 patients with minimally invasive plate osteosynthesis, and non-union was observed in 1 patient who was treated with ORIF and autologous cancellous bone grafting. Garnavos and Lasaianos [8] treated proximal diaphyseal comminuted fractures using IMN, and union was achieved in all patients—one patient was revised to plate osteosynthesis due to the proximal migration of a nail. In our study, only one patient had non-union, but did not consent to reoperation.
Yang [26] evaluated shoulder function in their patients according to Neer’s criteria and found good and excellent results in eight patients, while two patients were unsatisfied. Brunner et al. [1] started their patients on active assisted exercises on the first postoperative day and active exercises 8–12 weeks later and found that the mean FF was 145°, IR 40°, ER 70°, abduction 135°, Constant score 74, and DASH score 34. Garnavos and Lasaianos [8] evaluated 15 patients and reported that the FF was 146°, IR 38° ER 24.5°, abduction 137.5°, and the mean Constant score was 74. Because half-pins were inserted through the safe zone and rotator tendons were not damaged, active assisted exercises were started on the first day, and active exercises in the second week, postoperatively. ROMs and functional scores in the current study were similar to these previous reports.
In the studies of Brunner et al. [1] and Yang [26], implant removal was performed in three patients due to subacromial impingement. In our study, the mean FT was 2.5 months and implants were removed in the outpatient clinic without anesthesia.
CREF is an alternative method for treatment of comminuted proximal diaphyseal humeral fractures. Closed reduction can be obtained readily; thus, soft tissue coverage of the fractured fragments is maintained, and surgical site infection is avoided. Stable fixation even in osteoporotic, elderly patients with comminuted fractures is achievable; thus, early postoperative active assistive or active ROM exercises are safe. Postoperative compression, distraction, translation, or rotation between the fragments of the fracture over the EF, when needed, is also possible with this method. A shorter surgery time and no need for anesthesia for fixator removal are other advantageous of this technique. Pin site infection is the most common complication, with an incidence of 12–50 % [27]. Patient discomfort because of cosmetics and psychological compliance and increased radiation exposure may be other disadvantages.
The major limitations of this study were the small number of patients and the short duration of follow-up. Also, no comparison with other treatment method(s) was performed.
Conclusions
Proximal diaphyseal comminuted fracture of the humerus is a rare injury; the literature about this is limited; and there is no consensus on treatment methods. CREF is a safe and effective treatment method and may be a useful alternative surgical fixation method to other procedures, such as ORIF and nailing.
References
Brunner A, Thormann S, Babst R (2012) Minimally invasive percutaneous plating of proximal humeral shaft fractures with the Proximal Humerus Internal Locking System (PHILOS). J Shoulder Elbow Surg 21(8):1056–1063. doi:10.1016/j.jse.2011.05.016
Handoll HH, Gibson JN, Madhok R (2003) Interventions for treating proximal humeral fractures in adults. Cochrane Database Syst Rev 4:CD000434. doi:10.1002/14651858.CD000434
Flatow E (2001) Fractures of the proximal humerus. In: Bucholz R, Heckman JD (eds) Fractures in adults, 5th edn. Lippincot Williams & Wilkins, Philadelphia, pp 997–1040
Walker M, Palumbo B, Badman B, Brooks J, Van Gelderen J, Mighell M (2011) Humeral shaft fractures: a review. J Shoulder Elbow Surg 20(5):833–844. doi:10.1016/j.jse.2010.11.030
Broadbent MR, Quaba O, Hadjucka C, McQueen MM (2003) The epidemiology of multifocal upper limb fractures. Scand J Surg 92(3):220–223
Lewicky YM, Sheppard JE, Ruth JT (2007) The combined olecranon osteotomy, lateral paratricipital sparing, deltoid insertion splitting approach for concomitant distal intra-articular and humeral shaft fractures. J Orthop Trauma 21(2):133–139. doi:10.1097/01.bot.0000245988.23684.79
O’Donnell TM, McKenna JV, Kenny P, Keogh P, O’Flanagan SJ (2008) Concomitant injuries to the ipsilateral shoulder in patients with a fracture of the diaphysis of the humerus. J Bone Joint Surg Br Vol 90(1):61–65. doi:10.1302/0301-620X.90B1.19215
Garnavos C, Lasanianos N (2010) Intramedullary nailing of combined/extended fractures of the humeral head and shaft. J Orthop Trauma 24(4):199–206. doi:10.1097/BOT.0b013e3181b2b74d
Heim D, Herkert F, Hess P, Regazzoni P (1993) Surgical treatment of humeral shaft fractures: the Basel experience. J Trauma 35(2):226–232
An Z, He X, Zeng B (2009) A comparative study on open reduction and plating osteosynthesis and minimal invasive plating osteosynthesis in treating mid-distal humeral shaft fractures. Zhongguo xiu fu chong jian wai ke za zhi = Zhongguo xiufu chongjian waike zazhi =Chin J Reparative Reconstr Surg 23(1):41–44
Stedtfeld HW, Biber R (2014) Proximal third humeral shaft fractures: a fracture entity not fully characterized by conventional AO classification. Injury 45(Suppl 1):S54–S59. doi:10.1016/j.injury.2013.10.030
Hasegawa T, Inufusa A, Imai Y, Mikawa Y, Lim TH, An HS (2005) Hydroxyapatite-coating of pedicle screws improves resistance against pull-out force in the osteoporotic canine lumbar spine model: a pilot study. Spine J 5(3):239–243. doi:10.1016/j.spinee.2004.11.010
Neer CS 2nd (1987) Displaced proximal humeral fractures. Part I. Classification and evaluation. By Charles S. Neer, I, 1970. Clin Orthop Relat Res 223:3–10
Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, Prokuski L, Sirkin MS, Ziran B, Henley B, Audige L (2007) Fracture and dislocation classification compendium—2007: orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma 21(10 Suppl):S1–S133
Maresca A, Pascarella R, Bettuzzi C, Amendola L, Politano R, Fantasia R, Del Torto M (2014) Multifocal humeral fractures. Injury 45(2):444–447. doi:10.1016/j.injury.2013.10.010
Benetos IS, Karampinas PK, Mavrogenis AF, Romoudis P, Pneumaticos SG, Vlamis J (2012) External fixation for displaced 2-part proximal humeral fractures. Orthopedics 35(12):e1732–e1737. doi:10.3928/01477447-20121120-17
Ziran BH, Smith WR, Anglen JO, Tornetta P III (2008) External fixation: how to make it work. Instr Course Lect 57:37–49
Catagni MA (2003) Atlas for the insertion of transosseous wires and half-pins Ilizarov method. In: Malocchi AB (ed) Medi Surgical Video. Italy, Milan
Moroni A, Faldini C, Pegreffi F, Giannini S (2004) HA-coated screws decrease the incidence of fixation failure in osteoporotic trochanteric fractures. Clin Orthop Relat Res 425:87–92
Crates J, Whittle AP (1998) Antegrade interlocking nailing of acute humeral shaft fractures. Clin Orthop Relat Res 350:40–50
Modabber MR, Jupiter JB (1998) Operative management of diaphyseal fractures of the humerus. Plate versus nail. Clin Orthop Relat Res 347:93–104
Ingman AM, Waters DA (1994) Locked intramedullary nailing of humeral shaft fractures. Implant design, surgical technique, and clinical results. J Bone Joint Surg Br Vol 76(1):23–29
Reimer B (1998) Humeral shaft fractures-intramedullary nailing. In: Wiss D (ed) Master techniques in orthopaedic surgery. Lippincott-Raven, Philadelphia, pp 81–94
Chiu FY, Chen CM, Lin CF, Lo WH, Huang YL, Chen TH (1997) Closed humeral shaft fractures: a prospective evaluation of surgical treatment. J Trauma 43(6):947–951
Castella FB, Garcia FB, Berry EM, Perello EB, Sanchez-Alepuz E, Gabarda R (2004) Nonunion of the humeral shaft: long lateral butterfly fracture—a nonunion predictive pattern? Clin Orthop Relat Res 424:227–230
Yang KH (2005) Helical plate fixation for treatment of comminuted fractures of the proximal and middle one-third of the humerus. Injury 36(1):75–80. doi:10.1016/j.injury.2004.03.023
Mostafavi HR, Tornetta P 3rd (1997) Open fractures of the humerus treated with external fixation. Clin Orthop Relat Res 337:187–197
Conflict of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Uzer, G., Yıldız, F., Elmadağ, M. et al. Treatment of unusual proximal humeral fractures using unilateral external fixator: a case series. Eur J Orthop Surg Traumatol 25, 683–687 (2015). https://doi.org/10.1007/s00590-014-1579-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-014-1579-9